Abstract
Background
As lung impairment is an indicator of increased morbidity and mortality in patients receiving continuous ambulatory peritoneal dialysis (CAPD), the risk factors associated with impaired lung function are of great significance. The aim of this study is to elucidate the effects of inflammatory biomarkers and dialysis adequacy on pulmonary function, in CAPD patients.
Methods
101 patients undergoing CAPD, 30 CKD5 patients and 30 healthy subjects were enrolled. Spirometry and serum biomarkers were evaluated in each subject. Pulmonary function was compared among patients and control groups. Pearson analysis was used to analyze the correlation between serum biomarkers, dialysis adequacy and pulmonary function.
Results
Lower vital capacity, maximal voluntary ventilation (MVV), forced vital capacity (FVC), peak expiratory flow (PEF), maximal mid-expiratory flow rate (MMEF), and diffusing capacity of the lung for carbon monoxide (DLCO) were observed in the CAPD group (all P < 0.05) when compared with control subjects. DLCO % was negatively correlated with CRP (r = −0.349, P = 0.007) and positively correlated with albumin (r = 0.401, P = 0.002). Total Kt/V was associated positively with MMEF % (r = 0.316, P = 0.019), and MVV % (r = 0.362, P = 0.007). nPNA was positively correlated with FVC % (r = 0.295, P = 0.049) and MMEF % (r = 0.381, P = 0.010).
Conclusion
The results suggest that lung function decline was directly related to higher CRP level, hypoalbuminemia, and dialysis inadequacy. These findings provide the evidence that inflammation and dialysis adequacy play a role in predicting outcomes of CAPD patients with pulmonary impairment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Continuous ambulatory peritoneal dialysis (CAPD) is an important treatment for end-stage renal disease (ESRD), which may affect virtually every system and commonly involves the lungs [1]. Patients undergoing dialysis are exposed to continuous pulmonary injuries from multifactorial origin, such as hormonal and metabolic derangement associated with ESRD. This may induce pulmonary vascular alterations and airway resistance. As low lung function is an indicator of increased morbidity and mortality, the risk factors associated with impaired lung function are of great importance. Approximately 30–50 % of patients with ESRD have elevated serum levels of C-reactive protein (CRP), a marker of systemic inflammation [2, 3]. CRP has been identified as an index of chronic inflammation in patients receiving dialysis. Investigators have found that cardiovascular diseases are related directly to high CRP levels and inflammation is an important risk factor for lung impairment in patients receiving CAPD [4, 5]. Dialysis adequacy is also important for patients undergoing CAPD, as inadequacy induces volume overload and malnutrition, followed by lung deficits. Thus, the purpose of our study is to investigate the correlation between inflammatory biomarkers, dialysis adequacy and lung function in patients receiving CAPD.
Materials and methods
Patients
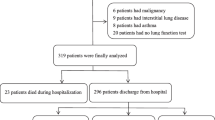
The study sample comprised 101 patients who had undergone CAPD in the nephrology department of the First Affiliated Hospital of Anhui Medical University from April 2012 toMarch 2013. The inclusion criteria were >2 months of CAPD. The study excluded subjects aged >70 years, those currently using drugs affecting the lung and respiratory muscles, those with chronic bronchitis, bronchial asthma, interstitial lung disease, pulmonary tuberculosis, history of chronic chest and lung inflammation, active lung infection, and those developing peritoneal dialysis–related peritonitis within 1 month. Control groups were classified into two, respectively 30 healthy subjects selected from outpatient medical centers, and 30 patients in chronic kidney disease stage 5 (CKD5) who had not received CAPD therapy. The 3 groups were basically equivalent regarding the subjects’ sex, age, and hypertension.The protocol was approved by the medical ehtics committee of the first affiliated hospital of Anhui Medical University, and the approval number was AF/SC-08/02.0.
Treatment protocol
All patients had CAPD with 1.5–2.5 % dextrose solution (Baxter), three to five dwell periods, and 6–10 L total volume, according to the type of dialysis membrane transport and clinical symptoms. Following routine procedure, peritoneal dialysate was preserved for 4–6 h in each dwell period. All patients were treated with necessary medications, i.e. antihypertensive drugs (Nitrendipine, nifedipine, amlodipine, felodipine, urapidil, Metoprolol), erythropoietin, calcium, vitamin D. No antibiotic was used in the patients.
Spirometric assessment
Standardized pulmonary function tests were performed with a spirometer (MS-IOS; Jaeger, Germany). The following measurements were obtained: vital capacity (VC) and forced vital capacity (FVC); maximal voluntary ventilation (MVV); forced expiratory volume in the first second (FEV1); peak expiratory flow (PEF); maximal mid-expiratory flow rate (MMEF); and diffusing capacity of the lung for carbon monoxide (DLCO). Values were calculated as % predicted using appropriate normal values for each patient’s sex, age, height, and weight.
Detection of serum biomarkers
Blood samples were collected in the morning. Serum levels of C-reactive protein (CRP), ferritin (Fer), and albumin were assessed with a modular automatic biochemical analyzer (Roche). Erythrocyte sedimentation rates (ESRs) were measured using an automatic ESR analyzer (Vital Diagnostics s.r.l., Italy).
Assessment of residual renal function, overnight urea clearance, and creatinine clearance
The adequacy of dialysis was assessed by measuring total, peritoneal, and renal urea clearance indices (Kt/Vs) and creatinine clearance rate (CCR). Peritoneal components of these parameters were estimated from 24-h effluent dialysate on the examination day, and renal components were estimated from 24-h urine collection. Total Kt/V values were calculated using the standard method recommended in the kidney disease outcomes quality initiative guidelines [6]. nPNA was calculated according to Bergström et al. [7, 8]. and normalized to standard body weight (VWatson/0.58) using the following equation: Normalized protein equivalent of nitrogen appearance rate, nPNA (g/kg/day) = [13 + 0.204 × urea appearance (mmol/day) + protein loss (g/day)]/(VWatson/0.58).
Statistical analyses
Continuous variables were reported as means ± standard deviations. Categorical variables were reported as proportion. Independent sample t test was used to compare the differences for two groups. ONE WAY ANOVA was used to compare the differences inthree groups. Chi square test was performed to compare the difference for categorical variables. A P value < 0.05 was considered to indicate statistical significance. Pearson correlation analysis was used to determine associations between biomarker values and FEV1 and FVC. All analysis was performed using SPSS software (version 12.0).
Results
Characteristics and PFT of the study population
A total of 101 patients (47 mens, 54 womens; mean age, 44.95 ± 11.79 years) having received CAPD were enrolled in this study. Patients had undergone dialysis for a mean of 10.5 months. Table 1 presents characteristics of the study population and etiology of renal failure.
Table 2 shows differences in lung function values between patients having had CAPD and control subjects. It’s found that VC, FVC, FEV1, PEF, MMEF, MVV, and DLCO % were significantly lower in CAPD patients than in healthy subjects (all P < 0.05), but there was no significant difference in VC, FVC, or FEV1 % between CAPD patients and CKD5 patients. These results indicated that CAPD therapy, by itself, did not affect the pulmonary ventilation function. However, DLCO % was lower in CAPD patients than in CKD5 patients.
Biomarkers, dialysis indices, and pulmonary function
Table 3 shows the relationship between biomarkers and pulmonary function. There are no positive or negative association of %VC, %FVC, MVV, FEV1.0, PEF, MEF, DLCO with Fer, ESR, urine volume and cardia-thoracic ratio, CRP have negative relationship with DLCO and PEF %, Relationship between dialysis indices and pulmonary function are showed in Table 4 shows. Renal Kt/v was positive associated with %VC, FEV1.0 and DLCO. There are no positive or negative association of %VC, %FVC, MVV, FEV1.0, PEF, MEF, DLCO with peritoneal Kt/v, total CCR, peritoneal CCR, renal CCR, rGFR.
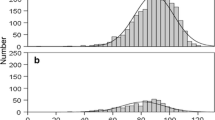
Pearson correlation analysis showed that CRP was associated negatively with DLCO % (r = −0.349, P = 0.007), and PEF % (r = −0.364, P = 0.006) meahwhile total Kt/V was associated positively with MMEF % (r = 0.316, P = 0.019), and MVV % (r = 0.362, P = 0.007). Normalized protein equivalent of nitrogen appearance rate (nPNA) was positively correlated with FVC % (r = 0.295, P = 0.049) as well as serum albumin was positive correlated with DLCO % (r = 0.401, P = 0.002) (Fig. 1).
Associations of pulmonary function with serum biomarkers and dialysis indices in patients undergoing peritoneal dialysis (R value). DLCO % was negatively correlated with CRP (r = −0.349, P = 0.007) and positively correlated with albumin (r = 0.401, P = 0.002). PEF % was negatively correlated with CRP (r = 0.364, P = 0.006). Total Kt/V was associated positively with MMEF % (r = 0.316, P = 0.019), and MVV % (r = 0.362, P = 0.007). nPNA was positively correlated with FVC % (r = 0.295, P = 0.049)
The PFT differences between the patients according to the CRP, Alb and total Kt/V
Pearson correlation analysis showed that CRP was associated negatively with DLCO % (r = −0.349, P = 0.007), and PEF % (r = −0.364, P = 0.006) meahwhile total Kt/V was associated positively with MMEF % (r = 0.316, P = 0.019), and MVV % (r = 0.362, P = 0.007). Normalized protein equivalent of nitrogen appearance rate (nPNA) was positively correlated with FVC % (r = 0.295, P = 0.049) as well as serum albumin was positive correlated with DLCO % (r = 0.401, P = 0.002) (Fig. 1).
Among CAPD patients, VC, FVC, PEF and DLCO % values were higher in those with serum CRP levels <10 mg/l than in those with CRP levels ≥10 mg/l, and DLCO % was higher in those with serum albumin levels ≥35 g/l than in those with albumin levels <35 g/l (both P < 0.05; Table 5). No parameter differed significantly according to serum ferritin level or ESR.
According to dialysis indices, patients with Kt/V values ≥1.7 had higher MMEF, and MVV % than those with Kt/V values <1.7 (all P < 0.05). Patients with residual glomerular filtration rates (rGFRs) ≥1 ml/min had higher DLCO % than those with rGFRs <1 ml/min (both P < 0.05). FVC, PEF, MMEF, and MVV % were higher in patients with nPNA ≥1 g/kg days than in those with nPNA <1 g/kg days (all P < 0.05; Table 6).
Discussion
It is well-known that a number of respiratory complications occur in patients with chronic renal failure (CRF). Common expressions of the uraemic lung are pulmonary edema, fibrosis, pulmonary hypertension, haemosiderosis and pleural effusion. In the present study, we observed overall significant pulmonary deficits in CAPD patients. Having ruled out suchconfounding factors assex, age, and smoking, we detected that lung function was worse in CAPD patients when compared with control subjects. This detection was consistent with previous study [9]. Serum albumin of CAPD and CKD5 patients were less than normal,suggesting that Uremic patients usually had hypoalbuminemia. However,there were no significant differencesin age,blood pressure and sex ratio among three groups.
We demonstrated for the first time that lung function decline was associated with inflammation, dialysis inadequacy and thus provided evidence for physicians to prevent reduced lung functionin CAPD patients. To the best of our knowledge, this is the first study to address the relationship between inflammation, dialysis adequacy and pulmonary dysfunction in PD patients. CRP is produced by human hepatocytes in response to inflammation, infection, or tissue damage.In the normal population, CRP is present at very low levels. Levels <1 mg/dl are considered insignificant, Levels from 1 to 10 mg/dl are considered moderately elevated, and levels >10 mg/dl are markedly elevated so 10 mg/l has been seen as the cut off value for CRP. In our study, VC, FVC, PEF, and DLCO % were significantly lower in patients with elevated serum CRP levels, and that CRP levels were correlated negatively with DLCO and PEF %, which coincided with previously reported inverse cross-sectional associations between CRP and spirometric measures of lung function (FEV1 and FVC) [10–13]. The observed association between CRP and lung function was also in consistence with data from several longitudinal studies documenting an association between the rate of FEV1 decline and CRP level [14, 15]. Some researchers further noted an inverse relationship between CRP level and FEV1 in adults aged 26–32 years [10], and a high CRP level at the age of 20 years was also found to be associated with greater declines in FEV1 and FVC measured at the age of 29 years [16]. However, theage ranges in these studies were markedly different from our study samples, andCRP level varied with age and ethnicity. In this way, our study further proved and complemented their finding. Further evidence of a link between systemic inflammation and pulmonary impairment has been reported in the form of an attenuation of pulmonary function decline attributable to statins, which may have inflammatory effects [17]. Poor lung function has also been found to be related to CRP level, leukocyte count, and vascular cell adhesion molecule 1 level [18]. Similarly, elevated CRP and fibrinogen levels and leukocyte counts in individuals with chronic obstructive pulmonary disease (COPD) were associated with increased risk of COPD exacerbation [19]. Longitudinal observational evidence has suggested that increases in systemic inflammation are associated with declines in lung function [20].
Current hypotheses state that the increased CRP reflects the severity of an “inflammatory state,” in dialysis patients, the inflammation can be caused by dialysis itself.An abnormally elevated serum high-sensitivity C-reactive protein (hs-CRP) level can cause airway epithelial cell damage and a decline in pulmonary function [21]. In patients with COPD, serum hs-CRP levels are in proportion todisease severity and thus are negatively correlated with patients’ condition [22]. Proinflammatory cytokines cause inflammation, triggering the ubiquitin–proteasome channel to break down proteins, and thereby causing muscle loss. This process potentially results in lung damage in patients with chronic renal failure. CRP may contribute to persistent obstruction of proximal pulmonary arteries in chronic thromboembolic pulmonary hypertension by promoting vascular remodeling, endothelial dysfunction, and in situ thrombosis [23].
Our data also demonstrated the lung damage occurred in CAPD patients with declining residual renal function and inadequate dialysis. MMEF, and MVV % were higher in patients with Kt/V values ≥1.7 than the other patients. DLCO % were higher in patients with residual glomerular filtration rates (rGFRs) ≥1 ml/min than in those with rGFRs <1 ml/min. Residual renal function decline resulted in volume overload and increased pulmonary capillary hydrostatic pressure in these patients. Increased vascular permeability, fluid overload, and low serum albumin concentration are favorable conditions for pulmonary edema in the patients with acute kidney injury [24]. Uremic pulmonary edema may have progressed to interstitial fibrosis, which in turn can lead to thickening of the alveolar capillary membrane [25], affecting pulmonary diffusion and causing airway obstruction. On the other hand the negative correlation between RRF and CRP suggested that a reduction in renal function aggravated the inflammatory state through retention of pro-inflammatory mediators. Renal failure was associated with increases in inflammatory mediators, including CRP and interleukin 6, which could be the result of increased monocyte activation or impaired clearance of inflammatory mediators.
Furthermore, the most common pathological condition of the lungs in chronic renal failure is pulmonary edema, usually due to a combination of fluid overload and abnormal permeability of the pulmonary circulation. Volume overload is a common problem in patients undergoing peritoneal dialysis and may contribute to the high cardiac mortality in this population [26–28]. Lung congestion is a relevant factor in the poor physical functioning of CKD-5D patients. Reducing asymptomatic lung congestion may translate into improved physical functioning in PD patients [29]. Inflammatory response and accumulation of proinflammatory cytokines have been found to contribute to muscle wasting by stimulating protein catabolism via the ubiquitin–proteasome pathway. This process may also affect respiratory muscles, potentially contributing to impaired pulmonary function in patients receiving CAPD [30].
Another important prognostic indicator is serum albumin level in CAPD patients. Our study showed that DLCO % was positively correlated with this indicator. Other investigators found that albumin levels <4.1 mg/dl predicted low FEV1 [31]. Hypoalbuminemia is acommon complication in PD patients and the causes of hypoalbuminemia are complex such as malnutrition, aging, excess protein loss through the peritoneal membrane, ultrafiltration failure, and systemic inflammation [32, 33]. Hypoalbuminemia reduces plasma colloid osmotic pressure. Fluid retention and left ventricular dysfunction induce an increase in pulmonary intravascular hydrostatic pressure, resulting in pulmonary interstitial edema. Pulmonary interstitial edema increases the diffuse distance, pulmonary fibrosis and anemia decreases the gas-diffusing capacity, causing a reduction in hemoglobin-carried oxygen. Furthermore, because pulmonary diffusion capacity decreases pulmonary ventilation, lung function is affected.
In conclusion, our results suggest that pulmonary decline is associated with chronic inflammation and hypoproteinemia. Dialysis inadequacy and the loss of residual renal function also contribute to the development of pulmonary dysfunction. In one word, inflammation, dialysis inadequacy and hypoproteinemia are risk factors of pulmonary impairment in CAPD patients, clinicians should seek to keep away from chronic inflammation and malnutrition, enhance dialysis adequacy, and delay the loss of residual renal function, so that pulmonary ventilation can be improved and ventilatory dysfunction avoided, and eventually better patient outcomes achieved.
This study does have some limitations. It was conducted on a small selection of CAPD patients at one center, limiting the generalizability of our findings. Expansion of the sample size and the inclusion of patients from multiple centers would have produced more convincing results. Further research is needed on treatments to prevent morbidity and mortality in patients with respiratory disorders.
Abbreviations
- CAPD:
-
Continuous ambulatory peritoneal dialysis
- CGN:
-
Chronic glomerulonephritis
- DN:
-
Diabetic nephropathy
- RPGN:
-
Rapidly progressive glomerulonephritis
- CIN:
-
Chronic interstitial nephritis
- NS:
-
Nephrotic syndrome
- VRKD:
-
Vasculitis-related kidney damage
- PD:
-
Peritoneal dialysis
- ESRD:
-
End-stage renal disease
- CRP:
-
C-reactive protein
- VC:
-
Vital capacity
- FVC:
-
Forced vital capacity
- MVV:
-
Maximal voluntary ventilation
- FEV1 :
-
Forced expiratory volume in the first second
- PEF:
-
Peak expiratory flow
- MMEF:
-
Maximal mid-expiratory flow rate
- DLCO:
-
Diffusing capacity of the lung for carbon monoxide
- Alb:
-
Albumin
- ESR:
-
Erythrocyte sedimentation rate
- Kt/V:
-
Renal urea clearance index
- CCR:
-
Creatinine clearance rate
- rGFR:
-
Residual glomerular filtration rate
- nPNA:
-
Normalized protein equivalent of nitrogen appearance rate
References
Turcios NL. Pulmonary complications of renal disorders. Paediatr Respir Rev. 2012;13:44–9.
Engstrom G, Lind P, Hedblad B, Wollmer P, Stavenow L, Janzon L, Lindgarde F. Lung function and cardiovascular risk—relationship with inflammation-sensitive plasma proteins. Circulation. 2002;106:2555–60.
Razeghi E, Parkhideh S, Ahmadi F, Khashayar P. Serum CRP levels in pre-dialysis patients. Ren Fail. 2008;30:193–8.
Balasubramanian VP, Varkey B. Chronic obstructive pulmonary disease: effects beyond the lungs. Curr Opin Pulm Med. 2006;12:106–12.
Sin DD, Man SFP. Systemic inflammation and mortality in chronic obstructive pulmonary disease. Can J Physiol Pharmacol. 2007;85:141–7.
II. NKF-K/DOQI Clinical practice guidelines for peritoneal dialysis adequacy: update 2000. Am J Kidney Dis. 2001; 37: S65–S136.
Bergstrom J, Furst P, Alvestrand A, Lindholm B. Protein and energy-intake, nitrogen-balance and nitrogen losses in patients treated with continuous ambulatory peritoneal-dialysis. Kidney Int. 1993;44:1048–57.
Bergstrom J, Heimburger O, Lindholm B. Calculation of the protein equivalent of total nitrogen appearance from urea appearance. Which formulas should be used? Perit Dial Int. 1998;18:467–73.
Tang X, Wang Y, Yang L, Yuan Y. The influence of peritoneal dialysis on the pulmonary function of patients with end-stage renal disease. J West China U Med Sci. 2002;33:123–46.
Hancox RJ, Poulton R, Greene JM, Filsell S, McLachlan CR, Rasmussen F, Taylor DR, Williams MJ, Williamson A, Sears MR. Systemic inflammation and lung function in young adults. Thorax. 2007;62:1064–8.
Bolton CE, Schumacher W, Cockcroft JR, Timpson NJ, Smith GD, Gallacher J, Rumley A, Lowe GD, Ebrahim S, Shale DJ, Ben-Shlomo Y. The CRP genotype, serum levels and lung function in men: the caerphilly prospective study. Clin Sci. 2011;120:347–55.
Jiang R, Burke GL, Enright PL, Newman AB, Margolis HG, Cushman M, Tracy RP, Wang Y, Kronmal RA, Barr RG. Inflammatory markers and longitudinal lung function decline in the elderly. Am J Epidemiol. 2008;168:602–10.
Shaaban R, Kony S, Driss F, Leynaert B, Soussan D, Pin I, Neukirch F, Zureik M. Change in C-reactive protein levels and FEV1 decline: a longitudinal population-based study. Resp Med. 2006;100:2112–20.
Olafsdottir IS, Gislason T, Gudnason V, Benediktsdottir B, Olafsson I, Aspelund T, Thjodleifsson B, Janson C. CRP is associated with lung function decline in men but not women: a prospective study. Resp Med. 2013;107:91–7.
Higashimoto Y, Iwata T, Okada M, Hiroaki S, Fukuda K, Tohda Y. Serum biomarkers as predictors of lung function decline in chronic obstructive pulmonary disease. Resp Med. 2009;103:1231–8.
Rasmussen F, Mikkelsen D, Hancox RJ, Lambrechtsen J, Nybo M, Hansen HS, Siersted HC. High-sensitive C-reactive protein is associated with reduced lung function in young adults. Eur Respir J. 2009;33:382–8.
Alexeeff SE, Litonjua AA, Sparrow D, Vokonas PS, Schwartz J. Statin use reduces decline in lung function—VA normative aging study. Am J Respir Crit Care Med. 2007;176:742–7.
Kuhlmann A, Olafsdottir IS, Lind L, Sundstrom J, Janson C. Association of biomarkers of inflammation and cell adhesion with lung function in the elderly: a population-based study. BMC Geriatr. 2013;13.
Thomsen M, Ingebrigtsen TS, Marott JL, Dahl M, Lange P, Vestbo J, Nordestgaard BG. Inflammatory biomarkers and exacerbations in chronic obstructive pulmonary disease. Jama J AM Med Assoc. 2013;309:2353–61.
Ahmadi-Abhari S, Kaptoge S, Luben RN, Wareham NJ, Khaw K-T. Longitudinal association of C-reactive protein and lung function over 13 Years The EPIC-norfolk study. Am J Epidemiol. 2014;179:48–56.
Feng J, Ni SS, Zhou J. Research of C-reactive protein and endothelial cell activation factor change in chronic obstructive pulmonary disease. Chin J Nauti Med Hyper. 2009;16:284–6.
Liu WJ, Liang R. Correlation study of detection of serumhs-CRP, TNF-α and IL-6 to lung function and life quality in COPD patients. J Clin Pulm Med. 2013;18:616–7.
Wynants M, Quarck R, Ronisz A, Alfaro-Moreno E, Van Raemdonck D, Meyns B, Delcroix M. Effects of C-reactive protein on human pulmonary vascular cells in chronic thromboembolic pulmonary hypertension. Eur Respir J. 2012;40:886–94.
Faubel S. Pulmonary complications after acute kidney injury. Adv Chronic Kidney Dis. 2008;15:284–96.
Feng C, Wang YJ, Tang H. Effects of hemodialysis on pulmonary function in patients with uremia. Med J West China. 2009;21:390–1.
Bloembergen WE. Cardiac disease in chronic uremia: epidemiology. Adv Ren Replace Ther. 1997;4:185–93.
Rubin LJ. Current concepts—primary pulmonary hypertension. N Engl J Med. 1997;336:111–7.
Tarrass F, Benjelloun M, Medkouri G, Hachim K, Benghanem MG, Ramdani B. Doppler echocardiograph evaluation of pulmonary hypertension in patients undergoing hemodialysis. Hemodial Int. 2006;10:356–9.
Giuseppe E, Rocco T, Vincenzo P, Claudia T, Maurizio G, Giovanni GB, Carmine Z. Pulmonary congestion and physical functioning in peritoneal dialysis patients. Perit Dialysis Int. 2012;32:531–53630.
Tao Y, Wang YJ, Yang SM. Measurement of respiratory excitability and respiratory muscle strength in uremic patients. China Pratic Med. 2001;3:4–6.
Souza dos Santos Simon MI, Drehmer M, de Abreu e Silva FA, Hoffmann A, Druck Ricachinewsky C, de Fonseca Andrade Procianoy E, Scattolin I, Saldanha Menna Barreto S. Association of nutritional status, plasma, albumin levels and pulmonary function in cystic fibrosis. Nutr Hosp. 2011; 26: 1322–27.
Cueto-Manzano AM, Espinosa A, Herna´ndez A, Correa-Rotter R. Peritoneal transport kinetics correlate with serum albumin but not with the overall nutritional status in CAPD patients. Am J Kidney Dis. 1997;30:229–36.
Shioya M, Yoshida T, Kasai K, Furuya R, Kato A, et al. Inflammatory factors for hypoalbuminemia in Japanese peritoneal dialysis patients. Nephrology. 2013;l8:539–544.
Acknowledgements
This study was supported by the project of Annual Research Project of Anhui Province (NO. 1208085QH172) and Key Lab of Geriatric molecular medicine of Anhui Province. We are grateful to Medjaden Bioscience Limited for assisting in the preparation of this manuscript. This study was also supported by the Natural Science Foundation of China (NO. 81170030, 81270082 and 81300027), National Education Ministry of China (NO. 20113420110006), Annual Research Project of Anhui Province (NO. 10021303028) and Key Lab of Geriatric molecular medicine of Anhui Province (1206c0805028).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Additional information
P. Zhang, H. -M. Wu, Q. -Y. Shen, X. -M. Qi contributed equally to this work.
About this article
Cite this article
Zhang, P., Wu, HM., Shen, QY. et al. Associations of pulmonary function with serum biomarkers and dialysis adequacy in patients undergoing peritoneal dialysis. Clin Exp Nephrol 20, 951–959 (2016). https://doi.org/10.1007/s10157-016-1244-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-016-1244-1