Abstract
Background
A combination of assays for the presence of serum anti-Helicobacter pylori IgG antibody (HPA) and serum pepsinogen (PG) concentrations can be used to screen for gastric cancer risk. In Japan, this “ABC method” is considered an effective means of stratifying gastric cancer risk. This study aimed to ascertain its cost-effectiveness for assessing gastric cancer risk.
Methods
A Markov model was constructed to compare the cost-effectiveness of two strategies for gastric cancer-risk screening over a 30-year period: the ABC method, which uses a combination of assessing the presence of HPA and measuring serum PG concentrations and scheduling endoscopies accordingly, and annual endoscopic screening. Clinical and epidemiological data on variables in the model were obtained from published reports. Analyses were made from the perspective of the Japanese health care payer.
Results
According to base-case analysis, the ABC method cost less than annual endoscopic screening (64,489 vs. 64,074 USD) and saved more lives (18.16 vs. 18.30 quality-adjusted life years). One-way analyses confirmed the robustness of the cost-effectiveness results. The probability that the ABC method is cost-effective in Japanese individuals aged 50 years was 0.997.
Conclusions
A combination of HPA and serum PG assays, plus scheduling endoscopy accordingly, is a cost-effective method of screening for gastric cancer risk in Japan.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the third leading cause of cancer-related deaths in both sexes worldwide, accounting for about 723,000 deaths in 2012. Although half of all gastric cancer cases are reportedly in eastern Asia, gastric cancer is also a burden in eastern and southern Europe [1].
More than 100,000 new cases of gastric cancer are diagnosed annually in Japan, resulting in 50,136 deaths. According to the Japanese Ministry of Health, Labour and Welfare, gastric cancer-related deaths accounted for 14.2% of all cancer deaths in 2010 [2]. Furthermore, according to a Survey of National Medical Care Insurance Services, medical expenses arising from gastric cancer treatment accounted for ~10% of medical expenses for all cancers in 2009. Gastric cancer prevention should thus be a priority in Japan [3].
Helicobacter pylori infection is associated with an increased risk of gastric cancer [4]; a meta-analysis of six randomised controlled trials concluded that H. pylori eradication reduces gastric cancer incidence by 66% [5]. Determining the presence of serum H. pylori IgG antibody (HPA) is useful for evaluating H. pylori status. Atrophic gastritis is also known to be associated with gastric cancer. Human pepsinogens (PGs), classified as PG I and PG II, are proenzymes for the digestive enzyme pepsin and are secreted by gastric mucosal cells. Serum PG concentrations reflect the status of the gastric mucosa and thus serve as markers of atrophic gastritis [6]. PGI is secreted by chief and mucous neck cells in the fundic glands, whereas PGII is also secreted by cells in the pyloric and Brunner glands. PG I concentration <70 μg/l and PG I/II ratio <3.0 are considered to indicate gastric atrophy; individuals with findings outside these ranges are considered not to have gastric atrophy.
H. pylori infection and atrophic gastritis are strong predictors of gastric cancer risk, especially in the Japanese population [7,8,9]. Screening for gastric cancer risk using a combination of serum HPA and PG assays, referred to as the “ABC method,” may be an appropriate and effective means of stratifying gastric cancer risk in Japan because it can differentiate between individuals at high and low risk of developing gastric cancer and detect both intestinal- and diffuse-type early stage gastric cancers [10]. By providing a measure of an individual’s cancer risk, the ABC method may help to determine the optimal strategy in relation to H. pylori eradication and frequency of endoscopic screening.
It is important to establish an efficient, cost-effective, and practical nationwide screening method for the early detection of gastric cancer in Japan. The recently revised version of the Japanese guidelines for gastric cancer screening recommends endoscopic screening for reducing gastric cancer-related mortality in Japan [11]. Several studies have attempted to estimate the cost-effectiveness of strategies for eliminating gastric cancer [12,13,14]. However, no study has examined the long-term cost-effectiveness of the ABC method in relation to gastric cancer in Japan. Given differences in epidemiological characteristics and health insurance systems, evidence from previous cost-effectiveness studies may not be applicable in Japan.
The aim of this study was to evaluate the cost-effectiveness of gastric cancer screening by the ABC method in Japanese individuals from the perspective of the Japanese health care payer.
Methods
Target population
The target population was defined as 50-year-old Japanese individuals who have high gastric cancer incidence and mortality who had not undergone H. pylori eradication [15]. Notably, the national cancer screening programme for gastric cancer recommends that all Japanese persons aged ≥50 years undergo screening annually [11].
Model
A Markov cohort model was designed to assess the costs of care and clinical effectiveness of the ABC method (assessing presence of HPA and measuring serum PG concentrations) for screening Japanese persons for gastric cancer risk (Fig. 1) [15].
After such screening, individuals can be classified into the following four groups: negative for both HPA and gastric atrophy (group A); seropositive for H. pylori but negative for gastric atrophy (group B); positive for both HPA and gastric atrophy (group C); gastric atrophy with HPA concentrations below the cut-off value (group D) [6].
Individuals in group A need no follow-up because they are considered to be at low risk of developing gastric cancer. In contrast, H. pylori eradication therapy is considered indicated for all individuals in groups B–D. Individuals in these higher risk groups are also candidates for periodic endoscopic follow-up. As the Markov modelling progressed, gastric cancer incidence differed between the groups in the study cohort [7] (Table 1).
A primary decision-analysis model compared two intervention strategies: scheduled screening with endoscopy after H. pylori eradication and annual endoscopic screening.
Assumptions
All individuals were allocated to four categories with different risks of gastric cancer and underwent scheduled endoscopic screening according to the level of gastric cancer risk. It was assumed that individuals in group A did not undergo endoscopic screening, whereas those in groups B and C underwent endoscopy every 3 and 2 years, respectively, and those in group D annually. These assumptions are based on the findings of a randomised clinical trial conducted by Gotoba et al. [16]. It was also assumed that detection rates did not differ between endoscopic screening at 2- and 3-year intervals compared with annual screening [17]. The rate of gastric cancer screening in Japan was assumed to be 36.7%, this figure being based on National Cancer Centre Cancer Information Service data [18]. The endoscopic screening rate for high-risk individuals was assumed to be 60% in those undergoing ABC screening because such gastric cancer risk testing may provide an incentive for individuals to also undergo endoscopic screening. Individuals with positive endoscopy findings underwent biopsies to obtain definite diagnoses and minimise false positives.
Patients in Groups B–D underwent H. pylori eradication by triple therapy with a proton pump inhibitor 30 mg/day, amoxicillin 1.5 g/day, and clarithromycin 800 mg/day for 7 days as first-line therapy. Patients in whom eradication was not achieved by this therapy received second-line H. pylori eradication therapy, in which metronidazole at 250 mg/day for 7 days is substituted for clarithromycin. Eradication rates for first- and second-line therapies were assumed to be 65.3 and 84.0%, respectively, on the basis of the findings of Sasaki et al. [19]. Eradication was assessed by the urea breath test and H. pylori stool-antigen test 8 weeks after completion of eradication therapy. According to a systematic review and meta-analysis conducted by Lee et al. [20], successful eradication is associated with an estimated reduction in risk of developing gastric cancer of 0.53 (range 0.44–0.64).
It was assumed that individuals in group D also underwent H. pylori eradication because, despite their HPA concentrations being below the cut-off value, some of these individuals would have had H. pylori infection. The incidence of gastric cancer is not decreased by eradication in these individuals because they already have advanced gastric mucosal atrophy.
The annual endoscopic screening assumed no H. pylori eradication and that all individuals underwent endoscopic screening every year. With both strategies, individuals who did not undergo screening were diagnosed as having gastric cancer only when they presented with symptoms. Transitions between gastric cancer stages and incidence of gastric cancer were assumed to be similar in the screened and unscreened groups.
Finally, to compensate for lead-time bias, it was assumed that patients whose gastric cancers were detected earlier by screening survived longer than those whose diagnoses of Stage I cancer were made on clinical grounds (Table 1).
Model variables
Table 1 shows variables believed to affect the incidence rate of gastric cancer, the distribution of TNM staging and 5-year survival, sensitivity and specificity of endoscopic screening, quality of life scores, and treatment costs (Table 1, Supplementary Table S1–S4) [7, 19,20,21,22,23,24,25,26,27,28,29,30,31, 33, 36].
We used age- and sex-adjusted incidence rates reported by Ikeda et al. as the baseline risk at age 50 among four categories with different risks of gastric cancer. The increasing incidence with age was based on Japanese epidemiological data that reflect the natural history of gastric cancer [7, 25].
The transition probability (p) of an event occurring over a specific time interval (t) was calculated using an incidence rate (r) according to the following formula: p = 1 − exp(−rt). The probabilities of transition from gastric cancer to death were drawn from published Japanese nationwide gastric cancer registration data [27]. Age-specific death rates for the general population were estimated from abridged life tables for Japan in 2014 [28].
The cost of endoscopic screening was set to 147 USD based on expert opinions because screening costs are not covered by health insurance in Japan and are therefore not listed in the tariffs. The screening costs do not include costs of pre- or post-test counselling.
Direct medical costs were considered only from the perspective of the Japanese health care payer. The cost of H. pylori eradication therapy was estimated from the Japanese medical fee list and price list for drugs in 2014 [29, 30]. Using medical record data in the database of Niigata University Medical and Dental Hospital for the years 2002 to 2009, the total costs for inpatients and outpatients with gastric cancer undergoing any treatments were derived for four groups, which were categorised by TNM staging. These costs included hospital visits, hospitalisation, laboratory tests, mucosectomy, surgery, chemo-/radiotherapy, and other medical procedures. The costs were calculated for three time periods, the first being the year from initiation of gastric cancer treatment and the third being the last year of life.
Health expenditures unrelated to gastric cancer in added life years were included in the analysis. National health expenditure in 2014 by age group was obtained from the Ministry of Health, Labour and Welfare; these values are also shown in Table 1 [31]. All costs were converted into USD using 2014 exchange rates (1 USD = 105.8 JPY), as reported by the Organization for Economic Co-operation and Development (Table 2) [32].
The primary measure of effectiveness in the present analysis was quality-adjusted life years (QALYs). Values for health-related quality of life, in which 1 year of life is multiplied by a utility factor between 0 (death) and 1 (perfect health), were taken from Miguel et al., who used the EQ-5D-5L quality of life questionnaire to estimate utility scores in patients with gastric pre-cancer and cancer [33] (Table 1). We obtained the value for utility of no symptoms from a report by Shiroiwa et al., who estimated the utility of the general Japanese population [34] (Supplementary Table S4).
Cost-effectiveness analysis
Cost-effectiveness was evaluated using an incremental cost-effectiveness ratio (ICER), which represents the additional cost of the ABC method over annual endoscopic screening required to achieve one extra QALY. Willingness-to-pay threshold was set at 50,000 USD, as in most economic analyses, and an ICER <50,000 USD/QALY was defined as being cost-effective [35]. Cost-effectiveness during the 30-year follow-up period was evaluated by calculating the lifetime cost and QALYs; the average life span in Japan is approximately 80 years.
A base-case analysis incorporating the baseline variables shown in Tables 1 and 2 was performed initially. The variability of the results was then assessed and multiple one-way sensitivity analyses performed by adjusting variables such as incidence of gastric cancer, endoscopy characteristics, eradication rate, 5-year survival rate, annual care costs, and quality of life utility scores. Finally, probabilistic sensitivity analysis (PSA) was performed using Monte Carlo simulations involving 100,000 samples to assess uncertainty in the base-case results for estimated costs and QALYs. For each run of the simulation, input values for variables were drawn randomly from appropriate distributions. In the PSA, the transition probabilities and quality of life utility scores were explored by assuming a beta distribution, whereas annual care costs for gastric cancer were varied according to a gamma distribution. Dirichlet distributions were assigned to the proportions of gastric cancer-risk groups and stage distributions of gastric cancer. Adverse endoscopic events and risk reduction associated with successful H. pylori eradication were assigned Poisson and log-normal distributions, respectively. Triangular distributions were introduced for other variables, using their lower and upper ranges. On the basis of guidelines for the economic evaluation of health insurance technologies in Japan [36], costs and QALYs were discounted at a rate of 2% per year in the base-case analysis. All analyses were performed using TreeAge Pro 2017 software (Williamstown, MA, USA).
Results
Base-case analysis
Base-case analysis indicated that the ABC method was less expensive than no intervention (64,489 vs. 64,074 USD, respectively) and prolonged QALYs (18.16 vs. 18.30 QALYs, respectively) (Table 3). The ABC method may therefore be considered preferable to annual endoscopic screening in terms of both QALY gains and cost. It was also shown that the ABC method reduced gastric cancer-related cost by 35% compared with annual endoscopic screening.
Sensitivity analysis
The results of the sensitivity analyses are shown in Table 4. The ABC method resulted in longer QALYs and lower costs or ICER <50,000 USD than annual endoscopic screening in all one-way sensitivity analyses and remained cost-effective across the range of all variables.
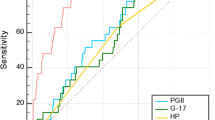
The cost-effectiveness acceptability curves resulting from the PSA for the ABC method are shown in Fig. 2. PSA demonstrated that the model results are consistent with the probability of the ABC method being cost-effective for a given ICER investment ceiling. At an investment of 10,000 USD/QALY, 99.7% of the simulations demonstrated that the ABC method was cost-effective in individuals aged 50 years. These conclusions were not significantly affected by uncertainties around the input variables.
Discussion
Early detection and treatment of gastric cancer are crucial for improving survival and reducing medical costs. We believe this study is the first to use a simulation model for cost-effectiveness analysis of the clinical effectiveness and economic consequences of the ABC method of gastric cancer screening in Japan.
The national cancer screening programme in Japan has historically used barium gastrography to detect gastric cancer. However, only ~10% of the at-risk population actually underwent such examinations in 2008. The current screening programme is also compromised by the lower sensitivity of barium gastrography than endoscopic screening for detecting early gastric cancer [23]. Moreover, because a previous study in Japan found that about 3% of the cumulative risk of cancer to age 75 years is attributable to diagnostic X-ray exposure [37], we did not use radiographic screening as a comparator in our study.
The national screening rate for gastric cancer in the whole of Japan was 37% in 2013. The screening rate of 60.2% in Yamagata was the highest among 47 Japanese regions, while the screening rate of 30.2% in Oosaka was the lowest in Japan [22]. In Japan, 93 local government areas and 5.3% of national government areas used the ABC method for opportunity screening for gastric cancer in 2014 [21]. We consider that the ABC method will become a major screening and prevention strategy for gastric cancer because annual endoscopic screening as a primary screening strategy is cumbersome and time-consuming.
A combination of serum pepsinogen concentration and H. pylori antibodies and the four-risk-group model is an effective strategy for predicting gastric cancer development [7, 9]. The ABC method may provide an incentive for individuals to undergo clinical examinations sooner after developing symptoms. It has the potential to be an effective screening method for gastric cancer because it reportedly halves the cost of detecting gastric cancer [38].
The present study has several limitations. First, we used the same sensitivity and specificity for all age groups and only included a reduction in the risk of gastric cancer when H. pylori eradication had been shown to be successful [20]. Furthermore, we did not obtain data on the effect of H. pylori eradication on gastric cancer risk in relation to patient age. Second, we estimated gastric cancer treatment costs based only on data for patients at Niigata University Medical and Dental Hospital and did not include costs associated with the use of medical services at other hospitals and clinics. Moreover, these data included costs for gastric cancer and other illnesses covered under the Japanese health insurance system. We attempted to minimise the effects of these limitations by performing PSA over a wide range of variables. Another limitation of this study was the unavailability of utility scores from Japanese sources for each stage. Data on utilities obtained by a single questionnaire would be helpful for conducting cost-effectiveness analyses in relation to gastric cancer. We therefore assigned a utility based on the findings of a Portuguese study [33] that determined the utilities of gastric pre-cancer and cancer using a single standardised instrument, namely the EQ-5D-5L.
As to the model assumptions, both the sensitivity of serum HPA for H. pylori infection and serum pepsinogen concentration, which predicts atrophic gastritis, were assumed to be higher than 90% provided that we had classified the participants correctly in our analysis [39, 40]. Atrophic gastritis is certainly related to the occurrence of gastric cancer. However, whether atrophic gastritis is associated with significant differences in cancer stage is controversial. We therefore did not consider differences in cancer stage between the groups in this study.
Because we calculated 5-year survival rates based on diagnosed stage, in our study we applied 5-year survival rates to the corresponding cancer stages at diagnosis without modelling transitions between stages. Our estimation of costs for care of gastric cancer included the occurrence of relapse. We did therefore take stage-specific costs into consideration, but only applied utility decrements in the final year of individuals who had relapses and had died. We incorporated lead times for earlier detection of cancers by screening by adding the assumption that early gastric cancer detected by screening has a 3% higher 5 years survival rate than clinically diagnostic gastric cancer. We examined the influence of this point on base-case results by sensitivity analysis [41].
Eradication of H. pylori reduces both the incidence of gastric cancer and peptic ulcer and the prevalence and costs of managing dyspepsia. Economic analyses suggest that eradication of H. pylori as a means of controlling gastric cancer is cost-effective in high-risk populations [42]. Several studies have attempted to estimate the cost-effectiveness of H. pylori eradication and endoscopic screening for gastric cancer. A study from Singapore using a similar simple screening model suggested that 2-yearly endoscopy screening in a moderate- to high-risk population is highly cost-effective [26]. Another study using the three-state Markov model has demonstrated that H. pylori eradication is cost-effective in Korea [13], suggesting that the costs of H. pylori eradication should be a priority for reimbursement because such eradication likely prevents subsequent cancer and thus reduces overall health care costs. The current study provides updated estimates of the cost-effectiveness of H. pylori eradication and scheduled endoscopic screening for gastric cancer. A Canadian economic evaluation of gastric cancer screening reported that the ICERs of several prevention strategies ranged from approximately $30,000 to $50,000 compared with no screening [43]. They used the Markov model split over nine states such as screening, H. pylori infection, and gastric cancer prognosis.
In conclusion, gastric cancer screening based on the ABC method is more cost-effective than annual endoscopic screening. However, the applicability of the ABC method should be further evaluated before its introduction as a method for mass screening for gastric cancer in populations with a high incidence of H. pylori infection and atrophic gastritis. Future economic evaluations of gastric cancer screening are needed to determine its effects on long-term mortality and to investigate the incidence of H. pylori infection and atrophic gastritis in screening populations.
References
International Agency for Research on Cancer. GLOBOCAN 2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012. http://globocan.iarc.fr/ (2012). Accessed 26 Mar 2015
National Cancer Center: Center for Cancer Control and Information Service. http://ganjoho.jp/reg_stat/statistics/dl/index.html (2014). Accessed 30 August 2015
Haga, K., Matsumoto, K., Kitazawa, T., et al.: Cost of illness of the stomach cancer in Japan—a time trend and future projections. BMC Health Serv. Res. (2013). doi:10.1186/1472-6963-13-283
Uemura, N., Okamoto, S., Yamamoto, S., et al.: Helicobacter pylori infection and the development of gastric cancer. N. Engl. J. Med. 345, 784–789 (2001)
Ford, A.C., Forman, D., Hunt, R.H., et al.: Helicobacter pylori eradication therapy to prevent gastric cancer in healthy asymptomatic infected individuals: systematic review and meta-analysis of randomised controlled trials. BMJ (2014). doi:10.1136/bmj.g3174
Watabe, H., Mitsushima, T., Yamaji, Y., et al.: Predicting the development of gastric cancer from combining Helicobacter pylori antibodies and serum pepsinogen status: a prospective endoscopic cohort study. Gut 54, 764–768 (2005)
Ikeda, F., Shikata, K., Hata, J., et al.: Combination of Helicobacter pylori antibody and serum pepsinogen as a good predictive tool of gastric cancer incidence: 20-year prospective data from the Hisayama Study. J. Epidemiol. 26, 629–636 (2016)
Sasazuki, S.: The ABC method and gastric cancer: evidence from prospective studies. J. Epidemiol. 26, 611–612 (2016)
Terasawa, T., Nishida, H., Kato, K., et al.: Prediction of gastric cancer development by serum pepsinogen test and Helicobacter pylori seropositivity in Eastern Asians: a systematic review and meta-analysis. PLoS One 14, e109783 (2014)
Miki, K.: Gastric cancer screening by combined assay for serum anti-Helicobacter pylori IgG antibody and serum pepsinogen levels–“ABC method”. Proc. Jpn Acad. Ser. B Phys. Biol. Sci. 87, 405–414 (2011)
Research Center for Cancer Prevention and Screening, National Cancer Center, Tokyo, Japan.: Japanese Guideline for Gastric Cancer Screening 2014. http://canscreen.ncc.go.jp/guideline/igan.html (2014). Accessed 30 August 2014
Yeh, J.M., Hur, C., Ward, Z., et al.: Gastric adenocarcinoma screening and prevention in the era of new biomarker and endoscopic technologies: a cost-effectiveness analysis. Gut (2015). doi:10.1136/gutjnl-2014-308588. (Epub ahead of print)
Shin, D.W., Yun, Y.H., Choi, I.J., et al.: Cost-effectiveness of eradication of Helicobacter pylori in gastric cancer survivors after endoscopic resection of early gastric cancer. Helicobacter. 14, 536–544 (2009)
Lansdorp-Vogelaar, I., Sharp, L.: Cost-effectiveness of screening and treating Helicobacter pylori for gastric cancer prevention. Best Pract. Res. Clin. Gastroenterol. 27, 933–947 (2013)
Asaka, M., Kato, M., Graham, D.Y.: Strategy for eliminating gastric cancer in Japan. Helicobacter. 15, 486–490 (2010)
Gotoda, T., Ishikawa, H., Ohnishi, H., et al.: Randomized controlled trial comparing gastric cancer screening by gastrointestinal X-ray with serology for Helicobacter pylori and pepsinogens followed by gastrointestinal endoscopy. Gastric Cancer 18, 605–611 (2015)
Hamashima, C., Ogoshi, K., Okamoto, M., et al.: A community-based, case-control study evaluating mortality reduction from gastric cancer by endoscopic screening in Japan. PLoS One 8, e79088 (2013)
Cancer Information Service, National Cancer Center, Japan.: Cancer Registry and Statistics. http://ganjoho.jp/reg_stat/statistics/dl/index.html (2016). Accessed 26 March 2015
Sasaki, H., Nagahara, A., Hojo, M., et al.: Ten-year trend of the cumulative Helicobacter pylori eradication rate for the ‘Japanese eradication strategy’. Digestion. 88, 27–28 (2013)
Lee, Y.C., Chiang, T.H., Chou, C.K., et al.: Association between Helicobacter pylori eradication and gastric cancer incidence: a systematic review and meta-analysis. Gastroenterology (2016). doi:10.1053/j.gastro.2016.01.028
Miki K.: Manual for gastric cancer risk-screening with ABC-method in Japan. (2nd edition), Tokyo (2014) (in Japanese)
Cancer Information Service, National Cancer Center, Japan.: Cancer Registry and Statistics. http://ganjoho.jp/reg_stat/statistics/dl/index.html (2015). Accessed 26 March 2015
Hamashima, C., Okamoto, M., Shabana, M., et al.: Sensitivity of endoscopic screening for gastric cancer by the incidence method. Int. J. Cancer 133, 653–659 (2013)
Yoshino, J.: 5th report of endoscopic complications: results of the Japan Gastroenterological Endoscopy Society survey from 2003 to 2007. Gastroenterol Endosc. 52, 95–103 (2010). (in Japanese)
Hori, M., Matsuda, T., Shibata, A., et al.: Cancer incidence and incidence rates in Japan in 2009: a study of 32 population-based cancer registries for the Monitoring of Cancer Incidence in Japan (MCIJ) project. Jpn. J. Clin. Oncol. 45, 884–891 (2015)
Dan, Y.Y., So, J.B., Yeoh, K.G.: Endoscopic screening for gastric cancer. Clin. Gastroenterol. Hepatol. 4, 709–716 (2006)
Nashimoto, A., Akazawa, K., Isobe, Y., et al.: Gastric cancer treated in 2002 in Japan: 2009 annual report of the JGCA nationwide registry. Gastric Cancer 16, 1–27 (2013)
Statistic Bureau, Ministry of Internal Affairs and Communications: Mortality rates by age group for Japan, 2015. Tokyo http://www.stat.go.jp/data/nihon/back15/02.htm (2017). Accessed 15 March 2017
Jihou Press.: Medicinal Supplies Price List, Tokyo (2014) (in Japanese)
Jihou Press.: National Health Insurance Price List, Tokyo (2014) (in Japanese)
Statistics and Information Department, Minister’s Secretariat, Ministry of Health, Labour, and Welfare: National health expenditures for Japan, 2014. Tokyo http://www.mhlw.go.jp/toukei/saikin/hw/k-iryohi/14/ (2015). Accessed 15 March 2017
Organization for Economic Co-operation and Development.: Monthly Monetary and Financial Statistics (MEI): Exchange rates (USD monthly averages). http://stats.oecd.org/index.aspx?queryid=169 (2015). Accessed 26 March 2015
Areia, M., Alves, S., Brito, D., et al.: Health-related quality of life and utilities in gastric premalignant conditions and malignant lesions: a multicentre study in a high prevalence country. J. Gastrointest. Liver Dis. 23, 371–378 (2014)
Shiroiwa, T., Fukuda, T., Ikeda, S., et al.: Japanese population norms for preference-based measures: EQ-5D-3L, EQ-5D-5L, and SF-6D. Qual Life Res 25, 707–719 (2016)
Shiroiwa, T., Sung, Y.K., Fukuda, T., et al.: International survey on willingness-to-pay (WTP) for one additional QALY gained: what is the threshold of cost effectiveness? Health Econ. 19, 422–437 (2010)
Fukuda, T., Shiroiwa, T., Ikeda, S., et al.: Guideline for economic evaluation of healthcare technologies in Japan. National Institute of Public Health. J Natl Inst Public Health 62, 625–640 (2013). (in Japanese)
de González, Berrington: A, Darby S.: risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet 31, 345–351 (2004)
Yamaguchi, Y., Nagata, Y., Hiratsuka, R., et al.: Gastric cancer screening by combined assay for serum anti-Helicobacter pylori IgG Antibody and serum pepsinogen levels-the ABC method. Digestion. 93, 13–18 (2016)
The Japanese Society for Helicobacter Research. Guideline of diagnosis and treatment for H. pylori infection. 2016 SENTAN IGAKU-SYA, Tokyo. (Japanese)
Agkoc, M., Dursun, H., Albayrak, F., et al.: Usefulness of serum pepsinogen levels as a screening test for atrophic gastritis and gastric cancer. Eurasian J. Med. 42, 15–18 (2010)
Wever, E.M., Draisma, G., Heijnsdijk, E.A., et al.: How does early detection by screening affect disease progression? Modeling estimated benefits in prostate cancer screening. Med. Decis. Mak. 31, 550–558 (2011)
O’Connor, A., O’Morain, C.A., Ford, A.C.: Population screening and treatment of Helicobacter pylori infection. Nat. Rev. Gastroenterol. Hepatol. (2017). doi:10.1038/nrgastro.2016.195
Xie, F., O’Reilly, D., Ferrusi, I.L., et al.: Illustrating economic evaluation of diagnostic technologies: comparing Helicobacter pylori screening strategies in prevention of gastric cancer in Canada. J. Am. Coll. Radiol. 6, 317–323 (2009)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Funding
This work was supported by a Grant-in-Aid for Research Activity Start-up and Challenging Research from the Niigata University of Health and Welfare, 2015 grant no. H27A01, and the Japan Society for the Promotion of Science KAKENHI grant no. 16K08889.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Saito, S., Azumi, M., Muneoka, Y. et al. Cost-effectiveness of combined serum anti-Helicobacter pylori IgG antibody and serum pepsinogen concentrations for screening for gastric cancer risk in Japan. Eur J Health Econ 19, 545–555 (2018). https://doi.org/10.1007/s10198-017-0901-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-017-0901-y