Abstract
France has first experimented, in 2009, and then generalized a practice level add-on payment to promote Multi-Professional Primary Care Groups (MPCGs). Team-based practices are intended to improve both the efficiency of outpatient care supply and the attractiveness of medically underserved areas for healthcare professionals. To evaluate its financial attractiveness and thus the sustainability of MPCGs, we analyzed the evolution of incomes (self-employed income and wages) of General Practitioners (GPs) enrolled in a MPCG, compared with other GPs. We also studied the impacts of working in a MPCG on GPs’ activity through both the quantity of medical services provided and the number of patients encountered. Our analyses were based on a quasi-experimental design, with a panel dataset over the period 2008–2014. We accounted for the selection into MPCG by using together coarsened exact matching and difference-in-differences (DID) design with panel-data regression models to account for unobserved heterogeneity. We show that GPs enrolled in MPCGs during the period exhibited an increase in income 2.5% higher than that of other GPs; there was a greater increase in the number of patients seen by the GPs’ (88 more) without involving a greater increase in the quantity of medical services provided. A complementary cross-sectional analysis for 2014 showed that these changes were not detrimental to quality in terms of bonuses related to the French pay-for-performance program for the year 2014. Hence, our results suggest that labor and income concerns should not be a barrier to the development of MPCGs, and that MPCGs may improve patient access to primary care services.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The health authorities of most OECD countries face a dual challenge in ambulatory health care delivery with both the shortage of health care supply and geographic imbalances [1]. Indeed, both aging populations and therapeutic innovations have drastically increased health care demand. On the outpatient care supply side, General Practitioners (GPs) are often overloaded and those wishing to retire find it difficult to attract locum doctors, in particular in remote rural areas and deprived urban areas where attracting new GPs has become a challenge for health authorities [2, 3]. In this context, which is common to many countries, fostering interprofessional teamwork has become a key goal of the reorganization of primary health care to align primary care provision with new health care needs [4].
Team-based primary care aims to improve continuity, accessibility, and the quality of health care by allowing a better sharing of medical records, an extension of opening hours, the implementation of multi-professional care protocols through interprofessional and intra-professional coordination.
So far, most of the literature has been devoted to understanding how teamwork contributes to improving outpatient care performance [5,6,7] and assessing both its impact on quality [8, 9] and its efficiency [10]. Moreover, group practices, especially those that include specialists, have been shown to be a significant driver of GPs’ choice of location and could be decisive in addressing the issue of medically underserved areas [11, 12]. However, promoting this type of primary care organization still faces many issues. From the health professionals’ point of view, collaboration and cooperation are quite demanding and the compensation of efforts and costs involved is uncertain. Hence, GPs wishing to join a Multi-Professional Primary Care Group (MPCG) may be discouraged from doing so by the perceived burden of different types of investments (the time required to adopt and organize a new practice style and information sharing, the uncertain implications of a larger scope and scales of functioning on costs, etc.), and may be subject to risk aversion or loss aversion behaviors. To our knowledge, little is known about the impact of a MPCG on GPs’ activity and even less on GPs’ income in France. Studying whether an MPCG is financially appealing for GPs is obviously essential to better apprehend the attractiveness and development of this practice model [13]. In addition, analyzing the impact of MPCGs on GPs’ medical activity may be useful to detect whether cooperation and coordination are effective in these structures and then contribute to the debate on the impact of primary care team organization.
In this paper, we provide new empirical results on the impact of reforms promoting multidisciplinary team-based practices by estimating their impacts on GPs’ income (self-employed and salaried incomes) and activity.Footnote 1 We used an original and rich database resulting from the pairing of National Health Insurance (NHI) medico-administrative data and doctors’ tax returns (DGFiP) over the period 2005–2014. We aimed to evaluate whether GPs’ income concerns could be a barrier to the development of MPCGs. We use the quasi-experimental framework provided by a French pilot program that experimented then generalized an accreditation which led many GPs to enroll into MPCGs. Thus, we studied the impact of the enrollment of GPs in a MPCG on their income (self-employed and salaried incomes), activity (patients seen and medical services), and, for 2014, the quality of care provided assessed through the French pay-for-performance (P4P) scheme. To address selection bias at GPs’ level, we used both the properties of a coarsened exact matching to identify a controlled group and difference-in-differences estimations using a fixed-effects model.
We found that between 2008 and 2014, GPs’ income increased by more than 10%, but GPs in MPCGs benefited from an additional increase of around €2000 (+ 2.5%). Furthermore, the number of patients seen at least once per year by GPs increased more rapidly for those who joined a MPCG: 4% more (about 80 patients per year) than their colleagues over the period, without resulting in a significantly different increase in the number of medical services delivered (office visits, home visits, and technical procedures). In addition, an analysis of P4P payments for GPs in 2014 showed that GPs practicing in MPCGs received around €600 (+ 9%) more than their colleagues.
The rest of the paper is organized as follows. Section 2 presents the French context, the main-empirical evidences on the impacts of team-based primary care, and the theoretical hypotheses on the potential effects of an MPCG practice on activity and income. Section 3 describes our data and the construction of the control group using the coarsened exact matching method. Section 4 presents the empirical strategy and Sect. 5 presents the main results and the robustness checks. Finally, Sect. 6 discusses the main results and concludes.
Background and theoretical framework
The French primary care system and the MPCG reform
The French primary care system is essentially publicly funded—the National Health Insurance finances two-thirds of the outpatient’s care expenditures and the remaining third belongs to households and complementary health insurance—and privately delivered by self-employed health professionals. In 2019, GPs are still mainly paid through a fee-for-service system (FFS) even if the payment mechanisms have become increasingly mixed over the past decade: in 2018, 88% of GPs’ payments were linked to FFS, 4% to per capita payment, and 8% to other payments, including continuity of care and P4P [14]. Indeed, since 2004, patients have been strongly encouraged to choosing and register with a GP as its “family GP” (also referred as registered patients in the paper) [15] and, in return for this gatekeeper role, GPs are compensated by a per capita payment roughly adjusted to risk: for example in 2019, €5 for ‘normal’ patients (from 7 to 79 years old), €6 for children under 6, €42 for patients over 80 or with chronic disease and €70 for patients over 80 and with chronic disease. For French doctors, the regulation mainly concerns the billing system: while some doctors are allowed to charge extra fees, overbilling, almost all GPs only charge regulated fees.Footnote 2 Besides, self-employed GPs are free in terms of location, practice style (solo or in teams), having an additional salaried activity (in a primary care center, hospitals or other).Footnote 3
Before 2008, multi-professional primary care teams remained a marginal way of practice in France with approximately ten structures in 2008 [11]. To foster the creation and development of MPCGs, an innovative add-on payment pilot scheme for multi-professional coordination dedicated to MPCGs was scheduled for an initial period of 5 years (2009–2013). The experimentation reached 150 MPCGs participant and the pilot scheme was extended to 150 additional MPCGs in 2014. Bolstered by the globally positive results from the evaluation [16] and supported by federations of health professional, the accreditation’s pilot was generalized in 2015.Footnote 4 Both the creation and accreditation process of MPCGs are on a voluntary basis but obtaining the accreditation, allowing to receive add-on payment, requires a formal application from the MPCG to the regional health authorities and compliance with important specifications (a health care project involving all professionals, a shared information system, days and opening hours to promote continuity of care, etc.). In 2015, around 400 MPCGs were accredited and more than 900 at the end of 2019. The average composition of accredited MPCGs has been quite stable since 2014 and was close, in 2017, to 10 full-time equivalent non-medical health care professionals (9.9, essentially nurses, but also physiotherapists), 4.8 GPs, 1.1 pharmacists, 0.5 midwives, 0.5 dental surgeons, 0.3 specialists, and 0.6 other care professionals. The estimated average yearly GPs’ patient list size is around 4380 patients for registered patients and 6500 for encountered patients. Around 10 million patients would be followed by GPs in an accredited MPCGs in 2019. Note that MPCGs without accreditation also exist, hence without receiving the associated funding. Though they cannot be identified in our study, we know from the previous literature that non-accredited MPCGs were around half of the total number of MPCGs in 2016. In this study, we focus on GPs joining accredited MPCGs between 2008 and 2014.
As any self-employed GP, GPs in the accredited MPCGs are paid individually, while the accredited MPCG also receives an add-on payment based on three predetermined set of targets: enhancement of accessibility for the patients (e.g., opening hours from 8 a.m. to 8 p.m. or opening hours without requested appointments during the week), multi-professional coordination and cooperation (time dedicated to coordination, development of multi-professional care guidelines, etc.), and information sharing (acquisition and use of accredited electronic medical records). Fulfilling a target is associated with a number of points, for each of which €7 are directly paid to the MPCG, at structure level, and which are used in a discretionary way. This add-on payment for the structure also depends on the total number of registered patients of all GPs involved in the MPCG and reached around €50 K per year for a team of 13 professionals in 2014 and €70 K in 2017. To our knowledge, this additional payment is most often used to remunerate a doctor or other professional dedicated to organizing coordination within the structure and with local partners (full-time or part-time), to cover investments such as the shared information system and its maintenance, to compensate the doctors themselves for the time spent for cooperation protocols with non-medical health care professionals, or even to recruit external professionals to improve care [16, 17].
Related literature
Promoting multi-professional group practices—i.e., increasing both horizontal and vertical integration, interprofessional work cooperation, and task substitution—aims to improve the efficiency and quality of primary care. This is a common trend in many countries [4, 18], so their potential virtues are now quite well acknowledged, and they have been empirically tested in an increasing number of studies.
According to organizational economics, intra-professional and interprofessional coordination and integration should improve doctors’ practice efficiency by allowing both economies of scope and scale. The complementarity of professionals within the teams should improve productivity (e.g., management of complex cases and chronic diseases), while the substitution of tasks should be facilitated (between nurses and GPs, for instance) and improve the allocative efficiency of care provision. The propensity of professionals working in MPCGs to effectively collaborate and the incentives that may promote cooperation remain crucial issues [19, 20]. The extent of potential economies of scope and scale also depends on the size of the group and its heterogeneity [21,22,23,24]. However, some studies have shown evidence of efficiency gains [16, 23, 25, 26]. Moreover, Rosenman and Friesner [24] found that the efficient allocation of the skills of different health professionals is usually achieved in practice, both within exclusive and non-exclusive primary care teams, though technical inefficiencies may arise. Thus, at a minimum, a reduction in the cost of care is to be expected, since the “least expensive” (qualified) professional takes care of each patient. In addition, as it has been argued by Strumpf et al. [10], any expected improvement expected in teamwork in terms of the quality and coordination leading, for instance, to an enhancement in the diagnosis, treatment, and management of a disease should result in a reduction in the rates of health care use and particularly of specialist use. In their context of patients who already have a good insurance, allowing them to easily access to primary care, this should imply an overall decrease in cost of care. Although the authors found that teamwork can reduce utilization rates in primary care, they concluded that the associated cost reduction did not offset the costs of implementing the reform.
MPCGs are also intended to improve continuity, accessibility, and the quality of health care. Regarding quality, for instance, the proximity and coordination of the professionals from different disciplines are supposed to improve the management of complex cases and chronic disease [27,28,29,30]. In addition, teamwork should facilitate the organization of extensive opening hours thanks to a better sharing of information and the ability of health care professionals to replace one to another, which seems to be confirmed by the perceptions of patients, who confirm that MPCGs have a positive impact on their access and on the quality and coordination of care [8]. Moreover, enhanced access can reduce the utilization of emergency care, though the evidence is mixed and may be dependent on the characteristics of the patients considered as the level of their insurance [10, 31].
However, the development of MPCGs remains slow [32] because of more or less strong barriers, such as the predominance of FFS payments that does not provide incentives for practitioners to work together, and the excessive compartmentalization of the medical professions. Hence, to promote teamwork, policy makers have tried to remove these barriers by promoting Multi-professional Primary Care Teams (e.g., Primary Care Medical Homes in the US, Family Medicine Groups in Canada, and accredited MPCGs in France), recognizing the new status of professionals with advanced practices, and by implementing additional payments (at the practice or group level). The payment mix aims to address the trade-off between the propensity of revenue-sharing to both foster collaboration, and degrade the individual’s incentives to increase productivity and avoid free-riding behavior [6, 33, 34]. Besides payments issues, it seems that MPCGs are attractive per se: although it depends on the propensity of professional to effectively collaborate [20, 35, 36], it appears that teamwork can increase satisfaction at work [9, 37] and allows GPs retainment in less attractive and medically underserved areas [11, 12].
How practicing in MPCG may affect GPs’ net income: potential mechanisms
This paper contributes to the previous literature by addressing the attractiveness of MPCGs from a financial perspective and examining whether GPs’ incomes may constitute a potential barrier or, on the contrary, reinforce the attractiveness of teamwork. The literature has widely documented the influence of financial incentives on GPs’ activities [26, 38,39,40] and location [15, 41,42,43]. Ammi et al., 2019 have recently shown that higher revenues favor the retention of care professionals within the primary care team [13] and, thus, there is no reason to believe that financial incentives (e.g., expected income) do not affect the decision to join an MPCG, as well. The following describes the main ways in which practicing in MPCGs can increase or decrease the net income of GPs, either through production costs or gross revenues.
As already mentioned, the impact of teamwork on production costs essentially results from economies of scope and scale. Most of the gains concern investment in equipment and running costs that are common and transversal within and between the disciplines and professions in a MPCG. Although cost reduction could also be achieved through the increased bargaining power of groups with respect to medical providers or insurers, it is not likely in France because of the important role of public health authorities in terms of both the share of funding and the regulation of the health insurance market. At the same time, teamwork can lead to additional costs such as the acquisition of a shared information system and salaries to compensate for time spent on cooperation (for health professionals or for an additional person in charge of cooperation within a MPCG) [44, 45]. Overall, whether integration leads to reduced average cost or not, it raises questions about the optimal size of primary care firms [21,22,23,24], which should also depend on the teams’ heterogeneity: the higher the number of professions and disciplines, the higher the coordination cost to achieve the allocative efficiency of care production.
In terms of gross revenues or annual revenue, the impact of teamwork should essentially depend on the capacity of teamwork to free up GPs’ working time and their propensity to use it to increase their medical activity. Indeed, in the French system, general practitioners practicing in an MPCG remain subject to the regulated FFS schedule, so teamwork should not lead to price effects, or only indirectly through the few other GPs who can charge extra fees. Moreover, the transfers dedicated to accredited MPCGs associated with the reform remain quite low compared to the sum of the incomes of all doctors and other health professionals involved in the MPCGs and should not significantly change the GPs’ well-known incentives related to FFS [40], nor induce substantial shirking strategies and moral hazards [6]. As a result, most expected revenue effects should be related to organizational changes in MPCGs’ care delivery and to the demand response to these changes. On the supply side, complementarities between professionals should smooth production of the whole group. At the same time, the delegation of non-medical tasks could free up medical work time for GPs, while the delegation of medical tasks may have a more ambiguous impact. GPs covering for each other, for instance, and GP-nurse substitution can be regarded as infra-firm competition as long as the residual demand for primary care is low [46, 47]. We believe that infra-firm competition should only be a little concern in France, since MPCGs are mostly concentrated in medically underserved areas where demand exceeds supply. However, the impact of delegating medical procedures on GPs’ income will also depend on the type of services concerned, since FFS payments are usually calibrated to remunerate the average cost of the services provided. Assuming, for instance, that the GP delegates mostly costly, time-intensive, services (e.g., therapeutic education or screening for cognitive impairment) to nurses, the GP could gain revenue if the regulated fee remains unchanged.
A larger patients list can also increase GPs’ revenues to the extent that, in France, the GPs receive per capita payment for following patients as their family practitioner and following patients with chronic disease. Indeed, one can expect the proximity of different services (one-stop-shop model), the implementation of extended opening hours, the fact that GPs cover for each other, and quality improvement should also contribute to enhancing the attractiveness of MPCGs for patients (and professionals). Another source of revenue effect concerns the French P4P program implemented in 2012. This payment created a positive revenue shock for all GPs, but might benefit even more to GPs in MPCGs if those primary care organizations are associated with quality improvements. Finally, financial attractiveness is obviously not the only GPs’ concern. Ultimately, it is perfectly believable that interaction between GPs and other health care professionals may improve working conditions and satisfaction at work in ways that conflict with financial concerns. According to labor-leisure trade-off, for instance, GPs may positively value a decrease in their workload thanks to tasks’ substitution, even though depending on the nature of the delegated tasks (see above), it can be at the expense of their own income.
Thus, multi-professional teamwork does not, a priori, have a clear effect on income, either in terms of costs or gross revenues. This study aims to explore the overall effect of practicing in MPCG on GPs’ income in the context of the French reform in which GPs are considered the pillar of any MPCG. To this aim, we will also analyze the impact of MPCGs on GPs’ medical activity in terms of both the quantity of medical services and the number of patients seen, to highlight the organizational features of MPCGs and their impact with respect to FFS and capitation payments.
Data and material
Data
We used an exhaustive anonymous administrative database that combined National Health Insurance data on self-employed GPs’ medical activities with information on both their earnings and family structure from household tax returns provided by the General Directorate of Public Finances (so-called “appariement Cnam-DGFiP”). The database provided information for the years 2005, 2008, 2011, and 2014 from which we essentially use 2008 and 2014 waves. Indeed, information from the 2011 wave cannot be identified as pre- or post-treatment period for each GP and, therefore, will not be used for our analysis, while 2005 data are mostly used for pre-treatment analyses and robustness checks. Furthermore, we used a taxonomy of the French living areas that captured the territorial heterogeneity of health care supply and demand between six clusters: peri-urban areas, rural and remote areas, retirement and tourism areas, urban deprived, heterogeneous cities, and privileged suburbs [48].
Medical activity, case mix, and gross revenues
In addition to the standard socio-demographic characteristics of GPs’ (gender, age, seniority of private practice, and location), administrative data provide detailed information on self-employed medical activity: the number of visits and technical procedures, GP’s gross revenues (related to FFS and to other private practice payments), the number of patients encountered at least once a year and the number of patients registered (followed in their role as family GP), and case mix (the respective share of the patients seen at least once by age, gender, chronic disease, and by beneficiaries of free complementary health insurance for deprived members of the French population). We distinguished three categories of service: office visits, home visits, and technical proceduresFootnote 5 as the fees vary according to the service. Since the French P4P reform was introduced in 2012, we observed the P4P bonus received by GPs (ROSP) in 2014 only. Finally, the database detailed whether, in 2014, a GP belonged to an accredited MPCG or not. However, we were unable to identify which MPCG a GP worked in and exactly when a GP joined an MPCG.
GPs’ income and family structure
From tax returns, we obtained the total net labor income of the GPs corresponding to the sum of the possible wages (salaried activities), and the total net self-employed income corresponding to the total gross revenues minus the total expenses, of which we did not have details (running costs and professional expenses such as social contributions, office rent, vacuum payments, etc.). Hence, the net self-employed income accounted for the impact of the add-on payments dedicated to MPCGs onto GPs income whenever they were redistributed to the professionals or used to cover costs that otherwise would have been incurred by the professionals. We also had original information on the family status of GPs (married/civil partnership/single/divorced/widowed; the number of children, and their respective years of birth), which is known to be an important determinant of GPs activity [49].
Study sample
There were over 58,351 self-employed GPs in 2014; 1548 practiced within an accredited MPCG. We excluded GPs who had a specific activity: GPs authorized to charge extra fees, GPs who exclusively carried out specific procedures (acupuncture, homeopathy, etc.); GPs who had an uncomplete year of activity; and those who were aged 66 and over (see Fig. 1). After some other controls, our study sample included 41,775 GPs in 2014, among whom 30,541 (844 within a MPCG) were followed over the 2008–2014 period.
The profile of GPs enrolling in MPCGs between 2008 and 2014
The first sets of columns of Table 1 show descriptive statistics of the GPs in 2008 for both the GPs who later joined an accredited MPCG and those who did not, thus exhibiting the self-selection regarding enrollment into MPCG. Indeed, The GPs who joined an accredited MPCG between 2008 and 2014) were more likely to be men, on average younger, more often in a couple (married or civil partnership), and had on average more young children, the latter two being known to affect the labor-leisure trade-offs within households in a gender-dependent manner [49]. Furthermore, we observed large disparities in terms of geographical location: GPs from the treatment group were heavily concentrated in rural and peri-urban areas with lower access to primary care, and where overloaded GPs had a higher average income (the GPs in underserved areas provided in around 20% more services than in non-underserved areas both in 2008 and 2014). In addition, they more frequently had a regular additional salaried activity, i.e., received an annual wage higher than €4000 (corresponding roughly to 5% of the average gross revenue) in addition to their self-employed activity. This may be related to the higher organizational flexibility that one can expect in MPCGs and that may be attractive for GPs already having additional salaried activity. Finally, a higher proportion of GPs working outside MPCGs performed specific procedures (homeopathy, acupuncture, etc.) as a non-exclusive activity (for which different fees apply).
Empirical strategy
Our empirical strategy aims at controlling for the self-selection into MPCG and proceeds in two steps: first, we built a control group by coarsened exact matching (CEM) [50], and then, we use parametric difference-in-differences design with fixed-effects estimation to identify the impact of having joined an accredited qMPCG on the evolution of GPs’ income (inter alia) over the period 2008–2014. The two steps complement each other. Preprocessing data with matching intend to increase the robustness of our further analyses: it reduces model dependence [51] by reducing our exposure to bias from model misspecification regarding nonlinearities and interactions terms involving the matching covariates (to the extent that they are well balanced between the treated group and the control group).Footnote 6 However, matching does not allow to capture the unobservable individual heterogeneity regarding, for instance, GPs’ abilities or tastes relative to their practice. We then relied on the quasi-experiment feature of the MPCG reform to use a difference-in-differences (DID) design together with fixed effect estimator to get rid of both observed and unobserved GPs’ time-invariant preferences and characteristics and limit bias due to any permanent differences between treated and controls in our estimates of the effect of practicing in accredited MPCGs.
Identification of a control group
The size of our study sample, and particularly the number of non-MPCG GPs, made possible to use a, non-parametric, exact matching method to balance the treated and non-treated GPs’ distribution over: age, number of years in private practice, gender, living areas, family status, number of children, and type of practice, i.e., whether or not the GP had an additional salaried activity and whether or not the GP performed specific procedures (see the “Appendix” for a more detailed presentation of the matching procedure). We chose not to include pre-treatment outcome as matching criteria for two reasons: a recent literature has pointed out the risk that it introduces time-varying bias [52, 53] and its justification when matching is combined with DID design remains unclear when the common trend assumption is reasonable. Next, given our set of matching criteria, we took advantage of the possibility to use CEM which approximates a fully blocked experiment and can achieve lower imbalance [54]. Hence, for instance, using CEM gives us the guarantee that the proportion of women in rural areas within a given age category is balanced among the treated and control group. Finally, to retain as much information as possible, we chose to use weights for controls’ GP over randomly sampling a fixed ratio of control for each treated GP (which amount to use only 0 and 1 weights) as in m-to-1 ratio approach. Defining weights by CEM allows to estimate the average treatment effect on the treated (ATT), and its standard errors by classic methods provided that the weights are used in our regressions [55].
The first two sets of columns of Table 1 describe the differences in 2008, i.e., prior the MPCGs’ accreditation was created (or even experimented) between the GPs who joined MPCGs later on and the other GPs, first before then after balancing socio-demographic and territorial distribution by matching. There were no significant differences between GPs (in or outside an MPCG) in terms of the number of medical services (office and home visits and technical procedures) and total net income in the 2008 pre-reform period after matching. Income and total activity differences in the original closed panel were, most likely, essentially due to the concentration of MPCGs in areas with an excessive workload (rural and peri-urban areas). The GPs in MPCGs saw more patients in 2008; this persisted after matching suggesting that, beyond socio-demographic and location considerations, the GPs who chose to join MPCGs had a particular approach to primary care practice which differed from the average GP, since they provided fewer medical services per patients. Such differential support the need to account for GPs unobserved individual characteristics and preferences in complement to the matching approach in our further analysis. Now concerning the post-matching description of trends, the differentials in terms of total net income, however, evolved in favor of GPs working in a MPCG in 2014, while the difference in terms of the number of patients seen and registered was widening (see the last two columns of Table 1). The remainder of the analysis is dedicated to parametrically testing the impact of joining accredited MPCGs using methods that enable to further address the GPs’ self-selection into MPCGs.
Parametric difference-in-differences with individual fixed effect
Like the classic DID setting, our identification strategy rely on the assumption of common trends between the two groups for all variables of interest. With regard to the two-pre-reform periods of observation (2005 and 2008) that were available, the assumption of common trends was reasonable for our three main outcomes (see Fig. 2 below and Table 4 in “Appendix”), i.e., incomes, number of patients seen at least once, and medical services (visits and procedures).Footnote 7 Given the secular trends of outcomes, this assumption is key as control GPs provide a counterfactual for what would have happened to the treated GPs in 2014, the post-treatment period, if they did not enroll into accredited MPCGs. Furthermore, we neutralized the effect of time-invariant GPs’ preferences and characteristics using (a.k.a. within transformation) to estimate the following fixed effect model by OLSFootnote 8:
where \(Y_{it}\) is one of the outcomes of interest, says income, for the GP \(i\) at year \(t\); \(\alpha_{i}\) is the individual fixed effect, \(d2014_{t}\) is a time dummy, and \({\text{MPCG}}_{it}\) a dummy indicating whether the GP \(i\) were treated (joined an accredited MPCG) at year \(t\). \(X_{it}\) is a vector of covariates varying over time, including those used in the matching process (if time-varying) and further control. While \(\lambda\) captures the effect of the time trend over the 2008–2014 period, \(\delta\) is the parameter of interest giving the estimated effect of joining a MPCG between 2008 and 2014 on the evolution of \(Y_{it}\) over this period.
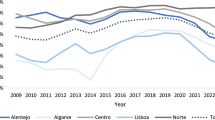
Figure 2 shows the trends of incomes, the number of patients seen at least once, and the number of services for the treated and control GPs, respectively. Even though the observation point 2011 could not be identified as a pre- or post-treatment period, it is included in Fig. 2 for the sake of the exhaustivity of the descriptive analysis. The most noticeable differential change in trend seems to have occurred between 2011 and 2014 and is most likely explained by the fact that many of the GPs that chose to practice in accredited MPCGs did after 2011 (even for those participating to the experimentation started in 2009, since it takes times to build a MPCG project). Also notice that not all the GPs in our closed panel (2008–2014) were observed in 2005, so we retained all those who were observed in 2005 for the graph below (our conclusions are robust to an alternative approach; see the section dedicated to robustness checks for more details).
Because the family GP reform was introduced in 2004 and patients registered rather slowly, the information on the number of registered patients was not usable for causal analyses prior to 2011. Instead, we decided to provide complementary cross-sectional OLS estimations of the effect in 2014 of practicing in MPCGs on both the breakdown of patients (non-registered or occasional and registered patients) and the P4P received by the GPs (for which information was available in 2014 only). These results enrich our understanding of the impact of practicing in a MPCG on essential dimensions, such as attractiveness, patient coverage, and the quality of care.
Results
The effects of practicing in a MPCG
Table 2 presents estimates using different models. On the left-hand side, the effects of the different covariates are presented concerning total net income using a pooled DID setting without fixed effectFootnote 9 (1) and different fixed-effects model specifications (2–4): first, the baseline model (2) that estimates the overall treatment effects and nested models, including controls for GPs’ medical services (3) and case mix (4). On the right-hand side of the table, the effects of the different covariates are presented concerning GPs’ activity measured by the number of medical services and the number of patients seen, which we both assumed as essential drivers of income variation through GPs’ gross revenues.
We found that joining an MPCG was associated with a faster increase in GPs’ total annual income in a consistent way across the different models; where models (3) and (4) both allow to assess the income effect of the reform which is not related to changes in the activity of GPs. Furthermore, we found that joining an MPCG had an overall non-significant impact on the number of medical services provided, but a positive impact on the number of patients seen at least once during the year. It suggests that MPCGs made it possible to attract and provide health care for a larger number of different patients (column 6); this may partially explain the faster increase in GPs’ total income, since the magnitude of the income effect is lower when, in addition to medical services (model 3), the number of patients seen is also controlled for (model 4). Indeed, a higher growth in the number of patients seen increases the probability of GPs following more patients in their role as family GPs and receiving higher per capita payments. In addition, one can observes that evolution of the composition of the patient seen from Table 2 did not indicate that GPs tended to select healthier patients after joining MPCGs, so that the explanations for their propensity to faster increase the number of patients they seen without providing more services are mostly likely related to team coordination properties.Footnote 10 Finally, though it is non-significant, the average slowdown of the number of medical services (paid through FFS) in MPCGs is consistent with a larger income effect of working in MPCG, once differences in terms of annual medical services are controlled for (model 3).
The socio-demographic and territorial effects on income were much as we expected, but many of them cannot be reliably identified by the within estimator due to the non-variation (or too low) of such variables over time and thus were estimated in the pooled OLS model (1) only. In model (1), we observed that GPs living in medically underserved areas (peri-urban, deprived urban, and rural and remote areas) had significantly higher incomes due to their heavy workload. GPs’ ages exhibited the usual non-linear concave (inverted U) relationship with incomes, and in line with the previous studies [49]. The effect of the number of dependent children appeared to be strongly gender-dependent and transmitted through activity effects, so that their impacts on income were non-significant, once medical services were controlled for in models (3) and (4). The NHI information about medical services and the number of patients seen concerned self-employed activity only; we consistently found that the levels of both were on average lower for GPs with an additional salaried activity, confirming some degree of substitution between the GPs self-employed and salaried activities. Perhaps, more remarkably, we found that GPs with an additional salaried activity earned on average more than other GPs. We believe that this may be due to the overall higher volume of activity of these GPs who, on average, seem to work half a day a week more than other GPs. In other words, salaried activity and self-employed activities were, at least, partially complement instead of only substitute; this is particularly understandable if additional salaried activity concerns on-call coverage or continuity of care in ambulatory health services (this is supported by specific descriptive analysis of these GPs, which are available on request).
Complementary cross-sectional results
Table 3 presents some complementary results obtained by cross-sectional analysis in 2014 to further highlight the composition the patient encountered by GPs and GPs’ care quality assessed through their performance to the French P4P program. The estimating equations are as follows:
where \(Y_{i}\) is the outcome of interest for GP \(i\) in 2014, and \(\delta\) is the parameter of interest giving the estimated differential between MPCGs’ GPs and other GPs’ outcomes. In addition, \(X_{i}\) control for a set of individual characteristics including socio-demographics, living areas, and further case-mix covariates are included to estimate the P4P payments differential in 2014 and are detailed hereafter.
The French P4P payments were introduced in 2012 and concerned all GPs whether they practice in MPCGs or not. The calculation of P4P payments depends on the number of patients registered to the GP as “family GPs”. In addition, obtaining the points rewarding GPs’ good practices regarding the care of patients with a specific condition, such as a chronic disease, requires having treated a certain number of patients with such a condition during the year. Hence, to reflect good practice indications and not volume or case-mix effects, we controlled our P4P payments analysis for the number of patients with a chronic disease, the number of patients registered to the GP as “family GPs” and shares of patients under 16 years old and above 65 years old (in addition to the control previously used). We found that GPs that joined an MPCG between 2008 and 2014 received significantly higher P4P payments than the other GPs in 2014. The P4P differential cannot be imputed to the MPCGs exercise, since the quality differential could have pre-existed the GPs’ entry into MPCGs and, hence, it cannot directly corroborates the literature about the positive relationship between multi-professional teamwork and the quality of care. However, regarding our previous results, at least two things can be inferred: P4P payments may also have contributed to the higher evolution of MPCGs’ GPs’ income and their propensity to see more patients without providing more medical services has not led MPCGs’ GPs to provide care of lower quality than the other GPs.
We also found that the difference in terms of the number of patients seen by GPs in MPCGs was driven by a larger number of both non-registered or occasional patients (+ 175 per year) and patients registered to the GP as “family GPs” (+ 49 per year). These additional results support our interpretation of the role played by the number of patients seen and capitation payments on MPCGs’ income effect captured by model (4) of Table 2. Notice that a panel analysis on the composition of patients seen would have led to a similar conclusion (available on request), but the interpretation of its evolution was made complicated by the slow adhesion of patients to the family GP reform, which could not be considered as stable until 2011.
Robustness checks
We conducted a series of robustness checks to ensure the reliability of our results.
We first performed a placebo falsification test of the common trend assumption by running the same regressions on the 2005–2008 pre-treatment period, hence allowing a specific trend for GPs who will join MPCGs later on (see Table 4 in “Appendix”). Because our pre-reform trend analysis could also be affected by the absence in 2005 of some of the GPs followed in the 2008–2011–2014 panel, we ran the matching and the parametric analyses by retaining only GPs observed during the 2005–2014 period, and obtained very similar results despite the loss of around a hundred GPs in MPCGs. We also evaluated the role of potential outliers by discarding the first and last percentile of GPs’ regarding self-employed income and the number of medical services, and obtained similar, slightly stronger, results. Given that we observed the GPs’ additional salaried income but not their related medical activities, we reconducted our analyses after excluding the GPs with additional salaried activity and reached the same conclusions. We ultimately stratified our analyses over medically underserved living areas (rural and remote, urban deprived, and peri-urban) where MPCGs’ GPs are concentrated vs non-medically underserved areas (privileged suburbs, heterogeneous cities, retirement, and tourism) and verified that our results were essentially driven by the GPs in underserved areas. However, due to the lack of statistical power only 228 GPs exercise in MPCGs, we doubt that anything can be inferred from the analysis in the non-medically underserved areas (see Table 5 in “Appendix”).
To assess the robustness of the results to our matching strategy, we ran our parametric analyses on different control groups. In particular, we used Propensity Score Matching (PSM), retaining the three closest neighbors for each treated unit, to evaluate robustness regarding our choice not to match in pre-treatment outcomes in our main analysis. Namely, the additional matching criteria which we used in the PSM matching include GPs’ pre-reform gross revenues, self-employment and salaried incomes, medical services, number of patients, and case mix to balance the distribution for the control and treatment group. Our results were robust (see Table 6 in “Appendix”) and balancing outcomes and case mix in 2008 did not appear to be crucial for our panel analyses. However, PSM leads to randomly discards considerable information [54] and we found it mostly appealing to palliate the impossibility of accounting for pre-reform differences using DID design in our, complementary, cross-sectional analyses (see Table 7 in “Appendix”).
Our analyses are also robust to different model specifications and the main differences that we highlighted correspond to model (3–4) in Table 2 and are consistent. Regarding our inferential assumption, we accounted for heteroscedasticity and decided to be conservative and allowed for errors to be dependent between GPs up to county level (also known as départements in France, of which there are 96). Unfortunately, we were not able to cluster at the GPs’ group level, as we thought it was the most relevant cluster, because we could not know which GPs worked together. In contrast, clustering at county level was likely an unnecessarily high level of clustering.
Discussion
We show, based on our quasi-experimental design and analysis, that incomes significantly increased for all GPs between 2008 and 2014, but that the increase was significantly faster (+ 2.5%) for GPs who joined accredited MPCGs during the period. We also show that this additional increase was associated with a greater growth in the number of patients seen at least once a year by GPs in MPCGs, without a more rapid increase in their provision of medical services (number of office or home visits and technical procedures). Thus, these results may be interpreted as first, MPCG practicing does not constitute a financial barrier for GPs and, second, the change in GP’s behavior is at the extensive margin—the number of patients seen—and not at the intensive margin—the amount of care and services delivered. In addition to these results and based on our cross-sectional analysis for the year 2014, we show that MPCGs’ GPs do provide care of better quality according to the average P4P payments which the GPs received. Moreover, our results suggested that the increasing number of patients seen by GPs practicing in an accredited MGPC compared to other GPs was due to an increase in the number of both occasional and registered patients, without any evidence of risk selection detrimental to patient accessibility.
All things considered, our results not only suggest that the additional payment at the practice level for accredited MPCG succeeds in preventing financial barrier for GPs, but also seems to succeed in supporting the organizational properties of teamwork that helps GPs in MPCG to see and follow more patients without increasing the quantity of their delivered services. This reform appears to favor coordination and cooperation, and this interpretation is consistent with the results of qualitative sociological studies on this reform [35]. Furthermore, the organizational impacts of MPCG on the activity of GPs may also suggest that multi-professional team-based primary care could be a relevant way to remedy the shortage of medical time in primary care by increasing the number of patient a GP can follow, particularly in underserved areas where a large majority of them are located. To that extent, this suggests that the accessibility to primary care is also improved thanks to MPCG.
However, our analysis presents some limits and raises a number of questions.
First, one should analyze the financial sustainability of multi-professional teamwork outside the accreditation created by the French MPCG reform. Indeed, we mentioned that the accreditation gives rights to additional payments made at the team level to cover some of the costs incurred by MPCGs and foster development of this primary care organization. To our knowledge, the annual amount received by average MPCG teams of 13 professionals as part of their accreditation reached around €50 K in 2014 and €66 K in 2017. Our data did not enable us to identify how these additional amounts were used or which amounts were actually distributed to each professional, since MPCGs have a complete discretion over the use and sharing of the add-on payments. Hence, whether the payment related to the accreditation of MPCGs is essential to their financial sustainability can only be assessed through rough extrapolations and whether the reform is cost efficient from the regulators’ point of view remains an open question that should be further investigated. Nevertheless, our results suggest that the amounts transferred in 2014 are at least sufficient to cover the financial costs related to multi-professional teamwork (if any), since MPCGs GPs did not experience income losses, and, beyond costs, that MPCGs may offer policy makers some advantages in terms of accessibility for patients and in terms of activity and attractive incomes for GPs.
Note that the satisfaction of GPs is obviously not limited to the dynamic of their income. The previous studies have already suggested that MPCGs could, in addition, increase satisfaction at work compared to solo practices, but little is known in France about working conditions and working time in MPCGs, though it seems not to affect the number of days worked [16]. Typically, any revenue decrease may result from a reduction of both activity and working time in MPCGs and this could be positively perceived by GPs with an excessive workload in medically underserved areas. Information about working time was not available for the GPs or for teams, and this would be invaluable to address the productive efficiency of MPCGs. Indeed, though GPs’ ability to treat a larger number of patients without increasing the quantity of services which they provided seems promising for policy makers, it stresses the need to highlight MPCGs’ impact in relation to inputs (including other primary care professional workforce) and the need to better understand their organizational properties.
This study focused on the accredited MPCGs and not on monodisciplinary teams and unaccredited multi-professional teams. It was impossible to take the typology of group practice into account due to lack of information in the data. However, thanks to both the large number of GPs in the study sample and the empirical strategy of using a weighted CEM, we reasonably believe that this limit does not call into question our results. Finally, our study design involved considering only those GPs already practicing in 2008 and, therefore, excluded all GPs who settled after that. Given that young GPs beginning their careers tend to work in a group setting and potentially in multi-professional teams, our analysis is de facto deprived of a significant number of young GPs who recently joined accredited MPCGs with a dynamic activity, and which offer a greater ease of adopting a new practice style in coordination with other professionals.
Finally, this study benefited from a rich database that made it possible to use exact matching on several socio-demographic and territorial dimensions, which are known to play a very significant role in GPs’ activity and income. As interim results, it allowed descriptive statistics to assess how MPCGs’ GPs differs from other GPs beyond those dimensions, and therefore constitute the originality of this study. Our results are novel and complement the results of other recent studies that evidence the benefits of MPCGs in terms of quality and cost efficiency. We believe that further work should now be devoted to better understanding the impact of MPCGs on the activity of nurses and other professionals involved in MPCGs to apprehend the sources of efficiency of these organizations at structure level.
Notes
This study is part of a broader evaluation project that aims to address several aspects of MPCGs using a mixed methods approach.
GPs who have fulfilled certain conditions can enter into a contract authorizing them to charge extra fees, which derogates from the standard fee schedule. They account for 10% of the self-employed GPs and will not be discussed further as they will be excluded from our study sample.
25% of GPs had additional salaried activities in 2014, and the associated income represented on average 20% of their total income.
The decrees of 23 February 2015 and 24 July 2017 endorsed a continuation of the scheme and presented the eligibility frameworks for voluntary structures (Accord Conventionel Interprofessionnel pour les Structures de Santé Pluriprofessionnelles de Proximité).
Technical procedures, such as stitches or imaging, for example, involve specific fees that are added to the regulated fees for the consultation.
Matching with different criteria including pre-treatment outcomes has also been performed to check the robustness of our results. It involved the use of propensity score matching to better deals with the several continuous matching criteria (see Sect. 5.3 for more details).
This assumption was, furthermore, supported by robustness analysis that parametrically tested the existence of differences in trends before 2008 (see Table 4 in Appendix).
More precisely, we used the felm function from the R package lfe with dummy variable for treatment and time (which amount to use xtreg, fe function in stata). We opted for introducing a time dummy over using the two-way fixed-effect estimator (which is equivalent in our setting), in order to acknowledge the trend of the control group.
The pooled DID model, (1), that we estimate by OSL was: \(Y_{it} = \alpha + \alpha_{g} {\text{MPCG}}_{i} + \lambda d14_{t} + \delta MPCG_{i} *d14_{t} + \beta_{1} Z_{i} + \beta_{2} X_{it} + u_{it}\), where \(\alpha_{g}\) captures the permanent difference between the group of treated and control GPS in the spirit of classic DID setting and \(Z_{i}\) is a vector of constant covariates over time. The pooled DID model does not fully exploit our individual panel dataset and, in principle, is less accurate for our purposes. However, it can be used as a benchmark and allows to estimate the interesting effects of time-invariant characteristics such as gender or living areas effects.
Those descriptive analyses have been further confirmed by replications of our parametric analyses to test dynamics differential in terms of the share of patients with chronic diseases, share of patients over 65 years old or under 15 years old and the share of patients with free complementary health insurance (CMU-C) (available upon request).
References
Ono, T., Schoenstein, M., Buchan, J.: Geographic imbalances in doctor supply and policy responses (2014). https://doi.org/10.1787/5jz5sq5ls1wl-en
Frélaut, M.: Les déserts médicaux. Regards 53, 105–116 (2018)
Vergier, N., Chaput, H.: Déserts médicaux : comment les définir ? Comment les mesurer ? Les dossiers de la Drees n°17. Mai (2017)
Groenewegen, P., Heinemann, S., Greß, S., Schäfer, W.: Primary care practice composition in 34 countries. Health Policy 119, 1576–1583 (2015). https://doi.org/10.1016/j.healthpol.2015.08.005
Mousquès, J.: Le regroupement des professionnels de santé de premiers recours : quelles perspectives économiques en termes de performance ? Revue francaise des affaires sociales. pp. 253–275 (2011)
Newhouse, J.P.: The economics of group practice. J. Hum. Resour. 8, 37–56 (1973). https://doi.org/10.2307/144634
Propper, C., Nicholson, A.: The organizational form of firms: why do physicians form groups? In Handbook in Health Economics. pp. 911–916 (2012)
Jesmin, S., Thind, A., Sarma, S.: Does team-based primary health care improve patients’ perception of outcomes? Evidence from the 2007–08 Canadian Survey of Experiences with Primary Health. Health Policy 105, 71–83 (2012). https://doi.org/10.1016/j.healthpol.2012.01.008
Mickan, S.M.: Evaluating the effectiveness of health care teams. Aust. Health Rev. 29, 211–217 (2005)
Strumpf, E., Ammi, M., Diop, M., Fiset-Laniel, J., Tousignant, P.: The impact of team-based primary care on health care services utilization and costs: Quebec’s family medicine groups. J. Health Econ. 55, 76–94 (2017). https://doi.org/10.1016/j.jhealeco.2017.06.009
Chevillard, G., Mousquès, J., Lucas-Gabrielli, V., Rican, S.: Has the diffusion of primary care teams in France improved attraction and retention of general practitioners in rural areas? Health Policy. 123, 508–515 (2019). https://doi.org/10.1016/j.healthpol.2019.03.002
Holte, J.H., Kjaer, T., Abelsen, B., Olsen, J.A.: The impact of pecuniary and non-pecuniary incentives for attracting young doctors to rural general practice. Soc. Sci. Med. 128, 1–9 (2015). https://doi.org/10.1016/j.socscimed.2014.12.022
Ammi, M., Diop, M., Strumpf, E.: Explaining primary care physicians’ decision to quit patient-centered medical homes: evidence from Quebec, Canada. Health Serv. Res. 54, 367–378 (2019). https://doi.org/10.1111/1475-6773.13120
Heam, J.C., Mikou, M., Ferreti, C., et al.: Les dépenses de santé en 2018 : Résultats des comptes de la santé. Edition 2018. Panoramas de la DREES (2019)
Dumontet, M., Buchmueller, T., Dourgnon, P., Jusot, F., Wittwer, J.: Gatekeeping and the utilization of physician services in France: evidence on the Médecin traitant reform. Health Policy 121, 675–682 (2017). https://doi.org/10.1016/j.healthpol.2017.04.006
Mousquès, J., Cartier, T., Chevillard, G., Couralet, P.-E., Daniel, F., Lucas-Gabrielli, V., Bourgueil, Y., Affrite, A.: L’évaluation de la performance des maisons, pôles et centres de santé dans le cadre des Expérimentations des nouveaux modes de rémunération (ENMR) sur la période 2009-2012. Rapport Irdes. (2014)
Bourgeois, I., Fournier, C.: Contractualiser avec l’Assurance maladie : un chantier parmi d’autres pour les équipes des maisons de santé pluriprofessionnelles. Rev. Fr. Aff. Soc. 1, 167–193 (2020)
Bont, A., Exel, J., Coretti, S., Ökem, Z., Janssen, M., Hope, K.L., Ludwicki, T., Zander-Jentsch, B., Zvonickova, M., Bond, C., Wallenburg, I.: Reconfiguring health workforce: a case-based comparative study explaining the increasingly diverse professional roles in Europe. BMC Health Serv. Res. 16, 637 (2016). https://doi.org/10.1186/s12913-016-1898-0
Grumbach, K., Bodenheimer, T.: Can health care teams improve primary care practice? JAMA 291, 1246–1251 (2004). https://doi.org/10.1001/jama.291.10.1246
Schuetz, B., Mann, E., Everett, W.: Educating health professionals collaboratively for team-based primary care. Health Aff. 29, 1476–1480 (2010). https://doi.org/10.1377/hlthaff.2010.0052
Defelice, L.C., Bradford, W.D.: Relative inefficiencies in production between solo and group practice physicians. Health Econ. 6, 455–465 (1997)
Kimbell, L.J., Lorant, J.H.: Physician productivity and returns to scale. Health Serv. Res. 12, 367–379 (1977)
Reinhardt, U.: A production function for physician services. Rev. Econ. Stat. 54, 55–66 (1972). https://doi.org/10.2307/1927495
Rosenman, R., Friesner, D.: Scope and scale inefficiencies in physician practices. Health Econ. 13, 1091–1116 (2004). https://doi.org/10.1002/hec.882
Milliken, O., Devlin, R.A., Barham, V., Hogg, W., Dahrouge, S., Russell, G.: Comparative efficiency assessment of primary care service delivery models using data envelopment analysis. Can. Public Policy 37, 85–109 (2011)
Sarma, S., Devlin, R.A., Hogg, W.: Physician’s production of primary care in Ontario, Canada. Health Econ. 19, 14–30 (2010). https://doi.org/10.1002/hec.1447
Adorian, D., Silverberg, D.S., Tomer, D., Wamosher, Z.: Group discussions with the health care team–a method of improving care of hypertension in general practice. J. Hum. Hypertens. 4, 265–268 (1990)
Bodenheimer, T., Wagner, E.H., Grumbach, K.: Improving primary care for patients with chronic illness. JAMA 288, 1775–1779 (2002). https://doi.org/10.1001/jama.288.14.1775
Callahan, C.M., Boustani, M.A., Unverzagt, F.W., Austrom, M.G., Damush, T.M., Perkins, A.J., Fultz, B.A., Hui, S.L., Counsell, S.R., Hendrie, H.C.: Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA 295, 2148–2157 (2006). https://doi.org/10.1001/jama.295.18.2148
Renders, C., Valk, G., Griffin, S., Wagner, E., van Eijk, J., Assendelft, W.: Interventions to improve the management of diabetes in primary care, outpatient, and community settings: a systematic review. Diabetes Care 24, 1821–1833 (2001). https://doi.org/10.2337/diacare.24.10.1821
Rosenthal, M.B., Sinaiko, A.D., Eastman, D., Chapman, B., Partridge, G.: Impact of the Rochester Medical Home Initiative on primary care practices, quality, utilization, and costs. Med. Care 53, 967–973 (2015). https://doi.org/10.1097/MLR.0000000000000424
Rebitzer, J.B., Votruba, M.E.: Organizational economics and physician practices. In: Culyer, A.J. (ed.) Encyclopedia of health economics, pp. 414–424. Elsevier, San Diego (2014)
Encinosa, W.E., Gaynor, M., Rebitzer, J.B.: The sociology of groups and the economics of incentives: Theory and evidence on compensation systems. J. Econ. Behav. Organ. 62, 187–214 (2007). https://doi.org/10.1016/j.jebo.2006.01.001
Gaynor, M., Gertler, P.: Moral hazard and risk spreading in partnerships. RAND J. Econ. 26, 591–613 (1995). https://doi.org/10.2307/2556008
Fournier, C.: Travailler en équipe en s’ajustant aux politiques : un double défi dans la durée pour les professionnels des maisons de santé pluriprofessionnelles. Journal de gestion et d’economie de la sante. 37(1), 72–91 (2019)
Harris, M.F., Advocat, J., Crabtree, B.F., Levesque, J.-F., Miller, W.L., Gunn, J.M., Hogg, W., Scott, C.M., Chase, S.M., Halma, L., Russell, G.M.: Interprofessional teamwork innovations for primary health care practices and practitioners: evidence from a comparison of reform in three countries. J. Multidiscip. Healthc. 9, 35–46 (2016). https://doi.org/10.2147/JMDH.S97371
Schadewaldt, V., McInnes, E., Hiller, J.E., Gardner, A.: Views and experiences of nurse practitioners and medical practitioners with collaborative practice in primary health care—an integrative review. BMC Fam. Pract. 14, 132 (2013). https://doi.org/10.1186/1471-2296-14-132
Gaynor, M., Pauly, M.V.: Compensation and productive efficiency in partnerships: evidence from medical groups practice. J. Political Econ. 98, 544–573 (1990)
Kantarevic, J., Kralj, B., Weinkauf, D.: Enhanced fee-for-service model and physician productivity: evidence from Family Health Groups in Ontario. J. Health Econ. 30, 99–111 (2011). https://doi.org/10.1016/j.jhealeco.2010.10.005
McGuire, T.G.: Physician agency and payment for primary medical care. In: The Oxford Handbook of Health Economics (2011). https://doi.org/10.1093/oxfordhb/9780199238828.013.002
Bolduc, D., Fortin, B., Fournier, M.-A.: The effect of incentive policies on the practice location of doctors: a multinomial probit analysis. J. Labor Econ. 14, 703–732 (1996)
Delattre, E., Samson, A.L.: Stratégies de localisation des médecins généralistes français: mécanismes économiques ou hédonistes ? Econ. Stat. 455, 115–142 (2012). https://doi.org/10.3406/estat.2012.10020
Hurley, J.: Physicians’ choices of specialty, location, and mode: a reexamination within an interdependent decision framework. J. Hum. Resour. 26, 47–71 (1991)
Becker, G.S., Murphy, K.M.: The division of labor, coordination costs, and knowledge. Q. J. Econ. 107, 1137–1160 (1992). https://doi.org/10.2307/2118383
Meltzer, D.O., Chung, J.W.: Coordination, Switching Costs and the Division of Labor in General Medicine: An Economic Explanation for the Emergence of Hospitalists in the United States. National Bureau of Economic Research, Cambridge (2010)
Gaynor, M.: Competition within the firm: theory plus some evidence from medical group practice. RAND J. Econ. 20, 59–76 (1989). https://doi.org/10.2307/2555651
Grumbach, K., Coffman, J.: Physicians and nonphysician clinicians: complements or competitors? JAMA 280, 825–826 (1998). https://doi.org/10.1001/jama.280.9.825
Chevillard, G., Mousquès, J.: Accessibilité aux soins et attractivité territoriale : proposition d’une typologie des territoires de vie français. Cybergeo : European Journal of Geography. (2018). https://doi.org/10.4000/cybergeo.29737
Mikol, F., Franc, C.: Gender differences in the incomes of self-employed french physicians: the role of family structure. Health Policy. (2019). https://doi.org/10.1016/j.healthpol.2019.05.002
Iacus, S.M., King, G., Porro, G.: Multivariate matching methods that are monotonic imbalance bounding. J. Am. Stat. Assoc. 106, 345–361 (2011). https://doi.org/10.1198/jasa.2011.tm09599
Ho, D.E., Imai, K., King, G., Stuart, E.A.: Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Political Anal. 15, 199–236 (2007). https://doi.org/10.1093/pan/mpl013
Chabé-Ferret, S.: Should we combine difference in differences with conditioning on pre-treatment outcomes? Toulouse school of economics (TSE) (2017)
Lindner, S., McConnell, K.J.: Difference-in-differences and matching on outcomes: a tale of two unobservables. Health Serv. Outcomes Res. Method. 19, 127–144 (2019). https://doi.org/10.1007/s10742-018-0189-0
King, G., Nielsen, R.: Why propensity scores should not be used for matching. Political Anal. 27, 435–454 (2019). https://doi.org/10.1017/pan.2019.11
Iacus, S.M., King, G., Porro, G.: A theory of statistical inference for matching methods in causal research. Political Anal. 27, 46–68 (2019)
Acknowledgements
We thank the Drees (Direction de la recherche, des études, de l’évaluation et des statistiques) for letting us access to their facilities and to the CNAMTS-DGFiP database.
Funding
Funding for the French survey. Research grant from NHI for the evaluation program pilot by IRDES and CESP.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Details of CEM criteria
CEM allows us to control imbalances bound between the treated and control groups, while the large size of the non-MGP sample allows us to use exact matching without discarding too many treated GPs. The continuous variable age was broken down into nine categories from 27 to 30-year-old GPs and then by 5-year increments from 30 to 60-year-old GPs (the oldest GP in the study sample was 59). Furthermore, to better control for GPs’ career profiles we also matched on whether GPs had practiced in private practice for more or less than 5 years. Indeed, depending on the year in which they set up in private practice (e.g., after practicing in a hospital), GPs could be exposed to early carrier ramp-up at different ages. With regard to the number of children, we included the GPs with strictly more than 3 in the same category. Finally, we defined a regular additional salaried activity as one that generated more than €4000 per year, which amounted to 5% of the average total income in 2008.
To achieve a balanced sample, we opted for weighting the standard GPs in each subclass, so that their distribution over the subclass corresponded to that of the GPs in MPCGs: all of whom had a weight equal to 1, while the weights of control GPs were normalized to sum up their actual number. More precisely, the CEM and consecutive weighting were computed with the MatchIt package in R, so that the control GPs’ weights within each exact matching’s subclass is (the number of treated within the subclass/the number of controls within the subclass) * (Overall number of control/Overall number of treated). In contrast to selecting a given ratio of control GPs within each subclass, as in m-to-1 matching approach, it enabled us to keep as much information as possible on the control group and to estimate the average treatment effect on the treated (ATT), provided that the same weights were used in the regression analysis.
Robustness analyses
The remainder of the “Appendix” presents selected tables from our robustness analysis (further results from robustness checks are available upon request).
The last two tables (Tables 6 and 7) present the replication of our parametric analysis when the control group was identified through PSM, and additional matching criteria were introduced. The following details more precisely the procedure which we used. The propensity score was estimated in 2008 (pre-reform period) using a logistic model that predicted the likelihood of joining an accredited MPCGs in function of: the socio-demographic and territorial covariates used in our original CEM, case mix details (share of patients according to their age, patients with free complementary health insurance, and patients with a chronic disease), as well as the number of patients seen, the number of medical services, the GP’s gross revenues, self-employed and salaried income, and the share of home visits and procedures in GPs’ gross revenues. The matching uses nearest-neighbor’s criterion to select 3 control GPs for each GP in a MPCG, and balances territorial socio-demographic characteristics, activity (visits and patients), and incomes. After the PSM, there were no significative differences in the pre-reform period in 2008 with regard to all the criteria included in the logistic model (descriptive statistics of the balanced sample are available on request).
Rights and permissions
About this article
Cite this article
Cassou, M., Mousquès, J. & Franc, C. General practitioners’ income and activity: the impact of multi-professional group practice in France. Eur J Health Econ 21, 1295–1315 (2020). https://doi.org/10.1007/s10198-020-01226-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-020-01226-4