Abstract
Background
Various systemic inflammatory and nutritional scores have been reported to predict postoperative outcomes. This study aimed to investigate the best systemic inflammatory and nutritional scores in colorectal cancer (CRC) patients who underwent potentially curative resection.
Method
We evaluated 468 consecutive CRC patients in this study. Comparisons of systemic inflammatory and nutritional scores, including the neutrophil to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR), prognostic index (PI), prognostic nutritional index (PNI), and modified Glasgow prognostic score (mGPS), were performed using univariate/multivariate analyses for patient survival.
Results
The PNI and mGPS, but not the NLR, PLR, and PI, were significantly associated with overall and relapse-free survival. The mGPS, but not the PNI, was strongly correlated with TNM stage (P < 0.001). Cox multivariate analysis showed that both the PNI and mGPS were exclusive independent prognostic factors for both overall and relapse-free survival (P < 0.001). Furthermore, the PNI status predicted patient survival more clearly than the mGPS in combination with TNM stage.
Conclusions
This study suggests that the PNI and mGPS are useful predictive scores in CRC patients who undergo potentially curative resection, especially the PNI in combination with TNM stage. Routine evaluation of the host status using the scores may be useful in CRC treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer patients are often in an accelerated metabolic state, and inflammation status is reportedly related to the degree of cancer progression [1]. In gastrointestinal cancer patients, difficulty in nutrient intake sometimes appears in the perioperative period, leading to poor postoperative outcomes [2]. Nutritional management is indispensable for successful gastrointestinal surgery. Therefore, various systemic inflammatory and nutritional scores have been reported to predict postoperative complications [3,4,5], recurrence, or prognosis [6]. However, in cancer patients, the type of cancer, location, histopathological type, and stage are not the same. Consequently, which is the best predictive score depending on the case needs to be considered.
In colorectal cancer (CRC) patients who underwent potentially curative resection, Park et al. recently reported that the combination of TNM stage and modified Glasgow prognostic score (mGPS) stratified postoperative outcomes [7]. However, how this finding might be used for Japanese patients and whether the mGPS is the best systemic inflammatory and nutritional score are still unclear because of different body types or dietary habits. As curative resection is the best treatment protocol in CRC, preoperative prediction of postoperative recurrence and prognosis is helpful in clinical use.
Therefore, in the present study, we aimed to determine the prognostic impact of systemic inflammatory and nutritional scores using a database of 468 CRC patients who underwent potentially curative resection. Our data may indicate the characteristics and usefulness of each score for CRC.
Methods
Patients
A total of 591 consecutive patients with primary CRC underwent colectomy at Kumamoto University Hospital in Kumamoto, Japan, from March 2005 to August 2014. Of these, 472 patients underwent potentially curative resection. Survival data were available in all cases. Among them, we excluded four patients for whom necessary preoperative data for calculating systemic inflammatory and nutritional scores were unavailable. Finally, a total of 468 patients were enrolled in this study (277 (59.2%) men and 191 (40.8%) women), with a mean age of 68 years (range 19–93 years).
Study design
Treatment data were obtained retrospectively from the patient records. Patients were observed until their death or until July 31, 2016, whichever came first. The mean follow-up time was 48.5 months (range 2–124 months). Surgical procedures, including the extent of colectomy and lymph node dissection, were based on the Japanese CRC treatment guidelines [8,9,10]. Disease staging was performed according to the 7th edition of Union for International Cancer Control classification [11]. Follow-up of all patients was carried out in our hospital or affiliated hospitals. Tumor markers were checked every 3 months and diagnostic imaging was performed at least every 6 months, based on surveillance suggested in the guidelines. In cases of suspected recurrence, ethoxybenzyl-magnetic resonance imaging or positron emission tomography-computed tomography was added to the diagnostic imaging. Use of the clinical data was approved by the human ethics review committee of the Graduate School of Medicine, Kumamoto University.
Systemic inflammatory and nutritional scores and other markers
Serum samples were collected and measured within 2 weeks prior to potentially curative resection. Laboratory measurements included C-reactive protein (CRP) levels, albumin levels, and white blood cell, neutrophil, lymphocyte, and platelet counts. We determined the following systemic inflammatory and nutritional scores—neutrophil to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR), prognostic index (PI), prognostic nutritional index (PNI), and mGPS, which were calculated as described in Supplementary Table 1. Cut-off values were determined according to previous reports. Briefly, the NLR was calculated by dividing the absolute neutrophil count by the absolute lymphocyte count. An NLR ≥5 was considered elevated [12]. The same calculation was applied to derive the PLR. A PLR ≥300 was considered elevated [13]. For PI scoring, patients with an elevated CRP serum level (>10 mg/L) and elevated white cell count (>11 × 109/L) were classified as PI 2; those with either abnormality were classified as PI 1, and those with neither abnormality were classified as PI 0 [14]. The PNI was calculated as follows—albumin value (g/Ll) +0.005 × total lymphocyte count. A PNI <45 was considered decreased [15]. In mGPS scoring, patients with an elevated CRP serum level (>10 mg/L) and hypoalbuminemia (<35 g/L) were classified as mGPS 2; those with either abnormality were classified as mGPS 1, and those with neither abnormality were classified as mGPS 0 [7].
Patient body mass index (BMI) was calculated from preoperative height and weight, which were measured by our clinical staff on the date of admission. BMI was divided into three groups—<18.5, 18.5–24.9, and ≥25. The cut-off values for serum carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9 (CA19-9) levels were set at 5.0 ng/ml [16] and 37 U/ml [17], respectively.
Statistical analysis
All statistical analyses were performed using JMP statistical software package version 10 (SAS Institute Inc., Cary, NC, USA) and Excel 2010 (Microsoft, Redmond, WA, USA). All analyses were performed in patients for whom all systemic inflammatory and nutritional scores were available (n = 468).
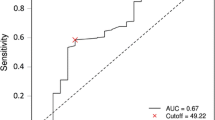
Univariate analyses were performed to investigate clinicopathological factors and systemic inflammatory and nutritional scores. The chi-squared test was used for categorical data and Student’s t test was used for age. The P value for significance was adjusted for multiple hypothesis testing by Bonferroni correction to P = 0.0045 (=0.05/11). The Kaplan–Meier method and log-rank test were used for survival analysis according to systemic inflammatory and nutritional score status. Cox proportional hazards regression models were used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs). Backward elimination was performed with a threshold of P = 0.05 to avoid overfitting. A P value of <0.05 was considered statistically significant in all multivariate analyses.
Results
Associations of systemic inflammatory and nutritional score status with the patient survival
Preoperative systemic inflammatory and nutritional scores for the 468 patients were constructed as mentioned above. Figure 1 shows the associations of systemic inflammatory and nutritional score status with overall survival (OS) and relapse-free survival (RFS). The PNI and mGPS, but not the NLR, PLR, PI, were significantly associated with both OS and RFS. The 5-year OS was 90.0 and 66.7% (P < 0.001), and the 5-year RFS was 83.2 and 57.2% (P < 0.001) with a high PNI and low PNI status, respectively. The 5-year OS was 88.0, 63.3, and 72.1% (P < 0.001), and the 5-year RFS was 80.8, 56.0, and 58.6% (P < 0.001) with mGPS 0, 1, and 2 status, respectively.
Associations of systemic inflammatory and nutritional score status with clinicopathological factors
We investigated the associations of PNI and mGPS status with clinicopathological factors because they had a strong correlation with patient survival. According to mGPS, we analysed them after integrating the mGPS 1 with the mGPS 2, because of similar survival data (Table 1). The mean age of low PNI status patients (71.3 ± 12.1 years) was significantly higher than that of high PNI status patients (65.9 ± 12.0 years, P < 0.001). However, the mGPS status did not show a significant correlation with age (P = 0.101). Both the PNI and the mGPS status showed a strong correlation with BMI, depth of tumor invasion, CEA levels, and CA19-9 levels. Interestingly, only the mGPS status showed a strong correlation with TNM stage (P < 0.001). All of these factors remained after Bonferroni correction (P < 0.0045; =0.05/11).
We also investigated the associations of NLR, PLR, and PI status with clinicopathological factors to identify the characteristic of each status (Supplementary Table 2). The NLR status did not have a strong correlation with clinicopathological factors, and the PLR status only had a strong correlation with BMI (P < 0.001). Additionally, the PI status showed a strong correlation with depth of tumor invasion (P < 0.001), TNM stage (P < 0.001), and histopathological type (P < 0.001).
Analysis for survival using systemic inflammatory and nutritional score status and clinicopathological factors
We next identified the factors that affected the survival of CRC patients who underwent potentially curative resection (Table 2). In our dataset (n = 468), postoperative recurrence occurred in 61 (13.0%) patients—eight (4.1%) in stage I, 20 (13.4%) in stage II, and 33 (27.0%) in stage III.
In univariate analysis, the PNI (P < 0.001) and mGPS (P < 0.001) were significantly associated with both OS and RFS. In addition, in multivariate analysis, we adjusted for clinicopathological factors that showed a significant difference for survival in univariate analysis to identify the usefulness of the PNI and mGPS (Table 2). Cox multivariate analysis showed that both the PNI and the mGPS were exclusive independent prognostic factors for both OS (P < 0.001) and RFS (P < 0.001).
Associations of PNI or mGPS status with TNM stage in predicting patient survival
We re-analyzed the association of PNI or mGPS status with patient OS and RFS in each TNM stage (Table 3). Subgroup analysis showed that in stage I and III, there were significant associations of PNI or mGPS with both OS and RFS. However, in stage II, PNI but not mGPS, had significant associations with OS and RFS.
Furthermore, OS and RFS were significantly different among the combinations of PNI or mGPS and TNM stage status (Fig. 2). Of interest for both OS and RFS, stage II patients with a low PNI status had worse survival than stage III patients with a high PNI status. However, the combination of mGPS and TNM stage status did not show the difference.
Overall (OS) and relapse-free survival (RFS) curves according to the combination of TNM stage and preoperative PNI or mGPS status. a, b OS (a) and RFS (b) curves according to the combination of TNM stage and preoperative PNI. c, d OS (c) and RFS (d) curves according to the combination of TNM stage and preoperative mGPS
Discussion
This study examined the associations of systemic inflammatory and nutritional scores, including the NLR, PLR, PI, PNI, and mGPS, with clinicopathological factors and survival of CRC patients who underwent potentially curative resection. We found that the PNI and mGPS could predict postoperative recurrence and prognosis. Additionally, in combination with TNM stage, the PNI predicted patient survival more clearly than the mGPS. This combination may be a useful strategy as a preoperative predictive method.
Systemic inflammatory and nutritional scores reportedly play an important role in various cancers in certain situations. Previous reports have shown that inflammation promotes tumor invasion and metastasis, through activation of interleukin-6 and recruitment of regulatory T lymphocytes [18]. In addition, malnutrition is a commonly encountered problem when treating CRC patients. Serum albumin levels are closely correlated with the degree of malnutrition and are also correlated with the prognosis in CRC patients [19]. Therefore, various systemic inflammatory and nutritional scores have been developed, which can reflect host status and predict cancer progression. However, there are few reports that have compared the five well-known scores of the NLR, PLR, PI, PNI, and mGPS [14, 20]. In patients with CRC who underwent potentially curative resection, Guthrie et al. demonstrated that the mGPS was an independent predictor of poor cancer-specific survival [21]. However, their study only compared the mGPS with the NLR.
Our study showed that the PNI and mGPS were selectively effective scores for CRC patients who underwent potentially curative resection. Interestingly, mGPS status, but not PNI status, had a strong correlation with TNM stage. In addition, subgroup analysis showed that PNI status predicted survival of stage II patients more clearly. Our data support previous reports showing that the PNI and mGPS are effective prognostic scores for cancer patients [7, 15]. However, although the NLR, PLR, and PI have been reported as predictive scores for cancer patients, they were not predictive in our study. This result might have been caused by the relatively small number of positive cases, or the scores were not suitable for CRC patients who underwent potentially curative resection.
The NLR, PLR, PI, PNI, and mGPS showed various characteristics in relation to clinicopathological factors in our study. Although the PI, PNI, and mGPS showed a strong correlation with tumor status, such as depth of tumor invasion, only the PI and mGPS were correlated with TNM stage. On the other hand, the PNI had a strong correlation with both age and BMI. The NLR and PLR are reportedly not useful predictive scores for curative resected cases, but are useful for inoperable cases and cases that received chemotherapy which have strong inflammation caused by the tumor [22,23,24,25]. However, the PNI and mGPS are validated prognostic factors even in cancer patients who underwent potentially curative resection [7, 15, 21, 26]. In our study, the PNI was a slightly more effective prognostic score than the mGPS, probably because of a closer relationship with host status. Furthermore, a report by Park et al. on mGPS status (n = 1000) [7] showed a ratio of 20.7% for mGPS 1 (our result 18.0%) and 15.8% for mGPS 2 (approximately double our result of 7.6%). In Japan, there are fewer patients with mGPS 2. The appropriate score may need to be used in a particular situation, depending on a patient’s body type or dietary habit.
CRC is a major cause of death worldwide. Molecular cancer research has shown that CRC can be divided into subtypes [27]. The malignancy potential or stage of cancer progression itself predicts patient outcomes. However, success in treatment, especially in surgery, also requires a stable host status. Therefore, systemic inflammatory and nutritional scores indicating the host status using commonly used serum data may be useful for routine medical care.
There are some limitations in this study. First, our dataset did not include data of visceral fat or sarcopenia, which is reportedly related to cancer progression [28, 29]. However, prognostic scores should be easy to use and simple. Second, nutritional disorders in cancer patients occur not only by cancer pathology itself, but also by preoperative chemotherapy or radiotherapy. In our study, the PNI and mGPS did not show a significant correlation with preoperative chemotherapy because of the small number of cases. Third, this study was retrospective and was performed at a single institution. Nevertheless, this is the first study to compare the significance of five systemic inflammatory and nutritional scores for CRC patients who underwent potentially curative resection, based on a dataset of 468 patients. Large-scale prospective studies accounting for these scores are needed to confirm our findings.
In conclusion, this study shows that the PNI and mGPS may be a useful predictive score in CRC patients who undergo potentially curative resection, especially the PNI in combination with TNM stage. Additionally, large-scale studies are warranted to assess the clinical utility of systemic inflammatory and nutritional scores.
Abbreviations
- CRC:
-
Colorectal cancer
- mGPS:
-
Modified Glasgow prognostic score
- CRP:
-
C-reactive protein
- NLR:
-
Neutrophil to lymphocyte ratio
- PLR:
-
Platelet to lymphocyte ratio
- PI:
-
Prognostic index
- PNI:
-
Prognostic nutritional index
- BMI:
-
Body mass index
- CEA:
-
Carcinoembryonic antigen
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- OS:
-
Overall survival
- DFS:
-
Disease-free survival
References
Oshima H, Nakayama M, Han TS et al (2015) Suppressing TGFbeta signaling in regenerating epithelia in an inflammatory microenvironment is sufficient to cause invasive intestinal cancer. Cancer Res 75:766–776
Bozzetti F (2002) Rationale and indications for preoperative feeding of malnourished surgical cancer patients. Nutrition 18:953–959
Meguid MM, Mughal MM, Debonis D et al (1986) Influence of nutritional status on the resumption of adequate food intake in patients recovering from colorectal cancer operations. Surg Clin North Am 66:1167–1176
Onodera T, Goseki N, Kosaki G (2014) Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi 10:1–7
Onodera T, Goseki N, Kosaki G (1984) Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi 85:1001–1005
Gomes de Lima KV, Maio R (2012) Nutritional status, systemic inflammation and prognosis of patients with gastrointestinal cancer. Nutr Hosp 27:707–714
Park JH, Watt DG, Roxburgh CS et al. (2015) colorectal cancer, systemic inflammation, and outcome: staging the tumor and staging the host. Ann Surg. 236(2): 326−36
The Japanese society for cancer of the colon and rectum (2005) JSCCR guidelines 2005 for the treatment of colorectal cancer. Kanehara and Co., Ltd, Tokyo
The Japanese society for cancer of the colon and rectum (2010) JSCCR Guidelines 2010 for the treatment of colorectal cancer. Kanehara and Co., Ltd, Tokyo
Watanabe T, Itabashi M, Shimada Y et al (2012) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol 17:1–29
Sobin LHGMWC (2009) TNM classification of malignant tumours, 7th edn. Wiley-Blackwell, New York
Mallappa S, Sinha A, Gupta S et al (2013) Preoperative neutrophil to lymphocyte ratio >5 is a prognostic factor for recurrent colorectal cancer. Colorectal Dis 15:323–328
Smith RA, Bosonnet L, Raraty M et al (2009) Preoperative platelet-lymphocyte ratio is an independent significant prognostic marker in resected pancreatic ductal adenocarcinoma. Am J Surg 197:466–472
Proctor MJ, Morrison DS, Talwar D et al (2011) A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow Inflammation Outcome Study. Eur J Cancer 47:2633–2641
Mohri Y, Inoue Y, Tanaka K et al (2013) Prognostic nutritional index predicts postoperative outcome in colorectal cancer. World J Surg 37:2688–2692
Tarantino I, Warschkow R, Worni M et al (2012) Elevated preoperative CEA is associated with worse survival in stage I-III rectal cancer patients. Br J Cancer 107:266–274
Stiksma J, Grootendorst DC, van der Linden PW (2014) CA 19-9 as a marker in addition to CEA to monitor colorectal cancer. Clin Colorectal Cancer 13:239–244
Mantovani A, Allavena P, Sica A et al (2008) Cancer-related inflammation. Nature 454:436–444
Heys SD, Walker LG, Deehan DJ et al (1998) Serum albumin: a prognostic indicator in patients with colorectal cancer. J R Coll Surg Edinb 43:163–168
Kinoshita A, Onoda H, Imai N et al (2012) Comparison of the prognostic value of inflammation-based prognostic scores in patients with hepatocellular carcinoma. Br J Cancer 107:988–993
Guthrie GJ, Roxburgh CS, Farhan-Alanie OM et al (2013) Comparison of the prognostic value of longitudinal measurements of systemic inflammation in patients undergoing curative resection of colorectal cancer. Br J Cancer 109:24–28
Cedres S, Torrejon D, Martinez A et al (2012) Neutrophil to lymphocyte ratio (NLR) as an indicator of poor prognosis in stage IV non-small cell lung cancer. Clin Transl Oncol 14:864–869
Jin H, Zhang G, Liu X et al (2013) Blood neutrophil-lymphocyte ratio predicts survival for stages III-IV gastric cancer treated with neoadjuvant chemotherapy. World J Surg Oncol 11:112
Lee S, Oh SY, Kim SH et al (2013) Prognostic significance of neutrophil lymphocyte ratio and platelet lymphocyte ratio in advanced gastric cancer patients treated with FOLFOX chemotherapy. BMC Cancer 13:350
Yao Y, Yuan D, Liu H et al (2013) Pretreatment neutrophil to lymphocyte ratio is associated with response to therapy and prognosis of advanced non-small cell lung cancer patients treated with first-line platinum-based chemotherapy. Cancer Immunol Immunother 62:471–479
Tokunaga R, Sakamoto Y, Nakagawa S et al (2015) Prognostic nutritional index predicts severe complications, recurrence, and poor prognosis in patients with colorectal cancer undergoing primary tumor resection. Dis Colon Rectum 58:1048–1057
Dutta S, Crumley AB, Fullarton GM et al (2012) Comparison of the prognostic value of tumour and patient related factors in patients undergoing potentially curative resection of gastric cancer. Am J Surg 204:294–299
Miyamoto Y, Baba Y, Sakamoto Y et al (2015) Sarcopenia is a negative prognostic factor after curative resection of colorectal cancer. Ann Surg Oncol 22:2663–2668
Moon HG, Ju YT, Jeong CY et al (2008) Visceral obesity may affect oncologic outcome in patients with colorectal cancer. Ann Surg Oncol 15:1918–1922
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Tokunaga, R., Sakamoto, Y., Nakagawa, S. et al. Comparison of systemic inflammatory and nutritional scores in colorectal cancer patients who underwent potentially curative resection . Int J Clin Oncol 22, 740–748 (2017). https://doi.org/10.1007/s10147-017-1102-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-017-1102-5