Abstract
Background
S-1 monotherapy is one of the standard adjuvant treatments for patients with stage II and III gastric cancers. Early recurrence after S-1 adjuvant therapy has a poor prognosis. This study aimed to clarify the treatment outcomes of systemic chemotherapy and explore encouraging regimens.
Methods
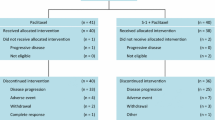
This was a multicenter retrospective study. Among gastric cancer patients who underwent curative gastrectomy followed by adjuvant S-1 monotherapy, patients who experienced a recurrence while receiving adjuvant therapy or within 6 months after completion and started systemic chemotherapy at four institutions between 2005 and 2015 were eligible.
Results
A total of 112 patients were included. The main treatment regimens were weekly paclitaxel (n = 38, 34%), irinotecan plus cisplatin (n = 31, 28%), capecitabine plus cisplatin (n = 7, 6%), and irinotecan monotherapy (n = 6, 5%). For all patients, median progression-free survival and overall survival were 3.7 and 11.4 months, respectively. Among 77 patients with measurable lesions, the overall response and disease control rates were 24.7% and 62.3%, respectively. Multivariate analyses for overall survival showed that Eastern Cooperative Oncology Group performance status 2 [hazard ratio (HR) 3.71; 95% confidence interval (CI) 1.78–7.73] and undifferentiated histological type (HR 2.04; 95% CI 1.35–3.44) were independent prognostic factors, and treatment regimens were not prognostic. Exploratory comparisons did not show statistically significant differences between treatment regimens.
Conclusions
This study of the largest number of patients with early recurrence after S-1 adjuvant monotherapy demonstrated that the prognosis for patients treated by all regimens was similar and poor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the fifth most common malignancy and the third leading cause of cancer death in the world, and it is more common in Eastern Asia than in western countries [1]. Although the mainstay of treatment is surgery, a substantial proportion of patients experiences recurrence even after curative resection. A phase III trial (ACTS-GC; The Adjuvant Chemotherapy Trial of S-1 for Gastric Cancer) that compared surgery followed by 1 year of S-1 adjuvant monotherapy with surgery alone demonstrated the effectiveness of S-1 for Japanese patients with curatively resected gastric cancer [2]. Although there are several options, such as capecitabine plus oxaliplatin, S-1 monotherapy is one of the standard adjuvant treatments for gastric cancer in Japan. However, in the ACTS-GC trial, approximately 30% of patients treated with S-1 adjuvant therapy had a relapse [3].
Previous studies indicated that recurrence after S-1 adjuvant therapy is associated with a poor prognosis. Hasegawa et al. reported that median overall survival (OS) for patients with a recurrence after S-1 adjuvant therapy (n = 30) was 9.4 months [4]. Aoyama et al. reported a poor outcome for this population (n = 34) as well, with median OS of 7.3 months [5]. In particular, patients who had an early recurrence after S-1 adjuvant therapy had a poor prognosis. Shitara et al. analyzed 52 patients who had a recurrence after S-1 adjuvant therapy and thereafter received S-1 plus cisplatin. Patients with recurrence-free interval < 6 months (n = 25) had poor treatment outcomes [6]. In addition, another retrospective study by Shitara et al. demonstrated that non-S-1-containing regimens were associated with better progression-free survival (PFS) compared with S-1-containing regimens in gastric cancer patients who had a recurrence after adjuvant S-1 monotherapy (median PFS, 4.3 vs. 2.3 months; p = 0.02) [7]. These findings suggested that non-S-1-containing regimens including taxanes or irinotecan are more appropriate for patients with early recurrence after S-1 adjuvant therapy than S-1-containing standard regimens. Recently, a phase II trial of capecitabine plus cisplatin for this population (n = 40) reported promising survival outcomes, with median PFS and OS of 4.4 and 13.7 months, respectively [8]. These previous studies have been based on small sample sizes, and most clinical trials of first-line or second-line chemotherapy excluded patients with early recurrent disease after S-1 adjuvant therapy.
Hence, the clinical outcomes and the optimal regimens for this population have not been fully elucidated. To address this issue, this study aimed to evaluate the treatment outcomes of systemic chemotherapy and explore encouraging regimens in a larger cohort of gastric cancer patients with early recurrence after S-1 adjuvant therapy.
Patients and methods
Patients
We retrospectively reviewed patients with gastric cancer who underwent curative gastrectomy followed by adjuvant S-1 monotherapy at four institutions. Among these patients, we identified patients who had a recurrence during adjuvant therapy or within 6 months after completion (early recurrence) and began systemic chemotherapy between January 2005 and December 2015. The eligibility criteria were a pathologically confirmed stage II or III gastric adenocarcinoma at curative surgery and Eastern Cooperative Oncology Group performance status (ECOG-PS) of 0–2, and adequate organ functions. The exclusion criteria were ascites extending throughout the entire abdominal cavity (massive ascites), discontinuation of adjuvant therapy within 4 weeks, and history of neoadjuvant chemotherapy. The study was approved by the institutional review boards of each participating center.
Evaluation and statistical analyses
Patient demographic data at the time of recurrence were obtained from institutional medical records. Survival was calculated using the Kaplan–Meier method and compared by the log-rank test. PFS was defined as the time between the initiation of chemotherapy and progression or death from any cause. OS was defined as the time between the initiation of chemotherapy and death from any cause. Tumor response was assessed by each investigator using Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1 [9] for patients with measurable lesions. Fisher’s exact test or the chi-squared test was used for comparison between groups. The following factors were included in the univariate analysis: age, gender, ECOG-PS, human epidermal growth factor receptor 2 (HER2) status, histological type, number of metastases, presence of peritoneal metastases, baseline alkaline phosphatase (ALP), baseline lactate dehydrogenase (LDH), neutrophil–lymphocyte ratio (NLR), timing of the recurrence, and chemotherapy regimen. In multivariate analyses, a forward stepwise selection procedure was used. To compare the efficacy of different treatment regimens, the patients were divided into three exploratory cohorts according to their regimens. The regimens were taxane-based regimens including paclitaxel or docetaxel, irinotecan plus cisplatin (IP), and regimens including fluoropyrimidines plus platinum agents (FP regimens). Because there is a clear difference in standard treatment between HER2-positive and -negative gastric cancers, we excluded patients with HER2-positive cancer in the exploratory analyses. Patients treated with regimens that included neither taxanes nor platinum agents were excluded from these analyses as well. The log-rank test and the Cox proportional hazards model were used to evaluate differences in survival. The adjusted hazard ratio (HR) was calculated by performing multivariate analyses among patients who were included in the exploratory comparison. A p value < 0.05 was considered to indicate statistical significance. All tests were two sided.
Results
Patients
A total of 112 patients were enrolled in the study. The baseline patient characteristics are listed in Table 1. The median age was 62 years (range 29–83), and 84 patients (75%) were male. Ten patients (9%) had an ECOG-PS of 2. The HER2 status was unknown for 49 patients (44%). The most common metastatic site was the peritoneum (n = 51, 46%), followed by lymph nodes (n = 40, 36%) and liver (n = 32, 29%). Sixty-eight patients (61%) had a recurrence during adjuvant therapy. The median duration of adjuvant S-1 monotherapy was 6.9 months (range, 1.0–16.2). The treatment regimens were weekly paclitaxel (PTX) (n = 38, 34%), IP (n = 31, 28%), capecitabine plus cisplatin (XP) (n = 7, 6%), irinotecan monotherapy (n = 6, 5%), S-1 plus cisplatin (SP) (n = 5, 4%), trastuzumab plus XP (n = 5, 4%), trastuzumab plus PTX (n = 5, 4%), nab-PTX (n = 4, 4%), S-1 plus PTX (n = 3, 3%), and others (n = 8, 7%). Most of the patients (n = 103, 92%) received non-S-1-containing regimens.
Treatment results and efficacy
With a median follow-up period of 14.2 months, median PFS and OS were 4.2 months [95% confidence interval (CI) 3.32–5.29] and 11.4 months (95% CI 9.00–14.6), respectively (Fig. 1). The 1-year OS rate was 48.3% (95% CI 38.6–57.4). Among the 77 patients with measurable lesions, the overall response and disease control rates were 24.7% (95% CI 15.6–35.8) and 62.3% (95% CI 50.6–73.1), respectively. Of 104 patients who discontinued chemotherapy, 69 (66%) received subsequent therapies. At the time of data cutoff, 84 (75%), 71 (63%), 60 (54%), 14 (13%), 4 (4%), and 4 (4%) patients were being treated with taxane agents, platinum agents, irinotecan, trastuzumab, ramucirumab, and immune checkpoint inhibitors, respectively.
Prognostic analyses
Univariate and multivariate Cox regression analyses for OS are shown in Table 2. Univariate analysis identified age, gender, ECOG-PS, histological type, and elevated LDH level as prognostic indicators. In multivariate analysis, ECOG-PS 2 (HR 3.71; 95% CI 1.78–7.73) and histological type (HR 2.04; 95% CI 1.35–3.44) were independent prognostic indicators. Treatment regimens were not prognostic.
Exploratory comparison among treatment regimens
Three cohorts consisted of patients receiving taxane-based regimens (n = 45), IP (n = 30), and FP regimens (n = 13). Taxane-based regimens included weekly PTX, nab-PTX, S-1 plus PTX, docetaxel monotherapy, and S-1 plus docetaxel. The FP regimens were capecitabine plus cisplatin, S-1 plus cisplatin, and capecitabine plus cisplatin. The baseline patient characteristics were well balanced among the three cohorts (Table 3). Median PFS was 3.7 months (95% CI 3.19–5.49) for taxane-based regimens, 3.0 months (95% CI 1.84–6.34) for IP, and 4.0 months (95% CI 1.77–not applicable) for FP regimens (log-rank p = 0.84) (Fig. 2a). Median OS was 7. 6 months (95% CI 6.60–11.27) for taxane-based regimens, 11.8 months (95% CI 7.36–15.2) for IP, and 13.3 months (95% CI 4.07–18.00) for FP regimens (log-rank p = 0.64) (Fig. 2b). According to a multivariate Cox model compared with taxane-based regimens, there were no statistically significant differences in PFS or OS among the three cohorts (HR of IP 0.79; 95% CI 0.49–1.31; adjusted HR of IP 0.78; 95% CI 0.42–1.42; HR of FP 0.79; 95% CI 0.49–1.31; adjusted HR of FP 0.76; 95% CI 0.35–1.65). Fifty-eight patients had measurable lesions. The overall response rate was 11.1% for taxane-based regimens, 33.3% for IP, and 25.0% for FP regimens (p = 0.17). The disease control rate was 44.4% for taxane-based regimens, 66.7% for IP, and 62.5% for FP regimens (p = 0.30). The rate of grade 3 or higher adverse events was 15.6% for taxane-based regimens, 50.0% for IP, and 38.5% for FP regimens. In particular, grade 3 or higher non-hematologic adverse events were more frequently observed for IP, with frequencies of 2.2% for taxane-based regimens, 23.2% for IP, and 7.7% for FP regimens.
Discussion
This study analyzed 112 patients who had an early recurrence during or after S-1 adjuvant monotherapy and received systemic chemotherapy. To our best of our knowledge, this is the largest study to focus on early recurrence after S-1 adjuvant monotherapy.
The survival outcomes in our study were better than those in previous reports. In our study, most of the patients received non-S-1-containing regimens (n = 103, 92%). In addition, a modest number of patients received relatively new anticancer drugs, such as trastuzumab (14 patients, 13%), ramucirumab (4 patients, 4%), and immune checkpoint inhibitors (4 patients, 4%). We excluded patients with massive ascites and inadequate organ function. These factors may have contributed to better outcomes in our cohort. On the other hand, the survival outcomes in our study were worse and the overall response rates were distinctly lower than those in recent Japanese phase III trials using S-1 plus platinum agents as first-line chemotherapy [10, 11].
We conducted prognostic analyses showing that ECOG-PS and histological type were independent prognostic indicators. ECOG-PS is a well-validated and universal factor predicting survival in metastatic gastric cancer [12]. Undifferentiated histological type was also an independent prognostic factor in the study by Aoyama et al. [5], supporting our findings. In addition, we compared the efficacy of representative treatment regimens to explore optimal therapies for this population, but no differences were observed among treatment regimens. All regimens selected so far have unfavorable outcomes, and new therapies should be established to improve treatment outcomes.
Several anticancer drugs have been approved recently in Japan. Ramucirumab was shown to prolong survival in patients with gastric cancer in the RAINBOW and REGARD trials [13, 14]. According to the results of the RAINBOW trial, which enrolled patients who received FP regimens as first-line chemotherapy, paclitaxel in combination with ramucirumab is the most recommended regimen as second-line chemotherapy for metastatic gastric cancer. In addition, nab-paclitaxel in combination with ramucirumab showed promising results for patients refractory to a fluoropyrimidine-containing chemotherapy regimen [15]. Based on these trials, paclitaxel or nab-paclitaxel in combination with ramucirumab seems to be a good candidate for this population. Capecitabine was approved in Japan in 2011, and capecitabine plus cisplatin or oxaliplatin has been used as one of the standard therapies as first-line chemotherapy. Although the effectiveness of capecitabine after failure of S-1 therapy is unclear, capecitabine plus cisplatin showed promising outcomes in a Japanese phase II trial [8]. Furthermore, immune checkpoint inhibitors were recently shown to have antitumor activity as later lines of therapy [16,17,18]. Although the effectiveness of immunotherapy is unclear as front-line chemotherapy for patients with early recurrence, clinical trials examining combination strategies in early lines of therapy are ongoing. Regimens using these newly approved agents would also be new promising candidates.
Our study has a few limitations. The major limitation is that the treatment regimens differed considerably due to its retrospective nature. This is because the optimal regimen for gastric patients with early recurrence remains unclear, proposing that there is an urgent need for focusing on this population. Second, we did not have a large enough number of patients who received the candidate treatments mentioned above, because most patients initiated chemotherapy before the approval of these agents. Further analyses evaluating these regimens are warranted in the future. Finally, HER2 status, which influences the clinical prognosis, was not examined in approximately half of the patients since HER2 testing was reimbursed in Japan in 2011. Despite these limitations, our study included the largest number of patients with early recurrences of any study known to us, and our results could serve as reference data for the development of further treatments.
In summary, the prognosis of early recurrence of gastric cancer after S-1 adjuvant therapy was poor, in consistency with previous reports. Prognostic analyses revealed that ECOG-PS and histological type were independent factors. The prognosis for patients treated by any regimen selected for early recurrent gastric cancer was similar and poor. Further research is warranted to establish new treatment regimens and improve outcomes.
References
Ferlay J, Soerjomataram I, Dikshit R et al (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359–386
Sakuramoto S, Sasako M, Yamaguchi T et al (2007) Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med 357:1810–1820
Sasako M, Sakuramoto S, Katai H et al (2011) Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol 29:4387–4393
Hasegawa H, Fujitani K, Kurokawa Y et al (2010) Effect of S-1 adjuvant chemotherapy on survival following recurrence and efficacy of first-line treatment in recurrent gastric cancer. Chemotherapy 56:436–443
Aoyama T, Yoshikawa T, Watanabe T et al (2011) Survival and prognosticators of gastric cancer that recurs after adjuvant chemotherapy with S-1. Gastric Cancer 14:150–154
Shitara K, Muro K, Ura T et al (2008) Chemotherapy for gastric cancer that recurs after adjuvant chemotherapy with S-1. Jpn J Clin Oncol 38:786–789
Shitara K, Morita S, Fujitani K et al (2012) Combination chemotherapy with S-1 plus cisplatin for gastric cancer that recurs after adjuvant chemotherapy with S-1: multi-institutional retrospective analysis. Gastric Cancer 15:245–251
Nishikawa K, Tsuburaya A, Yoshikawa T et al (2018) A phase II trial of capecitabine plus cisplatin (XP) for patients with advanced gastric cancer with early relapse after S-1 adjuvant therapy: XParTS-I trial. Gastric Cancer 21:811–818
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Koizumi W, Narahara H, Hara T et al (2008) S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol 9:215–221
Yamada Y, Higuchi K, Nishikawa K et al (2015) Phase III study comparing oxaliplatin plus S-1 with cisplatin plus S-1 in chemotherapy-naive patients with advanced gastric cancer. Ann Oncol 26:141–148
Chau I, Norman AR, Cunningham D et al (2004) Multivariate prognostic factor analysis in locally advanced and metastatic esophago-gastric cancer—pooled analysis from three multicenter, randomized, controlled trials using individual patient data. J Clin Oncol 22:2395–2403
Fuchs CS, Tomasek J, Yong CJ et al (2014) Ramucirumab monotherapy for previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (REGARD): an international, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet 383:31–39
Wilke H, Muro K, Van Cutsem E et al (2014) Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): a double-blind, randomised phase 3 trial. Lancet Oncol 15:1224–1235
Bando H, Shimodaira H, Fujitani K et al (2018) A phase II study of nab-paclitaxel in combination with ramucirumab in patients with previously treated advanced gastric cancer. Eur J Cancer 91:86–91
Kang YK, Boku N, Satoh T et al (2017) Nivolumab in patients with advanced gastric or gastro-oesophageal junction cancer refractory to, or intolerant of, at least two previous chemotherapy regimens (ONO-4538-12, ATTRACTION-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 390:2461–2471
Muro K, Chung HC, Shankaran V et al (2016) Pembrolizumab for patients with PD-L1-positive advanced gastric cancer (KEYNOTE-012): a multicentre, open-label, phase 1b trial. Lancet Oncol 17:717–726
Fuchs CS, Doi T, Jang RW et al (2018) Safety and efficacy of pembrolizumab monotherapy in patients with previously treated advanced gastric and gastroesophageal junction cancer: phase 2 clinical KEYNOTE-059 trial. JAMA Oncol 4:e180013
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for the English language review.
Funding
This study was conducted with no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Seiichiro Mitani has received honoraria from Eli Lilly. Shigenori Kadowaki has received honoraria from Eli Lilly, Bayer, Bristol-Myers, Chugai, Ono, and Yakult, and research funding from Eli Lilly, Boehringer Ingelheim, Bristol-Myers, Ono, and Taiho. Hiroki Hara has received honoraria from Chugai, Taiho, Merck Serono, Yakult, Eli Lilly, Ono, Takeda, Bristol-Myers, and research funding from AstraZeneca, Chugai, Merck Serono, MSD, Ono, Taiho, Takeda, Boehringer Ingelheim, Dainippon Sumitomo, Daiichi Sankyo, Eli Lilly, Pfizer, LSK BioPharma, Eisai, and Incyte. Kazuhiro Nishikawa has received honoraria from Chugai, Taiho, Yakult, Eli Lilly, Tsumura, and EA Pharma, and research funding from Yakult and Taiho. Kei Muro has received honoraria from Eli Lilly, Chugai, Merck Serono, Ono, Taiho, Takeda, and Yakult, and research funding from Daiichi Sankyo, Gilead Sciences, Kyowa Hakko Kirin, MSD, Ono, and Shionogi. None of the remaining authors have potential conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Mitani, S., Kadowaki, S., Hasegawa, H. et al. Systemic chemotherapy for gastric cancer with early recurrence after adjuvant S-1 monotherapy: a multicenter retrospective study. Int J Clin Oncol 24, 1197–1203 (2019). https://doi.org/10.1007/s10147-019-01477-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-019-01477-z