Abstract
Background
Anastomotic leakage (AL) is a major complication of colorectal surgery resulting in morbidity, mortality and poorer quality of life. The early diagnosis of AL is challenging due to the poor positive predictive value of tests available and reliance on clinical presentation which may be delayed. The aim of this systematic review was to assess the applicability of peritoneal cytokine levels as an early predictive test of AL in postoperative colorectal cancer patients.
Methods
A comprehensive literature search was performed from inception to January 2021, in MEDLINE and EMBASE databases using MeSH and non-MeSH terms in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. All studies evaluating peritoneal cytokines in the context of AL were included in this review.
Results
Two hundred ninety-two abstracts were screened, 30 full manuscripts evaluated, and 12 prospective studies were included. There were 8 peritoneal cytokines evaluated (interleukin [IL]-1β, IL-6, IL-8, IL-10, vascular endothelial growth factor [VEGF], tumour necrosis factor alpha [TNF alpha] and matrix metalloproteinase [MMP]2 and MMP9) between AL and non-AL groups on postoperative day 1. Those that included IL-6 (7 studies), IL-10 (4 studies), TNF alpha (6 studies) and MMP9 (2 studies) were included in the meta-analysis. IL-10 was the only cytokine in the meta-analysis that was significantly (p < 0.05) raised in drain fluid on postoperative day 1 in AL patients.
Conclusions
Peritoneal IL-10 was significantly raised on postoperative day 1 in patients who subsequently developed AL. This may be a useful early predictor of AL and aid in an earlier diagnosis for postoperative colorectal patients. The range of cytokines investigated within the literature is limited and from heterogeneous studies which suggests more research is needed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is the third most frequent cancer worldwide, with two-thirds of cases being treated surgically [1]. Surgical technique in oncological colorectal resection has advanced through the adoption of laparoscopic surgery and implementation of ‘Enhanced Recovery After Surgery’ (ERAS) protocols [2,3,4]. Despite these advances, anastomotic leakage (AL) continues to be a significant postoperative complication affecting up to 20% of primary anastomosis and accounting for a mortality of 0.7% amongst colorectal cancer patients [5]. It has a significant effect on morbidity, quality of life, duration of hospital stay and long-term cancer survival [6,7,8].
Earlier diagnosis of AL at a subclinical stage could minimise morbidity and mortality by reducing the impact of systemic sepsis and multi-organ failure [9]. Early clinical signs of AL include fever, oliguria, ileus, diarrhoea and leucocytosis, which are non-specific in the post-operative patients for other reasons including the postoperative systemic inflammatory response [10]. Investigations of suspected AL in the early post-operative period include computed-tomography (CT) scan and serum C-reactive protein (CRP) measurements but they have limitations. Diagnosis of AL from CT scan has a sensitivity of 59% [11] and serum CRP levels has a have a negative predictive value of 97.5% on day 3 post-operatively [12]. There continues to be a lack of a highly sensitive and specific diagnostic test for an AL in the early postoperative period (days 1–3).
Following a surgical colorectal anastomosis, there is a localised immune response within the peritoneal fluid associated with normal healing [13]. The development of an AL disrupts this normal healing process and there has been research into whether the inflammatory cytokines with the peritoneal fluid can be measured to detect AL at a subclinical stage. The aim of this systematic review and meta-analysis was to identify if any of these peritoneal immune biomarkers are significantly increased in peritoneal fluid postoperatively.
Materials and methods
The systematic review was conducted following the procedures specified in the 2009 update of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [14]. The protocol of the systematic review is available through PROSPERO (http://www.crd.york.ac.uk/PROSPERO/), where it has been assigned the following registration number CRD42021170089.
Two reviewers (NR and AG) determined the search terminology, undertook the study selection, data extraction and quality assessment independently. All data created were recorded electronically in an initially blinded and then later shared database. Disagreements in "study selection" or quality assessments were resolved by discussion between reviewers. The senior author (JT) was in place to resolve ongoing disparity between reviewers.
Search strategy
A comprehensive search of the literature was performed in MEDLINE and EMBASE in from inception to January 2021. No restrictions were placed on the publication date; but the searches were restricted to English language and human studies. The search terms were as follows: (colorectal surgery OR rectal surgery OR rectal cancer) AND (anastomotic leak OR anastomotic dehiscence OR anastomosis) AND (peritoneal fluid OR drain fluid OR biomarkers OR cytokines). The search was completed using MeSH and non-MeSH terms, with subsequent de-duplication.
Study selection
The titles and abstracts of manuscripts found in the literature search were screened for relevance. The inclusion criteria were human studies of any colorectal resections which evaluated peritoneal biomarkers postoperatively. Exclusion criteria included non-human studies, other gastrointestinal surgery (for example gastrectomy), letters or reviews, and studies that only evaluated serum biomarkers.
Data extraction
The data were extracted into a table with predefined fields, to compare biomarker levels, between the AL and non-AL groups. Only postoperative day 1 results were evaluated, to try and establish what happens in the immediate postoperative period. Also included were study design, study size, colorectal procedures included in the study and the rate of AL recorded in the study. Within the studies, to include the data on rate of AL, the methodology had to include the diagnostic criteria and the subsequent treatment details of the patients with AL. Authors were contacted to ensure completeness and accuracy of data extracted.
Quality assessment
The Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool was used to assess the quality of included studies. The risk of bias was assessed across the four domains stated in the tool: patient selection, index text, reference standard and the flow and timing of tests in relation to the patients in the study. The applicability of the studies was also evaluated.
Statistical analysis
Data from the included studies were only used in the meta-analysis if day 1 measurements for the cytokine were available with clearly stated units. If the data were not clearly available from the manuscripts, then the authors were contacted. Any study which did not have clear numerical measurements were excluded from the meta-analysis.
Heterogeneity was assessed using the I2 and X2 statistics, and the data were considered significant if the p value (X2) was < 0.1 and I2 was > 75%. Analysis was performed using Review Manager (RevMan, version 5.3. Copenhagen, Denmark: The Nordic Centre, the Cochrane Collaboration, 20.) Analysis was performed using a random effects model. The Inverse Variance method was used to calculate the mean difference and the 95% confidence interval using a random effects model, which were illustrated in forest plots. When a median value of the biomarkers was presented with an interquartile range, our method was used to covert to mean values with a standard deviation.
Results
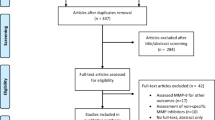
The literature search yielded 306 manuscripts of which 14 were duplicates. Two hundred ninety-two abstracts that were screened for inclusion. At this point, 262 were excluded as per the exclusion criteria. After a full-text review of the 30 manuscripts, 12 studies evaluating inflammatory cytokines found in peritoneal fluid were included, whilst the 18 articles with a focus only on serum biomarkers were excluded [15,16,17,18,19,20,21,22,23,24,25,26].
The PRISMA flowchart outlines the selection process of the studies included (Fig. 1). The summary of the 12 manuscripts included in the systematic review are within Table 1. There have been 8 different cytokines (interleukin [IL]-1β, IL-6, IL-8, IL-10, vascular endothelial growth factor [VEGF], tumour necrosis factor alpha [TNF alpha], matrix metalloproteinase [MMP]2 and MMP9) studied taken from measurements obtained at 6 h to 9 days postoperatively. The bias assessment of the studies was completed (Table 2). None of the studies included investigated every study patient for an AL, and they only defined those patients with an AL as those with a clinical AL. Also, there was no long-term follow-up of the patients beyond 30 days in any of the included studies for a subclinical AL, or late presentation of an AL. There was high bias in the patient diagnosis of AL, and this had an impact on the subsequent interpretation of the results.
Study details
There were 12 studies included in the systematic review (Table 1). The sample sizes ranged from 24 to 292 and all studies were prospective studies. Two of the studies used matched groups, hence the 50% AL rate, whilst the AL rate in the other studies ranged from 8.2 to 30.4%. Two of the studies had prospectively included patients with high risk for AL but this was not pre-defined in their methodology. Only six studies looked at a homogenous group of patients, those that underwent an anterior resection for sigmoid and rectal cancers. Three studies had a mixture of pathologies with benign cases (inflammatory bowel disease and adenomas) and cancer patients being analysed as the same cohort. Six studies had different colorectal operations being considered as one cohort, for example right hemicolectomies and anterior resections.
Follow-up was variable across the studies, from 14 days to 5 years, with 4 studies not stating follow-up time. All the studies considered the AL patients to be those with clinical AL requiring treatment but had different methods of determining the presence of an AL; with no studies considering asymptomatic AL as a subgroup in analysis. The definition of treatment varied between the studies, from only including those undergoing re-laparotomy to including both non-operative and operative treatments. Finally, the studies had different sample storage conditions and analysis techniques.
IL-1β
IL-1β was measured in three studies [18, 21, 26], however, there was not sufficient data within the published data to perform a meta-analysis. All three studies did demonstrate that there was an increasing trend in IL–1β from postoperative day 2 with it being significantly raised on postoperative day 3, whereas those patients with no peritonitis/AL did not have any rise in IL–1β levels.
IL-6
IL-6 was measured in 11 of the 12 studies included in this review [15,16,17,18,19,20,21, 23,24,25,26]. Data from 7 of the studies were included in the meta-analysis, seen within Fig. 2(A). There was no significant difference between those with an AL and those without in the meta-analysis although six of the seven studies demonstrated a raised IL-6 in those with an AL. However, there is a high degree of heterogeneity between the studies which may explain a non-significant p value.
Meta-analysis of peritoneal cytokines on postoperative day 1. (A) Comparison of peritoneal IL6 ng/ml anastomotic leak vs. control group. (B) Comparison of peritoneal Il10 pg/ml anastomotic leak vs. control group. (C) Comparison of peritoneal TNF alpha pg/ml anastomotic leak vs. control group. (D) Comparison of peritoneal MMP9 pg/ml anastomotic leak vs. control group
IL-8
IL-8 was measured in a single study by Sammour et al. who reported that there was no significant difference between those with an AL and those without [25].
IL-10
IL-10 was measured in six studies [17, 18, 20, 23,24,25,26], with data from four of the studies were included in the meta-analysis, seen within Fig. 2(B). IL-10 is significantly higher (p < 0.001) in patients with an AL on postoperative day 1 and all studies report homogenous results.
VEGF
VEGF was measured in a single study by Alonso et al. (2014), which demonstrated that VEGF was significantly higher (p = 0.001) in patients with an AL and correlated with IL-6 peritoneal levels [15].
TNF alpha
TNF alpha was measured in eight studies [16,17,18,19,20,21,22,23, 25], with six studies included in the meta-analysis in Fig. 2(C). There was no significant difference between those with an AL and those without, however, there was a high degree of heterogeneity between the studies.
MMP2
MMP2 was only measured in a single study, Sparreboom et al. There was no difference in the levels of MMP2 between those patients with an AL and those without.
MMP9
MMP9 was measured in two studies [22, 26] with both studies included in the meta-analysis in Fig. 2 (D). There was no significant difference between patients with an AL and those without, despite there being low heterogeneity between the two studies.
Discussion
AL is a significant complication which increases postoperative morbidity and mortality [6,7,8,9]. Current diagnosis of AL relies primarily on CT scanning and serum CRP [11, 12]. This meta-analysis has shown that of the eight cytokine biomarkers measured in peritoneal fluid, only IL-10 has been found to be significantly raised on postoperative day 1. However, VEGF was only measured in one study and was significantly higher in those with an AL (p = 0.001). IL-10 could form part of a more sensitive diagnostic test to indicate those patients developing an AL in the early postoperative period and give an insight into the localised immune process associated with the development of AL.
Following colorectal surgery, pro-inflammatory and anti-inflammatory mediators are released locally in the peritoneal cavity as part of the normal healing process [27]. Much attention has been given to IL-6 as it is a driver of the acute-phase response and can activate T-cell proliferation, which explains why it is raised in many inflammatory clinical conditions including sepsis [28]. IL-6 was measured in 11 of the 12 studies included in the review. Despite many studies measuring peritoneal IL-6 postoperatively, only five of the studies found a significant difference on postoperative day 1 and the meta-analysis did not find it significantly raised, likely due to the heterogeneity of the studies.
IL-10 is significantly raised in the meta-analysis of four studies in postoperative day 1 peritoneal fluid in those patients who then went on to develop an AL. IL-10 is an anti-inflammatory cytokine which is important in regulating the immune response to pathogens allowing normal tissue homeostasis, limiting tissue damage from an over-active immune response. However, elevated levels of IL-10 affects the local immune response to bacteria which is associated with tissue damage [29]. The presence of IL-10 may indicate an impaired tissue healing process in those with a primary anastomosis, hence a developing AL.
Due to the development of the ERAS protocol [2], the use of intraperitoneal drains to facilitate peritoneal fluid drainage has become reduced due to the consensus that peritoneal drains would reduce mobility postoperatively. Meta-analysis have been equivocal showing no benefit of peritoneal drains in reducing anastomotic complications, but with no significant increase in complications directly related to the drains [30, 31]. However, the abdominal drains give a unique window to testing the peritoneal fluid which has a larger local cytokine release after colorectal surgery than in the systemic circulation, and this has led to research studies into potential peritoneal biomarkers [13].
Though this review has found numerous studies which had individually significant findings, collectively the meta-analysis only found that IL-10 levels were significant, and this is due to the wide heterogeneity of the studies. Most of the studies included were only on open procedures or on a large proportion of open procedures, which is not representative of current practice with the shift towards increased laparoscopic surgery. The more recent study by Sparreboom et al. (2019) was the only study to represent current surgical practice with a rate of laparoscopic procedures of 55.1% and transanal procedures of 41.1% [26]. The impact of an open or laparoscopic approach due to the peritoneal immune response is well described, with Glatz et al. reported statistically significant lower IL-6 levels on postoperative day 1 after laparoscopic surgery compared to open procedures [32].
Other aspects of the studies were also heterogenous including comparing different colorectal pathologies (benign and malignant) and different colorectal operations in the same study cohorts (right and left resections). There were also different definitions of AL in each study, which means that it is difficult to accurately assess end points between the studies. It is becoming increasingly accepted that there are patients who may have a subclinical AL and these patients do not require immediate postoperative or non-operative treatment but often present later when a defunctioning stoma is reversed, or with poorer functional outcomes. None of the studies included longer follow-up imaging to check the integrity of the anastomosis, and all studies considered the group of subclinical AL patients as those that recover without complications, and this may have had an impact on the cytokines measured. Furthermore, there were two studies that used matched groups to explore the differences in the peritoneal biomarkers which may have introduced selection bias into their results.
Only the peritoneal cytokine measurements from postoperative day 1 were included in this systematic review, and this limits the understanding of the potential trends of cytokine levels in the immediate postoperative recovery period. The rationale for evaluating only postoperative day 1 is that the ability to accurately identify those patients that develop an AL early, within 24 h of surgery, could facilitate early interventions that may limit the impact of AL on the patient. An early diagnosis could prompt a diagnostic laparoscopy/endoscopy to inspect the anastomosis, allow a delayed creation of a defunctioning stoma only if high risk for AL, and prompt initiation of early antibiotics to prevent systemic sepsis. Early diagnosis and management of AL could even reduce the number of stomas formed overall and thus have a positive impact on long-term function.
AL and infectious complications following surgery are relatively uncommon, and therefore studies with large cohorts of patients focusing on only 1 surgical procedure are difficult to produce. In existing studies, IL-10 levels obtained from peritoneal fluid show promise as a predictor of AL, but in order to reduce type II error, larger sample sizes are needed. Studies aiming to only recruit patients undergoing one type of laparoscopic procedures (i.e. Anterior Resections) are needed, as the early research indicates that there is the potential to utilise the peritoneal immune response in early diagnosis of AL.
Conclusions
This systematic review and meta-analysis have demonstrated that IL-10 has the potential of being an early diagnostic test. However, the studies are heterogenous in design, and the number of cytokines studied are limited. Further work on different cytokines and the cellular immune responses and pathways within the local peritoneal fluid may give insight into the mechanism of an AL.
Data availability
Please contact the corresponding author for data/material.
Code availability
Not applicable.
References
NBOCA (2018) National Bowel Cancer Audit Annual Report 2018.
Fearon KCH, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CHC, Lassen K et al (2005) Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 24(3):466–477
ERAS Compliance Group (2015) the impact of enhanced recovery protocol compliance on elective colorectal cancer resection. Ann Surg 261(6):1153–1159
Aarts M, Rotstein ÃOD, Pearsall EA, Victor JC, Okrainec A, Mckenzie M et al (2018) Postoperative ERAS interventions have the greatest impact on optimal recovery experience with implementation of eras across multiple hospitals. Ann Surg 267(6):992–997
McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC (2015) Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg 102(5):462–479
Nachiappan S, Askari A, Malietzis G, Giacometti M, White I, Jenkins JT et al (2015) The impact of anastomotic leak and its treatment on cancer recurrence and survival following elective colorectal cancer resection. World J Surg 39(4):1052–1058
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg 253(5):890–899
Snijders HS, Wouters MWJM, Van Leersum NJ, Kolfschoten NE, Henneman D, De Vries AC et al (2012) Meta-analysis of the risk for anastomotic leakage, the postoperative mortality caused by leakage in relation to the overall postoperative mortality. Eur J Surg Oncol 38(11):1013–1019
Alves A, Panis Y, Trancart D, Regimbeau JM, Pocard M, Valleur P (2002) Factors associated with clinically significant anastomotic leakage after large bowel resection: multivariate analysis of 707 patients. World J Surg 26(4):499–502
Sutton C, Marshall L, Williams N, Berry D, Thomas W, Kelly M (2004) Colo-rectal anastomotic leakage often masquerades as a cardiac complication. Color Dis 6(1):21–22
Kornmann VNN, Van Ramshorst B, Smits AB, Bollen TL, Boerma D (2014) Beware of false-negative CT scan for anastomotic leakage after colonic surgery. Int J Colorectal Dis 29(4):445–451
Singh PP, Zeng ISL, Srinivasa S, Lemanu DP, Connolly AB, Hill AG (2014) Systematic review and meta-analysis of use of serum C-reactive protein levels to predict anastomotic leak after colorectal surgery. Br J Surg 101(4):339–346
Wiik H, Karttunen R, Haukipuro K, Syrjälä H (2001) Maximal local and minimal systemic cytokine response to colorectal surgery: the influence of perioperative filgrastim. Cytokine 14(3):188–192
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA et al (2020) statement: an updated guideline for reporting systematic reviews. BMJ 2021:372
Alonso S, Pascual M, Salvans S, Mayol X, Mojal S (2015) Postoperative intra-abdominal infection and colorectal cancer recurrence: a prospective matched cohort study of inflammatory and angiogenic responses as mechanisms involved in this association. Eur J Surg Oncol [Internet] 41(2):208–214. https://doi.org/10.1016/j.ejso.2014.10.052
Bertram P, Junge K, Schachtrupp A, Götze C, Kunz D, Schumpelick V (2003) Peritoneal release of TNFα and IL-6 after elective colorectal surgery and anastomotic leakage. J Investig Surg 16(2):65–69
Uǧraş B, Giriş M, Erbil Y, Gökpinar M, Çitlak G, Işsever H et al (2008) Early prediction of anastomotic leakage after colorectal surgery by measuring peritoneal cytokines: prospective study. Int J Surg 6(1):28–35
Yamamoto T, Umegae S, Matsumoto K, Saniabadi AR (2011) Peritoneal cytokines as early markers of peritonitis following surgery for colorectal carcinoma: a prospective study. Cytokine 53(2):239–242
Bilgin IA, Hatipoglu E, Aghayeva A, Arikan AE, Incir S, Mamal Torun M et al (2017) Predicting value of serum procalcitonin, C-reactive protein, drain fluid culture, drain fluid interleukin-6, and tumor necrosis factor-α levels in anastomotic leakage after rectal resection. Surg Infect (Larchmt) 18(3):350–356
Fouda E, El Nakeeb A, Magdy A, Hammad EA, Othman G, Farid M (2011) Early detection of anastomotic leakage after elective low anterior resection. J Gastrointest Surg 15(1):137–144
Herwig R, Glodny B, Kühle C, Schlüter B, Brinkmann OA, Strasser H et al (2002) Early identification of peritonitis by peritoneal cytokine measurement. Dis Colon Rectum 45(4):514–521
Kostić Z, Panišić M, Milev B, Mijušković Z, Slavković D, Ignjatović M (2015) Diagnostic value of serial measurement of C-reactive protein in serum and matrix metalloproteinase-9 in drainage fluid in the detection of infectious complications and anastomotic leakage in patients with colorectal resection. Vojnosanit Pregl 72(10):889–898
Matthiessen P, Strand I, Jansson K, Törnquist C, Andersson M, Rutegård J et al (2007) Is early detection of anastomotic leakage possible by intraperitoneal microdialysis and intraperitoneal cytokines after anterior resection of the rectum for cancer? Dis Colon Rectum 50(11):1918–1927
Oikonomakis I, Jansson D, Hörer TM, Skoog P, Nilsson KF, Jansson K (2019) Results of postoperative microdialysis intraperitoneal and at the anastomosis in patients developing anastomotic leakage after rectal cancer surgery. Scand J Gastroenterol 54(10):1261–1268
Sammour T, Singh PP, Zargar-Shoshtari K, Sua B, Hill AG (2016) Peritoneal cytokine levels can predict anastomotic leak on the first postoperative day. Dis Colon Rectum 59(6):551–556
Sparreboom CL, Komen N, Rizopoulos D, Verhaar AP, Dik WA, Wu Z et al (2020) A multicentre cohort study of serum and peritoneal biomarkers to predict anastomotic leakage after rectal cancer resection. Color Dis 22(1):36–45
Wu Z, Vakalopoulos KA, Boersema GSA, Kroese LF, Lam KH, van der Horst PH et al (2014) The prevention of colorectal anastomotic leakage with tissue adhesives in a contaminated environment is associated with the presence of anti-inflammatory macrophages. Int J Colorectal Dis 29(12):1507–1516
Hunter CA, Jones SA (2015) IL-6 as a keystone cytokine in health and disease. Nat Immunol 16(5):448–457
Iyer SS, Cheng G (2012) Role of interleukin 10 transcriptional regulation in inflammation and autoimmune disease. Crit Rev Immunol 32(1):23–63
Rolph R, Duffy JM, Alagaratnam S, Ng P, Novell R (2004) Intra-abdominal drains for the prophylaxis of anastomotic leak in elective colorectal surgery. Cochrane Database Syst Rev
Zhang HY, Zhao CL, Xie J, Ye YW, Sun JF, Ding ZH et al (2016) To drain or not to drain in colorectal anastomosis: a meta-analysis. Int J Colorectal Dis 31(5):951–960
Glatz T, Lederer AK, Kulemann B, Seifert G, Holzner PA, Hopt UT et al (2015) The degree of local inflammatory response after colonic resection depends on the surgical approach: an observational study in 61 patients. BMC Surg 15(1):1–7
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors. It is registered with PROSPERO with registration number CRD42021170089.
Informed consent
No Informed Consent in required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Reeves, N., Vogel, I., Ghoroghi, A. et al. Peritoneal cytokines as a predictor of colorectal anastomotic leaks on postoperative day 1: a systematic review and meta-analysis. Tech Coloproctol 26, 117–125 (2022). https://doi.org/10.1007/s10151-021-02548-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-021-02548-y