Abstract
Background
To evaluate the oncological outcomes of patients with metastatic renal cell carcinoma (mRCC) involving the inferior vena cava (IVC) who received cytoreductive nephrectomy.
Methods
This study included 75 consecutive metastatis renal cell carcinoma (mRCC) patients with inferior vena cava (IVC) tumor thrombus undergoing cytoreductive nephrectomy and tumor thrombectomy followed by systemic therapy.
Results
Of the 75 patients, 11, 33, 24 and 7 had level I, II, III and IV IVC thrombus, respectively. Following surgical treatment, 25 (group A), 27 (group B) and 23 (group C) received cytokine therapy alone, molecular-targeted therapy alone and both therapies, respectively, as management for metastatic diseases. The median overall survival (OS) of the 75 patients was 16.2 months. No significant differences in OS were noted according to the level of the IVC tumor thrombus. There were no significant differences in OS among groups A, B and C; however, OS in groups B and C was significantly superior to that in group A. Furthermore, multivariate analysis of several parameters identified the following independent predictors of poor OS—elevated C-reactive protein, liver metastasis and postoperative treatment with cytokine therapy alone.
Conclusions
The prognosis of mRCC patients with IVC thrombus undergoing cytoreductive nephrectomy may be significantly affected by the type of postoperative systemic therapy rather than the level of the IVC tumor thrombus. Accordingly, cytoreductive nephrectomy should be considered as a major therapeutic option for patients with mRCC involving the IVC, particularly in the era of targeted therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The propensity to extend to the venous system is recognized as one of the most unique characteristics of renal cell carcinoma (RCC). In fact, the involvement of the renal vein and/or inferior vena cava (IVC) has been reported to be present in approximately 5–10% of cases with RCC [1,2,3,4]. Furthermore, nearly one-third of RCC patients with venous system involvement have also been shown to have metastatic diseases at the time of diagnosis [5]. Significantly better overall survival (OS) in mRCC patients treated with cytoreductive nephrectomy followed by interferon-α (IFN-α) relative to those treated with IFN-α alone was demonstrated in two prospective randomized trials [6, 7]. In addition, a combined assessment of these two trials confirmed an OS advantage of 5.8 months in patients receiving cytoreductive nephrectomy [8]. Considering these findings, it is currently regarded as a standard therapeutic option for mRCC patients to receive cytoreductive nephrectomy prior to the introduction of systemic therapy. However, despite the recent progress in surgical techniques as well as perioperative care, the surgical removal of the kidney with the attached tumor thrombus, particularly that with IVC thrombus, remains a challenging procedure. Accordingly, it is still controversial whether cytoreductive nephrectomy could contribute to survival improvement in mRCC patients with IVC tumor thrombus.
During the past decade, several types of novel molecular-targeted agents have been developed based on a precise understanding of the molecular mechanisms mediating the progression of RCC. These have been introduced into clinical practice for the treatment of mRCC patients, resulting in the widespread use of these agents and, thus marked changes in multimodal therapeutic strategies for mRCC [9, 10]. Previous studies suggested that the prognosis of mRCC patients with IVC tumor thrombus may be improved by surgical resection and systemic therapy; however, these studies were mainly conducted before the current era of targeted therapies [11, 12]. Although several randomized trials have been launched to clarify the survival benefit of surgical resection combined with systemic therapy using molecular-targeted agents for patients with mRCC, limited information is available with respect to the significance of cytoreductive nephrectomy in the era of targeted therapy [13].
Considering these findings, we conducted a retrospective evaluation of oncological outcomes in mRCC patients with IVC tumor thrombus who underwent cytoreductive nephrectomy and tumor thrombectomy followed by either cytokine therapy alone, molecular-targeted therapy alone or both at our institutions in order to identify factors most likely to affect the prognosis of this cohort of patients.
Patients and methods
Patients
At our institutions, a total of 86 consecutive RCC patients were radiologically diagnosed with evident metastases and IVC tumor thrombus between 1989 and 2016. Of these 86 patients, 7 were treated with systemic therapy alone, while the remaining 79 received cytoreductive nephrectomy and IVC tumor thrombectomy. Of the 79 patients, 4 were excluded who were undergoing surgical therapy (2 died in the perioperative period and 2 did not receive postoperative systemic therapy due to the rapid progression of metastatic disease), leaving 75 patients to be included in the study. The design of this study was approved by the Research Ethics Committee of our institutions, and informed consent was waived due to the retrospective design of the study.
Evaluation
Information on the clinicopathological data of the included patients was retrieved from their medical records. All of the 75 patients underwent routine blood tests, chest and abdominal computed tomography (CT) and abdominal magnetic resonance imaging (MRI) prior to the surgery, and brain CT or bone scintigraphy was performed in selected patients. As baseline evaluations prior to surgery, clinicopathological examinations and performance status (PS) were assessed based on the seventh edition of the UICC TNM classification system and Karnofsky PS scale, respectively, while risk classification was performed using the Memorial Sloan-Kettering Cancer Center (MSKCC) system [14]. Gross extension of the tumor thrombus into the IVC was assessed by preoperative findings on contrast-enhanced CT and the sagittal view of MRI, and confirmed intraoperatively in these 75 patients. In this series, the level of the IVC tumor thrombus was classified according to the Mayo system as follows—level I, thrombus extending into the IVC to ≤2 cm above the renal vein; level II, thrombus extending into the IVC to >2 cm above the renal vein but not to the hepatic vein; level III, thrombus extending into the IVC to above the hepatic vein but not to the diaphragm; and level IV, thrombus extending into the supra diaphragmatic IVC or right atrium [15]. The detailed surgical procedures conducted in this series were previously reported [4, 16].
Treatment for metastatic diseases
As postoperative systemic therapies for metastatic diseases, immunotherapies using IFN-α and/or interleukin-2 were provided for all patients until 2007; however, molecular-targeted therapies were mainly selected thereafter due to the approval of targeted agents in Japan. Generally, dose modification of each agent was permitted based on the judgement of each physician considering the severity of adverse events. As a rule, all patients were followed by laboratory as well as radiological examinations every 6–12 weeks.
Statistical analysis
OS, which was defined as the time from cytoreductive nephrectomy to that of death due to any cause or the last follow-up, was calculated using the Kaplan–Meier method, and the differences were determined by the log-rank test. The prognostic significance of certain factors was evaluated employing the Cox proportional hazards regression model. All statistical analyses were performed using Statview 5.0 software (Abacus Concepts, Inc., Berkeley, CA, USA), and P < 0.05 was considered significant.
Results
Table 1 summarizes the clinicopathological characteristics of the 75 patients included in this study. All 75 patients underwent cytoreductive nephrectomy and IVC tumor thrombectomy, and were pathologically diagnosed with RCC. Of these 75 patients, 11 (14.7%), 33 (44.0%), 24 (32.0%) and 7 (9.3%) were judged to have level I, II, III and IV IVC thrombus, respectively, according to the Mayo system for classification of IVC tumor thrombus level [15]. Following surgery, systemic therapy for the management of metastatic diseases was introduced in all of the 75 patients, consisting of 25 (33.3%, group A), 27 (36.0%, group B) and 23 (30.7%, group C) who received cytokine therapy alone, molecular-targeted therapy alone and both therapies by introducing cytokine therapy followed by molecular-targeted therapy, respectively.
During the observation period (median 12.2 months; range 3.7–69.7 months), 45 (66.7%) of the 75 patients died. The 1-, 3- and 5-year OS rates were 63.3, 31.6 and 20.1%, respectively, and the median duration of OS in the 75 patients was 16.2 months (Fig. 1).
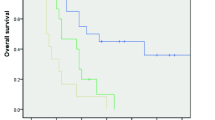
The differences in OS according to the level of the IVC tumor thrombus as well as the type of postoperative systemic therapy were then assessed. Regarding the level of IVC tumor thrombus, there were no significant differences in OS among the 4 groups classified according to the Mayo system [15] or between patients with levels I and II IVC thrombus versus those with levels III and IV IVC thrombus (Fig. 2). Moreover, there were no significant differences in OS among groups A, B and C; however, OS in groups B and C was significantly more favorable compared with that in group A (Fig. 3).
a Comparison of overall survival of patients with metastatic renal cell carcinoma (mRCC) involving the inferior vena cava (IVC) who received cytoreductive nephrectomy among four groups according to the level of the IVC tumor thrombus (level I, II, III vs IV). b Comparison of overall survival of patients with mRCC involving the IVC who received cytoreductive nephrectomy between two groups according to the level of the IVC tumor thrombus (levels I and II vs levels III and IV)
a Comparison of overall survival of patients with metastatic renal cell carcinoma (mRCC) involving the inferior vena cava (IVC) who received cytoreductive nephrectomy among three groups according to the type of postoperative systemic therapy (group A, B vs C). b Comparison of overall survival of patients with mRCC involving the IVC who received cytoreductive nephrectomy between two groups according to the type of postoperative systemic therapy (group A vs groups B and C)
Table 2 presents the findings on uni- and multivariate analyses evaluating the significance of several clinicopathological parameters as predictors of OS in the 75 patients. Of several factors examined, the tumor grade, MSKCC classification, preoperative value of C-reactive protein (CRP), bone metastasis, liver metastasis and type of postoperative systemic therapy, but not the level of the IVC tumor thrombus, were shown to be significantly correlated with OS by univariate analysis. Of these significant factors, only the preoperative CRP value, liver metastasis and type of postoperative systemic therapy were identified as independent predictors of OS on multivariate analysis.
Discussion
The extension of a tumor thrombus into the venous system is observed in up to approximately 10% of patients with RCC [1,2,3,4]. Despite being regarded as one of the most challenging surgeries in the field of urology, radical nephrectomy and tumor thrombectomy remain the standard treatments for RCC patients with a venous tumor thrombus, irrespective of its maximal level; however, it has been well-recognized that mRCC concurrently involving the venous system, particularly the IVC, is extremely aggressive [5]. In fact, several studies have identified the presence of metastasis as the strongest independent prognostic indicator in patients with RCC extending into the venous system [1, 2]. We also previously investigated the clinical outcome in 135 RCC patients with a venous tumor thrombus, and found that the presence of metastasis in addition to tumor size were independently associated with cancer-specific survival on multivariate analysis [4]. Furthermore, it is necessary to consider the impact of recently introduced molecular-targeted agents, which have been shown to markedly prolong the survival of mRCC patients compared with that in the era of cytokine therapy [9, 10], when determining the therapeutic strategy for mRCC patients with a venous tumor thromubus. Accordingly, it remains controversial whether cytoreductive nephrectomy and tumor thrombectomy significantly contribute to improve the prognosis of mRCC patients in the era of targeted therapy.
To date, there have been a limited number of studies evaluating the role of cytoreductive nephrectomy and tumor thrombectomy in mRCC patients with IVC tumor thrombus [11,12,13]. Two small retrospective studies previously suggested improved survival after surgical resection of mRCC patients with IVC tumor thrombus; however, these were conducted prior to the introduction of molecular-targeted agents [11, 12]. In addition, Westesson et al. [13] recently reported the favorable survival of mRCC patients with IVC tumor thrombus; however, it seems to be clear that this study consisted of a highly selected group of patients considering the good PS as well as the low volume of extrarenal disease [13]. Considering these findings, we retrospectively analyzed the oncological outcome in a total of 75 mRCC patients involving the IVC who were treated with cytoreductive nephrectomy and tumor thrombectomy followed by systemic therapy in order to clarify the prognostic significance of surgical therapy in this cohort of patients.
In this series, all of the 75 patients underwent cytoreductive nephrectomy and IVC thrombectomy, followed by postoperative systemic therapy for metastatic diseases. To our knowledge, this represents the largest study with available follow-up information on mRCC patients undergoing cytoreductive nephrectomy. At our institutions, surgical therapy has been provided as a standard treatment for RCC patients with IVC tumor thrombus, irrespective of the presence of metastases; therefore, the distribution of the level of the IVC thrombus evaluated by the Mayo system [15] was comparable to that reported in previous studies targeting overall patients with RCC involving the IVC [5]. In addition, the proportion of patients receiving cytokine therapy alone, molecular-targeted therapy alone and both following surgery was similar in this study. Collectively, these findings suggest that the characteristics of patients included in this study may be suitable for comprehensively investigating the prognostic significance of surgical therapy in mRCC patients with IVC tumor thrombus.
In several previous studies, the prognosis of mRCC patients with IVC thrombus receiving systemic therapy alone was reported to be extremely poor, i.e., the median survival ranged from 3.5−5 months with a mortality rate of >70% within 1 year [5, 17]. However, when surgical therapies were combined, the prognosis of mRCC patients with IVC tumor thrombus was shown to be relatively improved in a few previous studies [11,12,13, 18]. For example, Whitson et al. reported a 1-year disease-specific survival rate of 60% in mRCC patients treated with cytoreductive nephrectomy and IVC thrombectomy [18], while Westesson et al. revealed that the median interval of OS after surgery was 14 months in 60 mRCC patients with IVC thrombus, including 6 without postoperative systemic therapy [13]. In the present series, the median duration of OS in the 75 included patients was 16.2 months, which was the most favorable prognostic outcome among studies evaluating the prognosis of mRCC patients with IVC tumor thrombus undergoing surgical management.
No reliable model system has been developed to precisely reflect the postoperative prognosis of patients with RCC involving the IVC, especially those with metastatic diseases; therefore, it is of interest to identify parameters associated with OS in patients included in this study. In the present series, despite the lack of a significant impact of the level of IVC thrombus on OS, the elevation of the preoperative CRP value, the presence of liver metastasis and postoperative systemic treatment with cytokines alone were identified as independent predictive factors of poor OS. Although the prognostic significance of the extent of the IVC tumor thrombus has been widely examined, the findings on this point were not consistent, but relatively large series demonstrated no prognostic differences according to the level of the IVC thrombus [1,2,3,4,5]. Furthermore, in mRCC patients with IVC tumor thrombus, no significant effect of the extent of the IVC thrombus on postoperative survival was previously noted [13]. Taken together, it may not be important to consider the level of IVC tumor thrombus from a postoperative prognostic viewpoint when determining the therapeutic strategy for mRCC patients with IVC tumor thrombus.
Another point of interest is the role of cytoreductive nephrectomy for mRCC patients with IVC thrombus in the era of molecular-targeted therapy. Petrelli et al. recently conducted a meta-analysis and showed that mRCC patients treated with cytoreductive nephrectomy and a targeted agent had their risk of death reduced by >50% compared with those receiving targeted therapy alone [19]. In this study, OS in mRCC patients with an IVC thrombus receiving either targeted therapy alone or both cytokine and targeted therapies after surgery was significantly more favorable compared with those receiving cytokine therapy alone, despite the lack of significant differences in the major clinicopathological parameters among these three groups (data not shown). Furthermore, postoperative treatment with cytokine therapy alone appeared to be an independent factor associated with poor OS, irrespective of other parameters. Similarly, Westesson et al. also reported significantly superior median postoperative survival of mRCC patients with IVC thrombus who were treated with targeted agents compared to those treated with cytokines (20 vs 12 months) [13]. Taken together, even with the extension of a venous thrombus into the IVC, mRCC patients may be likely to benefit from cytoreductive nephrectomy and tumor thrombectomy if targeted agents can be introduced postoperatively.
We would like to emphasize several limitations of this study. First, despite this being the largest series including mRCC patients with IVC tumor thrombus receiving systemic therapy following cytoreductive surgery, this was a retrospective study involving multiple surgeons as operators, which could possibly affect the findings of this study. Second, there might be significant differences in the therapeutic strategy for mRCC among the previous and present studies, such as the indication of metastatectomy and sequential order of agents introduced as systemic therapy; thus, the present outcome should be interpreted considering this point. In particular, for the assessment of the impact of systemic therapies on the prognosis of mRCC patients receiving cytoreductive nephrectomy, the optimal classification system based on the types of postoperative systemic therapies should be further discussed, since the current classification may result in possible selection bias due to the inclusion of patients receiving both cytokine and molecular-targeted therapies. Fourth, several parameters possibly associated with the prognosis of the included patients in this study, such as PS, volume of extrarenal disease and laboratory abnormalities, were not evaluated. Finally, the strategy of systemic therapy against mRCC is currently changing, including the introduction of immune checkpoint inhibitors and the use of targeted agents in pre- and/or postoperative settings, which may result in an obstacle for the application of the present findings to future clinical practice.
In conclusion, the findings presented in this study suggest that mRCC patients who underwent cytoreductive nephrectomy and IVC tumor thrombectomy could achieve comparatively favorable oncological outcomes, shown to be markedly affected by the type of postoperative systemic therapy rather than the level of the IVC tumor thrombus. Therefore, cytoreductive nephrectomy and IVC tumor thrombectomy should be considered as major therapeutic options for mRCC patients with a venous tumor thrombus extending into the IVC, particularly in the era of targeted therapy.
References
Klatte T, Pantuck AJ, Riggs SB et al (2007) Prognostic factors for renal cell carcinoma with tumor thrombus extension. J Urol 178:1189–1195
Wagner B, Patard JJ, Méjean A et al (2009) Prognostic value of renal vein and inferior vena cava involvement in renal cell carcinoma. Eur Urol 55:452–459
Martínez-Salamanca JI, Huang WC, Millán I et al (2011) Prognostic impact of the 2009 UICC/AJCC TNM staging system for renal cell carcinoma with venous extension. Eur Urol 59:120–127
Miyake H, Terakawa T, Furukawa J et al (2012) Prognostic significance of tumor extension into venous system in patients undergoing surgical treatment for renal cell carcinoma with venous tumor thrombus. Eur J Surg Oncol 38:630–636
Reese AC, Whitson JM, Meng MV (2013) Natural history of untreated renal cell carcinoma with venous tumor thrombus. Urol Oncol 31:1305–1309
Flanigan RC, Salmon SE, Blumenstein BA et al (2001) Nephrectomy followed by interferon α-2b compared with interferon α-2b alone for metastatic renal-cell cancer. N Engl J Med 345:1655–1659
Mickisch GH, Garin A, van Poppel H et al (2001) Radical nephrectomy plus interferon-α-based immunotherapy compared with interferon α alone in metastatic renal-cell carcinoma: a randomised trial. Lancet 358:966–970
Flanigan RC, Mickisch G, Sylvester R et al (2004) Cytoreductive nephrectomy in patients with metastatic renal cancer: a combined analysis. J Urol 171:1071–1076
Figlin R, Sternberg C, Wood CG (2012) Novel agents and approaches for advanced renal cell carcinoma. J Urol 188:707–715
Bedke J, Gauler T, Grünwald V et al (2017) Systemic therapy in metastatic renal cell carcinoma. World J Urol 35:179–188
Slaton JW, Balbay MD, Levy DA et al (1997) Nephrectomy and vena caval thrombectomy in patients with metastatic renal cell carcinoma. Urology 50:673–677
Naitoh J, Kaplan A, Dorey F et al (1999) Metastatic renal cell carcinoma with concurrent inferior vena caval invasion: long-term survival after combination therapy with radical nephrectomy, vena caval thrombectomy and postoperative immunotherapy. J Urol 162:46–50
Westesson KE, Klink JC, Rabets JC et al (2014) Surgical outcomes after cytoreductive nephrectomy with inferior vena cava thrombectomy. Urology 84:1414–1419
Motzer RJ, Bacik J, Murphy BA (2002) Interferon-α as a comparative treatment for clinical trials of new therapies against advanced renal cell carcinoma. J Clin Oncol 20:289–296
Neves RJ, Zincke H (1987) Surgical treatment of renal cancer with vena cava extension. Br J Urol 59:390–395
Tsuji Y, Goto A, Hara I et al (2001) Renal cell carcinoma with extension of tumor thrombus into the vena cava: surgical strategy and prognosis. J Vasc Surg 33:789–796
Staehler M (2011) The role of metastasectomy in metastatic renal cell carcinoma. Nat Rev Urol 8:180–181
Whitson JM, Reese AC, Meng MV (2013) Population based analysis of survival in patients with renal cell carcinoma and venous tumor thrombus. Urol Oncol 31:259–263
Petrelli F, Coinu A, Vavassori I et al (2016) Cytoreductive nephrectomy in metastatic renal cell carcinoma teated with targeted therapies: a systematic review with a meta-analysis. Clin Genitourin Cancer 14:465–472
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have declared no conflict of interest.
About this article
Cite this article
Miyake, H., Sugiyama, T., Aki, R. et al. Oncological outcomes after cytoreductive nephrectomy for patients with metastatic renal cell carcinoma with inferior vena caval tumor thrombus. Int J Clin Oncol 23, 553–558 (2018). https://doi.org/10.1007/s10147-017-1232-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-017-1232-9