Abridged Abstract [1]
Background
This is the first systematic review specifically investigating ileocolic anastomosis.
Objectives
To compare outcomes of ileocolic anastomoses performed using stapling and handsewn techniques. The hypothesis tested was that the stapling technique is associated with fewer complications.
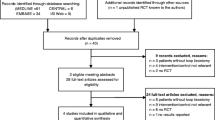
Search strategy
MEDLINE, EMBASE, Cochrane Colorectal Cancer Group specialised register SR-COLOCA, and Cochrane Library were searched for randomised controlled trials comparing the use of a linear cutter stapler with any type of suturing technique for ileocolic anastomoses in adults from 1970 to 2005. Selection criteria were randomised controlled trials comparing the use of linear cutter stapler (isoperistaltic side to side or functional end to end) with any type of suturing technique in adults. Regarding data collection and analysis, eligible studies were selected and their methodological quality assessed. Sub-group analyses for cancer and inflammatory bowel disease as indication for ileocolic anastomoses were performed.
Results
Six trials (including one unpublished) with 955 ileocolic participants were included. The three largest trials had adequate allocation concealment. Stapled anastomosis was associated with significantly fewer anastomotic leaks compared with the handsewn technique (S = 5/357, HS = 36/598, OR 0.34 [0.14, 0.82] p = 0.02). For the sub-group of 825 cancer patients in four studies, stapled anastomosis led to significantly fewer anastomotic leaks (S = 4/300, HS = 35/525, OR 0.28 [0.10, 0.75] p = 0.01). There were very less Crohn’s disease patients to perform a sub-group analysis. All other outcomes showed no significant difference.
Conclusions
Stapled functional end-to-end ileocolic anastomosis is associated with fewer leaks than handsewn anastomosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Commentary
The optimal ileocolic anastomotic configuration is generally accounted among the hot topics in colorectal surgery. This perhaps relates to the wide variety of options available and the lack of clarity from studies as to which, if any, is superior.
The most intriguing and worrisome factors associated with ileocolic anastomosis are clearly the risk of anastomotic leak, intra-abdominal abscesses, bleeding, strictures, wound infections and overall morbidity and mortality. All these factors have been investigated in the Cochrane review by Choy et al. [1]. This review includes 7 randomized controlled trials (1125 patients) comparing stapled anastomosis using a linear stapler (both isoperistaltic side-to-side or functional end-to-end) with any type of handsewn ileocolic anastomosis in adults. The most important finding from the pooled analysis is a significant reduction of the leak rate in the stapled anastomosis group compared with handsewn techniques. The review includes both cancer (4 studies) and Crohn’s disease trials (3 studies). In the subgroup analysis of non-cancer patients (mainly for Crohn’s disease), there is no difference for any reported outcomes, including the anastomotic leak rate.
If one considers other meta-analyses that focus only on Crohn’s disease, results are mixed. The meta-analysis by Simillis et al. [2] showed a reduction of the leak rate when comparing a wide lumen stapled side-to-side anastomosis with other anastomotic configurations. A meta-analysis by He et al. [3] showed a reduction in anastomotic leak and other complication rates when comparing a stapled side-to-side anastomosis to handsewn end-to-end. The most recent network meta-analysis by Feng et al. [4] suggests no difference between a stapled side-to-side and handsewn end-to end anastomosis for anastomotic leak and complications other than anastomotic leak. Despite these mixed results, the current consensus in favor a stapled side-to-side anastomosis after ileocolic resection for Crohn’s disease is based on a perceived reduction of the leak rate [5, 6].
However, when it comes to ileocolic Crohn’s resection, there is one other very important outcome to consider, and that is Crohn’s recurrence. In terms of recurrence, Simillis [2] suggested there was no significant difference between the anastomosis groups. He et al. [3] suggested a stapled side-to-side anastomosis was superior but the analysis included both randomized and non-randomized studies and, when only randomized studies were included, no anastomotic configuration was shown to be superior. Feng et al. [4] found a reduction in endoscopic recurrence but, again, of the 11 studies included, only 4 were randomized and more than half were retrospective.
The holy grail for surgeons treating Crohn’s disease is to find a surgical technique that reduces recurrence. From this standpoint, it is worth mentioning the potential role of Kono-S anastomosis in clinical practice, which has never been included in any pooled analysis to date.
The Kono-S anastomosis was first described in 2011 [7] the aim being to reduce surgical recurrence at the anastomotic site. It involves a combination of stapled and handsewn techniques utilizing a completely anti-mesenteric anastomosis. After stapled transection of ileum and colon, the two staple lines are simply approximated with interrupted sutures; two longitudinal enterotomies, 7–8 cm long, are performed and then closed in a transverse fashion. The mechanisms by which this configuration theoretically reduces recurrence are several: first, the mesenteric side of the bowel is completely excluded from the anastomotic lumen; it is known that Crohn’s disease always appears or recurs at the mesenteric bowel edge [8]. Second, the two staple lines are positioned at the back of the anastomosis providing an element of mechanical support to prevent anastomotic distortion. This prevents symptomatic stenosis if recurrent disease does occur. Third, the transverse closure creates a wide lumen anastomosis, similar to a strictureplasty. A potential fourth mechanism is the avoidance of any unnecessary devascularization and denervation of the remaining bowel ends which could theoretically lead to recurrence due to ischemia; the technique aims to spare the mesentery, ligating vessels as close to the bowel wall as possible.
In his first report, Kono et al. [7] demonstrated a dramatic reduction in the surgical recurrence rate from 15% to 0 at 5-year follow-up, when compared with a historical control cohort. These data are also confirmed at multivariate analysis and appear to be independent of the use of biologics. It should be emphasized that this anastomosis has not been proven to reduce endoscopic recurrence overall, but the recurrence is basically reduced, with lower Rutgeerts scores at endoscopic follow-up, thus avoiding the need for a reoperation.
These preliminary data have been confirmed in a larger multicenter study, including 187 patients coming from 4 hospitals from Japan and 1 from the USA. This study showed a surgical recurrence-free survival rate of 98.6% at long-term follow-up; nevertheless, this study is not comparative or randomized [9]. A more recent, comparative study from Shimada et al. [10] has again compared results after Kono-S anastomosis, performed in 117 patients and end-to-end anastomosis in 98 patients; all patients being consecutively operated on between 2006 and 2016. At a median follow-up of 54 months, 4 patients required a reoperation for anastomotic recurrence in the Kono-S group vs 24 in the end-to-end group (3.4 vs 24.4%); the 5-year surgery-free survival was, therefore, significantly higher after Kono-S anastomosis (95% vs 81.3%, p < 0.001), as confirmed at multivariate analysis. It should be mentioned that there are methodological weaknesses in all of these papers. None were randomized and all compared the intervention with a retrospectively gathered historical control group. Some of the reports may include the same patients as reported in earlier papers.
The Shimada paper showed another intriguing factor, which the authors suggest is the basis for surgical recurrence. They found a significantly lower leak rate in the Kono-S group (5.1% vs 17.3%). The rate in the control group is certainly higher than other studies report, but the fact that all leaks were treated conservatively might reflect particular accuracy in detecting complications on the part of these authors. Of relevance was the association between anastomotic leak and surgical recurrence. Patients with intra-abdominal septic complications, including anastomotic leakage, had a significantly higher surgical recurrence rate at 1, 2, 5 and 10 years (4%, 7%, 19% and 38%, respectively). The authors speculate that an additional inflammatory response may affect the mucosal healing after leakage; this abnormal inflammatory response may lead to excessive fibrosis, which may explain the stricture formation at the anastomotic site.
Part of the advantage of the Kono-S anastomosis lies in the theoretical role of the mesentery in inducing recurrence. Whilst Kono et al. believe in sparing the mesentery, Coffey et al. [11], have suggested the whole of the affected mesentery should be resected. Coffey et al. concluded that the inclusion of mesentery in the ileocolic resection specimen (similar to colon cancer surgery) is associated with a lower rate of surgical recurrence, compared to the standard surgery group where the mesentery is resected closer to the mesenteric border of the bowel (2.9% vs 40%, p = 0.003). They consider the key is local removal of mesenteric lymph nodes, which might trigger immunological input implicated in recurrence. Again, there are significant methodological weaknesses with this paper, the wide mesenteric group being compared with a historical pre-biological era control group. One should also mention the increased morbidity associated with the radical excision as well as the in difficulty carrying out such a resection laparoscopically.
Whilst the concept of close mesenteric ligation and wide excision could be considered contradictory, a linking feature could be that both techniques aim to exclude the affected mesentery from the anastomosis as far as possible. Kono seeks to do this with the configuration of the anastomosis whilst Coffey resects it.
Given the significant methodological flaws of all the trials, further higher quality trials are required before solid conclusions can be drawn about these novel techniques. Results from ongoing and novel designed randomized trials are certainly awaited with great interest to better assess the impact of anastomotic configuration, surgical techniques and leak rate on surgical recurrence in Crohn’s disease [12,13,14].
References
Choy PYG, Bissett IP, Docherty JG, Parry BR, Merrie AEH (2007) Stapled versus handsewn methods for ileocolic anastomoses. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004320.pub2
Simillis C, Purkayastha S, Yamamoto T, Strong SA, Darzi AW, Tekkis PP (2007) A meta-analysis comparing conventional end-to-end anastomosis vs. other anastomotic configurations after resection in Crohn’s disease. Dis Colon Rectum 50(10):1674–1687. https://doi.org/10.1007/s10350-007-9011-8
He X, Chen Z, Huang J et al (2014) Stapled side-to-side anastomosis might be better than handsewn end-to-end anastomosis in ileocolic resection for Crohn’s disease: a meta-analysis. Dig Dis Sci 59(7):1544–1551. https://doi.org/10.1007/s10620-014-3039-0
Feng JS, Li JY, Yang Z, Chen XY, Mo JJ, Li SH (2018) Stapled side-to-side anastomosis might be benefit in intestinal resection for Crohn’s disease. Medicine (United States). https://doi.org/10.1097/MD.0000000000010315
Bemelman WA, Warusavitarne J, Sampietro GM et al (2018) ECCO-ESCP consensus on surgery for Crohn’s disease. J Crohns Colitis. https://doi.org/10.1093/ecco-jcc/jjx061
Brown SR, Fearnhead NS, Faiz OD et al (2018) The Association of Coloproctology of Great Britain and Ireland consensus guidelines in surgery for inflammatory bowel disease. Color Dis. https://doi.org/10.1111/codi.14448
Kono T, Ashida T, Ebisawa Y et al (2011) A new antimesenteric functional end-to-end handsewn anastomosis: surgical prevention of anastomotic recurrence in Crohn’s disease. Dis Colon Rectum 54(5):586–592. https://doi.org/10.1007/DCR.0b013e318208b90f
Anthony A, Dhillon AP, Pounder RE, Wakefield AJ (1997) Ulceration of the ileum in Crohn’s disease: correlation with vascular anatomy. J Clin Pathol 50(12):1013–1017
Kono T, Fichera A, Maeda K et al (2016) Kono-S anastomosis for surgical prophylaxis of anastomotic recurrence in Crohn’s disease: an International Multicenter Study. J Gastrointest Surg 20(4):783–790. https://doi.org/10.1007/s11605-015-3061-3
Shimada N, Ohge H, Kono T et al (2019) Surgical recurrence at anastomotic site after bowel resection in Crohn’s disease: comparison of Kono-S and End-to-end anastomosis. J Gastrointest Surg. https://doi.org/10.1007/s11605-018-4012-6
Coffey JC, Kiernan MG, Sahebally SM et al (2018) Inclusion of the mesentery in ileocolic resection for Crohn’s disease is associated with reduced surgical recurrence. J Crohn’s Colitis. https://doi.org/10.1093/ecco-jcc/jjx187
Luglio G, Rispo A, Castiglione F et al (2016) Kono-type anastomosis in a patient with severe multi-recurrent Crohn’s disease. Int J Colorectal Dis. https://doi.org/10.1007/s00384-016-2567-9
Imperatore N, Rispo A, Luglio G, Bucci L, Castiglione F (2018) Letter: which risk factors for post-operative recurrence in Crohn’s disease can be modified? Aliment Pharmacol Ther. https://doi.org/10.1111/apt.14989
Michelassi F (2014) Crohn’s recurrence after intestinal resection and anastomosis. Dig Dis Sci. https://doi.org/10.1007/s10620-014-3096-4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Formal consent is not required for the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luglio, G., Corcione, F. Stapled versus handsewn methods for ileocolic anastomoses. Tech Coloproctol 23, 1093–1095 (2019). https://doi.org/10.1007/s10151-019-02105-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-019-02105-8