Abstract
Background
Evidence on early closure (EC) of defunctioning stoma (DS) after colorectal surgery shows a favorable effect when patients are carefully selected. Therefore, a clinical pathway adapted to the implementation of an EC strategy was developed in our center. The aim of this study was to carry out a comparative analysis of time until DS closure and DS-related morbidity before and after the implementation of an EC protocol (ECP).
Methods
This study is a before-and-after comparative analysis. Patients were divided into two cohorts according to the observational period: patients from the period before the ECP implementation (January 2015–December 2019) [Period 1] and those from the period after that (January 2020–December 2022) [Period 2]. All consecutive patients subjected to elective DS closure within both periods were eligible. Early closure was defined as the reversal within 30 days from DS creation. Patients excluded from EC or those not closed within 30 days since primary surgery were analyzed as late closure (LC). Baseline characteristics and DS-related morbidity were recorded.
Results
A total of 145 patients were analyzed. Median time with DS was shorter in patients after ECP implementation [42 (21–193) days versus 233 (137–382) days, p < 0.001]. This reduction in time to closure did not impact the DS closure morbidity and resulted in less DS morbidity (68.8% versus 49.2%, p = 0.017) and fewer stoma nurse visits (p = 0.029).
Conclusions
The ECP was able to significantly reduce intervals to restoration of bowel continuity in patients with DS, which in turn resulted in a direct impact on the reduction of DS morbidity without negatively affecting DS closure morbidity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The creation of a defunctioning stoma (DS), in most cases an ileostomy, is virtually a routine surgical practice in the context of risky colorectal anastomoses to minimize the adverse effects and severity of a potential anastomotic leak (AL) [1, 2]. However, this protective effect has a number of important drawbacks that must be properly balanced in each patient: morbidity secondary to the time the patient remains with the stoma (dermatitis, peristomal hernia, and hydro-electrolyte disturbances), morbidity attributable to DS reconstruction surgery [3], worsened functional outcomes after rectal cancer surgery with total mesorectal excision (TME) [4], costs of medical care and care devices [5], and direct impact on patient’s quality of life [6].
All these deleterious effects of DS may be directly dependent on the duration the ileostomy remains in place [7, 8]. Despite this, in many institutions the duration of DS remains long and most patients end up keeping it for at least 9 months; moreover, it is not uncommon that DS remains in place beyond 12 months or even becomes permanent because of progressive patient deterioration [3, 9].
Some of the reasons for this could be the high burden of care, the fear of delaying the administration of adjuvant treatments in patients with cancer [10, 11], the absence of standard definition of early closure (EC) [12], the existence of controversial data regarding its use, and the absence of clinical guidelines favorable to its implementation [13, 14]. Nevertheless, an in-depth review of the literature shows evidence favorable to EC use when patients are carefully selected and it is applied in centers and units specialized in colorectal surgery [15, 16].
On the basis of this favorable evidence, a clinical pathway was designed in our center for the safe implementation of an EC strategy, the Early Stoma Closure Clinical Protocol (ECP). ECP was developed to standardize the management and care of all patients with DS, enabling the safe selection of candidates for EC, defined as reversal within 30 days after stoma creation. The aim of this study was to carry out a comparative analysis of the time until DS closure as well as DS-related morbidity between the periods before and after the implementation of this protocol.
Materials and methods
Study design and patients
This study is a before-and-after comparative analysis conducted at a single tertiary hospital. Patients in this observational study were divided into two cohorts according to different study periods: the period before the implementation of the ECP (January 2015–December 2019) [Period 1] and the period after that (January 2020–December 2022) [Period 2]. Patients from Period 2 were prospectively collected and compared with patients from Period 1, who were retrospectively collected as a historical cohort. The local ethics committee approved our protocol and written informed consent for participation in the study was obtained from all prospectively recruited patients. The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
All consecutive adult patients subjected to elective DS closure between January 2015 and December 2022 were included in the study. Patients who underwent conversion to end-colostomy/end-ileostomy or abdominoperineal resection during DS reversal were excluded.
Early stoma closure clinical protocol
ECP is a multidisciplinary protocol implemented in our center since January 2020 to guide the selection of suitable patients for EC and standardize the assessment of colorectal anastomosis before DS closure. This pathway has a dedicated coordinator to achieve a timely assessment of the anastomosis and subsequent scheduling of closure in those patients eligible for EC. In addition, experienced stoma nurses who provide diligent follow-up and management for stoma patients were incorporated in our unit. Requirements for EC according ECP are summarized in Fig. 1
Regarding the primary surgery, an EC procedure was recommended exclusively for selected patients who underwent DS due to rectal oncological surgery, diverticular disease, or Hartmann’s reconstruction. Patients who required DS after inflammatory bowel disease (IBD) surgery or as management for anastomotic leak (AL) were not eligible for EC.
After the selected primary surgery, these patients were clinically and analytically assessed by a colorectal surgeon from day 1 to day 7 to ensure that there were no clinical signs of AL. Laboratory tests, including determination of white blood cell counts (WBC), C-reactive protein (CRP), and lactate levels, were performed on postoperative days (POD) 2 and 4 to assess inflammatory status. Patients were also non-eligible for EC if the recovery from their index surgery was complicated by one or more of the following events: AL, sepsis, or organ failure. All patients without any adverse event had a rectal examination, and a computed tomography enema (CTE) was performed from days 7–14 after stoma creation to check the integrity of the anastomosis. This contrast study is usually carried out during admission for the primary surgery or is scheduled at discharge. Gastrographin© is instilled by a colorectal surgeon using a Foley catheter placed in the rectum just below the anastomosis. CTE is always assessed by a radiologist and a colorectal surgeon. If there was a leak of contrast outside the rectum or any AL sign, the patient was not selected for EC. Otherwise, patients were scheduled for DS closure before any clinic appointments.
Stoma closure was performed under general anesthesia with a peristomal skin incision. After small bowel mobilization, a hand-sewn or stapled anastomosis was performed at the discretion of the surgeon responsible for the case, on the basis of their own preferences, intraoperative conditions of the patient, and the bowel limb where the ileostomy was set. The wound was partially closed with a purse string according to current evidence [17].
Patients excluded from EC or not closed within 30 days since primary surgery were analyzed as late closure (LC).
Outcomes and definitions
Primary outcome was the time until closure before and after ECP implementation. Secondary outcome was DS-related morbidity in both periods.
Patient demographic data, comorbidities, primary surgery details such as emergency indication, postoperative complications, DS-related morbidity, hospital readmissions, and visits to stoma nurse consultation were collected.
-
Primary surgery was defined as any elective or emergent colorectal resection that involved the creation of a DS, either directly after resection or as management of AL requiring a reintervention.
-
DS morbidity: morbidity associated with DS management (during and after admission for primary surgery). Data were collected by a surgeon or stoma nurse.
-
DS closure morbidity: morbidity associated with DS closure (during the first 30 days postoperative or during admission for stoma reversal). Data were collected by a surgeon.
-
DS-related morbidity: general stoma-related complications, including DS morbidity and DS closure morbidity.
-
Postoperative complications: those occurring after any surgical procedure (either for primary colorectal surgery or for DS closure, collected separately). They were categorized according to the Clavien–Dindo classification [18]. If multiple complications happened, the highest grade was used in both groups. Major complications were defined as those requiring some interventions under general anesthesia (Clavien–Dindo IIIb).
-
Ileus: absence of flatus/stool and inability to tolerate an oral diet for 4 days after the operation.
Statistical methods
Quantitative variables are expressed as mean and standard deviation (SD) in case of normal distribution, or median and interquartile range (IQR) for those with non-normal distribution. Qualitative variables are presented as absolute numbers and percentages. Contingency tables and χ2 analysis were used to determine the association between categorical variables, and Student’s t test or Mann–Whitney U test was used for continuous variables. Statistical significance was set at p value < 0.05. The statistical analysis was carried out with the IBM SPSS® v.24 software (SPSS®, Chicago, Illinois, USA).
A multivariable linear regression model was used to assess the effect of different factors on the time to stoma closure. Results were expressed as regression coefficients with 95% confidence interval (CI). In addition, a logistic regression model was used to assess the effect of baseline variables, primary surgery variables, and time with DS on the appearance of complications related to DS. Results were expressed as odds ratio (OR) with 95% CI.
Results
Demographic characteristics
During both periods, a total of 157 consecutive patients were subjected to DS after colorectal surgery in our institution. After the application of exclusion criteria, 145 were included in this analysis: 80 patients underwent DS closure in Period 1 (between January 2015 and December 2019) and 65 patients in Period 2 (between January 2020 and December 2022) (Fig. 2). Demographic and clinical data, including the initial indication for DS, are summarized in Table 1. More than half of the patients were men (n = 79; 54.5%) and the median age was 66 (IQR 58–76) years. TME for rectal cancer was the main indication to perform a DS in both periods (n = 107; 73.8%). No significant baseline differences were observed between patients of both groups apart from a higher rate of hypertension and higher body mass index (BMI) in those of Period 2.
Consolidated Standards of Reporting Trials (CONSORT) diagram of the study. DS defunctioning stoma, Period 1 Period before the implementation of the Early Stoma Closure protocol, Period 2 Period after the implementation of the Early Stoma Closure protocol, EC early closure group (< 30 days), LC late closure group, CTE computed tomography enema, IBD inflammatory bowel disease
Time from primary surgery and DS closure
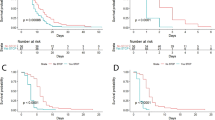
Median time from primary surgery to stoma closure was significantly higher in Period 1 [233 (137–382) days] than in Period 2 [42 (21–193) days] (p < 0.001). During Period 2, 43.1% of patients (n = 28) underwent closure within 30 days from DS creation, while the remaining patients (n = 37) underwent LC (Fig. 3A). The main reasons for LC in Period 2 were exclusion criteria for EC in 22 patients (59.5%), inability to schedule the intervention within the EC lapse time in 13 patients (35.1%), and severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2) infection in 2 patients (5.4%) as shown in Fig. 2.
A subanalysis was performed to assess whether a reduction in stoma time was achieved in patients who were not candidates for EC. Median time from primary surgery to stoma closure in the LC group was 164 (52–223) days in Period 2, which was also significantly lower compared with this time in Period 1 [233 (137–382) days], p = 0.004) (Fig. 3B).
Results from the multivariable linear regression analysis of the effect of different factors on the time to DS closure are presented in Table 2. ECP implementation (Period 2) was significantly associated with reduction of time to DS closure, while primary surgery complications were significantly associated with increased time.
Colorectal anastomosis assessment and DS reversal technique
Colorectal assessment was heterogeneous in Period 1: 21 (27.6%) CTE, 25 (32.9%) contrast enema (CE), 17 (22.4%) endoscopy, and 13 (17.1%) any combination of those. Meanwhile, in Period 2 all colorectal anastomoses were investigated radiologically with CTE to ensure correct assessment of anastomotic integrity according to ECP. Two patients in this period needed an extra exploration with endoscopy because of stenosis of the anastomosis, and two asymptomatic AL were successfully detected. CTE performed from POD 7–14 had a 3.1% false negative rate in this study. One patient required a reintervention (DS and endo-sponge®) and the other one a percutaneous drainage and intravenous antibiotic therapy. Median time from primary surgery to evaluation of colorectal anastomosis was lower in Period 2 than in Period 1 [(10 (7–162) days versus 149 (69–298) days, p < 0.001].
Median duration of the reversal procedure (including both the surgical and anesthetic procedures) was shorter in Period 2 than in Period 1 [110 (90–120) min versus 120 (90–147) min, p = 0.018), while no differences in technical anastomotic reconstruction were observed between both periods. In accordance with ECP, the skin closure technique used was a purse-string in all Period 2 patients, while linear closure was the main technique in Period 1 (65/80 patients, 81.3%), with a significant statistical difference (p < 0.001).
DS-related morbidity
DS-related complications in each period are presented in Table 3. During the follow-up between primary surgery and reversal, DS morbidity was higher in Period 1 (68.8% versus 49.2%, p = 0.017), including conditions such as skin irritation (50% versus 32.3%, p = 0.032) and parastomal hernia (17.5% versus 6.2%, p = 0.045). Accordingly, the number of visits to the stoma nurse was also higher in this period (p = 0.029). However, no significant difference was detected between the two groups regarding overall incidence and severity of DS closure complications, reinterventions, length of hospital stay, and readmissions. During the 90-day postoperative period after DS closure, no mortality was recorded in any period.
Multivariate analysis was performed to identify risk factors for DS-related morbidity (Table 4). Late closure resulted as an independent risk factor for DS morbidity. Regarding past medical history, only patients with ASA scores III–IV and patients who suffered from complications after primary surgery were more likely to have complications after DS closure.
Early closure versus late closure
A subanalysis was performed within Period 2 between EC and LC patients aiming to evaluate the effectiveness and safety of implementing our ECP (Table 5).
The overall DS morbidity rate was significantly higher in the LC group (64.9% versus 28.6%, p < 0.001), with skin irritation as the only DS complication in the EC group. High-volume output with acute kidney failure was higher in the LC group (27% versus 0%, p < 0.001), leading to readmissions in the same group (16.2% versus 0%, p = 0.002). In accordance with these results, the EC group had lower number of stoma nurse visits (p < 0.001).
Overall DS closure morbidity rate and severity did not differ between the EC and LC groups (p = 0.073), and neither were there differences in any type of AL between both groups. Two patients underwent reoperation in the EC group. One of them was reoperated due to early bleeding of the anastomotic mesentery to resolve this complication and ensure an adequate anastomosis vascularization. The other one underwent a re-defunctioning ileostomy due to a late colorectal AL. No significant difference was detected between the two groups regarding the length of hospital stay or readmissions.
Oncological patients
A total of 107 patients with TME and DS for rectal cancer in both study periods were included in a subanalysis. Demographic, DS-related morbidity, and chemotherapy data are summarized in Supplementary Table 1. More patients received total neoadjuvant therapy (TNT) in Period 2 (p < 0.001). However, there was no statistically significant difference between the two periods in the time from primary surgery to the start of adjuvant therapy. In Period 2, only one patient with LC and another patient with EC experienced AL complications, which subsequently interfered with adjuvant treatment. The remaining patients who have an indication for adjuvant treatment did not receive it due to patient’s comorbidities.
Discussion
The ECP implementation in our unit was associated with markedly shorter intervals to restoration of bowel continuity in patients with DS after colorectal surgery (42 days versus 233 days, p < 0.001). This outcome was observed not only in patients selected for EC, but also in those from Period 2 who were not considered eligible (164 days versus 233 days, p = 0.004) (Fig. 3). This reduction in time to closure did not impact the postoperative morbidity and resulted in fewer stoma complications and fewer stoma nurse visits.
Time to DS closure varies widely and is not subject to national targets [14]. The CLOSE-IT study reported that 35% of DS following TME for rectal cancer were not closed at 18 months in the UK [19]. This result is in line with findings observed during Period 1 in our study, in which 27.5% of DS have not been closed at 12 months (Fig. 3), mainly due to patient comorbidity, need for chemotherapy, or extended waiting list, thus mirroring the outcomes reported in CLOSE-IT. However, multiple randomized control trials and meta-analyses conducted in Europe have demonstrated that EC is safe, cost-effective, and improves functional outcomes and patients’ quality of life (QoL) in a subset of patients [4, 15, 20,21,22]. Such an approach appears attractive and has demonstrated in a recent study to be a priority for both surgeons and patients [23]. For this reason, we wanted to apply it to our clinical practice by developing a multidisciplinary protocol encompassing the following essential components: selection of patients according to their primary surgery and postoperative recovery, an adequate assessment of the colorectal anastomosis within a target time [24], and according to other groups [14, 25], a preemptive scheduling of patients by a dedicated team coordinator for closure immediately after primary surgery. Furthermore, a driving force of the reduced DS closure times in the LC group since ECP implementation was identified in our study; an experienced team (surgeons and stoma nurses) that provides consistency to the planning of reversal, which has been suggested to exert an influence on closure times [13, 23]. Accordingly, our multivariable linear regression demonstrated that ECP implementation (Period 2) was significantly associated with reduction of time to DS closure, while primary surgery complications were significantly associated with increased time to DS closure. These results have important clinical consequences, since time to stoma reversal can be significantly reduced in a vast majority of patients with the implementation of an ECP with strict selection criteria, independently of their primary diagnosis, ASA score, or other comorbidities.
Patient selection is a crucial part of this approach because only patients without clinical or radiological signs of adverse events after some primary colorectal surgery (TME, diverticular disease, or Hartman’s reconstruction) are suitable for EC (Fig. 1) [26]. Consequently, differences of some variables were observed between the EC and LC groups prior to stoma closure, as presented in Table 5 in Period 2. In prior studies, EC exclusion rates have been reported to range from 25% to 33% [27, 28]. In our study, after ECP implementation (Period 2), 59.5% of the patients did not meet the strict requirements for EC. However, ECP was an evidence-based safety measure, and even though only 40% of the patients of the entire period qualified for EC, the remaining patients (LC) still benefited from a substantial reduction in the time to DS closure. This represents a significant improvement for all patients in this period.
Most would agree that engaging in early reversal of DS without confidence regarding the integrity of the anastomosis has tremendous implications for patients’ safety [26], as Elsner et al. showed in their randomized controlled trial [30]. A recent study by Kitaguchiet et al. [31] described that routine use of CE at POD 7 was insufficient to detect occult AL and more cases were detected with a following CTE. A 33% rate of false negative radiological results was determined for CE in their study, while Danielsen et al. [16] reported no false negative radiologic results using CTE before EC. In light of current evidence on EC, CTE from POD 7 onward was the diagnostic method chosen in our study prior to performing DS closure surgery, with a 3.1% false negative rate.
EC has traditionally been related to two major threats for patients: the possibility of higher morbidity rates at the time of DS closure, and the eventual delay or rejection of chemotherapy administration if major complications happen after DS closure in patients with rectal cancer.
Morbidity findings of the current study are consistent with previous studies [16, 28] showing less overall DS morbidity and fewer readmission in EC patients, in particular relieving patients from high-volume output problems. This advantage had an impact on Period 2, in which patients had less overall DS morbidity compared with Period 1 without impact on DS closure morbidity. We believe that the reduction in complications can be explained by the fact that time is a variable that directly affects these results [7], as shown in the multivariate analysis.
A subanalysis was conducted in patients with rectal cancer showing that ECP implementation did not lead to a delay in the initiation of adjuvant treatment (Supplementary Table 1). Currently, there is no evidence regarding optimal timing for DS closure in relation to adjuvant chemotherapy and its influence on overall survival [11, 32]. Two randomized controlled trials are in progress to clarify this question (CoCStom and STOMAD) [33, 34]. Nevertheless, the emergence of TNT has reduced the concerns regarding the potential delay in adjuvant therapy caused by DS closure, thereby facilitating the patients to benefit from the favorable outcomes associated with EC.
The findings presented in this study, combined with published evidence on timing and patient selection for EC, could be considered as valuable resources for future projects focusing on the development of national pathways to DS closure, as proposed in other countries [14].
Our study has some limitations. Firstly, the retrospective nature of Period 1 could determine selection bias and underestimate complication rate. Secondly, the participation of stoma nurses in patient management only in Period 2 could be a source of observer bias. Thirdly, both periods were homogeneous in terms of primary surgery indication, and the recommendation was strong, in most cases, to proceed with a temporary DS when creating a high-risk anastomosis. Despite this, patient selection and the type of primary surgery could have been possible sources of bias. Further comparative research with each primary surgery indication is necessary. Finally, the SARS-CoV-2 pandemic may have caused a delay in DS closure due to changes in protocols in our center during the pandemic. Despite these limitations, this study has significant strengths, as it provides evidence that could contribute to improving DS closure in clinical practice in a tertiary hospital.
In conclusion, the implementation of an ECP with strict inclusion and exclusion criteria has been very satisfactory in terms of compliance and safety. This protocol has been able to reduce intervals to restoration of bowel continuity in patients with DS after colorectal surgery, which in turn has resulted in a direct reduction of morbidity attributable to long intervals.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Mu Y, Zhao L, He H, Zhao H, Li J (2021) The efficacy of ileostomy after laparoscopic rectal cancer surgery: a meta-analysis. World J Surg Onc 19(1):318
Matthiessen P, Hallböök O, Rutegård J, Simert G, Sjödahl R (2007) Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg 246(2):207–214
Yang M, McClure JA, Wanis KN, Vogt KN, Van Koughnett JAM, Ott MC et al. (2022) From formation to closure: aggregate morbidity and mortality associated with defunctioning loop ileostomies. Dis Colon Rectum 65(9):1135–1142
Vogel I, Reeves N, Tanis PJ, Bemelman WA, Torkington J, Hompes R et al. (2021) Impact of a defunctioning ileostomy and time to stoma closure on bowel function after low anterior resection for rectal cancer: a systematic review and meta-analysis. Tech Coloproctol 25(7):751–760
Robertson J, Linkhorn H, Vather R, Jaung R, Bissett IP (2015) Cost analysis of early versus delayed loop ileostomy closure: a case-matched study. Dig Surg 32(3):166–172
Herrle F, Sandra-Petrescu F, Weiss C, Post S, Runkel N, Kienle P (2016) Quality of life and timing of stoma closure in patients with rectal cancer undergoing low anterior resection with diverting stoma: a multicenter longitudinal observational study. Dis Colon Rectum 59(4):281–290
Rubio-Perez I (2014) Increased postoperative complications after protective ileostomy closure delay: an institutional study. WJGS 6(9):169
Climent M, Frago R, Cornellà N, Serrano M, Kreisler E, Biondo S (2022) Prognostic factors for complications after loop ileostomy reversal. Tech Coloproctol 26(1):45–52
Barenboim A, Geva R, Tulchinsky H (2022) Revised risk factors and patient characteristics for failure to close a defunctioning ileostomy following low anterior resection for locally advanced rectal cancer. Int J Colorectal Dis 37(7):1611–1619
Hoshino N, Hida K, Fukui Y, Takahashi Y, Nakayama T, Obama K (2022) Relationship between diverting stoma and adjuvant chemotherapy in patients with rectal cancer: a nationwide study using the national database of health insurance claims and specific health checkups of Japan. Int J Clin Oncol 27(3):545–552
Cheng HH, Shao YC, Lin CY, Chiang TW, Chen MC, Chiu TY et al. (2023) Impact of chemotherapy on surgical outcomes in ileostomy reversal: a propensity score matching study from a single centre. Tech Coloproctol. https://doi.org/10.1007/s10151-023-02790-6
Podda M, Coccolini F, Gerardi C, Castellini G, Wilson MSJ, Sartelli M et al. (2022) Early versus delayed defunctioning ileostomy closure after low anterior resection for rectal cancer: a meta-analysis and trial sequential analysis of safety and functional outcomes. Int J Colorectal Dis 37(4):737–756
Vogel I, Vaughan-Shaw PG, Gash K, Withers KL, Carolan-Rees G, Thornton M et al. (2022) Improving the time to ileostomy closure following an anterior resection for rectal cancer in the UK. Colorectal Dis 24(1):120–127
Dukes’ Club Research Collaborative, Chambers A, Stearns A, Walsh A, Rankin A, Khan A et al. (2021) Factors impacting time to ileostomy closure after anterior resection: the UK closure of ileostomy timing cohort study (CLOSE-IT). Colorectal Dis 23(5):1109–1119
O’Sullivan NJ, Temperley HC, Nugent TS, Low EZ, Kavanagh DO, Larkin JO et al. (2022) Early vs. standard reversal ileostomy: a systematic review and meta-analysis. Tech Coloproctol 26(11):851–862
Danielsen AK, Park J, Jansen JE, Bock D, Skullman S, Wedin A et al. (2017) Early closure of a temporary ileostomy in patients with rectal cancer: a multicenter randomized controlled trial. Ann Surg 265(2):284–290
Hajibandeh S, Hajibandeh S, Kennedy-Dalby A, Rehman S, Zadeh RA (2018) Purse-string skin closure versus linear skin closure techniques in stoma closure: a comprehensive meta-analysis with trial sequential analysis of randomised trials. Int J Colorectal Dis 33(10):1319–1332
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
NBOCA-annual-report-2017-v2.pdf
Menahem B, Lubrano J, Vallois A, Alves A (2018) Early closure of defunctioning loop ileostomy: is it beneficial for the patient? A meta-analysis. World J Surg 42(10):3171–3178
Walma MS, Kornmann VNN, Boerma D, de Roos MAJ, van Westreenen HL (2015) Predictors of fecal incontinence and related quality of life after a total mesorectal excision with primary anastomosis for patients with rectal cancer. Ann Coloproctol 31(1):23
Park J, Angenete E, Bock D, Correa-Marinez A, Danielsen AK, Gehrman J et al. (2020) Cost analysis in a randomized trial of early closure of a temporary ileostomy after rectal resection for cancer (EASY trial). Surg Endosc 34(1):69–76
Caminsky NG, Moon J, Morin N, Alavi K, Auer RC, Bordeianou LG et al. (2023) Patient and surgeon preferences for early ileostomy closure following restorative proctectomy for rectal cancer: why aren’t we doing it? Surg Endosc 37(1):669–682
Lindner S, Eitelbuss S, Hetjens S, Gawlitza J, Hardt J, Seyfried S et al. (2021) Less is more—the best test for anastomotic leaks in rectal cancer patients prior to ileostomy reversal. Int J Colorectal Dis 36(11):2387–2398
Chand M, Nash GF, Talbot RW (2008) Timely closure of loop ileostomy following anterior resection for rectal cancer. Eur J Cancer Care. https://doi.org/10.1111/j.1365-2354.2008.00972.x
Panis Y (2021) Early stoma closure after rectal resection for cancer: still a matter of debate? Dis Colon Rectum 64(11):1303–1304
Bakx R, Busch ORC, Van Geldere D, Bemelman WA, Slors JFM, Van Lanschot JJB (2003) Feasibility of early closure of loop ileostomies: a pilot study. Dis Colon Rectum 46(12):1680–1684
Alves A, Panis Y, Lelong B, Dousset B, Benoist S, Vicaut E (2008) Randomized clinical trial of early versus delayed temporary stoma closure after proctectomy. Br J Surg 95(6):693–698
Dimitriou N, Panteleimonitis S, Dhillon A, Boyle K, Norwood M, Hemingway D et al. (2015) Is the routine use of a water-soluble contrast enema prior to closure of a loop ileostomy necessary? A review of a single institution experience. World J Surg Onc 13(1):331
Elsner AT, Brosi P, Walensi M, Uhlmann M, Egger B, Glaser C et al. (2021) Closure of temporary ileostomy 2 versus 12 weeks after rectal resection for cancer: a word of caution from a prospective, randomized controlled multicenter trial. Dis Colon Rectum 64(11):1398–1406
Kitaguchi D, Enomoto T, Ohara Y, Owada Y, Hisakura K, Akashi Y et al. (2020) Exploring optimal examination to detect occult anastomotic leakage after rectal resection in patients with diverting stoma. BMC Surg 20(1):53
Koc MA, Akyol C, Gokmen D, Aydin D, Erkek AB, Kuzu MA (2023) Effect of prehabilitation on stoma self-care, anxiety, depression, and quality of life in patients with stomas: a randomized controlled trial. Dis Colon Rectum 66(1):138–147
Calderillo-Ruíz G, López-Basave HN, Muñoz-Montaño WR, Díaz-Romero MC, Carbajal-López B, Castillo-Morales C et al. (2023) Impact of ileostomy in the adjuvant treatment and outcome of colon cancer. Int J Colorectal Dis 38(1):158
Acknowledgements
We thank Manuel Gómez Gutiérrez from Instituto de Investigación Sanitaria Princesa (IIS-IP) for professional English editing of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by LBT, LDB, and ACB. The first draft of the manuscript was written by LBT and CCS and all authors commented on the different versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflicts of interest.
Ethical approval
All the procedures performed complied with the rules of the institutional and/or national research ethics committees and with the Declaration of Helsinki of 1964 and its later modifications or similar ethics rules. The study was approved by the Clinical Research Ethics Committee (CREC) of our institution (registry number 4390) in February 2021.
Informed consent
The authors declare that informed consent was obtained from all individual participants for whom identifying information is included in this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Blanco Terés, L., Cerdán Santacruz, C., Correa Bonito, A. et al. Early diverting stoma closure is feasible and safe: results from a before-and-after study on the implementation of an early closure protocol at a tertiary referral center. Tech Coloproctol 28, 32 (2024). https://doi.org/10.1007/s10151-023-02905-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10151-023-02905-z