Abstract
Background
Proton pump inhibitors (PPIs) may be associated with gastric cancer, but studies in recent years have proven still inconsistent results. We conducted a systematic review and meta-analysis to investigate the association between PPI use and gastric cancer.
Methods
Pubmed, EMBASE, and Cochrane library were searched for studies published up to 15th February 2022. Studies on the association between PPI and the risk of gastric cancer, pooled the odds ratios (ORs) using a random-effects model. The subgroup analysis for study design, site of gastric cancer, and the duration of PPI use was performed. Heterogeneity was assessed using the I2 and Cochran’s Q statistics.
Results
Sixteen cohorts and case–control studies were included. PPI use was significantly associated with gastric cancer (OR: 1.75, 95% CI: 1.28–2.40). The subgroup analysis found a significant risk increase in non-cardia gastric cancer (OR: 2.14, 95%CI: 1.50–3.07). There was no duration-dependent effect of PPI use and gastric cancer risk (< 1 year: OR: 2.56, 95% CI: 1.41–4.64, I2 = 98%; 1–3 years: OR: 1.47, 95% CI: 1.26–1.71, I2 = 41%; > 3 years: OR: 1.58, 95% CI: 1.16–2.14, I2 = 74%).
Conclusions
PPIs were significantly associated with an increased risk of gastric cancer. However, this association does not confirm causation. Several well-design studies are needed to confirm the findings in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Proton pump inhibitors (PPIs) have been extensively prescribed for excessive gastric acid [1]. PPIs were clinically prescribed for peptic ulcer, gastroesophageal reflux disease, dyspepsia, and Helicobacter pylori (H. Pylori) eradication [2,3,4]. In addition, patients exposed to some drugs (aspirin, non-steroidal anti-inflammatory drugs, etc.) consider taking PPI to prevent ulcers. PPIs have been considered to be safe for clinical use [5]. However, an increasing number of observational studies on the risk of gastric cancer in patients taking long-term PPI therapy.
Gastric cancer is the sixth most common cancer and the third leading cause of cancer-related mortality worldwide [6]. There are many risk factors for stomach cancer, such as Helicobacter pylori infections, dietary habits, smoking, obesity, and atrophic gastritis. An association between gastric cancer and PPI use has been found for many years. The previous meta-analysis pooled large observational studies and found a 2.5-fold increased gastric cancer risk [7, 8]. The mechanisms of PPI therapy with the risk of gastric cancer are not well understood and have drawn attention. Due to three new shreds of evidence from the United Kingdom [9] and Korea [10, 11], we performed an updated systematic review and meta-analysis. This study aims to evaluate the available data on the suggested association between PPIs and gastric cancer through a meta-analysis.
Methods
Ethical statement
Ethical approval and informed consent are not required, as the study will be a literature review and will not involve direct contact with patients or alterations to patient care.
Literature search strategy
We performed literature searches in PubMed, Cochrane Library, Embase, and ClinicalTrials.gov through 15th February 2022, limiting to human patients and publications in English. The following search terms were included in the search: “proton pump inhibitor”, “omeprazole”, “esomeprazole”, pantoprazole”, “lansoprazole”, “dexlansoprazole”, “rabeprazole”, “gastric cancer”, “gastric carcinoma”, “gastric adenocarcinoma”, “gastric neoplasm”, “gastric neoplasia”, “stomach cancer”, “stomach carcinoma”, “stomach adenocarcinoma”, “stomach neoplasm” and “stomach neoplasia”. All retrieved abstracts, studies, and citations were reviewed. The details of the search strategy for eligible studies are given in the flowchart provided by Preferred Reporting Items for Systematic Reviews and Meta-Analyses [12]. Two reviewers (T. W. W. and T. R. P.) screened all titles and abstracts independently and evaluated relevant articles.
Inclusion and exclusion criteria
We included trials that met the following criteria: (1) observational studies (case–control studies or cohort studies); (2) defined use of PPIs (users and non-users); (3) defined outcomes of gastric or stomach cancers; (4) data were reported with standardized incidence ratio (SIR), relative risk (RR), hazard ratio (HR) or odds ratio (OR) for risk of gastric or stomach cancers and with the 95% confidence interval (CI). We excluded studies with any of the following features (1) literature review or case reports; (2) no related data in the study; (3) studies on other malignant gastric tumors.
Data extraction
This study was performed by Cochrane Collaboration guidelines [13]. Two reviewers (T. W. W. and T. R. P.) extracted data independently. The following information was extracted, including first author, year of publication, study design, country, number, and mean age of the included population, period, and lag time.
Risk of bias of included studies
Two reviewers (T. W. W. and T. R. P.) independently assessed the quality of the included studies. The Newcastle–Ottawa scale was used to assess the quality of observational studies [14]. This scale evaluated the quality from the following 3 aspects: reporting of participant selection, comparability, and outcome assessment. The total quality scale was 9 points. The outcome was considered high quality for studies with ≥ 6 points.
Statistical analyses
Statistical analysis was performed according to the Cochrane Handbook for Statistical Review of Interventions (version 6.2) [13]. The statistical analyses were performed using RevMan software (Cochrane Review Manager Version 5.4, Oxford, UK) and Comprehensive Meta-Analysis software. The odds ratios (ORs) were used as the common measure of association across studies. As the incidence of cancer is rare, SIRs, HR, OR, and RR were treated as equivalent measures of risk estimates [15,16,17]. The pooled adjusted ORs were calculated by DerSimonian–Laird random-effects meta-analysis [18]. We assessed heterogeneity using a χ2 test with p < 0.10 considered statistically significant. Heterogeneity was considered low, moderate, or high for I2 values of < 25, 25–50, and > 50%, respectively. Results were considered statistically significant with a p-value of < 0.1. Subgroup analysis was performed according to different study designs, different sites of gastric cancer, duration of PPIs use, and H. pylori infection status. We used a funnel plot to assess the publication bias. Egger’s and Begg’s tests were also used. A p-value of > 0.05 based on the results of Egger’s and Begg’s tests indicated the absence of publication bias.
Ethics approval
Ethics approval was not required for this study since the analyzed data had been published previously.
Results
Studies retrieved
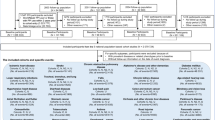
The initial search using electronic databases and manual searching retrieved 2,179 peer-reviewed articles and abstracts. After Records were removed before screening and removing duplicates, 308 records remained. Preliminary screening of titles and abstracts resulted in 54 remaining articles, and a further 36 review articles, case reports, and studies not meeting the inclusion and exclusion criteria were rejected upon detailed evaluation. Of the 18 remaining records, 3 were excluded due to a lack of sufficient relevant data. The remaining 15 contained data relating to the prevalence of gastric cancer in PPI users or PPI use in subjects with gastric cancer. Figure 1 is a detailed flow diagram of the selection process described.
Study characteristics
A summary of the study characteristics is provided in Table 1. A total of 2,936,935 subjects from 15 studies were included and one study included 2 different study designs (population-based, and case–control studies). Eight were cohort studies, eight were case–control studies. The sixteen studies were from different regions: seven from Asia, six from Europe, and three from America. PPI is used after H. pylori eradication among three of the included studies [10, 24, 25]. Most studies did not report on the age distribution of participants and the type or dose of PPIs. The risk-of-bias assessment results of the 16 included trials are summarized in Table 2.
Association between PPI use and gastric cancer
All of the 16 studies contained information on PPIs and gastric cancer risk. This meta-analysis of all 16 studies revealed that PPIs users was associated with an increased risk of gastric cancer than PPIs non-users (OR: 1.75, 95% CI: 1.28–2.40, I2 = 97%; p < 0.001; Fig. 2). We also performed analyses of different study designs (cohort studies vs. case–control studies). Compared to PPI users in the case–control studies (OR: 1.54, 95% CI: 1.30–1.84, I2 = 73%; Fig. 3), PPI users in the cohort studies (OR: 2.00, 95% CI: 1.17–3.41, I2 = 98%) had a higher risk of gastric cancer.
Association between PPI use and gastric cancer according to the gastric cancer site
Seven out of 16 studies contributed to a stratified meta-analysis according to the gastric cancer site. There was a significant increase risk in non-cardia gastric cancer (OR: 2.14, 95% CI: 1.50–3.07, I2 = 77%) with a non-significant trend towards an increased risk in the cardia (OR: 1.45, 95% CI: 0.77–2.74, I2 = 90%; Fig. 4).
Association between PPI use and gastric cancer according to PPI duration
Eleven out of 16 studies contributed to a stratified meta-analysis according to the PPI duration. There was no duration-dependent effect of PPI use and risk of gastric cancer (< 1 year: OR: 2.56, 95% CI: 1.41–4.64, I2 = 98%; 1–3 years: OR: 1.47, 95% CI: 1.26–1.71, I2 = 41%; > 3 years: OR: 1.58, 95% CI: 1.16–2.14, I2 = 74%; Fig. 5).
Association between PPI use and gastric cancer according to H. pylori infection status
Eight out of 16 studies contributed to a stratified meta-analysis according to PPI use and H. pylori infection status. A higher risk of gastric cancers was observed in individuals who received PPI therapy even after H. pylori eradication (OR: 2.67, 95% CI: 1.79–4.0, I2 = 0%; Fig. 6). There was no significant risk increase in PPI users with or without H. pylori eradication treatment (OR: 2.14, 95% CI: 0.62–7.46, OR: 0.97, 95% CI: 0.49–1.89, respectively; Fig. 6).
Sensitivity analysis
Sixteen studies were included in this study. A total of 14 included studies that data were reported with HR and OR for risk of gastric cancer. Only 2 studies used incidence rate ratios (IRRs) or SIR to estimate the risk of gastric cancer [21, 23]. Therefore, we will carry out a sensitivity analysis by excluding these 2 studies. When these 2 studies were removed from this meta-analysis, similar results were shown in the risk of gastric cancer (OR: 1.57, 95% CI: 1.33–1.85, I2 = 80%).
Publication bias
A visual inspection of the funnel plot of OR from these studies revealed asymmetry (Fig. 7). However, neither Egger’s nor Begg’s test suggested statistical evidence of publication bias, with p values of 0.101 and 0.086, respectively.
Discussion
In the previous study, data pooled from 13 studies demonstrated that PPI users are more than twice as likely to develop gastric cancer as non-PPI users [32]. The possible mechanisms of PPIs cause gastric cancer because significantly reduce gastric acid and lead to increase secretion of gastrin. An animal study found that hypergastrinemia may cause acid suppression and result from hyperplasia of enterochromaffin-like cells [33]. Hypergastrinemia commonly occurs in PPIs user, and the relation to the risk of gastric cancer is still controversial [34]. Another mechanism is to decrease gastric acidity by PPIs therapy may result in bacterial overgrowth in the gut. Studies have proven that gastric bacterial overgrowth is predictive of many clinical diseases, including lung, liver disease, and cancer [35, 36].
Many previous meta-analyses have explored the relationship between PPI and gastric cancer, but their results are inconsistent. The results of them are all based on a small number of observational studies [8, 37,38,39]. The latest meta-analysis conducted by Segna et al. includes thirteen studies on the association between PPI use and the risk of gastric cancer [32]. Our study was supplemented with five recent observational studies [9,10,11, 31], thus making the overall meta-analysis more complete and the subgroup analysis was more robust. A meta-analysis based on seven trials evaluated the effects of PPIs use and gastric mucosa changes [40]. This study shows no clear evidence that the long-term use of PPIs can cause the progression of corpus gastric atrophy or intestinal metaplasia. In addition, PPI maintenance treatment may have a higher possibility of experiencing enterochromaffin-like cell hyperplasia. However, long-term PPI therapy-induced moderate hypergastrinemia in most patients and an increased prevalence of enterochromaffin-like cell hyperplasia [41].
According to the Bradford Hill criteria, the biological gradient (dose–response) is one of the important criteria confirming a causal relationship [42]. However, there was no duration-dependent effect of PPI use and risk of gastric cancer in our study. Our study did not meet the Bradford Hill criteria, so it is difficult to confirm the causal relationship. Therefore, there are still doubts about PPIs and the risk of gastric cancer. Whether PPIs and Helicobacter pylori have synergistic effects to cause gastric cancer is also a highly concerning issue. Long-term use of PPIs may cause non-H pylori bacterial overgrowth; exacerbates gastritis because of the infection with H. pylori and non-H. pylori bacterial species [43]. H. pylori-driven gastric inflammation has been seeming to be a risk of gastric cancer [44]. Patients with H. pylori infection and PPIs therapy may worsen gastritis, thereby increasing the risk of atrophic gastritis. Therefore, if H. pylori are eradicated, long-term use of PPI may develop gastric cancer. In our subgroup study, we also found that long-term use of PPI after H. pylori were eradicated was associated with nearly three times the risk of gastric cancer.
Our subgroup analysis found that long-term use of PPI is increased the risk of non-cardia gastric cancer. The majority of non-cardia gastric cancers are related to peptic ulcers and chronic mucosal infections caused by H. pylori [19]. This may explain the strong relationship between the long-term use of PPIs and the development of non-cardia gastric cancer.
This study has some limitations. First, cohort and case–control studies were included in this meta-analysis. We cannot assess the causal relationship between PPIs and gastric cancer risk. Second, the results have potential confounders, such as the result from several studies and adjusted outcomes with different covariates. Third, the type and dose of PPI were not reported in the included studies. Fourth, some of the studies included in this study did not provide risk estimates or reported incomplete information. However, these unadjusted point estimates may pose a risk of confounding and are responsible for the high heterogeneity of this study. Therefore, the results should be interpreted cautiously. However, we performed a sensitivity analysis combining studies reporting OR and HR, which indicated consistent results. Fifth, information on precancerous lesions such as intestinal dysplasia and metaplasia were not provided in most included studies [19,20,21, 26, 28, 30], which may be prone to long-term use of PPIs and gastric cancer. Finally, overestimating the risk of occurrence is due to confounding. Sixth, there is a lack of information on many important risk factors such as smoking, drinking, eating habits, and H. pylori infection.
Conclusions
This meta-analysis found that PPIs were significantly associated with an increased risk of gastric cancer. However, this association does not confirm causation. Further well-design studies are needed to confirm the findings in the future.
Data availability
All data, models, and code generated or used during the study appear in the submitted article.
References
Pham CQ, Regal RE, Bostwick TR, et al. (2006) Acid suppressive therapy use on an inpatient internal medicine service, Ann Pharmacother 40: 1261e6.
Kuna L, Jakab J, Smolic R et al (2019) Peptic ulcer disease: a brief review of conventional therapy and herbal treatment options. J Clin Med 8(2):179
Maret-Ouda J, Markar SR, Lagergren J (2020) Gastroesophageal reflux disease: a review. JAMA 324(24):2536–2547
Yun J, Wu Z, Qi G et al (2021) The high-dose amoxicillin-proton pump inhibitor dual therapy in eradication of Helicobacter pylori infection. Expert Rev Gastroenterol Hepatol 15(2):149–157
Farrell B, Pottie K, Thompson W et al (2017) Deprescribing proton pump inhibitors: evidence-based clinical practice guideline. Can Fam Physician 63:354–364
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Song HJ, Jeon N, Squires P (2020) The association between acid-suppressive agent use and the risk of cancer: a systematic review and meta-analysis. Eur J Clin Pharmacol 76(10):1437–1456
Wan QY, Wu XT, Li N et al (2019) Long-term proton pump inhibitors use and risk of gastric cancer: a meta-analysis of 926386 participants. Gut 68(4):762–764
Abrahami D, McDonald EG, Schnitzer ME et al (2022) Proton pump inhibitors and risk of gastric cancer: population-based cohort study. Gut 71(1):16–24
Seo SI, Park CH, You SC et al (2021) Association between proton pump inhibitor use and gastric cancer: a population-based cohort study using two different types of nationwide databases in Korea. Gut 70(11):2066–2075
Shin GY, Park JM, Hong J et al (2021) Use of proton pump inhibitors vs Histamine 2 receptor antagonists for the risk of gastric cancer: population-based cohort study. Am J Gastroenterol 116(6):1211–1219
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Higgins JPT, Thomas J, Chandler J, et al. (editors) (2021) Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, available at https://www.training.cochrane.org/handbook.
Wells GA, Shea B, O’Connell D, et al. (2014) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses, available at http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Greenland S (1987) Quantitative methods in the review of epidemiologic literature. Epidemiol Rev 9: 130.
Grant RL (2014) Converting an odds ratio to a range of plausible relative risks for better communication of research findings. BMJ 348:f7450
Ronksley PE, Brien SE, Turner BJ et al (2011) Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 342:d671
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
García Rodríguez LA, Lagergren J, Lindblad M (2006) Gastric acid suppression and risk of oesophageal and gastric adenocarcinoma: a nested case control study in the UK. Gut 55:1538–1544
Tamim H, Duranceau A, Chen LQ et al (2008) Association between use of acid-suppressive drugs and risk of gastric cancer. Drug Saf 31:675–684
Poulsen AH, Christensen S, McLaughlin JK et al (2009) Proton pump inhibitors and risk of gastric cancer: a population-based cohort study. Br J Cancer 100:1503–1507
Brusselaers N, Wahlin K, Engstrand L et al (2017) Maintenance therapy with proton pump inhibitors and risk of gastric cancer: a nationwide population-based cohort study in Sweden. BMJ Open 7:e017739
Brusselaers N, Lagergren J, Engstrand L (2019) Duration of use of proton pump inhibitors and the risk of gastric and oesophageal cancer. Cancer Epidemiol 62:101585
Cheung KS, Chan EW, Wong AYS et al (2018) Long-term proton pump inhibitors and risk of gastric cancer development after treatment for Helicobacter pylori: a population-based study. Gut 67:28–35
Niikura R, Hayakawa Y, Hirata Y et al (2017) Long term proton pump inhibitor use is a risk factor of gastric cancer after treatment for Helicobacter pylori: a retrospective cohort analysis. Gut 22:22
Lai SW, Lai HC, Lin CL et al (2019) Proton pump inhibitors and risk of gastric cancer in a case control study. Gut 68:765–767
Peng YC, Huang LR, Lin CL et al (2019) Association between proton pump inhibitors use and risk of gastric cancer in patients with GERD. Gut 68:374–376
Chien LN, Huang YJ, Shao YH et al (2016) Proton pump inhibitors and risk of periampullary cancers: a nested case-control study. Int J Cancer 138:1401–1409
Lee JK, Merchant SA, Schneider JL et al (2020) Proton pump inhibitor use and risk of gastric, colorectal, liver, and pancreatic cancers in a community based population. Am J Gastroenterol 115:706–715
Liu P, McMenamin ÚC, Johnston BT et al (2020) Use of proton pump inhibitors and histamine-2 receptor antagonists and risk of gastric cancer in two population-based studies. Br J Cancer 123:307–315
Duan L, Wu AH, Sullivan-Halley J et al (2009) Antacid drug use and risk of esophageal and gastric adenocarcinomas in Los Angeles County. Cancer Epidemiol Biomarkers Prev 18(2):526–533
Segna D, Brusselaers N, Glaus D et al (2021) Association between proton-pump inhibitors and the risk of gastric cancer: a systematic review with meta-analysis. Therap Adv Gastroenterol 14:17562848211051464
Havu N (1986) Enterochromaffin-like cell carcinoids of gastric mucosa in rats after life-long inhibition of gastric secretion. Digestion 35:42–55
Schenk BE, Kuipers EJ, Klinkenberg-Knol EC et al (1998) Hypergastrinaemia during long-term omeprazole therapy: influences of vagal nerve function, gastric emptying and Helicobacter pylori infection. Aliment Pharmacol Ther 12:605–612
Rosen R, Amirault J, Liu H et al (2014) Changes in gastric and lung microflora with acid suppression: acid suppression and bacterial growth. JAMA Pediatr 168(10):932–937
Bajaj JS (2019) Alcohol, liver disease and the gut microbiota. Nat Rev Gastroenterol Hepatol 16(4):235–246
Islam MM, Poly TN, Walther BA et al (2018) Adverse outcomes of long-term use of proton pump inhibitors: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol 30(12):1395–1405
Tran-Duy A, Spaetgens B, Hoes AW et al (2016) Use of proton pump inhibitors and risks of fundic gland polyps and gastric cancer: systematic review and meta-analysis. Clin Gastroenterol Hepatol 14(12):1706-1719.e5
Jiang K, Jiang X, Wen Y et al (2019) Relationship between long-term use of proton pump inhibitors and risk of gastric cancer: a systematic analysis. J Gastroenterol Hepatol 34(11):1898–1905
Song H, Zhu J, Lu D (2014) Long-term proton pump inhibitor (PPI) use and the development of gastric pre-malignant lesions. Cochrane Database Syst Rev 12: CD010623.
Lundell L, Vieth M, Gibson F et al (2015) Systematic review: the effects of long-term proton pump inhibitor use on serum gastrin levels and gastric histology. Aliment Pharmacol Ther 42(6):649–663
Ab HILL (1965) The environment and disease: association or causation. Proc R Soc Med 58(5):295–300
Sanduleanu S, Jonkers D, De Bruine A et al (2001) Double gastric infection with Helicobacter pylori and non-Helicobacter pylori bacteria during acid-suppressive therapy: increase of proinflammatory cytokines and development of atrophic gastritis. Aliment Pharmacol Ther 15:1163–1175
Song H, Ekheden IG, Zheng Z et al (2015) Incidence of gastric cancer among patients with gastric precancerous lesions: observational cohort study in a low risk Western population. BMJ 351:h3867
Acknowledgements
This study was supported by grants from the Taipei Tzu Chi Hospital, and Buddhist Tzu Chi Medical Foundation (TCRD-TPE-111-53 & TCRD-TPE-111-54).
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
TRP wrote the first draft of the manuscript. TWW and TRP searched databases and extracted the data. TWW and TRP evaluated the risk of bias. TWW and TRP performed the statistical analysis. CHL and TWW critically revised the manuscript. All authors contributed to the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Peng, TR., Wu, TW. & Li, CH. Association between proton-pump inhibitors and the risk of gastric cancer: a systematic review and meta-analysis. Int J Clin Oncol 28, 99–109 (2023). https://doi.org/10.1007/s10147-022-02253-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-022-02253-2