Abstract
Background
Pancreatic fistula is one of the most common and potentially fatal surgical complications after radical gastrectomy. The purpose of this study was to assess the validity of extrapolating the definition of pancreatic fistula by the International Study Group on Pancreatic Surgery to include situations surrounding gastric cancer surgery.
Methods
The clinicopathological data of 443 patients who underwent elective gastrectomy with suprapancreatic lymph node dissection (D1+, D2, or D2+ dissection) without pancreatic resection were reviewed. The relationship between postoperative pancreas-related complications (PPRC) and laboratory data, including drain fluid amylase levels on postoperative day 1 (dAmy1) and day 3 (dAmy3), were investigated.
Results
Twenty-four patients (5.4%) developed PPRC of ≥ grade II according to Clavien–Dindo classification. Among them, 15 patients had dAmy3 levels ≥ 375 IU/L, while all 24 patients had dAmy1 levels ≥ 375 IU/L. None of the patients with dAmy1 levels < 375 IU/L developed PPRC. The area under the curve of dAmy1 and dAmy3, calculated by drawing receiver operating characteristic curves, were 0.896 and 0.791, respectively. Univariate and multivariate analyses demonstrated that both dAmy1 and dAmy3 were significant predictors of PPRC; however, dAmy1 (p < 0.001) was more strongly correlated with PPRC than dAmy3 (p = 0.049).
Conclusions
DAmy1 is more sensitive than dAmy3 as an indicator of pancreatic fistula after gastric cancer surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radical gastrectomy with lymph node dissection remains the mainstay of treatment for resectable gastric cancer [1]. However, lymph node dissection around the pancreas may cause minute trauma or burns on the surface of the pancreas, causing a postoperative pancreatic fistula. Pancreatic fistula is one of the most common and potentially fatal surgical complications after radical gastrectomy, and the incidence of pancreatic fistula has been reported to be 2–12.6% after open radical gastrectomy in large clinical trials [2, 3]. According to a recent nationwide survey, the incidence of grade B or higher pancreatic fistula according to the International Study Group on Pancreatic Surgery (ISGPS) after laparoscopic distal gastrectomy was 2.2% [4]. In addition, after robotic gastrectomy, pancreatic fistula of grade II or higher according to the Clavien–Dindo (CD) classification occurred in 3.7% of patients [5].
Pancreatic fistula is defined as an abnormal communication between the pancreatic ductal system and another epithelial surface containing a pancreas-derived enzyme-rich fluid. The diagnosis of the pancreatic fistula is given using the criteria of the ISGPS as follows: “Output via an operatively-placed drain of any measurable volume of drain fluid on or after postoperative day 3, with amylase activity greater than 3 times the upper normal serum value for each specific institution.” When this condition leads to clinically relevant, it is called a pancreatic fistula [6]. However, this definition is based on the experience of pancreatic resection, in which drains are usually placed near the cut end of the pancreas, and pancreatic fistula usually represents a failure of healing of a pancreatic-enteric anastomosis [7] or the “cut end” of the remnant pancreas after distal pancreatectomy. In gastric cancer surgery, drain tubes are not always placed at the site of pancreatic injury as it is not always easy to know where the pancreas is injured by heat or trauma.
The aim of this study was to assess the validity of extrapolating the ISGPS definition to include situations surrounding elective gastrectomy with suprapancreatic lymph node dissection but without pancreatic resection.
Methods
Patients
A total of 506 patients underwent elective surgery for gastric cancer at Yodogawa Christian Hospital between January 2012 and December 2020. The following 54 patients were excluded from the study: 5 patients who underwent pancreatoduodenectomy due to duodenal invasion, concomitant pancreatic or bile duct cancer, 12 patients who underwent gastrectomy for remnant stomach cancer, 3 patients who underwent palliative partial gastrectomy, 1 who underwent subtotal esophagectomy due to esophageal invasion, 5 patients who underwent total gastrectomy with distal pancreatectomy and splenectomy, 1 patient who underwent distal gastrectomy with partial pancreatectomy, and 27 patients who underwent gastrectomy without suprapancreatic lymph node dissection (D0 or D1 according to the 2018 Japanese Gastric Cancer Treatment Guidelines) [1]. From the remaining 452 patients who underwent gastrectomy with suprapancreatic lymph node dissection (D1+, D2, or D2+ dissection) without pancreatic resection, we also excluded 9 patients whose drain-fluids amylase levels (dAmy) on postoperative day 1 (dAmy1) or day 3 (dAmy3) data were not available. Finally, the remaining 443 patients were included in the analysis. The clinicopathological data of these patients were retrospectively obtained by reviewing their medical records and operative reports.
The drain tube was routinely placed in the suprapancreatic area from the right side of the body. In cases of total gastrectomy, another drain tube was usually placed in the left subphrenic area from the left side of the body. When plural drain tubes were placed, the highest amylase concentration was selected for the analyses.
Postoperative pancreas-related complications (PPRC) in this study were defined as postoperative complications of ≥ grade II according to the CD classification system [8] in patients with increased dAmy1 or dAmy3 to ≥ 3 times the upper limit of normal serum amylase levels (≥ 125 IU/L × 3) whose drain fluid became purulent or clinical imaging showed intra-abdominal abscess, peripancreatic fluid, or intra-abdominal bleeding, without any sign of other conditions that could cause systemic inflammatory reactions such as anastomotic leakage, pneumonia, or urinary tract infection. We compared the laboratory data of patients with and without PPRC to investigate the appropriate day to assess dAmy after gastrectomy with suprapancreatic lymph node dissection (D1+, D2, or D2+ dissection) without pancreatic resection.
The protocol was approved by the Institutional Ethical Committee on Human Research (No. 2021-048) and was in accordance with the tenets of the Helsinki Declaration of 1964 and later versions. Informed consent was obtained as comprehensive consent regarding the use of personal information from all patients for inclusion in the study.
Statistics
Receiver operating characteristic (ROC) curve analysis was used to determine the optimal cutoff values that were identified by the Youden index (Youden’s J statistic), or J = max{sensitivity + specificity − 1} [9]. The area under the curve (AUC) was calculated using ROC. Differences in the proportion or frequency between the two groups were compared using Fisher’s exact test or the Chi-squared test. Statistical significance was set at p < 0.05. Variables with p values < 0.10 in the univariate analysis were included in the multivariate logistic regression analysis to identify the predictive factors of PPRC. All statistical analyses were performed using JMP software 12.2.0 (SAS Institute Inc., Cary, NC, USA).
Results
Details of the clinicopathological features of the 443 patients included in the analysis are shown in Table 1.
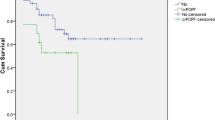
Among these 443 patients, 24 (5.4%) developed PPRC according to our definition. A total of 320 patients (72.2%) showed high dAmy1, and 130 (29.3%) showed high dAmy3 (of ≥ 375 IU/L) (Fig. 1). Among the 24 patients with PPRC, 15 had dAmy3 ≥ 375 IU/L, while all 24 patients had dAmy1 ≥ 375 IU/L, and no patients with dAmy1 < 375 IU/L developed PPRC. Among the 15 patients with both high dAmy1 and dAmy3 (≥ 375 IU/L), 7 patients developed grade II PPRC according to the CD classification, and 8 developed grade III. Among the 9 patients with both high dAmy1 (≥ 375 IU/L) and low dAmy3 (< 375 IU/L), 4 patients developed a PPRC of grade II, and 5 patients developed grade III.
The numbers in the upper and lower lines indicate the distribution of all the patients, and patients with postoperative pancreas-related complications, respectively, according to the surgical drain amylase levels on postoperative days 1 and 3. dAmy1 amylase level in the drain fluid on postoperative day 1, dAmy3 amylase level in the drain fluid on postoperative day 3
Figure 2 demonstrates the relationship between dAmy1 and dAmy3 in all 24 patients who developed PPRC. DAmy1 was 6637 ± 8941 IU/L, dAmy3 was 772 ± 697 IU/L, while dAmy3 was significantly lower than dAmy1 (p < 0.001). Among these 24 patients, dAmy3 was higher than dAmy1 in only two patients.
ROC curves of dAmy1 and dAmy3 were drawn to compare the predictive value for PPRC and to calculate the appropriate cutoff values for each parameter (Fig. 3). The AUC of dAmy1 and dAmy3 was 0.896 and 0.791, respectively. Thus, the AUC of dAmy1 was greater than that of dAmy3. The optimal cutoff values of dAmy1 and dAmy3 to predict PPRC identified with Youden indices were 1545 IU/L and 254 IU/L, respectively. Importantly, 254 IU/L as a cutoff value of dAmy3 is inappropriate because it is lower than 375 IU/L, which is three times the upper limit of normal serum amylase levels at our institution. Thus, we calculated a cutoff value that would be 375 IU/L or larger with max{sensitivity + specificity − 1} within range and established 761 IU/L as a more appropriate cutoff value of dAmy3 (Fig. 3b).
Receiver operating characteristic curves of the amylase concentration of the drainage fluid on postoperative day 1 (a) and day 3 (b) for predicting postoperative pancreas-related complications. Optimal cutoff values and area under the curve are a 1545 IU/L and 0.896, b 761 IU/L and 0.791, respectively
The AUCs and cutoff values of serum C-reactive protein levels (sCRP) on postoperative days 1 and 3 (sCRP1 and sCRP3, respectively) were calculated using ROC curves in the same manner. The AUCs and cutoff values of sCRP1 were 0.682 and 7.89 mg/dL and those of sCRP3 were 0.838 and 15.15 mg/dL, respectively.
With these cutoff values, the relationships between these four variables and PPRC were investigated (Table 2). In univariate analysis, all four variables, including dAmy1 (p < 0.001), dAmy3 (p < 0.001), sCRP1 (p = 0.001), and sCRP3 (p < 0.001), correlated with PPRC. In multivariate analysis, including all four variables, dAmy1 (odds ratio 22.377) and sCRP3 (odds ratio 7.098) were strongly correlated with PPRC. DAmy3 was also a significant predictor of PPRC (odds ratio 2.805); however, the correlation was weaker than that of dAmy1.
Discussion
According to the ISGPS definition, the diagnosis of pancreatic fistula requires the amylase levels in drain fluid on or after postoperative day 3 to be > 3 times the upper limit of normal serum amylase level for each specific institution. When this condition leads to clinically relevant, it is called a pancreatic fistula [6]. However, some authors [10,11,12,13] reported that dAmy generally peaked on postoperative day 1 and gradually declined thereafter. This phenomenon has been reported to occur even in cases with pancreatic fistula of grade III or IV according to the CD classification [13]. In our cohort, dAmy3 was lower than dAmy1 in all patients who developed PPRC except for two patients. Among the 24 patients who developed PPRC, dAmy1 was ≥ 375 IU/L in all patients; however, dAmy3 was < 375 IU/L in nine patients (Fig. 1). This means that these nine patients (37.5%) would have been missed if the ISGPS definition of the pancreatic fistula was used. In addition, among these 9 patients, 4 developed a grade II PPRC according to CD classification, and 5 developed grade III; thus, low dAmy3 did not imply low severity of PPRC. On the contrary, there were no cases of PPRC in which dAmy1 was < 375 IU/L. Although the positive predictive value when dAmy1 was used (7.5%) was lower than that calculated using dAmy3 (11.5%), dAmy1 seemed more suitable than dAmy3 to use as an indicator of pancreatic fistula to detect all cases of PPRC where dAmy3 dropped below < 375 IU/L.
There may be two possible reasons for dAmy3 dropping lower than dAmy1. First, pancreatic fluid leaked from the injured portion on the surface of the pancreas is in remission. In this condition, pancreatic fluid leakage would not cause clinical problems but would rather result in what is called a “biochemical leak”. The other possible reason for low dAmy3 is insufficient drainage of peripancreatic enzyme-rich fluid in the peritoneal cavity. Inappropriate location of surgically placed drain tubes, fibrin formation around the drain tubes, or adhesion of the surrounding tissue or organs making drain tubes apart from injured sites of the pancreas may lead to insufficient drainage, resulting in low amylase concentrations as well. Adhesion or fibrin formation in the peritoneal cavity is usually mild on the day of surgery and postoperative day 1, so dAmy1 levels can reflect the concentration of amylase in the fluid collected from a wide area, including the surgical site, even when the drain tubes are slightly distal to the injured sites of the pancreas. Thus, dAmy1 is considered to be more suitable for detecting PPRC in cases of gastric cancer surgery, in which the location of the pancreatic injury is not always recognizable.
When dAmy1 and dAmy3 were compared as predictive factors of PPRC, drawing ROC curves, the AUCs of dAmy1 and dAmy3 were 0.896 and 0.791, respectively. Thus, the AUC of dAmy1 was greater than that of dAmy3, indicating that dAmy1 was a better predictor. In addition, both dAmy1 and dAmy3 were significant predictive factors for PPRC in univariate and multivariate analyses; however, the p value of dAmy3 was much lower than that of dAmy1 (< 0.001 vs. 0.049) in multivariate analysis, indicating that dAmy1 is a stronger predictive factor than dAmy3. Thus, dAmy1 is a more reliable predictive biomarker for pancreatic fistula than dAmy3.
The weakness of using dAmy1 instead of dAmy3 is that more patients were screened as candidates for PPRC. DAmy1 was ≥ 375 IU/L in 320 patients (72.2%), while dAmy3 was ≥ 375 IU/L in 130 patients (29.3%) (Fig. 1). Among the 320 patients with dAmy1 ≥ 375 IU/L, 24 patients (7.5%) developed PPRC. Among the 130 patients with dAmy3 ≥ 375 IU/L, 15 patients (11.5%) developed PPRC. Thus, the positive predictive value of dAmy1 was lower than that of dAmy3; however, it is more important to avoid overlooking patients who may go on to develop PPRC.
This study had several limitations. First, this was a single-institution retrospective study; hence, the sample size was small, and there were only 24 patients who developed PPRC of CD ≥ II, making the statistical power weak. However, the strength of this study is that the patients were limited to those who underwent gastrectomy with suprapancreatic lymph node dissection (D1+, D2, or D2+ dissection) without pancreatic resection; thus, we could exclude the influence of pancreatic resection. In addition, we also excluded patients whose dAmy1 or dAmy3 were not available, which meant that there were no data defects. Second, we did not consider the volume of drainage fluid. If postoperative lymphorrhea caused dilution of the amylase in the drainage fluid, this could have affected the results. However, Fukami et al. [14] reported that dAmy was more reliable than the total amount of amylase in the drain fluid as a predictor of postoperative pancreatic fistula after pancreatic surgery.
In conclusion, dAmy1 is more suitable than dAmy3 for use as an indicator of pancreatic fistula after gastrectomy with suprapancreatic lymph node dissection (D1+, D2, or D2+ dissection) without pancreatic resection.
References
Japanese Gastric Cancer Association (2021) Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer 24:1–21
Kurokawa Y, Doki Y, Mizusawa J et al (2018) Bursectomy versus omentectomy alone for resectable gastric cancer (JCOG1001): a phase 3, open-label, randomized controlled trial. Lancet Gastroenterol Hepatol 3(7):460–468
Sano T, Sasako M, Mizusawa J et al. Stomach Cancer Study Group of the Japan Clinical Oncology Group (2017) Randomized controlled trial to evaluate splenectomy in total gastrectomy for proximal gastric carcinoma. Ann Surg 265(2):277–283
Hiki N, Honda M, Etoh T et al (2018) Higher incidence of pancreatic fistula in laparoscopic gastrectomy. Real-world evidence from a nationwide prospective cohort study. Gastric Cancer 21(1):162–170
Uyama I, Suda K, Nakauchi M et al (2019) Clinical advantages of robotic gastrectomy for clinical stage I/II gastric cancer: a multi-institutional prospective single-arm study. Gastric Cancer 22(2):377–385
Bassi C, Marchegiani G, Dervenis C et al. International Study Group on Pancreatic Surgery (ISGPS) (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161(3):584–591
Bassi C, Dervenis C, Butturini G et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Akobeng AK (2007) Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr 96(5):644–647
Iwata N, Kodera Y, Eguchi T et al (2010) Amylase concentration of the drainage fluid as a risk factor for intra-abdominal abscess following gastrectomy for gastric cancer. World J Surg 34(7):1534–1539
Kobayashi D, Iwata N, Tanaka C et al (2015) Factors related to occurrence and aggravation of pancreatic fistula after radical gastrectomy for gastric cancer. J Surg Oncol 112(4):381–386
Taniguchi Y, Kurokawa Y, Mikami J et al (2017) Amylase concentration in drainage fluid as a predictive factor for severe postoperative pancreatic fistula in patients with gastric cancer. Surg Today 47(11):1378–1383
Kanda M, Fujiwara M, Tanaka C et al (2016) Predictive value of drain amylase content for peripancreatic inflammatory fluid collections after laparoscopic (assisted) distal gastrectomy. Surg Endosc 30(10):4353–4362
Fukami Y, Saito T, Osawa T et al (2021) Which is the best predictor of clinically relevant pancreatic fistula after pancreatectomy: drain fluid concentration or total amount of amylase? Ann Gastroenterol Surg 5(6):844–852
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by TW, SM and MS. The first draft of the manuscript was written by TW and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Wakahara, T., Miura, S., Yasuhara, Y. et al. Is the ISGPS definition of pancreatic fistula applicable after gastrectomy?. Int J Clin Oncol 27, 1273–1278 (2022). https://doi.org/10.1007/s10147-022-02177-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-022-02177-x