Abstract
Background
Recent reports have described the efficacy of rituximab in treating steroid-dependent nephrotic syndrome (SDNS) in pediatric patients. However, few reports describe data regarding adult-onset SDNS. We investigated the efficacy of rituximab for the management of adult-onset SDNS.
Methods
We performed a retrospective cohort study investigating eight patients with adult-onset SDNS who were treated with rituximab. Clinical data were obtained at the initiation of rituximab therapy. The primary outcomes evaluated were successful suppression of relapses and CD19+ cells after rituximab treatment. The corticosteroid- and immunosuppressant-sparing effect and adverse events were additionally evaluated.
Results
All eight patients were diagnosed with minimal change nephrotic syndrome and received immunosuppressants in addition to corticosteroid. Total number of relapses was 10.5 times as a median value. Rituximab administration was repeated in two patients, whereas six received single-dose rituximab. Three of eight (37.5%) patients showed relapse after rituximab therapy. A rituximab-induced depletion in CD19+ cells noted initially was followed by their reappearance in all patients. There were cases with no relapse after the reappearance of CD19+ cells. The median relapse time pre- and post-rituximab therapy showed a decrease from 1 time/year (interquartile range [IQR] 1–3 times/year) to 0 time/year (IQR 0–1 time/year). Rituximab treatment induced a significant reduction in the required doses of corticosteroid and cyclosporine (P < 0.01). No serious adverse events were observed.
Conclusion
Rituximab treatment was effective not only in childhood-onset but also in adult-onset SDNS. Further studies are needed to establish optimal treatment regimens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
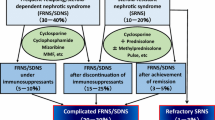
Minimal change nephrotic syndrome (MCNS) shows a high prevalence in pediatric patients; however, most patients show a good response to corticosteroid therapy and > 90% of patients achieve complete remission with initial treatment. MCNS is also a major cause of idiopathic nephrotic syndrome (NS) in adults. Although MCNS patients show a favorable response to steroids, the relapse rate following a reduction of the steroid dose is reportedly as high as 30–70% [1, 2]. In those with steroid-dependent NS (SDNS) and frequently relapsing NS (FRNS), relapse prevention and reduction of steroids is managed with the addition of immunosuppressants such as cyclosporine (CyA), cyclophosphamide (CPA), mizoribine (MZR), tacrolimus (TAC), and mycophenolate mofetil (MMF). However, serious side effects and increased medical costs associated with long-term administration act as major drawbacks related to the use of these drugs.
Recent reports have described the therapeutic efficacy of rituximab, a monoclonal antibody targeting the CD20 antigen of B lymphocytes, in treating idiopathic NS. Standard treatment methods for membranous nephropathy (MN) remain controversial [3]. Ruggenenti et al. demonstrated the efficacy and safety of rituximab in a large-scale cohort study [4]. The authors also reported the therapeutic effect of rituximab in Japanese patients with MN [5]. Moreover, rituximab has been reported to significantly reduce the relapse rate in children with SDNS and FRNS [6,7,8,9,10,11,12,13,14]. However, few reports have described the efficacy of rituximab in adults [15,16,17,18,19,20]. Additionally, the optimal dosing regimen for rituximab treatment has not been established. We evaluated the efficacy of rituximab in treating adult-onset SDNS.
Materials and methods
Study design and population
We performed a retrospective cohort study at a single hospital. Our study comprised eight patients with adult-onset SDNS who were administered rituximab at Nagoya University Hospital between May 2014 and March 2017. NS was diagnosed based on the clinical practice guidelines established by the Collaborative Working Group of the Ministry of Health, Labour and Welfare NS Research Group and the Japanese Society of Nephrology [21]. This study protocol was approved by The Ethics Committee for Human Research of Nagoya University Hospital (IRB approval number 2017-0192).
Clinical data collection
Baseline characteristics including clinical findings at the initiation of rituximab therapy and medical history were obtained from patients’ medical records. The clinical parameters evaluated were age, gender, body mass index, systolic and diastolic blood pressure, complete blood count, serum total protein and albumin, serum total and low-density lipoprotein cholesterol, serum creatinine, glomerular filtration rate (GFR calculated using the equation for Japanese patients: eGFR [mL/min/1.73 m2] = 194 × Scr−1.094 × Age−0.287 [× 0.739 if female]) [22], CD19+ cell levels, and urinary protein-creatinine ratio (uPCR). With regard to medical history, hypertension, diabetes mellitus, total number of relapses prior to initiation of rituximab therapy, previous use of immunosuppressive agents, and the dosage of prednisolone (PSL) at the time of rituximab infusion were recorded.
Renal pathological diagnosis
A renal biopsy was performed in all patients to establish the histopathological diagnosis. The kidney specimens were studied by light microscopy (LM), immunofluorescence stain (IF), and electron microscopy (EM) using standard techniques. For direct IF stain, 3-µm cryostat sections were stained using polyclonal fluorescein isothiocyanate conjugated antibodies to IgG, IgA, IgM (Medical & Biological Laboratories, Nagoya, Japan), C3, C4, and C1q (Dako, Copenhagen, Denmark). Renal pathological diagnosis was done by two independent pathologists to gain objective assessment.
Rituximab treatment
Screening for infectious diseases was performed in all patients prior to the initiation of rituximab. When necessary, the influenza and pneumococcal vaccines were administered to patients. A single intravenous dose of rituximab was administered to all patients. Only in the first patient, rituximab was infused at a dose of 375 mg/m2 of body surface area. After the second patient, a single fixed dose of rituximab (500 mg) was administered. In the first two patients, rituximab was regularly administered every 6 months, whereas the remaining six patients were administered only a single dose of rituximab (500 mg), and thereafter the clinical course was monitored in all patients. In those who presented with sequential relapses, rituximab was added at a dose of 500 mg after complete remission (CR) was obtained by increasing the steroid dose. Rituximab was reconstituted in saline and instilled at a recommended rate based on the attached document. We administered 100 mg of hydrocortisone sodium succinate, 30 mg of diphenhydramine hydrochloride, and 400 mg of acetaminophen 30 min prior to the rituximab infusion as premedication to minimize infusion reactions. Patients were closely observed, and in those in whom infusion reactions were suspected, we decreased the rate of rituximab administration. The CD19+ cell levels were confirmed immediately prior to the initiation of rituximab and measured each month after the drug was administered. Written informed consent was obtained from all patients prior to the initiation of rituximab therapy.
Outcomes and definitions
The primary endpoint was the occurrence of relapse following rituximab therapy. The reappearance of CD19+ cells was also evaluated. Additionally, the doses of corticosteroid and immunosuppressants required were compared prior to and after administration of rituximab. CR was defined as a decline in the proteinuria to < 0.3 g/day. Relapse was defined as the condition that urine protein ≧ 1 g/day runs or ≧ (2+) continues 2–3 times in a row after CR. If collection of 24-h urine was impossible, the uPCR (represented as g/g creatinine, g/gCr) measured in a spot urine sample was utilized for diagnostic and therapeutic evaluation. SDNS was defined as follows based on the therapeutic response: steroid therapy is impossible to discontinue because repeated over two times relapses appear after the reduction or discontinuation of steroid. These definitions were based on the clinical practice guidelines established for NS [21].
Statistical analysis
Clinical data have been presented as medians with interquartile ranges (IQR) or as numbers denoting percentages (%). Differences between groups were analyzed using the Wilcoxon rank-sum test (for continuous variables) or the Fisher exact test (for categorical variables). The paired t test was used to analyze changes in clinical parameters. The Kaplan–Meier method was used to evaluate the relapse and CD19+ cell reappearance after rituximab therapy. Statistical significance was set at a P value of < 0.05. All statistical tests were performed using the Stata software version 14.0 (Stata Corp LLC, College Station, TX, USA).
Results
Patient characteristics
Patients’ baseline characteristics are summarized in Table 1. The median age at the initiation of rituximab therapy was 43 years (IQR 30–49.5 years) with a predominance of women (62.5% of the patients). The median total number of relapses was 10.5 times (IQR 5.5–14.5 times), and the maximum number of relapses was 16. Regarding renal function, the median serum creatinine and eGFR were 0.69 mg/dL (IQR 0.61–0.99 mg/dL) and 76.7 mL/min/1.73 m2 (IQR 68.2–87.8 mL/min/1.73 m2), respectively. The median urinary protein was 0.10 g/gCr (IQR 0.02–0.42 g/gCr), and six of eight patients showed CR. PSL was administered in all patients at the initiation of rituximab therapy at a median dose of 22.5 mg/day (IQR 15–31.3 mg/day). CyA was also administered in all patients prior to the initiation of rituximab therapy. TAC, MZR, MMF, and CPA were the other immunosuppressive drugs that were administered.
Renal pathological findings
LM findings revealed no significant lesions including cellular proliferation and segmental sclerosis. IF showed nonspecific deposition of IgG or IgM in one and three cases, respectively. On EM, the effacement of foot process was confirmed and electron dense deposits were not observed. Based on these pathological findings, cases presented were finally diagnosed with MCNS by pathologists.
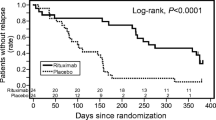
Relapse and reappearance of CD19+ cells after rituximab therapy
The clinical course of all patients with SDNS who were treated with rituximab has been summarized in Table 2. The median observation period was 13.9 months (IQR 11.6–20.0 months). Among eight patients included in the study, rituximab administration was repeated in two (patient # 1, 2). The number of infusions was 7 and 3, respectively, totaling 3100 mg and 1500 mg of rituximab, respectively. The remaining six patients received a single dose of rituximab (500 mg). Two patients (patient # 2, 5) did not demonstrate CR prior to rituximab treatment but achieved and maintained CR after treatment. We observed that three of eight (37.5%) patients showed relapse (patient # 6–8) during the observation period. The time until the onset of relapse after rituximab was 8.1, 10.0, and 13.6 months, respectively (Fig. 1). No relapse was observed in two patients in whom rituximab injections were repeated. The relapse rate was 50% at a median observation period of 13.0 months (IQR 10.3–14.9 months) in those who received a single dose of rituximab (500 mg). In three patients who relapsed after rituximab therapy, PSL dosage was temporarily increased to 15–30 mg/day. CR was confirmed 7 days (patient # 6), 14 days (patient # 7), and 21 days (patient # 8) after increasing steroid, and subsequently the second rituximab administration was carried out. CD19+ cells rapidly declined after rituximab therapy but reappeared in all patients. The median period until reappearance was 8.9 months (IQR 5.4–15.6 months) (Fig. 1). Restricted to the single-dose rituximab group, CD19+ cells reappeared with a median of 6.5 months (IQR 5.3–10.3 months). The reappearance of CD19+ cells was confirmed prior to relapse in two of three patients who showed relapse. The interval between reappearance and relapse was 3.3 and 4.9 months, respectively, in these patients. One patient showed an overlap between the reappearance of CD19+ cells and relapse. No patient demonstrated a relapse while the CD19+ cells were observed to be suppressed. In five patients (patient # 1–5), CR was maintained even after CD19+ cells reappeared. The number of relapses during a year prior to and after rituximab therapy was compared in six patients with observation period of more than 1 year. The median relapse times were decreased from 1 time/year (IQR 1–3 times/year) to 0 time/year (IQR 0–1 time/year) (P = 0.08) (Fig. 2).
Corticosteroid and immunosuppressive drugs
At the time of last observation, the corticosteroid dose could be reduced in 87.5% of patients. In 50%, the dose of PSL could be decreased to 5 mg or less, and steroid administration was discontinued in one patient. The median PSL dosage at the last visit was 5.5 mg/day (IQR 2.5–7 mg/day), which was significantly lower than that required prior to rituximab treatment (P < 0.01). CyA was used in seven of eight patients at the time of initiation of rituximab therapy at a median dose of 75 mg/day (IQR 75–150 mg/day). After rituximab administration, CyA could be reduced in all seven patients. Among these, CyA was discontinued in three. The dosage of CyA at the final observation time point was 25 mg/day (IQR 0–100 mg/day), which was significantly lower than that required prior to initiation of rituximab therapy (P < 0.01) (Fig. 3). Similarly, even in the single-dose group, a significant reduction in PSL and CyA dosages was observed from 20 mg/day (IQR 10–27.5 mg/day) to 6 mg/day (IQR 5–8 mg/day) (P = 0.03), and 87.5 mg/day (IQR 75–150 mg/day) to 25 mg/day (IQR 0–100 mg/day) (P < 0.01). MZR and MMF were being administered in one and two patients, respectively, at the time of initiation of rituximab therapy; however, both drugs could be discontinued. No patient reported using immunosuppressants other than CyA.
The corticosteroid- and cyclosporine-sparing effects of rituximab therapy. At the time of the last observation, the doses of corticosteroid and CyA required in patients with adult-onset SDNS were significantly decreased following rituximab therapy. The plus symbols show the median value. *P < 0.01. CyA cyclosporine, PSL prednisolone, SDNS steroid-dependent nephrotic syndrome
Adverse events
Adverse events noted during the observation period have are summarized in Table 3. Among the 19 rituximab infusions administered in 8 patients, infusion reaction of hypotension was observed in association with only 1 infusion (5.3%). This episode was mild and was managed with a decrease in the drip rate. Adverse events such as infectious diseases, progressive multifocal leukoencephalopathy, bone marrow suppression, mucocutaneous damage, pneumonopathy, liver dysfunction, gastrointestinal disorder, nephrotoxicity, and malignant neoplasm were not observed during the observation period.
Discussion
Rituximab has been recognized as a novel therapeutic agent to treat idiopathic NS. Several reports have demonstrated the efficacy of rituximab in pediatric patients for the management of SDNS or FRNS, which is primarily categorized as MCNS [7,8,9,10,11]. Randomized controlled trials have already been performed involving children with SDNS, and the effectiveness of this drug has been demonstrated [12, 13]. Iijima et al. have reported a multicenter, double-blind, randomized, placebo-controlled trial in Japan [14] demonstrating that among 48 pediatric patients with SDNS or FRNS, relapses were significantly decreased in the rituximab-treated group compared to a placebo group. However, few studies have described adult SDNS [15,16,17,18,19,20].
In this cohort study, we showed that rituximab reduced the frequency of relapses. The characteristics of this study are that all subjects were limited to adult-onset SDNS, and in most patients, the clinical course was observed after a single-dose infusion of rituximab. Despite the majority of patients were treated with a single dose of rituximab, the relapse rate was 37.5%, which is comparable with previous reports [15, 16, 18, 19]. The treatment of idiopathic NS is associated with various adverse effects secondary to the long-term use of corticosteroid and immunosuppressive drugs. Notably, rituximab treatment for adult-onset SDNS enables reduction in the required doses of steroid and immunosuppressants.
Usually, relapses are observed to occur after the reappearance of CD19+ cells in the patient’s blood; however, previous reports have shown that a few patients did not show relapse even after the reappearance of B cells [15, 16]. In all our patients, CD19+ cells were depleted immediately after rituximab administration. However, even after they reappeared in all patients, the relapse rate remained 37.5%. In 2 out of 3 patients who showed relapse, CD19+ cells had been observed to reappear prior to confirmation of relapse suggesting that the reappearance of B cells can be a predictive marker of relapse. In contrast, similar to previous reports, a few patients did not demonstrate relapse even after the reappearance of B cells. Ruggenenti et al. [16] have recommended that it is important to disrupt the activity of pathogenic autoreactive B lymphocyte clones. Based on these findings, it is necessary to further investigate whether B cell-target therapy would be a valid intervention in this context. The pathomechanism contributing to the action of rituximab on B lymphocytes to effectively treat idiopathic NS remains unclear, although this is hypothesized to be the primary pathology of T lymphocyte-related disorders and permeability factors. It has been hypothesized that targeting and removing B cells indirectly interferes with the activity of immunoregulatory cells such as regulatory T cells, natural killer cells, and macrophages [23]. Another pathomechanism suggested by Fornoni et al. indicates that rituximab might promote the stabilization of the podocyte cytoskeleton and prevent apoptosis, through interaction with glomerular epithelial cells [24], thus indicating that the role of rituximab in the management of SDNS is not attributable to only the removal of B cells. Therefore, a few patients maintain remission despite the reappearance of CD19+ cells, suggesting individual differences in the effect of rituximab irrespective of B cell depletion.
To date, the optimal dosing regimen for rituximab therapy to treat SDNS has not been established. Munyentwali et al. [15] reported no relationship between the dose of rituximab and relapse. Our results showed that a few patients maintained remission even with a small dose of rituximab. Further studies are needed to determine whether applied dose complying with non-Hodgkin’s lymphoma, re-treatment following the reappearance of B lymphocytes, or prophylactically repeated administration would be effective treatment methods. Treatment with single-dose rituximab therapy is beneficial in minimizing the risk of infusion reactions and reducing the frequency of hospitalizations and medical expense. Moreover, exposure to small quantities of rituximab reduces the possibility of antibody production and facilitates re-treatment.
It has not been determined whether CR should be achieved at the time of initiation of rituximab infusion to prevent the loss of rituximab in the urine. In our cohort, two patients did not achieve CR, but eventually showed a favorable course. Thus, it may not be necessary to achieve CR at the onset of rituximab treatment. The fact that rituximab is effective in treating nephrotic MN supports this conclusion.
Regarding adverse events, although mild infusion reaction was observed, no serious events were noted. High tolerability is considered a major advantage of rituximab treatment.
Limitations of our study: (1) the lack of a control group and the small number of patients studied would count as a limitation. However, adult-onset SDNS is a rare disease entity, and the number of patients affected is not large. In this cohort, all patients with adult-onset SDNS treated with rituximab at our hospital were enrolled in this study, thereby reducing the selection bias. (2) The observation period was relatively short and long-term observation is necessary to investigate the utility of single-dose rituximab therapy.
In conclusion, we observed that rituximab treatment for SDNS reduced the number of relapses, as well as the corticosteroid and immunosuppressant dosages required in these patients, not only in childhood-onset but also in adult-onset SDNS. Our study showed that in a few patients, relapse was suppressed despite the reappearance of B cells following single-dose rituximab therapy. Considering the safety, medical costs, and anti-drug antibody formation, it would be beneficial to reduce the dosage of rituximab as much as possible. Further investigations are needed to develop an optimal treatment regimen and to determine predictive factors associated with a therapeutic response.
References
Fujimoto S, Yamamoto Y, Hisanaga S, Morita S, Eto T, Tanaka K. Minimal change nephrotic syndrome in adults: response to corticosteroid therapy and frequency of relapse. Am J Kidney Dis. 1991;17:687–92.
Nakayama M, Katafuchi R, Yanase T, Ikeda K, Tanaka H, Fujimi S. Steroid responsiveness and frequency of relapse in adult-onset minimal change nephrotic syndrome. Am J Kidney Dis. 2002;39:503–12.
Sato M, Takei T, Moriyama T, Itabashi M, Nitta K. Long-term outcomes of initial therapy for idiopathic membranous nephropathy. Clin Exp Nephrol. 2017;21:842–51.
Ruggenenti P, Cravedi P, Chianca A, Perna A, Ruggiero B, Gaspari F, et al. Rituximab in idiopathic membranous nephropathy. J Am Soc Nephrol. 2012;23:1416–25.
Katsuno T, Ozaki T, Kim H, Kato N, Suzuki Y, Akiyama S, et al. Single-dose rituximab therapy for refractory idiopathic membranous nephropathy: a single-center experience. Intern Med. 2017;56:1679–86.
Iijima K, Sako M, Nozu K. Rituximab for nephrotic syndrome in children. Clin Exp Nephrol. 2017;21:193–202.
Benz K, Dötsch J, Rascher W, Stachel D. Change of the course of steroid-dependent nephrotic syndrome after rituximab therapy. Pediatr Nephrol. 2004;19:794–7.
Guigonis V, Dallocchio A, Baudouin V, Dehennault M, Hachon-Le Camus C, Afanetti M, et al. Rituximab treatment for severe steroid- or cyclosporine-dependent nephrotic syndrome: a multicentric series of 22 cases. Pediatr Nephrol. 2008;23:1269–79.
Kamei K, Ito S, Nozu K, Fujinaga S, Nakayama M, Sako M, et al. Single dose of rituximab for refractory steroid-dependent nephrotic syndrome in children. Pediatr Nephrol. 2009;24:1321–8.
Sellier-Leclerc AL, Macher MA, Loirat C, Guérin V, Watier H, Peuchmaur M, et al. Rituximab efficiency in children with steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2010;25:1109–15.
Kemper MJ, Gellermann J, Habbig S, Krmar RT, Dittrich K, Jungraithmayr T, et al. Long-term follow-up after rituximab for steroid-dependent idiopathic nephrotic syndrome. Nephrol Dial Transplant. 2012;27:1910–5.
Ravani P, Magnasco A, Edefonti A, Murer L, Rossi R, Ghio L, et al. Short-term effects of rituximab in children with steroid- and calcineurin-dependent nephrotic syndrome: a randomized controlled trial. Clin J Am Soc Nephrol. 2011;6:1308–15.
Ravani P, Rossi R, Bonanni A, Quinn RR, Sica F, Bodria M, et al. Rituximab in children with steroid-dependent nephrotic syndrome: a multicenter, open-label, noninferiority, randomized controlled trial. J Am Soc Nephrol. 2015;26:2259–66.
Iijima K, Sako M, Nozu K, Mori R, Tuchida N, Kamei K, et al. Rituximab for childhood-onset, complicated, frequently relapsing nephrotic syndrome or steroid-dependent nephrotic syndrome: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet. 2014;384:1273–81.
Munyentwali H, Bouachi K, Audard V, Remy P, Lang P, Mojaat R, et al. Rituximab is an efficient and safe treatment in adults with steroid-dependent minimal change disease. Kidney Int. 2013;83:511–6.
Ruggenenti P, Ruggiero B, Cravedi P, Vivarelli M, Massella L, Marasà M, et al. Rituximab in steroid-dependent or frequently relapsing idiopathic nephrotic syndrome. J Am Soc Nephrol. 2014;25:850–63.
Iwabuchi Y, Takei T, Moriyama T, Itabashi M, Nitta K. Long-term prognosis of adult patients with steroid-dependent minimal change nephrotic syndrome following rituximab treatment. Medicine (Baltim). 2014;93:e300.
Guitard J, Hebral AL, Fakhouri F, Joly D, Daugas E, Rivalan J, et al. Rituximab for minimal-change nephrotic syndrome in adulthood: predictive factors for response, long-term outcomes and tolerance. Nephrol Dial Transplant. 2014;29:2084–91.
Bruchfeld A, Benedek S, Hilderman M, Medin C, Snaedal-Jonsdottir S, Korkeila M. Rituximab for minimal change disease in adults: long-term follow-up. Nephrol Dial Transplant. 2014;29:851–6.
Takei T, Itabashi M, Moriyama T, Kojima C, Shiohira S, Shimizu A, et al. Effect of single-dose rituximab on steroid-dependent minimal-change nephrotic syndrome in adults. Nephrol Dial Transplant. 2013;28:1225–32.
Nishi S, Ubara Y, Utsunomiya Y, Okada K, Obata Y, Kai H, et al. Evidence-based clinical practice guidelines for nephrotic syndrome 2014. Clin Exp Nephrol. 2016;20:342–70.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
van den Berg JG, Weening JJ. Role of the immune system in the pathogenesis of idiopathic nephrotic syndrome. Clin Sci (Lond). 2004;107:125–36.
Fornoni A, Sageshima J, Wei C, Merscher-Gomez S, Aguillon-Prada R, Jauregui AN, et al. Rituximab targets podocytes in recurrent focal segmental glomerulosclerosis. Sci Transl Med. 2011;3:85ra46.
Acknowledgements
This study was supported partly by a Grant-in-Aid for Progressive Renal Diseases Research, and Research on Rare and Intractable Disease, from the Ministry of Health, Labour and Welfare of Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The Department of Nephrology and Rheumatology, Aichi Medical University received research promotion grants from Chugai Pharmaceutical Co., Ltd., Daiichi Sankyo Co., Ltd., Eisai Co., Ltd., Kyowa Hakko Kirin Co., Ltd., Mitsubishi Tanabe Pharma Co., Novartis Pharma K.K., Otsuka Pharmaceutical Co., Ltd., Pfizer Japan Inc., Takeda Pharmaceutical Co., Ltd., Teijin Pharma Limited., and Torii Pharmaceutical Co., Ltd. The Department of Nephrology, Nagoya University Graduate School of Medicine received research promotion grants from Astellas Pharma Inc., Bristol-Myers Squibb., Chugai Pharmaceutical Co., Ltd., Daiichi Sankyo Co., Kissei Pharmaceutical Co., Ltd., Kowa Pharmaceutical Co., Ltd., Kyowa Hakko Kirin Co., Ltd., Mitsubishi Tanabe Pharma Co., Mochida Pharmaceutical Co., Ltd., MSD K.K., Nippon Boehringer Ingelheim Co., Ltd., Novartis Pharma K.K., Otsuka Pharmaceutical Co., Ltd., Pfizer Japan Inc., Takeda Pharmaceutical Co., Ltd., Teijin Pharma Limited., Torii Pharmaceutical Co., Ltd., and Sumitomo Dainippon Pharma Co., Ltd.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of The Ethics Committee for Human Research of Nagoya University Hospital at which the studies were conducted (IRB approval number 2017-0192) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The Ethical Committee approved this retrospective cohort study without written informed consent from patients; however, informed consent was obtained from most patients at the time of performing a renal biopsy.
About this article
Cite this article
Katsuno, T., Masuda, T., Saito, S. et al. Therapeutic efficacy of rituximab for the management of adult-onset steroid-dependent nephrotic syndrome: a retrospective study. Clin Exp Nephrol 23, 207–214 (2019). https://doi.org/10.1007/s10157-018-1630-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-018-1630-y