Abstract
Background
Endoplasmic reticulum (ER) stress has been implicated in the development of various renal diseases. Thus, inhibition of ER stress using pharmacological agents may serve as a promising therapeutic approach. We postulated that febuxostat, a novel xanthine oxidase inhibitor, could suppress the ER stress through upregulation of SIRT1 (silent mating type information regulation 2 homolog 1)-AMPK (AMP activated protein kinase)-HO-1 (heme oxygenase-1)/thioredoxin expression.
Methods
We examined the effect of febuxostat on the ER stress induced by a chemical inducer, tunicamycin and non-chemical agents such as angiotensin II, aldosterone, high glucose, and albumin in renal tubular cells. We further examined the in vivo effects of febuxostat using mouse model of kidney disease induced by unilateral ureteral obstruction (UUO). Expression of ER stress was measured by western blot analysis and immunohistochemical stain.
Results
Febuxostat suppressed the ER stress induced by tunicamycin and non-chemical agents, as shown by inhibition of increased GRP78 (glucose-related protein78) and p-eIF2α (phosphospecific-eukaryotic translation initiation factor 2α) expression. Inhibitory effect of febuxostat was mediated through upregulation of SIRT1-AMPK followed by induction of HO-1 and thioredoxin. In animal model of UUO, febuxostat reduced the UUO-induced ER stress, which was abolished by pretreatment with SIRT1 inhibitor (sirtinol) and AMPK inhibitor (compound C).
Conclusion
Febuxostat could suppress the ER stress caused by various ER stress inducers through upregulation of SIRT1-AMPK-HO-1/thioredoxin expression. Targeting these pathways might serve as one of the possible therapeutic approaches in kidney diseases under excessive ER stress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Accumulation of abnormal misfolded proteins in the endoplasmic reticulum (ER) induces stress. To reduce the ER stress, a homeostatic signaling network called unfolded protein response (UPR) is activated. Activation of the UPR usually triggers an adaptive survival response by facilitating the recovery from stress. However, prolonged and excessive ER stress induces cell death through apoptosis to eliminate the affected cell [1]. Furthermore, it has been suggested that excessive ER stress plays an important role in the development of organ fibrosis and inflammation [2].
In kidney, it has been suggested that excessive ER stress contributes to the pathogenesis of various renal diseases, including acute kidney injury, chronic kidney disease, glomerulonephritis, diabetic nephropathy, and renal fibrosis. Chemical agents that modulate the ER stress pathways are known to reduce the renal injury in experimental animal models [3]. Thus, inhibition of ER stress using pharmacological agents may serve as a promising therapeutic approach. However, it has not been known much about whether the drugs commonly used in kidney medicine are able to reduce the ER stress.
Febuxostat is a well-known drug for the treatment of hyperuricemia and gout. It is a non-purine-selective inhibitor of xanthine oxidase (XO), which has higher bioavailability, more potent XO inhibitory effect and fewer side effects than allopurinol. Febuxostat is metabolized to active metabolite by conjugation and oxidation, which is excreted via urine and feces. Half-life elimination time is known as 5–8 h. On the other hand, allopurinol is almost completely metabolized to oxipurinol within 2 h, which is slowly excreted by the kidney over 18–30 h [4].
It has been reported that febuxostat contributes to cardiovascular and renal benefits in animal models with various diseases [5,6,7,8]. However, whether febuxostat is able to inhibit the ER stress is largely unknown.
We postulated that febuxostat could suppress the ER stress in renal tubular epithelial cells. We examined the effect of febuxostat on the ER stress caused by chemical inducer, tunicamycin and non-chemical inducers such as angiotensin II, aldosterone, high glucose, and albumin in renal tubular cells. We also examined the in vivo effects of febuxostat on the ER stress using animal model of kidney disease induced by unilateral ureteral obstruction (UUO).
Sirtuins, a family of NAD+-dependent deacetylases, regulate a wide range of biological processes and link cellular energy and redox state to multiple signaling pathways. Seven sirtuins (SIRT1–7) have been identified in mammals. SIRT1 (silent mating type information regulation 2 homolog 1) is known to exert reno-protective effects by reducing renal fibrosis, suppressing inflammation and apoptosis, inducing autophagy, and protecting against renal aging [9].
AMP-activated protein kinase (AMPK) is a serine/threonine kinase that functions as a critical regulator of intracellular homeostasis. It acts as an energy sensor and modulates multiple biological pathways such as ROS balance, autophagy, apoptosis, and protein synthesis [10]. Activation of AMPK is known to provide therapeutic benefits in several experimental animal models with various kidney diseases [11,12,13]. Thus, SIRT1 and AMPK are considered to serve as future pharmacological targets for renal diseases.
We postulated that inhibitory effect of febuxostat on the ER stress was mediated through upregulation of SIRT-1, followed by activation of AMPK. We examined the effects of SIRT1 inhibitor and AMPK inhibitor on the febuxostat-induced inhibition of ER stress in renal tubular cells and animal model of kidney disease induced by unilateral ureteral obstruction (UUO).
Heme oxygenase-1 (HO-1) is an inducible antioxidant enzyme involved in the degradation of heme. HO-1 plays an important role in cytoprotection by protecting against oxidative stress [14]. Thioredoxin is an endogenous redox protein that shows antioxidative, anti-apoptotic, and anti-inflammatory effects [15]. Both HO-1 and thioredoxin are able to protect cells from oxidative damage. In other studies, HO-1 and thioredoxin have been suggested as modulators of ER stress [16, 17].
We postulated that inhibitory effect of febuxostat on the ER stress was mediated through upregulation of SIRT1-AMPK, followed by induction of HO-1 and thioredoxin in renal tubular epithelial cells. We examined the effect of HO-I inhibitor and thioredoxin inhibitor on the febuxostat-induced inhibition of ER stress. In addition, we investigated the effect of SIRT1 inhibitor and AMPK inhibitor on the febuxostat-induced induction of HO-1 and thioredoxin expression in both cell culture and animal studies.
Materials and methods
Reagent
Febuxostat powder was obtained from Teijin Pharma Limited, Tokyo, Japan. Tunicamycin, PX 12, sirtinol, aldosterone, and albumin were purchased from Sigma Chemical Company (St Louis, MO, USA). Angiotensin II and glucose were acquired from R&D Systems (Minneapolis, MN, USA). Antibodies against GRP78 were obtained from Santa Cruz Biotechnology (Santa Cruz, California, USA). Antibodies against SIRT1, heme oxygenase-1, thioredoxin, phosphospecific-AMPK, total eIF2α (eukaryotic translation initiation factor 2α), phosphospecific-eIF2α (Ser51) and horseradish peroxidase-conjugated secondary antibody were purchased from Cell Signaling Technology (Beverly, MA, USA). Compound C and zinc protoporphyrin IX (Zn (II) PPIX) were supplied by Calbiochem (San Diego, CA, USA).
Cell culture and conditioning
Cell culture experiments were performed using HK-2 cell, a human proximal tubular cell line [18], which was purchased from the American type culture collection. Cells were growth-arrested in serum-free medium for 24 h before being used in the experiments.
To examine whether febuxostat suppressed the tunicamycin-induced ER stress, cells were incubated with tunicamycin (0.2 μM) with or without febuxostat (3–30 μM) for 24 h. To evaluate whether febuxostat inhibited the angiotensin II-, aldosterone-, high glucose-, and albumin-induced ER stress, cells were incubated with angiotensin II (1 μM), aldosterone (100 nM), high glucose (30 mM), and albumin (5 mg/mL) for 3 days and then treated with or without febuxostat, sirtinol, and compound C for 2 days. The concentrations of tunicamycin, angiotensin II, aldosterone, glucose, and albumin used in our experiment were based on the previous study [19].
Western blot analysis
Equal amount of protein from whole cell lysates were separated using a 10% SDS polyacrylamide gels and transferred to nylon membrane. The membranes were incubated with 5% non-fat milk, probed with primary antibody for 2 h, followed by peroxidase-conjugated secondary antibody. Antibody–antigen complexes were detected using ECL system (Amersham Pharmacia Biotech, Arlington, IL, USA). The intensity of each band was measured using a GS-710 densitometer and QuantityOne software (Bio-Rad, Hercules, CA, USA). The results were normalized to the intensity of beta-actin for standardization.
Experimental mouse model of chronic kidney injury induced by unilateral ureteral obstruction (UUO)
It has been well documented that activation of ER stress is associated with UUO-induced renal apoptosis and fibrosis. Angiotensin II and aldosterone were involved in the initiation of UUO-induced renal injury [20, 21]. Therefore, we used a mouse model of UUO to test the hypothesis that febuxostat could reduce the UUO-induced ER stress. Male mouse (C57BL/6) weighing about 20 g was given free access to water and standard chow. UUO model was made by ligation of left ureter through flank incision. Mice were randomly divided into five groups: control mice (n = 5), mice with UUO (n = 5), mice with UUO plus febuxostat (n = 5), mice with UUO plus febuxostat and sirtinol (n = 5), mice with UUO plus febuxostat and compound C (n = 5). Febuxostat was administered by gavage at 10 mg/kg/day. Sirtinol (5 mg/kg) and compound C (20 mg/kg) were administered through intraperitoneal injection. On the 14th day after induction of UUO, the mice were killed. The kidney tissue was fixed in 4% buffered formalin and embedded in paraffin. Tubulointerstitial collagen deposit was assessed semi-quantitatively by the blue color change induced by Masson’s trichrome stain.
Immunohistochemical stain
Paraffin-embedded kidney tissues were cut into 4 μm sections and mounted on glass slides. Sections were deparaffinized with xylene and rehydrated with graded ethanol. Endogenous peroxidase activity was blocked by 0.3% hydrogen peroxide for 30 min. A microwave-based antigen retrieval method was used with 10 mmol/L citrate buffer for 10 min. Non-specific binding was prevented using 1% BSA. Sections were then incubated with primary antibodies against GRP78, HO-1, and thioredoxin for 2 h and biotinylated secondary antibodies for 1 h and horseradish peroxidase–streptavidin conjugate for 30 min, followed by detection using diaminobenzidine DAB stain (Dako, Glostrup, Denmark). Then the sections were counterstained with hematoxylin.
Statistical analysis
Data were expressed as n-fold increase over control as mean ± S.E. Statistical analysis was performed using Kruskal—Wallis test, followed by a Mann–Whitney U test using SPSS (SPSS Inc., Chicago. USA). P < 0.05 value was considered statistically significant.
Results
Febuxostat suppressed the ER stress caused by chemical ER stress inducer, tunicamycin, in tubular epithelial cells
To investigate whether febuxostat inhibited the tunicamycin-induced ER stress in tubular HK-2 cells, we examined the change of ER stress biomarkers, GRP78 (glucose-related protein78) and p-eIF2α (phosphospecific-eukaryotic translation initiation factor 2α). Tunicamycin induced the ER stress, as shown by upregulation of GRP78 and p-eIF2α. Febuxostat suppressed the tunicamycin-induced ER stress in a dose-dependent manner (3–30 μM) (Fig. 1).
Dose-dependent inhibition of tunicamycin-induced ER stress by febuxostat in HK-2 cells. Proximal tubular cells (HK-2 cells) were incubated with tunicamycin (TM, 0.2 μM) with or without febuxostat (3–30 μM) for 24 h. Expression of GRP78 and p-eIF2α was examined by western blot analysis. The relative densities of the bands for GRP78 and p-eIF2α were normalized to those for actin and total eIF2α, respectively, for standardization. Representative blots and quantitative analysis from three independent experiments were shown. Results were expressed as n-fold increase over control as mean ± S.E. #P < 0.05 vs. con (control), ##P < 0.05 vs. TM. GRP78 glucose-related protein 78, p-eIF2α phosphospecific-eukaryotic translation initiation factor 2α
Inhibitory effect of febuxostat on the tunicamycin-induced ER stress was mediated through upregulation of SIRT1, followed by activation of AMPK
Febuxostat (30 μM) upregulated the expression of SIRT1 and phosphospecific-AMPK (p-AMPK) in a dose-dependent manner (3–30 μM) (Fig. 2a).
Reversal of the inhibitory effect of febuxostat on tunicamycin-induced ER stress by sirtinol (SIRT1 inhibitor) and compound C (AMPK inhibitor). Proximal tubular cells were incubated with tunicamycin (TM, 0.2 μM) with or without febuxostat (3–30 μM) for 24 h. Expression of SIRT1 and p-AMPK was examined by western blot analysis (a). Proximal tubular cells were incubated with tunicamycin (TM, 0.2 μM) with or without febuxostat (febu, 30 μM), sirtinol (sirt, SIRT1 inhibitor, 10 μM), and compound C (comp C, AMPK inhibitor, 20 μM) for 24 h. Expression of GRP78 and p-eIF2α was examined by western blot analysis (b). The relative densities of the bands for SIRT1, p-AMPK, GRP78, and p-eIF2α were normalized to those for actin, total AMPK, and total eIF2α, respectively, for standardization. Representative blots and quantitative analysis from three independent experiments were shown. Results were expressed as n-fold increase over control as mean ± S.E. #P < 0.05 vs. con (control), ##P < 0.05 vs. TM, ###P < 0.05 vs. TM + febu
To determine whether upregulation of SIRT1 and p-AMPK by febuxostat was directly involved in febuxostat’s inhibitory effect on the tunicamycin-induced ER stress, we examined the effect of SIRT1 inhibitor (sirtinol, 10 μM) and AMPK inhibitor (compound C, 20 μM) on the febuxostat’s inhibitory effect. It has been known that sirtinol is a selective inhibitor for SIRT1 and SIRT2.
Western blot analysis showed that both sirtinol and compound C reversed the febuxostat’s inhibitory effect, suggesting that inhibitory effect of febuxostat on the ER stress was mediated through upregulation of SIRT1 and p-AMPK (Fig. 2b).
To verify whether upregulation of SIRT1 by febuxostat was ahead of activation of AMPK, we examined the effect of sirtinol and compound C on the febuxostat-induced SIRT1 and p-AMPK. Sirtinol inhibited the febuxostat-induced upregulation of SIRT1 and p-AMPK, whereas compound C suppressed the febuxostat-induced upregulation of p-AMPK, but not SIRT1, suggesting that effect of febuxostat on the tunicamycin-induced ER stress was mediated through upregulation of SIRT1, followed by activation of AMPK (Fig. 3).
Upregulation of SIRT1, followed by activation of AMPK by febuxostat. Proximal tubular cells were incubated with tunicamycin (TM, 0.2 μM) with or without febuxostat (febu, 30 μM), sirtinol (sirt, SIRT1 inhibitor, 10 μM), compound C (comp C, AMPK inhibitor 20 μM) for 24 h. Expression of SIRT1 and p-AMPK was examined by western blot analysis. The relative densities of the bands for SIRT1 and p-AMPK were normalized to those for actin and total AMPK, respectively, for standardization. Representative blots and quantitative analysis from three independent experiments were shown. Results were expressed as n-fold increase over control as mean ± S.E. #P < 0.05 vs. TM, ##P < 0.05 vs. TM + febu
Inhibitory effect of febuxostat on the tunicamycin-induced ER stress was mediated through induction of heme oxygenase-1 and thioredoxin
Febuxostat (30 μM) induced the expression of heme oxygenase-1 (HO-1) and thioredoxin in a dose-dependent manner (3–30 μM) (Fig. 4a). To investigate whether induction of HO-1 and thioredoxin by febuxostat was directly involved in febuxostat’s inhibitory effect on the tunicamycin-induced ER stress, we examined the effect of HO-I inhibitor (Zinc protoporphyrin IX, Zn (II) PPIX, 20 μM) and thioredoxin inhibitor (PX12, 25 μM) on the febuxostat’s inhibitory effect. Western blot analysis revealed that both Zn (II) PPIX and PX12 blocked the febuxostat’s inhibitory effect on the tunicamycin-induced ER stress, suggesting that inhibitory effect of febuxostat was mediated through induction of HO-1 and thioredoxin (Fig. 4b).
Reversal of the inhibitory effect of febuxostat on tunicamycin-induced ER stress by PPIX (HO-1 inhibitor) and PX12 (thioredoxin inhibitor). Proximal tubular cells were incubated with tunicamycin (TM, 0.2 μM) with or without febuxostat (3–30 μM) for 24 h. Expression of heme oxygenase-1 (HO-1) and thioredoxin was examined by western blot analysis (a). Proximal tubular cells were incubated with tunicamycin (TM, 0.2 μM) with or without febuxostat (febu, 30 μM), PPIX (HO-1 inhibitor, 20 μM), and PX12 (thioredoxin inhibitor, 25 μM) for 24 h. Expression of GRP78 and p-eIF2α was examined by western blot analysis (b). The relative densities of the bands for SIRT1 and p-AMPK, GRP78, and p-eIF2α were normalized to those for actin, total AMPK, and total eIF2α, respectively, for standardization. Representative blots and quantitative analysis from three independent experiments were shown. Results were expressed as n-fold increase over control as mean ± S.E. #P < 0.05 vs. con (control), ##P < 0.05 vs. TM, ###P < 0.05 vs. TM + febu
Inhibitory effect of febuxostat on the tunicamycin-induced ER stress was mediated through upregulation of SIRT1-AMPK-HO-1/thioredoxin expression
To explore whether induction of HO-1 and thioredoxin by febuxostat was mediated through upregulation of SIRT1 and activation of AMPK, we examined the effect of SIRT1 inhibitor (sirtinol, 10 μM) and AMPK inhibitor (compound C, 20 μM) on the tunicamycin-induced induction of HO-1 and thioredoxin. Western blot analysis revealed that both sirtinol and compound C reversed the febuxostat-induced induction of HO-1 and thioredoxin, indicating that inhibitory effect of febuxostat on the tunicamycin-induced ER stress was mediated through upregulation of SIRT1-AMPK-HO-1/thioredoxin expression (Fig. 5).
Upregulation of SIRT1 and activation of AMPK, followed by induction of HO-1 and thioredoxin by febuxostat. Proximal tubular cells were incubated with tunicamycin (TM, 0.2 μM) with or without febuxostat (febu, 30 μM), sirtinol (sirt, SIRT1 inhibitor, 10 μM), compound C (comp C, AMPK inhibitor 20 μM) for 24 h. Expression of heme oxygenase-1 (HO-1) and thioredoxin was examined by western blot analysis. The relative densities of the bands for HO-1 and thioredoxin were normalized to those for actin for standardization. Representative blots and quantitative analysis from three independent experiments were shown. Results were expressed as n-fold increase over control as mean ± S.E. #P < 0.05 vs. TM, ##P < 0.05 vs. TM + febu
Febuxostat suppressed the ER stress caused by non-chemical ER stress inducers such as angiotensin II, aldosterone, high glucose, and albumin through upregulation of SIRT1 and activation of AMPK
Angiotensin II, aldosterone, high glucose, and albumin induced the ER stress, as shown by upregulation of GRP78 and p-eIF2α. Febuxostat (30 μM) inhibited the angiotensin II-, aldosterone-, high glucose-, and albumin-induced ER stress, which were abolished by pretreatment with SIRT1 inhibitor (sirtinol, 10 μM) and AMPK inhibitor (compound C, 20 μM). These data suggested that inhibitory effect of febuxostat on the angiotensin II-, aldosterone-, high glucose-, and albumin-induced ER stress was mediated through upregulation of SIRT1 and activation of AMPK (Fig. 6).
Inhibition of angiotensin II-, aldosterone-, high glucose-, and albumin-induced ER stress by febuxostat through upregulation of SIRT1 and activation of AMPK. Proximal tubular cells were incubated with angiotensin II (AgII, 1 μM), aldosterone (aldo, 100 nM), high glucose (glu, 30 mM), and albumin (alb, 5 mg/ml) for 3 days and then treated with or without febuxostat (febu, 30 μM), sirtinol (sirt, SIRT1 inhibitor, 10 μM), compound C (comp C, AMPK inhibitor 20 μM) for 2 days. Expression of GRP78 and p-eIF2α was examined by western blot analysis. The relative densities of the bands for GRP78 and p-eIF2α were normalized to those for actin and total eIF2α, respectively, for standardization. Representative blots and quantitative analysis from three independent experiments were shown. Results were expressed as n-fold increase over control as mean ± S.E. #P < 0.05 vs. con (control), ##P < 0.05 vs. AgII, aldo, glu, or alb, ###P < 0.05 vs. AgII + febu, aldo + febu, glu + febu, alb + febu
Febuxostat reduced the unilateral ureteral obstruction (UUO)-induced ER stress through upregulation of SIRT1 and activation of AMPK
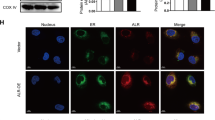
To examine the in vivo inhibitory effect of febuxostat on the ER stress, we conducted an animal study using UUO mouse model. Febuxostat reduced the UUO-induced tubular expression of GRP78 and also increased the expression of HO-1 and thioredoxin, which were prevented by pretreatment with SIRT1 inhibitor (sirtinol) and AMPK inhibitor (compound C), suggesting that inhibitory effect of febuxostat on the UUO-induced ER stress was mediated through upregulation of SIRT1 and activation of AMPK (Fig. 7). Febuxostat also reduced the UUO-induced collagen deposit, which was abolished by pretreatment with sirtinol or compound C (Fig. 8).
Inhibition of unilateral ureteral obstruction (UUO)-induced ER stress by febuxostat through upregulation of SIRT1 and activation of AMPK in a mouse model of UUO. UUO model was made by ligation of left ureter through flank incision. Mice were randomly divided into five groups: control mice (n = 5), mice with UUO (n = 5), mice with UUO plus febuxostat (n = 5), mice with UUO plus febuxostat and sirtinol (n = 5), and mice with UUO plus febuxostat and compound C (n = 5). Febuxostat (febu, 10 mg/kg/day) was administered by gavage for 14 days. Sirtinol (sirt, 5 mg/kg/day) and compound C (comp C, 20 mg/kg/day) were administered by intraperitoneal injection for 14 days. Immunohistochemical staining (a), and western blot analysis of renal cortical tissue (b) were shown. #P < 0.05 vs. con (control), ##P < 0.05 vs. U, ###P < 0.05 vs. U + febu
Inhibition of unilateral ureteral obstruction (UUO)-induced collagen deposit by febuxostat through upregulation of SIRT1 and activation of AMPK in a mouse model of UUO. Mice were randomly divided into five groups: control mice (n = 5), mice with UUO (n = 5), mice with UUO plus febuxostat (n = 5), mice with UUO plus febuxostat and sirtinol (n = 5), and mice with UUO plus febuxostat and compound C (n = 5). Febuxostat (febu, 10 mg/kg/day) was administered by gavage for 14 days. Sirtinol (sirt, 5 mg/kg/day) and compound C (comp C, 20 mg/kg/day) were administered by intraperitoneal injection for 14 days. Masson’s trichrome staining (a) and collagen deposit score (b) were shown. #P < 0.05 vs. con (control), ##P < 0.05 vs. U, ###P < 0.05 vs. U + febu
Discussion
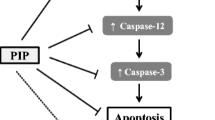
In the present study, we demonstrated that febuxostat could suppress the tunicamycin-induced ER stress through upregulation of SIRT1-AMPK-HO-1/thioredoxin expression in renal tubular HK-2 cells. Febuxostat also inhibited the ER stress induced by angiotensin II, aldosterone, high glucose, and albumin through activation of SIRT1 and AMPK. Animal study showed that treatment with febuxostat reduced the unilateral ureteral obstruction (UUO)-induced ER stress, which was blocked by pretreatment with SIRT1 inhibitor (sirtinol) and AMPK inhibitor (compound C). Febuxostat induced the HO-1 and thioredoxin expression in UUO animal model, which was also abolished by pretreatment with SIRT1 inhibitor and AMPK inhibitor. These data indicated that febuxostat could suppress the ER stress caused by various ER stress inducers and inhibitory effect of febuxostat was mediated through upregulation of SIRT1-AMPK-HO-1/thioredoxin expression (Fig. 9).
It is becoming clear that ER stress is involved in various kidney diseases. Treatment of experimental animals with chemical compounds that inhibit the specific ER stress signaling pathways is known to reduce the renal injury [3]. However, the effect of drugs commonly used in kidney disease on the ER stress has not been revealed much.
Febuxostat, a non-purine selective inhibitor of xanthine oxidase, provides therapeutic benefits in 5/6 nephrectomized rats, renal ischemic-reperfusion injury rats, unilateral ureteral obstruction rats, and tacrolimus-induced nephrotoxicity [5,6,7,8]. However, the potential effect of febuxostat on the ER stress has not been analyzed in detail.
We found that febuxostat suppressed the ER stress induced by tunicamycin as well as non-chemical agents such as angiotensin II, aldosterone, high glucose, and albumin in renal tubular epithelial cells. Febuxostat also reduced the unilateral ureteral obstruction (UUO)-induced ER stress. Similar to our findings, it had been reported that febuxostat was able to reduce the renal ER stress in ischemia-perfusion animal model and hyperuricemic nephropathy model [6, 22]. Together with these reports, our data suggested that inhibition of ER stress by febuxostat might be another mechanism by which febuxostat exerted the reno-protective effects.
Next, we elucidated the mechanism by which febuxostat inhibited the ER stress. SIRT1 is known to be involved in the process of aging, transcription, inflammation, apoptosis, and stress resistance [9]. Recent studies show that SIRT1 is expressed in the kidney and acts as a renal survival factor [23]. However, association between SIRT1 and ER stress has not been verified well.
AMPK (AMP-activated protein kinase) plays an important role in maintaining intracellular homeostasis and is abundantly expressed in the kidney. It had been reported that induction of AMPK by metformin attenuated the albumin-induced and glucosamine-induced ER stress, respectively, in renal epithelial cells [24, 25].
We found that febuxostat upregulated the expression of SIRT1 and p-AMPK in a dose-dependent manner in renal tubular cells. Both SIRT1 inhibitor (sirtinol) and AMPK inhibitor (compound C) blocked the febuxostat’s inhibitory effect on the tunicamycin-induced ER stress, as well as on the angiotensin II-, aldosterone-, high glucose-, and albumin-induced ER stress. Animal study also showed that both SIRT1 inhibitor and AMPK inhibitor abolished the inhibitory effect of febuxostat on the UUO-induced ER stress. These data indicated that inhibitory effect of febuxostat on the ER stress was mediated through upregulation of SIRT1 and activation of AMPK, suggesting that SIRT1 and AMPK could be novel therapeutic targets for the treatment of ER stress-induced injury.
It has been reported that SIRT1 and AMPK regulate each other and share many common target molecules. Several studies showed that the interaction between the AMPK and SIRT1 pathways were reciprocal [26].
We found that upregulation of SIRT1 by febuxostat was located upstream of the activation of AMPK in the inhibitory signaling pathway of febuxostat. Similar to our study, it had been reported that SIRT1 activated the AMPK by liver kinase B1 (LKB1) deacetylation in HEK293T cells and in the rat liver [27].
Heme oxygenase-1 (HO-1) and thioredoxin exert cytoprotective effects through antioxidant, anti-inflammatory, anti-apoptotic, and anti-proliferative actions [20, 21]. They are known to be involved in the inhibition of ER stress in renal tubular epithelial cells [16, 17].
We found that febuxostat induced the expression of HO-1 and thioredoxin in a dose-dependent manner in renal tubular cells. Both HO-I inhibitor (Zinc protoporphyrin IX) and thioredoxin inhibitor (PX12) reversed the febuxostat’s inhibitory effect on the tunicamycin-induced ER stress. In addition, SIRT1 inhibitor and AMPK inhibitor suppressed the febuxostat-induced induction of HO-1 and thioredoxin in both cell culture and animal studies, suggesting that inhibitory effect of febuxostat on the ER stress was mediated through upregulation of SIRT1 and activation of AMPK, followed by induction of HO-1 and thioredoxin.
These data suggested that modulating the SIRT1-AMPK-HO-1/thioredoxin signaling pathway might be another strategy to reduce the excess ER stress in addition to blocking the specific ER stress signaling pathway.
Clinical trials of urate-lowering therapy have shown inconsistent results in terms of reno-protection in patients with chronic kidney disease. However, Sato et al. have recently suggested that it is better to consider urate-lowering therapy, among those who are hyperuricemic with evidence of deteriorating renal function [28].
In conclusion, our study provided new insights into reno-protective mechanism of febuxostat and suggested that modulating the SIRT1-AMPK-HO-1/thioredoxin signaling pathway might be another therapeutic strategy for kidney diseases under excessive ER stress condition.
References
Cybulsky AV. Endoplasmic reticulum stress in proteinuric kidney disease. Kidney Int. 2010;77:7–193.
Tanjore H, Lawson WE, Blackwell TS. Endoplasmic reticulum stress as a pro-fibrotic stimulus. Biochim Biophys Acta. 2013;1832(7):940–7.
Cybulsky AV. Endoplasmic reticulum stress, the unfolded protein response and autophagy in kidney diseases. Nat Rev Nephrol. 2017;13(11):681–96.
Julee PS, Deepa RP, Dhrubo JS. Febuxostat: the new generation novel xanthine oxidase inhibitors. Int Pharm Sci. 2011;1:107–15.
Sanchez-Lozada LG, Tapia E, Soto V, et al. Effect of febuxostat on the progression of renal disease in 5/6 nephrectomy rats with and without hyperuricemia. Nephron Physiol. 2008;108:69–788.
Tsuda H, Kawada N, Kaimori JY, et al. Febuxostat suppressed renal ischemia-reperfusion injury via reduced oxidative stress. Biochem Biophys Res Commun. 2012;427:266–72.
Omori H, Kawada N, Inoue K, et al. Use of xanthine oxidase inhibitor febuxostat inhibits renal interstitial inflammation and fibrosis in unilateral ureteral obstructive nephropathy. Clin Exp Nephrol. 2012;16:549–56.
Kim HS, Lim SW, Jin L, Jin J, Chung BH, Yang CW. The protective effect of febuxostat on chronic tacrolimus induced nephrotoxicity in rats. Nephron. 2017;135(1):61–71.
Kitada M, Kume S, Koya D. Role of sirtuins in kidney disease. Curr Opin Nephrol Hypertens. 2014;23(1):75–9.
Fisslhaler B, Fleming I. Activation and signaling by the AMP-activated protein kinase in endothelial cells. Circ Res. 2009;105:114–27.
Lee MJ, Feliers D, Mariappan MM, et al. A role for AMP-activated protein kinase in diabetes-induced renal hypertrophy. Am J Physiol Ren Physiol. 2007;292(2):F617–27.
Morales AI, Detaille D, Prieto M, et al. Metformin prevents experimental gentamycin-induced nephropathy by a mitochondria-dependent pathway. Kidney Int. 2010;77(10):861–9.
Takiar V, Nishio S, Seo-Mayer P, et al. Activating AMP-activated protein kinase (AMPK) slows renal cystogenesis. Proc Natl Acad Sci USA. 2011;108(6):2462–7.
Kirkby KA, Adin CA. Products of heme oxygenase and their potential therapeutic applications. Am J Physiol Ren Physiol. 2006;290:F563–71.
Yamawaki H, Haendeler J, Berk BC. Thioredoxin: a key regulator of cardiovascular homeostasis. Circ Res. 2003;93(11):1029–33.
Chung J, Shin DY, Zheng M, et al. Carbon monoxide, a reaction product of heme oxygenase-1, suppresses the expression of C-reactive protein by endoplasmic reticulum stress through modulation of the unfolded protein response. Mol Immunol. 2011;48(15–16):1793–9.
Kim Y, Li E, Park S. Insulin-like growth factor-1 inhibits 6-hydroxydopamine-mediated endoplasmic reticulum stress-induced apoptosis via regulation of heme oxygenase-1 and Nrf2 expression in PC12 cells. Int J Neurosci. 2012;122(11):641–9.
Ryan MJ, Johnson G, Kirk J, Fuerstenberg SM, Zager RA, Torok-Storb B. HK-2: an immortalized proximal tubule epithelial cell line from normal adult human kidney. Kidney Int. 1994;45(1):48–57.
Kim H, Moon SY, Kim JS, et al. Activation of AMP-activated protein kinase inhibits ER stress and renal fibrosis. Am J Physiol Ren Physiol. 2015;308(3):F226–36.
Pimentel JL Jr, Sundell CL, Wang S, Kopp JB, Montero A, Martinez-Maldonado M. Role of angiotensin II in the expression and regulation of transforming growth factor-beta in obstructive nephropathy. Kidney Int. 1995;48(4):1233–46.
Trachtman H, Weiser AC, Valderrama E, Morgado M, Palmer LS. Prevention of renal fibrosis by spironolactone in mice withy complete unilateral ureteral obstruction. J Urol. 2004;172(4 Pt 2):1590–4.
He L, Fan Y, Xiao W, et al. Febuxostat attenuates ER stress mediated kidney injury in a rat model of hyperuricemic nephropathy. Oncotarget. 2017;8(67):111295–308.
Hao CM, Haase VH. Sirtuins and their relevance to the kidney. J Am Soc Nephrol. 2010;21(10):1620–7.
Lee EK, Jeong JU, Chang JW, et al. Activation of AMP-activated protein kinase inhibits albumin-induced endoplasmic reticulum stress and apoptosis through inhibition of reactive oxygen species. Nephron Exp Nephrol. 2012;121:e38–48.
Thériault JR, Palmer HJ, Pittman DD. Inhibition of the unfolded protein response by metformin in renal proximal tubular epithelial cells. Biochem Biophys Res Commun. 2011;409(3):500–5.
Ruderman NB, Xu XJ, Nelson L, et al. AMPK and SIRT1: a long-standing partnership? Am J Physiol Endocrinol Metab. 2010;298(4):E51–60.
Lan F, Cacicedo JM, Ruderman N, Ido Y. SIRT1 modulation of the acetylation status, cytosolic localization, and activity of LKB1. Possible role in AMP-activated protein kinase activation. J Biol Chem. 2008;283(41):27628–35.
Sato Y, Feig DI, Stack AG, et al. The case for uric acid-lowering treatment in patients with hyperuricemia and CKD. Nat Rev Nephrol. 2019. https://doi.org/10.1038/s41581-019-0174-z.
Acknowledgements
Reprints request to Sang Koo Lee M.D., Division of Nephrology, Department of Internal Medicine, Asan Medical Center, 88, Olympic-ro 43-gil, Songpa-gu, Seoul 138-736, Korea. E-mail: sklee2@amc.seoul.kr.
Funding
No funding received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors have declared no competing interest.
Ethical approval
All procedures performed in animal experiments were approved by Institutional Animal Care and Use Committee of Asan Institute for Life Sciences (Subject No: 2017-13-039).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kim, H., Baek, C.H., Chang, J.W. et al. Febuxostat, a novel inhibitor of xanthine oxidase, reduces ER stress through upregulation of SIRT1-AMPK-HO-1/thioredoxin expression. Clin Exp Nephrol 24, 205–215 (2020). https://doi.org/10.1007/s10157-019-01804-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-019-01804-8