Abstract
Background
Research has shown that a small proportion of patients account for the majority of health care spending. The objective of this analysis was to determine the amount and proportion of preventable acute care spending among high-cost patients.
Methods
We examined a population-based sample of all adult high-cost patients using linked administrative health care data housed at ICES in Toronto, Ontario. High-cost patients were defined as those in and above the 90th percentile of the cost distribution. Preventable acute care (emergency department visits and hospitalisations) was defined using validated algorithms. We estimated costs of preventable and non-preventable acute care for high- and non-high-cost patients by category of visit/condition. We replicated our analysis for persistent high-cost patients and high-cost patients under 65 years and those 65 years and older.
Results
We found that 10% of all acute care spending among high-cost patients was considered preventable; this figure was higher for non-high-cost patients (25%). The proportion of preventable acute care spending was higher for persistent high-cost patients (14%) and those 65 years and older (12%). Among ED visits, the largest portion of preventable care spending was for primary care treatable conditions; for hospitalisations, the highest proportions of preventable care spending were for COPD, bacterial pneumonia and urinary tract infections.
Conclusions
Although high-cost patients account for a substantial proportion of health care costs, there seems to be limited scope to prevent acute care spending among this patient population. Nonetheless, care coordination and improved access to primary care, and disease prevention may prevent some acute care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Health care costs are rising. As such, policy makers are seeking ways to bend the cost curve [1, 2]. Previous work has shown that a small proportion of patients account for the majority of health care spending [1, 2]. Thus, focusing on high-cost patients is likely to yield the most impact on health system costs. Many jurisdictions have implemented strategies, such as high-risk care management, to reduce costs and improve quality; however, it is not clear which costs can be reduced, especially among patients that require costly care. One potential way to decrease costs, without sacrificing care, may be to target preventable (i.e., potentially unnecessary) acute care among high-cost patients. Previous research has shown that emergency department (ED) visits and inpatient hospitalisations make up more than half of all costs among the high-cost population [1]. Furthermore, some studies have shown that a substantial proportion of ED visits [3, 4] and hospitalisations may be preventable [5,6,7,8].
While research has analysed preventable care among the general population or disease-specific sub-populations, little work has been done on high-cost patients. Most of the existing work has been done in the United States (US). Joynt et al. [9] examined preventable and non-preventable acute care among high-cost Medicare patients using validated algorithms [9]. They found only a small percentage (9.6%) of costs was due to preventable acute care. In particular, the largest drivers of acute care spending were orthopaedic procedures and ischemic heart disease, both of which are considered non-preventable. Graven et al. [10] replicated this analysis using the State of Oregon’s All Payer All Claims database and Medicaid data from the Oregon Health Authority, which enabled them an almost comprehensive analysis of all patients across a single region for multiple payers [10]. The authors found that preventable acute care spending for high-cost patients accounted for less than 6% of total spending. In Canada, Ronksley et al. [11] examined preventable acute care spending among high-cost patients hospitalised at the Ottawa Hospital [11]. The authors used an ambulatory care sensitive conditions algorithm to determine preventable acute care. They found that, among a high-cost inpatient population, most costs were due to a single, non-preventable, acute care episode and only 6% of costs were due to an ambulatory care sensitive hospital encounter. The main limitation of these studies is that they examined subsets of patient groups, which limits the generalisability of findings to the entire population. Given the interest in identifying strategies to reduce health care costs incurred by high-cost patients, this study seeks to fill this gap by determining the amount and proportion of preventable acute care spending for the entire adult high-cost population in Ontario. In addition, it explores whether preventable acute care spending varies by age groups.
Methods
Study design and setting
We undertook a population-based, cross-sectional study of all adult high-cost patients in Ontario to determine potentially preventable acute care.
Data
We used administrative health care data available through ICES in Toronto, Ontario, which includes individual-level linkable and longitudinal data on most publicly funded health care services for all legal residents of Ontario, Canada’s most populous province. Given universal health care coverage for all insured services, defined as hospital-based care and physician services in the Canada Health Act, virtually all legal residents of Ontario are captured in the data. Data on institution-based care are captured in the Discharge Abstract Database (acute hospitalisations), the Ontario Mental Health Reporting System (psychiatric hospitalisations), the Continuing Care Reporting System (continuing and long-term care), and the National Rehabilitation Reporting System (rehabilitation); data on ambulatory care are recorded in the National Ambulatory Care Reporting System. The Ontario Health Insurance Plan claims database captures data on physician visits, including fee-for-service visits and shadow-billed services, as well as laboratory and diagnostic claims. The Ontario Drug Benefit Program database includes information on all outpatient prescriptions dispensed to individuals covered under the public provincial drug plan (i.e., individuals aged 65 years and older and those under the age of 65 years who are eligible for social assistance). The Home Care Database records all unique visits provided by home care professionals. The ICES data repository also includes other databases, which provide useful information on individuals who contact the health care system. The Registered Persons Database, a population-based registry, provides basic demographic data, such as age and sex, on all legal residents of Ontario and their eligibility for public health care insurance. The Immigration, Refugees and Citizenship Canada database provides information on all legal immigrants and refugees in Canada. The Census data, obtained through Statistics Canada, contain information on neighbourhood-level characteristics, such as median income and degree of rurality. All databases were linked using unique encoded identifiers and analysed at ICES, in compliance with Ontario privacy legislation. A full description of the databases can be found in Table A1 in the Appendix.
Patient cohort
Using the Registered Persons Database, we selected all adult patients (18 years and older) eligible for public health care insurance and residing in Ontario in calendar year 2013. We excluded all patients who died before January 1 2013 or were born after December 31 2013, as well as those who did not contact the health care system in 2013. In addition, we excluded all patients who died in 2013, in line with previous research [9] as assessing the preventability of end-of-life care costs was beyond the scope of this analysis.
Identifying high-cost patients
We used a cost estimation algorithm, available at ICES, to estimate health care costs incurred by patients and borne by the public third-party payer (i.e., Ontario Ministry of Health and Long-term Care) [12] in 2013. This algorithm estimates costs of inpatient hospitalisations (acute and psychiatric), other institution-based care (complex continuing care, long-term care, inpatient rehabilitation), emergency department (ED) visits and other ambulatory care, outpatient clinic visits, physician visits and outpatient care, outpatient prescription drugs, and home care. The costs captured by the algorithm account for roughly 92% of all government paid health care [13].
High-cost patients were defined as those in and above the 90th percentile of the cost distribution (i.e., top decile), in line with previous work [2]. All other patients were defined as non-high-cost patients. We also examined persistent high-cost users, who were defined as all patients who remained in and above the 90th percentile of the cost distribution from 2013 to 2015.
Identifying preventable acute care
Preventable acute care was defined as ED visits and hospitalisations. To identify preventable ED visits, we used an updated version of a validated algorithm created by Billings et al. [14] and used in prior research, [3, 9, 15] and expanded by Johnston et al. [16]. The original algorithm uses specified diagnosis codes to create the following four categories: non-emergent; emergent but primary care treatable; emergent, ED care needed, but preventable; and emergent, ED care needed, and not preventable. Based on these classifications, the authors compiled a set of probabilistic weights that were applied to ED discharge data using primary discharge ICD-10 diagnosis codes to determine the percentage of ED use attributable to each of the four categories [17]. The updated version of the algorithm, developed by Johnston et al. [16], includes additional ED visit categories: alcohol use, drug use, injury and mental health. ED visits with diagnosis codes that were not mapped to any of the eight categories were assigned to the “unclassified” category. Despite some criticism around its use as a potential triage tool or mechanism to determine whether an ED visit is appropriate for reimbursement by managed care plans, [18] the algorithm has been widely used in the US. In line with previous work, we defined non-emergent, emergent/primary care treatable, and emergent/ED care needed/preventable or avoidable visits as preventable ED visits, and ED care needed, not preventable, alcohol use, drug use, injury and mental health as non-preventable ED visits [9].
We used the Prevention Quality Indicators developed by the Agency for Healthcare Research and Quality, and used elsewhere [19,20,21], to identify potentially preventable hospitalisations [22]. These indicators define potentially preventable hospitalisations as those for which good outpatient care can likely prevent the need for hospitalisation. These include acute conditions, such as bacterial pneumonia and urinary tract infections, as well as chronic conditions, such as COPD and diabetes. We also used the respective Prevention Quality Indicators for common non-preventable clinical diagnosis groups to identify non-preventable hospitalisations. (See Table A2 in the Appendix for a list of diagnoses and codes for preventable and non-preventable hospitalisations.). We adapted the list of diagnosis codes (and procedure codes, where applicable) to the Ontario data. In particular, given that only the first 3 or 4 digits of the ICD-10 hospitalisation diagnosis codes were available in our data, we had to aggregate some diagnostic categories, which, in some cases, may have limited how we classified some hospitalisations (e.g. diabetes-related hospitalisations).
Analysis
We examined two patient groups: high- and non-high-cost patients. Patient groups were characterised and compared in terms of socio-demographic characteristics (sex, age, migrant status, neighbourhood income quintile, and urban/rural residence), and clinical characteristics (chronic conditions, frailty and long-term care residence). We used the existing ICES-derived cohorts/registries to ascertain chronic conditions among patients [23,24,25,26,27,28,29,30,31,32,33,34] and the Johns Hopkins Adjusted Clinical Groups Software [35] to determine patient frailty. Residence in a long-term care facility was determined through the Continuing Care Reporting System. Patient characteristics between high-cost and non-high-cost individuals were compared through the use of a Chi square test for differences. We estimated total costs of preventable and non-preventable acute care by category of visit (for ED visits) and condition (for inpatient hospitalisations) for both patient groups. We repeated all analyses for persistent high-cost patients. All costs were reported in 2016 constant Canadian dollars using Statistics Canada Consumer Price Index for health care [36].
Sensitivity analysis
Our analysis focused on all adult high-cost patients. However, previous work in the US examined Medicare high-cost patients [9]. Results are likely to differ by sample composition; therefore, we re-ran all analyses on high-cost patients under the age of 65 and those 65 years and older to compare our findings with those from previous research.
All analyses were performed using SAS Enterprise Guide 7.1. The study was approved by the research ethics board of Sunnybrook Health Sciences Centre in Toronto, Ontario.
Results
Patient characteristics
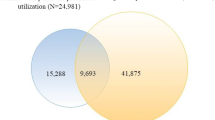
In 2013, 9,941,310 individuals contacted the Ontario health care system, excluding those who died during that year (n = 90,555). Among those, 929,726 were high-cost patients. These patients were older (mean age 62 versus 46 years), more often female (58% versus 52%) and non-migrant (89% versus 81%), slightly more represented in the lower neighbourhood income quintile (22% versus 18%) and slightly more likely to live in urban areas (13% versus 11%) compared to non-high-cost patients (Table 1). High-cost patients also had a higher proportion of chronic conditions, such as dementia, congestive heart failure, HIV, psychosis and cancer, a higher degree of frailty, and were more likely to be living in long-term care homes (Table 1).
Costs of preventable and non-preventable acute care
ED visits
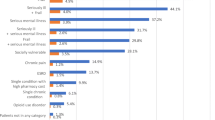
Among the high-cost cohort, 32.0% of ED visits were deemed preventable according to the algorithm. These visits were associated with 29.5% of ED costs (Table 2). Proportions were slightly higher for non-high-cost patients, with 37.7% of visits and 34.6% of costs considered preventable. The categories with the highest proportion (excluding other/unclassified) were ED care needed, not preventable (17.9%), injury (13.0%) and emergent, primary care treatable (12.5%) for high-cost patients, and injury (19.3%), not emergent (15.3%) and emergent, primary care treatable (15.2%) for non-high-cost patients.
Hospitalisations
Within the high-cost group, 9.0% of hospital admissions were attributable to preventable causes, which corresponded to 8.5% of spending (Table 3). For non-high-cost patients, 3.4% of all hospital admissions were preventable while 3.9% of spending was classified as preventable. The preventable hospitalisations with the highest proportions of spending among high-cost patients included COPD (2.6%), bacterial pneumonia (1.8%) and urinary tract infections (1.5%) (and diabetes if all related hospitalisations were combined); this was also the case for non-high-cost patients (albeit different rankings). The non-preventable hospitalisations with the highest proportions of spending were orthopaedic conditions (7.3%), ischemic heart disease (7.3%) and cancer and chemotherapy (7.2%) for high-cost patients, and GI infections and disorders (2.9%), orthopaedic conditions (1.6%), and syncope and dizziness (1.0%) for non-high-cost patients.
Combining both ED and inpatient settings, 10.4% of high-cost patients’ costs were considered potentially preventable while the corresponding value was 24.8% for non-high-cost patients.
Persistent high-cost cohort
We also examined a cohort of patients who persisted in the high-cost state from 2013 to 2015. Of the 929,726 high-cost patients, 53.7% (n = 498,906) remained in the high-cost category in 2014 while 37.0% (n = 343,337) remained in the high-cost category in both 2014 and 2015. Patients in the persistent high-cost cohort (n = 343,337) were on average older than other high-cost patients (68 versus 58; p value < .0001) and more likely to live in low-income neighbourhoods (26% versus 21%; p value < .0001) but similar on all other socio-demographic characteristics. Not surprisingly persistent high-cost patients had a higher proportion of chronic conditions (in particular HIV) than other high-cost patients (see Table A3 in the Appendix). Among the persistent group, 33.1% of ED visits were considered preventable, which corresponded to 31.3% of total ED costs (Table 4). With regard to hospitalisations, 14.4% were deemed preventable, which corresponded to 12.0% of total hospitalisation costs (Table 4). (See Tables A4 and A5 in the Appendix for a more detailed breakdown.). As a whole, 13.8% of all acute care spending was considered preventable.
Sensitivity analysis
We re-ran all analyses on high-cost patients under the age of 65 and those 65 years and older. We found that older high-cost patients were more likely to be Canadian born and less likely to live in low-income neighbourhoods compared to younger high-cost patients. In addition, older high-cost patients had a higher proportion of dementia and congestive heart failure but a lower proportion of HIV, chronic kidney disease and psychosis. Older high-cost patients also had a higher proportion of preventable acute care costs than younger high-cost patients for both ED visits (31.4% versus 27.6%) and hospitalisations (10.4% versus 6.3%). (See Tables A6–A8 and A9–A11 in the Appendix for patient characteristics, and preventable and non-preventable acute care spending for high-cost patients 65 years and older, and those under the age of 65 years, respectively.) Overall, 12.1% and 8.3% of acute care spending was classified as preventable for patients 65 years and older and patients under the age of 65 years, respectively.
Discussion
We examined preventable acute care spending among a population-based sample of all adult high-cost patients in Ontario. We found that 29.5% of ED visit costs and 8.5% of hospitalisations costs could potentially be avoided. Overall, 10.4% of high-cost patients’ acute care costs were considered potentially preventable. This percentage was slightly higher for persistent high-cost patients (13.8%) and those 65 and older (12.1%). The largest drivers of acute care costs were hospitalisations for catastrophic illnesses, such as ischemic heart disease and stroke, and orthopaedic conditions and cancer and chemotherapy, all of which were classified as non-preventable. Among preventable acute care, the largest drivers of spending were hospitalisations for COPD, bacterial pneumonia and urinary tract infections.
Our results are largely in line with previous work but differ in some regards. Using data from a large Canadian hospital in Ottawa, Ronksley et al. [11] examined preventable acute care spending among hospitalised high-cost patients using an ambulatory care sensitive conditions algorithm (which included hypertension, diabetes, angina, asthma, COPD, epilepsy, and heart failure/pulmonary edema) [11]. They found that most costs were due to a single, non-preventable, acute care episode and only 6% of costs were due to preventable care. The difference between our results is likely due to the use of different hospitalisation algorithms, given that the Agency for Healthcare Research Quality Prevention Quality Indicators include more conditions than those in the ambulatory care sensitive conditions algorithm, but also the type of population examined (hospitalised adults in one hospital versus entire adult population). Nonetheless, they also found that COPD was most common preventable hospitalisation. Joynt et al. [9] examined preventable and non-preventable acute care among high-cost Medicare patients in the US. The authors found that a small percentage of costs (9.6%) were due to preventable acute care, which is close to our value (10.4%) [9]. Graven et al. [10] replicated the Joynt et al. analysis using Oregon’s All Payer All Claims database and Medicaid data from Oregon Health Authority [10]. They found that preventable health care spending for high-cost patients accounted for less than 6% of total spending. We were also interested in replicating the Joynt et al. [9] study to understand whether their findings would differ for the full adult population. While we found that 29.5% ED visit costs were due to potentially preventable care, this figure was 41.0% for US Medicare population. This is likely due to different population makeup but also the large proportion of unclassified ED visits in our data. We found higher proportions of ED visit costs due to alcohol, drugs and mental health. Although ED visits for substance use and mental health were not broken down into preventable or non-preventable care, it is possible that some care could have been avoided with appropriate outpatient and community care. With regard to preventable hospitalisation costs, we found a slightly lower proportion (8.5%) than in the US Medicare high-cost population (9.6%). In particular, we found a higher proportion of hospitalisation costs for COPD (2.6%) and urinary tract infections (1.5%) (but similar proportion for bacterial pneumonia − 1.8% versus 1.9%), while previous work in the US found higher proportions for congestive heart failure (3.0% versus 0.1%), followed by bacterial pneumonia (1.9%) and COPD (1.7%). Again, our results differed from the US for the proportion of preventable ED visit spending among persistent high-cost patients (31.3% versus 43.3%) but were closer in value for the proportion of preventable hospitalisation spending (12.0% versus 13.5%).
Our results suggest that the percentage of preventable acute care costs varies with age. For example, the proportions of preventable alcohol-, drug- and mental health-related ED visit spending were far greater among younger high-cost patients while older patients had higher proportions of hospitalisation spending for COPD, bacterial pneumonia and urinary tract infections. Overall, we found that older high-cost patients had a higher percentage of preventable acute care than younger ones (12.1% versus 8.3%) likely in part due to greater comorbidity. Thus, for older patients, there may be more scope to lower acute care costs through better care coordination programs and improved access to primary care or disease prevention (although not without substantial investments and lead time for changes to occur). Previous research has shown that Bridges to Care, an ED-initiated, multidisciplinary, community-based program, reduced acute care use and increased primary care visits among frequent emergency care users [37]. Moreover, there may be advantages in targeting lower-income high-cost patients [6, 38]. For instance, this could potentially be achieved through improved access to care for low-income individuals and/or targeted prevention/educational interventions to ensure these patients do not delay seeking care until their condition is too advanced. Nonetheless, while disease management may provide some cost savings to the system, previous research suggests that substantial reductions in preventable acute care are not likely to have a large impact on health care spending, despite these visits being expensive at the aggregate level [9]. Our findings are in line with previous research. Thus, other strategies may be required, such as finding ways to make hospital care more efficient and, in turn, inpatient stays less costly [9]. This could potentially be achieved by a greater focus on preventing the development of multi-morbidity in older populations.
Our study adds to prior literature on this topic. We provide estimates of preventable acute care spending for the entire adult high-cost population, thus addressing a data limitation that is common when using US data. As such, this analysis will be relevant to other jurisdictions with similar health care systems, such as the United Kingdom and other European countries. Furthermore, we examine how preventable acute care spending varies by age groups. We provide an in-depth characterisation of the high-cost population and follow them over time, which enabled us to examine preventable care among patients who persist in the high-cost state. We made use of rich administrative health care data and were able to account for all ED visit and inpatient hospitalisation costs given the presence of a (sole) third-party public payer for acute care in Ontario.
Limitations
We did not examine patients under the age of 18, as some health services for this population are funded by ministries other than the Ontario Ministry of Health and Long-term Care. We did not examine preventability of end-of-life care costs, as this what outside the scope of our analysis. We used previously defined algorithms developed in the US to identify preventable acute care, which are not without limitations [10]. In particular, when applied to the Ontario data, the ED algorithm was not able to classify a large proportion of visits while the Prevention Quality Indicators required more than 4 ICD-10 coding digits for a perfect match. This has likely affected the degree to which we were able to ascertain preventable acute care costs given the large proportion of non-classified events (e.g. for individuals 65 years and older, we found that only 31.4% of ED costs were preventable, while Joynt et al. [9] found that 41.0% of ED costs were preventable for the US Medicare population). Furthermore, while the algorithm was able to classify ED visits into alcohol use, drug use and mental health visits, it did not explore potential avoidable ED visits within each of these categories. This was also the case for the hospitalisation algorithm, which focused on physical health only.
Conclusion
Research suggests that some acute care spending can be preventable. In a time of rising health care costs, focusing on high-cost patients is likely to yield cost-savings. We found there was limited scope to prevent acute care spending among high-cost patients (though this varied by whether high-cost patients persist in that state or whether they are older). Nonetheless, better access to primary care as well as disease prevention may help prevent some acute care. While previous work has examined preventable acute medical care among patients with mental illness or addiction [39, 40], no studies have specifically focused on preventable acute psychiatric care. Future work should explore preventable acute psychiatric care, such as ED visits for self-harm or psychiatric hospitalisations for depression, for example.
References
Riley, G.F.: Long-term trends in the concentration of Medicare spending. Health Aff. (Millwood) 26(3), 808–816 (2007)
de Oliveira, C., Cheng, J., Vigod, S., Rehm, J., Kurdyak, P.: Patients with high mental health costs incur over 30 percent more costs than other high cost patients. Health Aff. (Millwood) 35(1), 36–43 (2016)
Smulowitz, P.B., Lipton, R., Wharam, J.F., et al.: Emergency department utilization after the implementation of Massachusetts health reform. Ann. Emerg. Med. 58(3), 225–234 (2011)
Ballard, D.W., Price, M., Fung, V., et al.: Validation of an algorithm for categorizing the severity of hospital emergency department visits. Med. Care 48(1), 58–63 (2010)
Niefeld, M.R., Braunstein, J.B., Wu, A.W., Saudek, C.D., Weller, W.E., Anderson, G.F.: Preventable hospitalization among elderly Medicare beneficiaries with type 2 diabetes. Diabetes Care 26(5), 1344–1349 (2003)
Billings, J., Anderson, G.M., Newman, L.S.: Recent findings on preventable hospitalizations. Health Aff. (Millwood) 15(3), 239–249 (1996)
Oster, A., Bindman, A.B.: Emergency department visits for ambulatory care sensitive conditions: insights into preventable hospitalizations. Med. Care 41(2), 198–207 (2003)
Braunstein, J.B., Anderson, G.F., Gerstenblith, G., et al.: Noncardiac comorbidity increases preventable hospitalizations and mortality among Medicare beneficiaries with chronic heart failure. J. Am. Coll. Cardiol. 42(7), 1226–1233 (2003)
Joynt, K.E., Gawande, A.A., Orav, E.J., Jha, A.K.: Contribution of preventable acute care spending to total spending for high-cost Medicare patients. JAMA 309(24), 2572–2578 (2013)
Graven, P.F., Meath, T.H.A., Mendelson, A., Chan, B.K.S., Dorr, D.A., McConnell, K.J.: Preventable acute care spending for high-cost patients across payer types. J. Health Care Financ. 42(3), 1–22 (2016)
Ronksley, P.E., Kobewka, D.M., McKay, J.A., et al.: Clinical characteristics and preventable acute care spending among a high cost inpatient population. BMC Health Serv. Res. 16, 165 (2016)
Wodchis, W.P., Bushmeneva. K., Nikitovic, M., McKillop, I.: Guidelines on person-level costing using administrative databases in Ontario [Internet]. Health System Performance Research Network, Toronto. (Working paper vol. 1). http://www.hsprn.ca/uploads/files/Guidelines_on_PersonLevel_Costing_May_2013.pdf (2013). Accessed 10 Nov 2015
Wodchis, W.P., Austin, P.C., Henry, D.A.: A 3-year study of high-cost users of health care. CMAJ 188, 182–188 (2016)
Wagner, N.Y.U.:. NYU ED algorithm: background. https://wagner.nyu.edu/faculty/billings/nyued-background (2000). Accessed 09 Aug 2017
Wharam, J.F., Landon, B.E., Galbraith, A.A., Kleinman, K.P., Soumerai, S.B., Ross-Degnan, D.: Emergency department use and subsequent hospitalizations among members of a high-deductible health plan. JAMA 297(10), 1093–1102 (2007)
Johnston, K.J., Allen, L., Melanson, T.A., Pitts, S.R.: A “Patch” to the NYU emergency department visit algorithm. Health Serv. Res. 52(4), 1264–1276 (2017)
Billings, J., Parikh, N., Mijanovich, T.: Emergency department use: the New York Story. Issue Brief (Commonw Fund) 434, 1–12 (2000)
Lowe, R.A.: Updating the emergency department algorithm: one patch is not enough. Health Serv. Res. 52(4), 1257–1263 (2017)
Basu, J., Friedman, B., Burstin, H.: Primary care, HMO enrollment, and hospitalization for ambulatory care sensitive conditions: a new approach. Med. Care 40(12), 1260–1269 (2002)
Bindman, A.B., Grumbach, K., Osmond, D., et al.: Preventable hospitalizations and access to health care. JAMA 274(4), 305–311 (1995)
Jiang, H.J., Russo, C.A., Barrett, M.L.: Nationwide frequency and costs of potentially preventable hospitalizations. Agency for Healthcare Research & Quality, Rockville (2006). (HCUP Statistical Brief 72)
Agency for Healthcare Research and Quality. Prevention quality indicators overview. http://www.qualityindicators.ahrq.gov/modules/pqi_overview.aspx (2011). Accessed 10 Aug 2017
Antoniou, T., Zagorski, B., Loutfy, M.R., et al.: Validation of case-finding algorithms derived from administrative data for identifying adults living with human immunodeficiency virus infection. PLoS One 6(6), e21748 (2011)
Benchimol, E., Guttmann, A., Mack, D.R., et al.: Validation of international algorithms to identify adults with inflammatory bowel disease in health administrative data from Ontario, Canada. J. Clin. Epidemiol. 67(8), 887–896 (2014)
Gershon, A.S., Wang, C., Guan, J., et al.: Identifying patients with physician diagnosed asthma in health administrative databases. Can. Respir. J. 16(6), 183–188 (2009)
Gershon, A.S., Wang, C., Guan, J., et al.: Identifying individuals with physician diagnosed COPD in health administrative databases. COPD 6(5), 388–394 (2009)
Hux, J.E., Ivis, F., Flintoft, V., et al.: Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care 25(3), 512–516 (2002)
Jaakkimainen, R.L., Bronskill, S.E., Tu, K., et al.: Identification of physician-diagnosed Alzheimer’s disease and related dementias in population-based administrative data: a validation study using family physicians’ electronic medical records. J. Alzheimer’s Dis. 54(1), 337–349 (2016)
Paul, Kurdyak, Elizabeth, Lin, Diane, Green, Simone, Vigod: Validation of a population-based algorithm to detect chronic psychotic illness. Can. J. Psychiatry 60(8), 362–368 (2015)
Moist, L.M., Fenton, S., Kim, J.S., et al.: Canadian Organ Replacement Register (CORR): reflecting the past and embracing the future. Can. J. Kidney Health Dis. 1, 26 (2014)
Prodhan, S., King, M.J., De, P., Gilbert, J.: Health services data: the Ontario Cancer Registry (a unique, linked, and automated population-based registry). In: Sobolev, B., Levy, A., Goring, S. (eds.) Data and Measures in Health Services Research. Springer, Boston (2016)
Schultz, S.E., Rothwell, D.M., Chen, Z., et al.: Identifying cases of congestive heart failure from administrative data: a validation study using primary care patient records. Chronic Dis. Inj. Can. 33(3), 160–166 (2013)
Tu, K., Chen, Z., Lipscombe, L.L., Canadian Hypertension Education Program Outcomes Research Taskforce: Prevalence and incidence of hypertension from 1995 to 2005: a population-based study. CMAJ 178(11), 1429–1435 (2008)
Widdifield, J., Bernatsky, S., Paterson, J.M., Tu, K., Ng, R., Thorne, J.C., et al.: Accuracy of Canadian Health administrative databases in identifying patients with rheumatoid arthritis: a validation study using the medical records of rheumatologists. Arthritis Care Res. (Hoboken) 65(10), 1582–1589 (2013)
The Johns Hopkins University Bloomberg School of Public Health. The Johns Hopkins ACG Case-Mix System Version 7.0 Release Notes (Systems Documentation). In: Weiner, J.P. (ed.) Johns Hopkins University, Baltimore (2005)
The consumer price index. Statistics Canada, Ottawa (ON) (2016). Cat. no. 62-001-X
Capp, R., Misky, G.J., Lindrooth, R.C., Honigman, B., Logan, H., Hardy, R., Nguyen, D.Q., Wiler, J.L.: Coordination program reduced acute care use and increased primary care visits among frequent emergency care users. Health Aff. (Millwood) 36(10), 1705–1711 (2017)
Blustein, J., Hanson, K., Shea, S.: Preventable hospitalizations and socioeconomic status. Health Aff. (Millwood) 17(2), 177–189 (1998)
Medford-Davis, L.N., Shah, R., Kennedy, D., Becker, E.: The role of mental health disease in potentially preventable hospitalizations: findings from a large state. Med. Care 56(1), 31–38 (2018)
Hensel, J.M., Taylor, V.H., Fung, K., Yang, R., Vigod, S.N.: Acute care use for ambulatory care-sensitive conditions in high-cost users of medical care with mental illness and addictions. Can. J. Psychiatry 63, 816 (2018)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was conducted with the support of Cancer Care Ontario through funding provided by the Government of Ontario. Parts of this material are based on data and information provided by Cancer Care Ontario (CCO). The opinions, results, view, and conclusions reported in this paper are those of the authors and do not necessarily reflect those of CCO. No endorsement by CCO is intended or should be inferred. This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results, and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed in the material are those of the author(s), and not necessarily those of CIHI.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
de Oliveira, C., Cheng, J. & Kurdyak, P. Determining preventable acute care spending among high-cost patients in a single-payer public health care system. Eur J Health Econ 20, 869–878 (2019). https://doi.org/10.1007/s10198-019-01051-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-019-01051-4