Abstract
Objective
Phase III clinical trials demonstrated the efficacy of enzalutamide and apalutamide in patients with non-metastatic castration-resistant prostate cancer (nmCRPC) and PSA doubling time ≤10 months. Although these drugs have been shown to vary in their adverse event (AE) profiles, the differences in their efficacy profiles remain to be evaluated. Therefore, this retrospective study was conducted to evaluate the efficacy of these drugs in patients with nmCRPC.
Methods
This study evaluated 191 patients with nmCRPC treated with enzalutamide (n = 137) or apalutamide (n = 54) in the first-line setting at Jikei University Hospital or its affiliated hospitals between May 2014 and November 2022. Endpoints were defined as oncological outcomes (i.e., PSA response, PFS, PSA-PFS, MFS, CSS, and OS) and AEs.
Results
No significant differences were noted in patient backgrounds between the two groups. Patients exhibiting a maximum PSA response of >50% and >90% accounted for 74.5% and 48.9% of patients in the enzalutamide group, and 75.9% and 42.6% of patients in the apalutamide group, respectively, with no significant difference between the groups. The median PSA-PFS was 10 months in the enzalutamide group but not in the apalutamide group, with no significant difference between the groups (P = 0.48). No significant differences were observed in MFS, CSS, or OS between the groups. Patients reporting AEs of all grades and grade 3 or higher accounted for 56.2% and 4.3% of those in the enzalutamide group and 57.4% and 7.4% of those in the apalutamide group, respectively. The most common AE was fatigue (26.3%) in the enzalutamide group and skin rash (27.8%) in the apalutamide group.
Conclusion
In this retrospective study of their efficacy and safety, enzalutamide and apalutamide were shown to exhibit comparable oncological outcomes but quite different AE profiles, suggesting that their differential use may be warranted based on these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PC) represents a significant healthcare burden as the most common solid cancer and the second most common cause of cancer-related mortality in men [1]. Systemic therapy involving androgen deprivation therapy (ADT) is the primary standard of care for patients with advanced PC, and the disease eventually progresses to castration-resistant prostate cancer (CRPC) despite adequate systemic therapy [2]. CRPC without metastases on conventional imaging was classified as non-metastatic CRPC (nmCRPC). In nmCRPC, preventing or delaying progression to metastatic disease remains an unmet clinical need. The phase III PROSPER, SPARTAN, and ARAMIS trials conducted in patients with high-risk nmCRPC demonstrated a significantly longer median metastasis-free survival (MFS) with androgen receptor signaling inhibitor (ARSI) agents (enzalutamide, apalutamide, or darolutamide) than with placebo [3,4,5]. Based on these results, current guidelines recommend these drugs for patients with nmCRPC and a prostate-specific antigen doubling time (PSADT) of <10 months. Of note, having been marketed in Japan in 2014 with indications for treating CRPC regardless of the presence of metastasis, enzalutamide and abiraterone have since been widely used in clinical practice in the country [6]. We have previously reported the results of a retrospective study comparing the efficacy of these ARAT agents before the release of their phase III trial results [7].
However, given that, to date, no head-to-head trials comparing these ARAT agents have been conducted and choosing the best treatment for each patient may pose challenges, we compared these treatments for nmCRPC in a network meta-analysis [8, 9]. As this network meta-analysis has many limitations despite the trials being compared with similar inclusion criteria, it is deemed essential to evaluate and compare the efficacy and safety profiles of these agents to inform treatment decisions and optimize patient outcomes using real-world data. Therefore, we conducted a multicenter retrospective study to compare the efficacy of enzalutamide and apalutamide in patients with nmCRPC.
Methods
Patients
This retrospective study included 191 patients with nmCRPC treated with enzalutamide or apalutamide as a first-line treatment at Jikei University Hospital or its affiliated hospitals between May 2014 and November 2022. All patients were histologically diagnosed with prostate adenocarcinoma and had previously undergone ADT in the form of medical or surgical castration. The onset of CRPC was defined as PSA and/or radiographic progression despite maintaining castration levels of serum testosterone [10,11,12]. No patients were confirmed to have metastasis at the time of CRPC diagnosis based on conventional imaging studies [computed tomography (CT), magnetic resonance imaging (MRI), and bone scintigraphy (BS)]. In Japan, enzalutamide was launched in May 2014 and apalutamide in May 2019. Therefore, enzalutamide was used for 5 years prior. After the launch of apalutamide, the choice of drug was left to the discretion of individual clinicians. This study was approved by the Institutional Review Board of the Jikei University School of Medicine, Tokyo, Japan (34-192 [11343]).
Outcome measures
The primary outcome measures were oncological outcomes, including PSA response, progression-free survival (PFS), PSA progression-free survival (PSA-PFS), MFS, cancer-specific survival (CSS), and overall survival (OS). PSA progression was defined as a 25% increase in PSA levels from the baseline or nadir PSA levels. PSA assessments are performed once every month, and imaging assessments (CT and BS) are performed every 3–6 months, as predetermined at baseline. The secondary outcome measure was adverse events (AEs).
Statistical analysis
Categorical variables are reported as frequencies and proportions. Continuous coded variables were reported as the median and interquartile range (IQRs). Patient demographics were compared between the groups using the t test, Pearson’s χ2 test and Fisher’s exact test. OS/CSS/PFS/PSA-PFS were graphically visualized using the Kaplan–Meier method. All differences between the groups were assessed for significance using the log-rank test. All P values were two-sided, and the level of significance was set at P < 0.05. Statistical analyses were performed using R version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria) and Stata/MP 14.2 statistical software (Stata Corp., College Station, TX, USA).
Results
Patient characteristics
The patient demographics are shown in Table 1. In total, 191 patients were enrolled in this study (median age, 72 years; initial PSA level, 30.64 ng/mL). The demographic and clinical characteristics of the patients at baseline were generally balanced. However, there were significant differences in BMI and median age at start of ARSI administration. The median follow-up durations were 25 and 20 months for the enzalutamide and apalutamide groups, respectively. CSS, OS, PFS, PSA-PFS, and MFS were analyzed for evaluable cases.
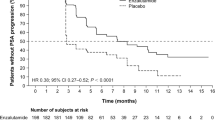
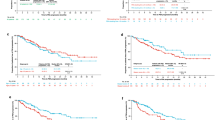
CSS
The use of enzalutamide and apalutamide did not significantly differently impact CSS in patients with nmCRPC (P = 0.93), with the hazard ratio (HR) for CSS shown to be 0.95 (95% confidence interval [CI], 0.33–3.41). The median CSS was not reached in both the apalutamide and enzalutamide groups (Fig. 1).
OS
No significant difference was shown in OS between the enzalutamide and apalutamide groups (P = 0.47), with the HR for OS shown to be 1.32 (95% CI, 0.61–3.29). The median OS was not reached for apalutamide and 83 months for the enzalutamide group (Fig. 1).
PFS (PSA–PFS, rPFS, clinical PFS)
Enzalutamide and apalutamide exhibited comparable effects on PFS among patients with nmCRPC (P = 0.49), with the HR for PFS shown to be 0.84 (95% CI 0.53–1.38), indicating no statistically significant difference in the risk of disease progression between the treatment groups. The median PFS was 22 months in the apalutamide group and 24 months in the enzalutamide group (Fig. 1).
PSA-PFS
No significant difference was observed in PSA-PFS between the enzalutamide and apalutamide groups (P = 0.49). The HR for PSA-PFS was 0.84 (95% CI 0.53–1.40), indicating a similar likelihood of PSA progression between the two treatment groups. The median PSA—PFS was 32 months in the apalutamide group and 24 months in the enzalutamide group (Fig. 1).
MFS
There was no significant difference in MFS between the enzalutamide and apalutamide groups (P = 0.14) with the HR for MFS shown to be 0.56 (95% CI 0.27–1.21). The median MFS was not reached for apalutamide and 80 months for enzalutamide group (Fig. 1). There were no significant differences in MFS with or without local treatment.
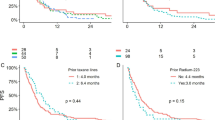
PSA response
No significant difference was observed between the enzalutamide and apalutamide groups in the proportion of patients achieving >90% reduction in PSA levels (P = 0.18), with similar results observed in the proportion of those achieving >50% or >70% reduction in PSA levels (Fig. 2).
AEs
No statistically significant difference was observed in the frequency of both overall and grade 3 or higher events between the treatment groups. However, it should be noted that the AE profiles differed significantly between the two groups, with rash being the most commonly reported AE in the apalutamide group (27.8%) and fatigue being the most frequently reported AE in the enzalutamide group (26.3%) (Table 2). All AE of Grade 3 or higher were Grade 3. In the enzalutamide group, 5 of 6 cases were fatigue and 1 case was hypertension. In the apalutamide group, all 4 cases were skin rashes, including one case of osteonecrosis of the jaw.
Discussion
We conducted a retrospective study to compare the efficacy of enzalutamide and apalutamide in patients with nmCRPC. Our study revealed similar oncological efficacy for both treatments. However, notable differences were observed in the AE profiles of the two drugs, and these distinct adverse event profiles offer important implications for clinical practice, suggesting that physicians should carefully weigh the potential side effects associated with each drug when selecting the appropriate treatment for individual patients. This highlights the need for shared decision-making between patients and healthcare providers to ensure an optimal balance between treatment efficacy and the tolerability of the treatment chosen [13].
Positive results have been reported with enzalutamide and apalutamide in the PROSPER and SPARTAN trials, respectively, demonstrating a significant MFS benefit (median MFS, 36.6 months with enzalutamide vs. 14.7 months with placebo in the PROSPER trial [HR for metastasis or death, 0.29; 95% CI 0.24–0.35; P < 0.001]); 40.5 months with apalutamide vs. 16.2 months with placebo in the SPARTAN trial [HR for metastasis or death, 0.28; 95% CI 0.23–0.35; P < 0.001]) [3, 4, 14, 15]. In light of these positive MFS outcomes, ARAT agents have now been deemed the standard of care, and their use is advised in clinical practice guidelines for patients with nmCRPC at high risk of developing metastasis (PSADT <10 months) to delay the time to metastasis [16, 17]. However, certain caution must be maintained when translating these trial results into clinical practice.
First, the PROSPER trial included only patients without lymph node enlargement (N0), whereas the SPARTAN trial included patients with lymph nodes measuring up to 2 cm in the short-axis diameter (N1) below the aortic bifurcation. Again, in light of the subgroup analyses of MFS and OS from these trials, which suggested potentially greater benefits of ARAT agents in patients with N1 disease than in those with N0 disease, it is likely that enzalutamide may have been unfairly undervalued for its efficacy compared to other agents. Although the PROSPER trial included no patients with N1 disease thought likely to benefit from ARAT agents, if it included a similar proportion of patients with N1 disease to that included in the SPARTAN trial (16%), they may have been associated with a more favorable HR for both MFS and OS. This must be validated and investigated in greater detail, drawing on more reliable data on the relevance of lymph node positivity and the therapeutic efficacy of these agents. Moreover, the inclusion criteria differed, with a minimum serum PSA level of 2 ng/mL included in the PROSPER trial and no minimum included in the SPARTAN trial.
Second, while the primary endpoint of these RCTs was defined as radiographic progression to metastatic disease and the study protocols required that no patients in the control arm received therapeutic intervention until radiographic progression to metastatic disease, this may have led to delays in the implementation of optimal intervention in these patients, and the differences in outcomes between the investigational and control arms may have been smaller if those in the control arm had received timely intervention. In addition, 48% and 65% of all patients in the PROSPER trial received effective anticancer interventions at median follow-ups of 15.1 months and 48 months, respectively. In contrast, many more patients received effective therapy in the SPARTAN trial (77.7% and 84% at median follow-ups of 20.3 months and 50.4 months, respectively). The proportions in the SPARTAN trial were similar to those observed in real-world clinical settings, suggesting that appropriate interventions were implemented in the SPARTAN trial. Therefore, clinicians should interpret the HRs for OS in these trials, considering the differences in the proportions of effective anticancer interventions.
To summarize, the results of the PROSPER and SPARTAN trials demonstrated that both enzalutamide and apalutamide positively affect the oncological outcomes of patients [3, 4, 14, 15]. Although both agents exhibited similar effectiveness in terms of oncological outcomes, our study identified differences in their AE profiles, which may be attributed to slight differences in their molecular structures, with the skin rash observed with apalutamide potentially linked to these subtle distinctions [18]. Apalutamide, but not enzalutamide, was shown to react with various protein sources (plasma, hepatocytes, and bovine serum albumin) in a series of binding experiments [19]. Apalutamide was shown to produce positive responses in a mouse model used to test for hypersensitivity reactions. However, this was not the case with enzalutamide or analog 1 when evaluated in the same mouse model. Taken together, the clinical characteristics of apalutamide associated with the occurrence of rash and findings from structural studies combine to support the hypothesis that the 2-cyanopyridine moiety in apalutamide may react with proteins, thus eliciting an immune-mediated response that manifests as a rash exhibiting the characteristics of type IV delayed hypersensitivity.
Overall, our retrospective study may be of interest in that it provides valuable insights into the comparative efficacy and AE profiles of enzalutamide and apalutamide in patients with nmCRPC. Further prospective investigations involving larger cohorts and longer follow-up periods are required to validate and expand upon these findings.
Limitation
A major limitation of our study was the relatively small number of cases included in the analyses. In addition, enzalutamide was launched in Japan five years before apalutamide, which inevitably leads to a shorter follow-up period for apalutamide. On the other hand, the 25 month follow-up period for enzalutamide was shorter than the difference in launch date. The reason was that our cohort incorporated more cases that were increased as a result of the PROSPER trial published in 2018.
In terms of patient background, there were differences in BMI and median age at start of ARSI administration; for BMI, the apalutamide group was higher, possibly due to avoidance of skin rashes in skinny patients when selecting the drug. The median age at start of ARSI administration was older in the apalutamide group, possibly due to avoidance of enzalutamide-induced fatigue in older patients, or due to a delay in the launch of apalutamide. These could constrain the applicability of our findings and limit the statistical power of certain analyses. A larger sample size should generate more robust evidence and allow subgroup analyses to explore factors potentially influencing treatment outcomes. Another limitation is the variability in follow-up duration between patients receiving enzalutamide or apalutamide. Thus, differing follow-up durations could have introduced bias and affected the accuracy of the outcomes reported herein; longer-term follow-up should provide a more reliable picture of treatment effects and potential late adverse events. In addition, basic research suggests the superiority of darolutamide over apalutamide or enzalutamide because of its higher biological activity, as assessed by its affinity for AR or its antiproliferative effects against VCap cells because of its lower penetration through the blood–brain barrier [20,21,22]. While our study fell short of addressing these issues, further studies are strongly anticipated to delve closely into these features.
In addition to these limitations, the accurate distinction between non-metastatic and metastatic diseases based solely on conventional imaging studies could pose challenges due to their limited sensitivity. Over 90% of men with nmCRPC diagnosed based on conventional imaging were ultimately observed to have metastases using prostate-specific membrane antigen positron emission tomography (PSMA-PET) in a retrospective series [23]. Thus, the patients included in this study should have had low-volume metastatic disease rather than nmCRPC, and the primary endpoint of progression to metastases on conventional imaging is becoming less relevant as PSMA-PET imaging is becoming increasingly used in clinical settings.
References
Siegel RL, Miller KD (2020) Jemal A (2020) Cancer statistics. CA Cancer J Clin 70(1):7–30. https://doi.org/10.3322/caac.21590
Kluth LA, Shariat SF, Kratzik C et al (2014) The hypothalamic-pituitary-gonadal axis and prostate cancer: implications for androgen deprivation therapy. World J Urol 32(3):669–676. https://doi.org/10.1007/s00345-013-1157-5
Sternberg CN, Fizazi K, Saad F et al (2020) Enzalutamide and survival in nonmetastatic, castration-resistant prostate cancer. N Engl J Med 382(23):2197–2206. https://doi.org/10.1056/NEJMoa2003892
Smith MR, Saad F, Chowdhury S et al (2021) Apalutamide and overall survival in prostate cancer. Eur Urol 79(1):150–158. https://doi.org/10.1016/j.eururo.2020.08.011
Fizazi K, Shore N, Tammela TL et al (2020) Nonmetastatic, castration-resistant prostate cancer and survival with darolutamide. N Engl J Med 383(11):1040–1049. https://doi.org/10.1056/NEJMoa2001342
Mori K, Kimura T, Fukuokaya W et al (2020) Values of alkaline phosphatase at the diagnosis of castration resistance and response to primary androgen deprivation therapy as predictors of subsequent metastasis in non-metastatic castration-resistant prostate cancer. Int J Clin Oncol 25(3):479–485. https://doi.org/10.1007/s10147-019-01541-8
Mori K, Kimura T, Ito K et al (2018) Earlier use of androgen receptor-axis-targeted drugs may improve overall survival in patients with non-metastatic castration-resistant prostate cancer. Prostate 78(10):766–772. https://doi.org/10.1002/pros.23534
Mori K, Mostafaei H, Pradere B et al (2020) Apalutamide, enzalutamide, and darolutamide for non-metastatic castration-resistant prostate cancer: a systematic review and network meta-analysis. Int J Clin Oncol 25(11):1892–1900. https://doi.org/10.1007/s10147-020-01777-9
Mori K, Quhal F, Katayama S et al (2022) Androgen receptor axis-targeted agents for non-metastatic castration-resistant prostate cancer impact on overall survival and safety profile. Minerva Urol Nephrol 74(3):292–301. https://doi.org/10.23736/s2724-6051.21.04431-1
Scher HI, Halabi S, Tannock I et al (2008) Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol 26(7):1148–1159. https://doi.org/10.1200/jco.2007.12.4487
Sweeney CJ, Chen YH, Carducci M et al (2015) Chemohormonal Therapy in Metastatic Hormone-Sensitive Prostate Cancer. N Engl J Med 373(8):737–746. https://doi.org/10.1056/NEJMoa1503747
Cornford P, Bellmunt J, Bolla M et al (2017) EAU-ESTRO-SIOG guidelines on prostate cancer. Part II: treatment of relapsing, metastatic, and castration-resistant prostate cancer. Eur Urol 71(4):630–642. https://doi.org/10.1016/j.eururo.2016.08.002
Mori K, Mostafaei H, Sari Motlagh R et al (2022) Systemic therapies for metastatic hormone-sensitive prostate cancer: network meta-analysis. BJU Int 129(4):423–433. https://doi.org/10.1111/bju.15507
Hussain M, Fizazi K, Saad F et al (2018) Enzalutamide in men with nonmetastatic, castration-resistant prostate cancer. N Engl J Med 378(26):2465–2474. https://doi.org/10.1056/NEJMoa1800536
Smith MR, Saad F, Chowdhury S et al (2018) Apalutamide treatment and metastasis-free survival in prostate cancer. N Engl J Med 378(15):1408–1418. https://doi.org/10.1056/NEJMoa1715546
Mottet N, van den Bergh RCN, Briers E et al (2021) EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer-2020 update. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 79(2):243–262. https://doi.org/10.1016/j.eururo.2020.09.042
Cornford P, van den Bergh RCN, Briers E et al (2021) EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer. Part II-2020 update: treatment of relapsing and metastatic prostate cancer. Eur Urol 79(2):263–282. https://doi.org/10.1016/j.eururo.2020.09.046
Ji C, Guha M, Zhu X et al (2020) Enzalutamide and apalutamide: in vitro chemical reactivity studies and activity in a mouse drug allergy model. Chem Res Toxicol 33(1):211–222. https://doi.org/10.1021/acs.chemrestox.9b00247
Guha M, Ji C, Zhu X et al (2019) 1892P—Enzalutamide (ENZA) and apalutamide (APA) in vitro chemical reactivity studies and activity in a mouse drug allergy model (MDAM). Ann Oncol 30:v767–v768. https://doi.org/10.1093/annonc/mdz268.019
Moilanen AM, Riikonen R, Oksala R et al (2015) Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies. Sci Rep 5:12007. https://doi.org/10.1038/srep12007
Pajouhesh H, Lenz GR (2005) Medicinal chemical properties of successful central nervous system drugs. NeuroRx J Am Soc Exp NeuroTher 2(4):541–553. https://doi.org/10.1602/neurorx.2.4.541
Yu J, Zhou P, Hu M et al (2019) Discovery and biological evaluation of darolutamide derivatives as inhibitors and down-regulators of wild-type AR and the mutants. Eur J Med Chem 182:111608. https://doi.org/10.1016/j.ejmech.2019.111608
Fendler WP, Weber M, Iravani A et al (2019) Prostate-specific membrane antigen ligand positron emission tomography in men with nonmetastatic castration-resistant prostate cancer. Clin Cancer Res 25(24):7448–7454. https://doi.org/10.1158/1078-0432.ccr-19-1050
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Takahiro Kimura is a paid consultant/advisor of Astellas, Bayer, Janssen and Sanofi.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Hara, S., Mori, K., Fukuokaya, W. et al. Effectiveness and safety of enzalutamide and apalutamide in the treatment of patients with non-metastatic castration-resistant prostate cancer (nmCRPC): a multicenter retrospective study. Int J Clin Oncol 29, 1191–1197 (2024). https://doi.org/10.1007/s10147-024-02548-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-024-02548-6