Abstract
Background
In Japan, positron emission tomography using 18F-fluorodeoxyglucose (FDG-PET) has been covered by the national health insurance for esophageal cancer since 2006. FDG-PET is commonly performed in advanced esophageal cancer. The aim of this study was to determine the effect of FDG-PET on survival in patients with locally advanced inoperable esophageal cancer.
Methods
We retrospectively reviewed all patients with cT4 and without M1 esophageal cancer on CT in our institution between 2000 and 2014, and data for 78 patients who meet the eligibility criteria described below were used for analysis in this study. The eligibility criteria included (1) cT4 esophageal cancer without distant metastases or M1 lymph node metastasis (UICC 2002), (2) histologically proven squamous cell carcinoma, (3) 20–79 years of age, (4) having undergone at least 1 cycle of concomitant chemotherapy, (5) having been irradiated with 50 Gy or more, and (6) no other active malignant tumor during treatment.
Results
Two patients were excluded because abdominal lymph node metastases or neck lymph node metastases were detected by FDG-PET. In 78 eligible patients, FDG-PET was not performed before treatment in 41 of the 78 patients and was performed in the other patients. The median observation period was 68 months. The 3-year and 5-year overall survival rates in 78 patients were 36.9% and 30.8%, respectively. There was no significant difference in overall survival or progression-free survival between patients in whom FDG-PET was performed and those in whom FDG-PET was not performed (12.0 months vs. 11.0 months, p = 0.920 and 6.0 months vs. 6.0 months, p = 0.844, respectively).
Conclusions
Compared with only CT, additional information from FDG-PET is not associated with improving survival in patients with locally advanced esophageal cancer. Our results suggest that FDG-PET might not have much meaning for survival in locally advanced esophageal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal cancer is the eighth most common form of cancer and the sixth most common cause of cancer-related death [1]. In Japan, positron emission tomography using 18F-fluorodeoxyglucose (FDG-PET) has been covered by the national health insurance for esophageal cancer since 2006. Advances have been made in the staging and selection of treatment method for esophageal cancer. Distant metastasis, including M1 lymph nodes, is the most important factor that restricts therapeutic strategies and prognosis. Barber et al. reported that FDG-PET/CT changed the stage group in 56 (40%) of 139 patients and changed management in 47 (34%) of 139 patients with esophageal cancer and that post-FDG-PET/CT stage group and treatment intent were both strongly associated with survival (p < 0.001) [2]. Their results suggest that the use of FDG-PET would enable identification and exclusion of patients with distant metastases and could prolong the survival of patients with locally advanced esophageal cancer. The aim of this study was, therefore, to determine the effect of FDG-PET on survival in patients with locally advanced inoperable esophageal cancer.
Patients and methods
We retrospectively reviewed data for all 84 patients treated by radiotherapy, who were aged less than 80 years and had no other active malignant tumor during treatment, with esophageal squamous cell carcinoma staged cT4N0M0 or cT4N1M0 on CT between 2000 and 2014 in our institution. In 40 of 84 patients, FDG-PET was performed median 12 (range 3–20) days before initiation of treatment. Two patients were excluded because abdominal lymph node metastases or neck lymph node metastases were detected by FDG-PET. One of the remaining 38 patients was excluded because he was treated with radiotherapy alone due to renal failure. Thirty-seven patients were enrolled in this study as group I. In 44 of 84 patients, FDG-PET was not performed. Three of 44 patients were excluded because they were treated by radiotherapy alone due to renal failure, dementia and poor performance status. Forty-one patients were enrolled in this study as group II (Fig. 1). Data for total 78 patients who underwent at least 1 cycle of concomitant chemotherapy and radiotherapy with 50 Gy or more were used for analysis in this study. We compared the results of chemoradiotherapy among those 2 groups.
FDG-PET/CT methods
After at least a 4-h fast, FDG at a dose of 3.7 MBq /kg was injected. After 60 min, a whole body scan was performed using a PET/CT scanner (Biograph Duo LSO or Biograh 40 Truepoint; Siemens Medical Solution, Erlangen Germany) in our institution.
Treatment
Radiotherapy
A linear accelerator (4 MV or 10 MV) was used as the X-ray source. The target volume was localized for radiotherapy in all patients by CT planning. The daily fractional dose of radiotherapy was 1.8–2.0 Gy, administered 5 days a week, and the total dose was 50.0–70.0 Gy. The gross tumor volume (GTV) was defined as the primary tumor and any involved nodes on CT (> 0.5 cm on the short axis). The clinical target volume for the primary lesion (CTV-p) was defined as a GTV with a 3.0-cm margin in the cranio-caudal direction and with a 0.5-cm margin in the horizontal direction. The initial clinical target volumes (CTV initial) included CTV-p plus the bilateral supraclavicular, mediastinal and abdominal regions (so-called long T), except for cases of cervical esophageal cancer. For cervical esophageal cancer without a skip lesion, CTV initial included CTV-p plus the bilateral supraclavicular and upper mediastinal regions (so-called short T). Planning target volume (PTV) was defined as CTV with a 0.5–1.5-cm margin. After 39.6–40 Gy, radiotherapy was performed for only the primary tumor with a 3-cm cranio-caudal margin and for metastatic lymph nodes with a 1-cm circular margin avoiding the spinal cord.
Concurrent chemotherapy
All patients underwent one of the following three platinum-based chemotherapy regimens concurrent with radiotherapy as described below.
-
a)
Cisplatin (CDDP) (60 mg/m2/day) + 5-fluorouracil (5-FU) (1000 mg/m2/24 h for 5 days) + docetaxel (DOC) (50 mg/m2/day).
-
b)
CDDP (70 mg/m2/day) + 5-FU (700 mg/m2/24 h for 4 days).
-
c)
Nedaplatin (CDGP) (70 mg/m2/day) + 5-FU (500 mg/m2/24 h for 5 days).
If possible, two cycles of those regimens were performed during radiotherapy.
Follow-up
Follow-up evaluations for all patients were performed every 2–3 months for the first 2 years and every 6 months thereafter by endoscopy and/or CT.
Endpoints
Endpoints of the present study were overall survival (OS) rate, progression-free survival (PFS) rate and patterns of failure.
Statistics
The characteristics of patients in group I and group II were compared using Pearson’s Chi-square test and the Mann–Whitney test.
Survival estimates were calculated from the first day of radiotherapy using the Kaplan–Meier method, and differences were evaluated by the log-rank test. Cox’s regression hazard analysis using a backward stepwise selection model was used for multivariate analysis.
Statistical significance was defined as a value of p < 0.05 in the present study. SPSS software for Windows version 22.0 was used for all calculations.
Ethics
The present study protocol was reviewed and approved by our institutional review board, and written informed consent for definitive chemoradiotherapy was obtained from each patient before conducting the treatment.
Results
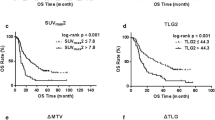
The characteristics of patients in group I and group II are summarized in Table 1. The median observation period of survivors was 68.0 months. Thirty-seven of total 78 patients had recurrence or residual in primary tumor and/or involved nodes after chemoradiotherapy. In only one patient with recurrence in primary tumor, regional lymph node metastatic recurrence occurred in elective nodal irradiation field. In twenty-eight patients, metastases occurred in distant organ or non-regional lymph node after chemoradiotherapy. In eight of the 28 patients, local recurrence occurred simultaneously. In all patients, the 3-year and 5-year OS were 36.9% [95% confidence interval (CI) 25.9–47.9%] and 30.8% (95% CI 20.2–41.4%), respectively (Fig. 2), and the 3-year and 5-year PFS rates were 22.2% (95% CI 12.8–31.6%) and 19.4% (95% CI 10.4–28.4%), respectively. There were no significant differences in OS and PFS rates between patients in whom FDG-PET was performed before treatment (n = 37) and patients in whom FDG-PET was not performed (n = 41) [5-year OS, 31.6% (95% CI 16.3–46.9%) vs. 30.5% (95% CI 15.6–45.4%), log-rank; p = 0.92 and 5-year PFS, 18.9% (95% CI 6.4–31.4%) vs. 19.8% (95% CI 7.1–32.5%), log-rank; p = 0.782] (Figs. 3, 4). Among the patients in whom FDG-PET was performed (group I), loco-regional recurrence and metastases in distant organ or non-regional lymph node occurred in 19 (51.4%) and 14 (37.8%) patients, respectively. Among patients in whom FDG-PET was not performed (group II), loco-regional recurrence and metastases in distant organ or non-regional lymph node occurred in 18 (43.9%) and 14 (34.1%) patients, respectively. There was no significant difference in patterns of failure (Table 2). In multivariate analysis for overall survival and progression-free survival, only gender (female was favorable) was selected as a significant prognostic factor (p = 0.018 and p = 0.028, respectively). FDG-PET was not selected.
Discussion
To the best of our knowledge, this is the first report on the inefficacy of FDG-PET for improving survival focused on locally advanced inoperable esophageal cancer. Wong et al. reported that PET can improve the accuracy of M staging for staging workup of patients with esophageal cancer who were potential candidates for curative therapy [3]. Katsoulis et al. reported that both the sensitivity and specificity of FDG-PET for the detection of distant organ metastases were better than those of CT (50% vs. 33% and 100% vs. 88%, respectively) (p < 0.05) [4]. Gilloes et al. reported that PET/CT provided additional information in 18.5% of patients and directly altered management in 17% of patients, 11% of patients were upstaged, 7.5% were downstaged, and 6% received radical treatment [5]. However, those studies included patients with all stages. Therefore, the positive impact of FDG-PET might not correspond to our results.
Metzger et al. reported that the treatment method was changed to palliative care due to PET-CT findings in only three of a total of 208 eligible patients [6]. Furthermore, a large prospective study showed that PET enabled detection of occult metastases in only 4% of patients [7]. It was almost consistent with the present study. The number of patients enrolled in the present study was relatively small, and the small number might have affected the results; however, it might be impossible to detect such small change in clinical study.
Since there was a significant difference in prognosis after chemoradiotherapy between patients with cT4NxM0 and those with M1 lymph metastasis [8], improvement of prognosis could be expected if FDG-PET has additional information to information provided by CT for patient with cT4NxM0 esophageal cancer. However, there were no differences in OS and PFS rates in the present study. Since T staging is dependent on CT and/or bronchoscopy in patients with T4 and without M1, FDG-PET can only enable a decision to be made for upstaging with findings of occult metastases. There is no possibility to make a decision for downstaging by FDG-PET in those patients. Inversely, M1 lym metastasis determined by CT cannot be ruled out by FDG-PET in consideration of the partial volume effect. For these reasons, FDG-PET seldom has a favorable impact for prognosis in patients with locally advanced inoperable esophageal cancer.
On the other hand, Metzger et al. reported that the use of PET-CT before chemoradiotherapy for patients with esophageal cancer had a favorable impact on survival. However, there was a difference in treatment between patients in whom FDG-PET was performed and those in whom FDG-PET was not performed. They suggested that the difference influenced the results [6]. They reported that no correlation was found between the use of PET-CT and OS in a definitive chemoradiotherapy subgroup, being consistent with our results. Unfortunately, there were also some differences in backgrounds and treatment methods between patients in whom FDG-PET was performed (group I) and those in whom FDG-PET was not performed (group II) in our study because most of patients in group II were treated before 2005, although some backgrounds of patients in whom FDG-PET was performed (group I) were better (e.g., age and PS). A prospective comparing study is needed to resolve this issue. However, if occult distant metastases were detected in only 4–5% of patients by FDG-PET [7], because the difference of OS between patients in whom FDG-PET was performed (group I) and those in whom FDG-PET was not performed (group II) is very small, twenty to thirty thousand patients per group is required and, therefore, it is not realistic.
There have been many reports showing that various parameters of FDG-PET including maximum standardized uptake value (\({\text{SU}}{{\text{V}}_{{\text{max}}}}\)), metabolic tumor volume (MTV) and decreasing SUV during radiotherapy could predict prognosis of patients with esophageal cancer [9, 10]. Although FDG-PET before treatment has seemed to be meaningful, our results suggested that FDG-PET in patients with cT4 and without M1 who have already undergone staging by CT (and/or bronchoscopy) has only limited significance.
However, there were some other limitations in this study. This study was performed in one institution. Nishimura et al. reported that the prognosis of esophageal cancer treated by definitive radiotherapy tended to depend on the number of cases experienced [11]. The present study was performed in one of the highest volume centers. We do not know if the results of this study apply equally to institutions. Furthermore, all of the patients enrolled in this study had squamous cell carcinoma. The histological background is different from that in Western countries, in which half of all esophageal malignancy cases are adenocarcinoma. We also do not know if the results of this study apply equally to other histological types.
Conclusions
Compared with only CT, information from FDG-PET is not associated with improving survival in patients with locally advanced inoperable esophageal cancer. Our results suggest that FDG-PET might not have much meaning for survival in locally advanced inoperable esophageal cancer.
Abbreviations
- FDG-PET:
-
Positron emission tomography using 18F-fluorodeoxyglucose
- GTV:
-
Gross tumor volume
- CTV-p:
-
Clinical target volume for the primary lesion
- PTV:
-
Planning target volume
- CDDP:
-
Cisplatin
- 5-FU:
-
5-Fluorouracil
- DOC:
-
Docetaxel
- CDGP:
-
Nedaplatin
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- CI:
-
Confidence interval
- \({\text{SU}}{{\text{V}}_{{\text{max}}}}\) :
-
Maximum standardized uptake value
References
Ferlay J, Soerjomataram I, Ervik M et al (2012) GLOBOCAN 2012: estimated cancer incidence, mortality and prevalence worldwide in 2012. International Agency for Research on Cancer (IARC), Lyon
Barber TW, Duong CP, Leong T et al (2012) 18F-FDG PET/CT has a high impact on patient management and provides powerful prognostic stratification in the primary staging of esophageal cancer: a prospective study with mature survival data. J Nucl Med 53(6):864–871
Wong R, Walker-Dilks C, Raifu A (2012) Evidence-based guideline recommendations on the use of positron emission tomography imaging in oesophageal cancer. Clin Oncol (R Coll Radiol) 24(2):86–104
Katsoulis IE, Wong WL, Mattheou AK et al (2007) Fluorine-18 fluorodeoxyglucose positron emission tomography in the preoperative staging of thoracic oesophageal and gastro-oesophageal junction cancer: a prospective study. Int J Surg 5(6):399–403
Gillies RS, Middleton MR, Maynard ND et al (2011) Additional benefit of 18F-fluorodeoxyglucose integrated positron emission tomography/computed tomography in the staging of oesophageal cancer. Eur Radiol 21(2):274–280
Metzger JC, Wollschläger D, Miederer M et al (2017) Inclusion of PET-CT into planning of primary or neoadjuvant chemoradiotherapy of esophageal cancer improves prognosis. Strahlenther Onkol 193(10):791–799
van Westreenen HL, Westerterp M, Sloof GW et al (2007) Limited additional value of positron emission tomography in staging esophageal cancer. Br J Surg 94:1515–1520
Jingu K, Umezawa R, Matsushita H et al (2016) Chemoradiotherapy for T4 and/or M1 lymph node esophageal cancer: experience since 2000 at a high-volume center in Japan. Int J Clin Oncol 21(2):276–282
Chen SW, Hsieh TC, Ding HJ et al (2014) Pretreatment metabolic tumor volumes to predict the short-term outcome of unresectable locally advanced squamous cell carcinoma of the esophagus treated with definitive chemoradiotherapy. Nucl Med Commun 35(3):291–297
Pan L, Gu P, Huang G et al (2009) Prognostic significance of SUV on PET/CT in patients with esophageal cancer: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol 21(9):1008–1015
Nishimura Y, Jingu K, Itasaka S et al (2016) Clinical outcomes of radiotherapy for esophageal cancer between 2004 and 2008: the second survey of the Japanese Radiation Oncology Study Group (JROSG). Int J Clin Oncol 21(1):88–94
Acknowledgements
This paper was presented at the 12th Congress of the World Federation of Nuclear Medicine and Biology to be held during 20–24th April 2018 in Melbourne.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
KJ, HM and KT participated in the design of the study, performed treatment, collected the data and drafted the manuscript; RU, TY, YI and NT and KT participated in the design of the study, performed treatment, and collected the data; and NK participated in the design of the study and performed treatment.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The present study protocol was reviewed and approved by Ethics Committee of Tohoku University Graduate School of Medicine (2014-1-541), and written informed consent for definitive chemoradiotherapy was obtained from each patient before conducting the treatment.
Availability of data and material
All data generated or analyzed during this study are included in this published article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Jingu, K., Umezawa, R., Yamamoto, T. et al. FDG-PET might not contribute to improving survival in patients with locally advanced inoperable esophageal cancer. Int J Clin Oncol 24, 927–933 (2019). https://doi.org/10.1007/s10147-019-01428-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-019-01428-8