Abstract
Objective
The aim of this study was to examine the prognostic significance of preoperative inflammatory-based indices, platelet–lymphocyte ratio (PLR), neutrophil–lymphocyte ratio (NLR), and carcinoembryonic antigen (CEA) in predicting overall survival (OS) in patients with colorectal peritoneal carcinomatosis (CPC) treated with cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC).
Methods
Sixty patients with pathologically confirmed CPC treated with CRS and HIPEC between 2003 and 2015 were included. Levels of preoperative PLR, NLR, and CEA were recorded. Univariate and multivariate analyses were conducted to identify prognostic factors associated with OS.
Results
Median OS was 36 months (95% CI, 26.6–45.4) and 5-year OS was 40.5% (95% CI, 27.3–51.6%). Preoperative PLR (p = 0.034) and CEA (p = 0.036) were found to be significant prognostic markers of OS, whereas NLR did not affect OS. PLR remained significant on multivariate analysis (hazard ratio, 1.035; 95% CI, 1.027–1.043; p < 0.001).
Conclusion
Our study indicates that preoperative PLR may be used as a prognostic marker in CPC patients undergoing CRS and HIPEC and could be useful in the preoperative setting when selecting patients for surgery. The subset of patients with PLR > 300 have a median OS of 5 months (95% CI, 0–24.6 months), indicating that CRS and HIPEC may not be superior to systemic chemotherapy in this subset of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The peritoneum is the second most common site of metastasis from colorectal cancer, after the liver [1, 2]. There have been significant advances in overall survival (OS) for metastatic colorectal cancer with liver and lung metastases, in light of modern chemotherapy and usage of targeted agents [3]. However, patients with colorectal peritoneal carcinomatosis (CPC) treated with systemic chemotherapy continue to have poor survival outcomes [4, 5]. CPC is ideally considered a regional rather than a systemic disease, which explains the rationale for regional therapy with optimal cytoreductive surgery (CRS) and instillation of hyperthermic intraperitoneal chemotherapy (HIPEC) [5].
The randomized controlled trial comparing CRS and HIPEC with systemic chemotherapy (fluorouracil-leucovorin), with or without palliative surgery, reported significant increase in survival with CRS and HIPEC, with median overall survival ranging from 22.3 months in the former to 12.6 months in the latter [6]. The benefits of CRS and HIPEC may be questioned now that oxaliplatin, irinotecan, and molecular agents are available. However, Franko et al. demonstrated that when modern systemic chemotherapy was combined with CRS/HIPEC, the median survival was improved (34.7 vs. 16.8 months; p < 0.001) [7]. The authors concluded that (1) contemporary chemotherapy was associated with prolonged survival among patients with carcinomatosis as compared with historical controls, and (2) addition of CRS and HIPEC to modern chemotherapy regimens may significantly prolong survival. CRS and HIPEC, however, are associated with high morbidity and mortality, i.e., 16–64% and 0–8%, respectively [8, 9], which underscores the importance of identifying preoperative prognostic factors that can be used in selecting patients for optimal benefit.
Many clinicopathological variables have been investigated as prognostic markers for overall survival (OS). Well-established factors include number of lymph node metastases at the time of CRS/HIPEC [10, 11], Eastern Cooperative Oncology Group (ECOG) score [10], tumor histology [10], grade of tumor differentiation [10], completeness of cytoreduction (CC) score [12], peritoneal cancer index (PCI) [12, 13], and angiogenesis-related markers [14, 15], such as vascular endothelial growth factor. The main drawback of these markers is that they can only be determined intraoperatively or postoperatively, negating their relevance in selecting patients for the procedure. One feared scenario encountered during laparotomy for planned CRS and HIPEC is “open-and-close” surgery when surgeons find the tumor too extensive and unresectable. Consequently, there is a need for preoperative parameters that can aid with selecting patients who will benefit from CRS and HIPEC.
The inflammatory-based markers platelet–lymphocyte ratio (PLR) and neutrophil–lymphocyte ratio (NLR) are affordable and easily obtained in the preoperative setting in most hospital laboratories. Previous studies have evaluated their use in various groups of oncological patients, including colorectal cancer patients. However, these studies have focused on their prognostic significance in colorectal cancer patients with local disease [16–20] or nonperitoneal metastasis [21]. To our knowledge, no study reported in the literature has evaluated the use of PLR and NLR as candidate prognostic factors in CPC patients undergoing CRS and HIPEC. The current study aimed to delineate the ability of PLR and NLR to prognosticate OS for these patients.
Methods
The study was carried out with the approval of the Singhealth Centralized Institutional Review Board. Retrospective analysis of a prospectively maintained database of consecutive patients who underwent CRS and HIPEC in a single institution was performed. All CPC patients who underwent CRS and HIPEC between February 2003 and October 2015 were included. Appendiceal cancers were not included.
CRS and HIPEC
CRS and HIPEC were performed as described by Sugarbaker [22]. The goal of CRS is to remove all visible tumor by diaphragmatic, parietal, and pelvic peritonectomy with greater and lesser omentectomy. Resection of viscera, for example, gastrectomy, colectomy, splenectomy, cholecystectomy, and hysterectomy with or without salpingooophrectomy, is performed if necessary to achieve a complete cytoreduction.
HIPEC was conducted with a closed-abdomen technique that utilized an extracorporeal device for intraperitoneal administration of heated (41–42 °C) chemotherapy for 60 min. The chemotherapy regimen used for the CPC patients was mitomycin-C at 10 mg/body surface area (m2).
Peritoneal cancer index
The peritoneal cancer index (PCI) reflects the extent of intraperitoneal tumor determined at the time of surgical exploration of the abdomen and pelvis (Fig. 1) [23]. The PCI is a combined numerical score of tumor distribution throughout 13 abdominopelvic regions and lesion size. It serves as an estimate of probability of complete cytoreduction and has been found to predict survival in CPC patients undergoing CRS and HIPEC [23].
Peritoneal cancer index (PCI) score. (From [51])
Completeness of cytoreduction score
Residual disease after CRS is classified by the completeness of cytoreduction (CC) score [23]: CC-0 indicates no visible residual tumor, CC-1 indicates residual tumor nodules ≤2.5 mm, CC-2 indicates residual tumor nodules between 2.5 mm and 2.5 cm, and CC-3 indicate residual tumor nodules >2.5 cm. Complete (CC-0 or CC-1) or incomplete (CC-2 or CC-3) cytoreduction is typically recorded by this score.
Study parameters
The PLR and NLR were retrospectively calculated for all patients from neutrophil, lymphocyte, and platelet counts obtained within 1 week before surgery. NLR was defined as the absolute neutrophil count divided by the absolute lymphocyte count; similarly, PLR was defined as the absolute platelet count divided by the absolute lymphocyte count. Carcinoembryonic antigen (CEA) level was similarly documented preoperatively for all patients.
Previous studies have dichotomized patients based on NLR values of <5 and ≥5 [19–21]. We defined the ideal NLR cutoff value for use as a predictor of OS by constructing a receiver-operating characteristics (ROC) curve; the area under the ROC curve was 0.756. The sensitivity and the specificity of each NLR value were determined, and the value of 4.95 gave the combined highest sensitivity and specificity. A modified ROC curve was generated that indicated that the ideal cutoff NLR value to predict disease recurrence was 4.95 (Fig. 2), congruent with the cutoff value of 5 used in previous studies. The PLR was classified into three groups (<150, 150–300, >300) as per previous validated cutoff values [24].
Statistical analysis
The associations between PLR, NLR, CEA, and clinicopathological variables were assessed via Fisher’s exact test. OS was calculated from the date of CRS and HIPEC to date of death or the date of last follow-up, whichever came first. Postoperative deaths were not excluded from the survival analysis. Survival analysis was performed using the Kaplan–Meier method and compared using the log-rank test. To identify independent factors related significantly to patient prognosis, Cox’s proportional hazard analysis with a stepwise procedure was used.
All tests were two sided, and p values <0.05 were considered statistically significant. Analyses were conducted using SPSS version 14.0 (SPSS, Chicago, IL, USA).
Results
Sixty CPC patients underwent CRS and HIPEC between February 2003 and October 2015.
Patient characteristics
Patient characteristics are listed in Table 1. The median age of patients was 56 years; there were 22 (36.1%) male patients and 38 (63.9%) female patients. The primary tumor histology was adenocarcinoma (66.7%), followed by mucinous carcinoma (30.0%) and signet-ring carcinoma (3.3%).
Treatment
Of the 60 patients, 52 (86.7%) achieved a CC-0 and 8 (13.3%) had a CC-1. During CRS, the median number of visceral resections was 2 ± 1.2 (range, 0–5). The median operative time was 462 min (range, 200–960 min). A median of 2 units (range, 0–9) of packed cells was transfused intraoperatively.
Inflammatory markers and CEA
The median (SD, range) of NLR, PLR, and CEA were 2.28 (3.23, 22.5), 148 (80.1, 402), and 5.9 (108, 500.5), respectively.
Overall survival
On univariate analyses, CEA (p = 0.036) and PLR (p = 0.034) were found to have significant prognostic impact on OS (Table 2).
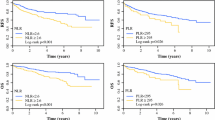
Patients with PLR > 300 had significantly poorer 5-year OS (19%; 95% CI, 0–45.0%) compared to patients with a PLR of 151–300 (32.1%; 95% CI, 4.86–59.3%) or a PLR < 150 (38.6%; 95% CI, 8.03–69.1%) (p = 0.034) (Fig. 3).
An elevated CEA level was also found to have a significant impact on OS on univariate analysis. Patients with CEA ≥ 5 had a significantly poorer 5-year OS (18%; 95% CI, 0–46.8%) as compared to patients with CEA < 5 (31.4%; 95% CI, 0–65.8%) (Fig. 4).
The median OS for patients with PLR > 300, PLR = 151–300, and PLR < 150 were 5 months (95% CI, 0–24.6 months), 36 months (95% CI, 15.8–56.2 months), and 47 months (95% CI, 25.5–68.5 months), respectively. The median OS for patients with CEA < 5 was 37 months (95% CI, 33.6–40.4 months) and that of CEA ≥ 5 was 29 months (95% CI, 16.4–41.6 months).
Multivariate analysis with Cox regression modeling was performed to identify independent prognostic factors of overall survival (Table 3). Only PLR remained an independent prognostic marker (HR 1.035; p < 0.001).
Discussion
CPC has traditionally been regarded as distant metastases, portending a terminal state of colorectal cancer for which only palliative surgery or systemic chemotherapy was recommended. The development of CRS and HIPEC has changed the course of the condition, with reported median survival ranging from 13 to 63 months [25–29]. In this study, the median OS was 36 months (95% CI, 26.6–45.4) with 5-year overall survival of 40.5% (27.3–51.6%). Our 60-day postoperative mortality (0%) and morbidity (17.5%) were low and comparable to those from other institutions [12].
Several scoring systems are available for prognosticating CPC patients undergoing CRS and HIPEC, including scores reflecting extent of disease (PCI [30], peritoneal surface disease severity score (PSDSS) [31], Verwaal’s N score [29], Gilly score [32]), or degree of cytoreduction (CC score) [25]. In a paper recently published by our group, we reported that PCI scoring remained a better prognostic tool when compared to the PSDSS score in our patients [33]. However, these scores all require intra- or postoperative findings, negating their use as preoperative selection tools to identify patients who will benefit from CRS and HIPEC. Furthermore, well-established clinical factors, i.e., TNM staging, appear to be insufficiently discriminatory for selecting patients for CRS and HIPEC.
The combined index of platelets and lymphocytes (PLR) has been investigated as a prognostic marker in various cancers. A meta-analysis that included 12,754 patients investigated the relationship of PLR and overall survival in solid tumors, concluding that PLR was independently associated with OS in various solid tumors [34]. In colorectal cancer patients, NLR was validated as an independent predictor in metastatic colorectal cancer [35], whereas PLR was identified as an independent risk factor for resectable colorectal cancer [36, 37]. These inflammatory-based indices, however, have not been investigated in colorectal peritoneal carcinomatosis patients.
There have been several postulations behind the mechanisms for the establishment and progression of CPC. Through spontaneous or iatrogenic causes, loose cancer cells from the primary mass penetrate the colorectal wall, which is facilitated by downregulation of cell–cell adhesion molecules such as E-cadherin [38–40]. Once in the abdominal cavity, the cancer cells are transported to various anatomical regions by the forces of gravity, peristalsis, or negative pressure generated by diaphragmatic movement [41]. In establishing peritoneal carcinomatosis, inflammation has a key function by enhancing the expression of adhesion molecules including vascular cell adhesion molecule 1 [VCAM-1 (CD106)], intercellular adhesion molecule 1 [ICAM-1 (CD54)], and platelet endothelial cell adhesion molecule [PECAM-1 (CD31)] to allow the free-floating cancer cells to adhere to the peritoneum [42, 43]. Therefore, the association between a relative thrombocytosis and adverse OS in PC patients might be explained on the basis that the platelet count reflects an additional index of systemic inflammation that enhances peritoneal adhesion of cancer cells and, consequently, the extent of peritoneal carcinomatosis.
In predicting 5-year OS, PLR and CEA were found to be significant prognosticators on univariate analysis. However, on multivariate analysis, only PLR retained its significance. NLR was not found to be significant on either univariate or multivariate analysis. Increasing evidence has suggested platelets facilitate multiple steps of tumor development and progression by promoting tumor cell proliferation, angiogenesis, and metastasis. Platelets have been shown in vitro to inhibit apoptosis and reverse cell-cycle arrest caused by chemotherapy regimens such as 5-fluorouracil and paclitaxel and to enhance DNA repair in cancer cells [44]. In addition, platelets contain many pro-angiogenic factors that initiate tumor angiogenesis [45] and have been associated with tumor metastasis [46, 47]; the underlying mechanism is thought to be protection of circulating tumor cells against immune surveillance by attenuation of natural killer cells [48]. Tumor cells also induce release of vascular endothelial growth factor from platelets [45]. Similar to platelets, lymphocytes are associated with immune surveillance, which explains why high lymphocytic count translates to better survival [49] whereas low counts are related to poor tumor prognoses [50].
NLR and PLR are easily obtained from full blood counts routinely ordered preoperatively. Such markers, if proven to have prognostic significance, could potentially allow for improved patient selection for CRS and HIPEC.
As demonstrated in this article, patients with PLR > 300 have a median OS of 5 months (95% CI, 0–24.6 months), indicating that CRS and HIPEC may not be superior to systemic chemotherapy in this subset of patients. On the other hand, the median OS of patients with PLR 150–300 and PLR < 150 were 36 months (95% CI, 15.8–56.2 months) and 47 months (95% CI, 25.5–68.5 months), respectively. This finding implies that PLR > 300 may be used as a tool to define a subset of patients wherein CRS and HIPEC might be contraindicated.
There are several limitations to this study. As a retrospective review, there are inherent biases associated with the data, including missing data, which might have reduced the power of our study. In addition, as this is a single-center review, the characteristics of our patient population may not make our findings applicable to other populations. Also, the sample size is relatively small. In spite of these limitations, we believe that this study convincingly demonstrates the prognostic influence of PLR in predicting overall survival in colorectal patients with peritoneal metastases undergoing CRS and HIPEC and, at present, remains the only additional tool apart from clinical and radiologic factors to aid in the preoperative selection of patients for this procedure.
Conclusion
Preoperative PLR is an independent prognostic marker for OS in colorectal peritoneal carcinomatosis patients undergoing CRS and HIPEC and may be used when selecting patients for the procedure. We hope to be able to verify this prospectively in a larger cohort of patients.
References
Lemmens V et al (2010) Predictors and survival of synchronous peritoneal carcinomatosis of colorectal origin: a population-based study. Int J Cancer 128:2717–2725
Segelman J et al (2012) Incidence, prevalence and risk factors for peritoneal carcinomatosis from colorectal cancer. Br J Surg 99:699–705
Chua T, Liauw W, Chu F, Morris D (2012) Viewing metastatic colorectal cancer as a curable chronic disease. Am J Clin Oncol 35:77–80
Klaver Y et al (2012) Outcomes of colorectal cancer patients with peritoneal carcinomatosis treated with chemotherapy with and without targeted therapy. Eur J Surg Oncol (EJSO) 38:617–623
Franko J et al (2011) Treatment of colorectal peritoneal carcinomatosis with systemic chemotherapy: a pooled analysis of north central cancer treatment group phase III trials N9741 and N9841. J Clin Oncol 30:263–267
Verwaal V (2003) Randomized trial of cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis of colorectal cancer. J Clin Oncol 21:3737–3743
Franko J, Ibrahim Z, Gusani N et al (2010) Cytoreductive surgery and hyperthermic intraperitoneal chemoperfusion versus systemic chemotherapy alone for colorectal peritoneal carcinomatosis. Cancer (Phila) 116(16):3756–3762
Randle R et al (2014) Peritoneal surface disease with synchronous hepatic involvement treated with cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC). Ann Surg Oncol 22:1634–1638
Saxena A, Yan T, Morris D (2009) A critical evaluation of risk factors for complications after cytoreductive surgery and perioperative intraperitoneal chemotherapy for colorectal peritoneal carcinomatosis. World J Surg 34:70–78
Kwakman R, Schrama A, van Olmen J et al (2016) Clinicopathological parameters in patient selection for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for colorectal cancer metastases. Ann Surg 263(6):1102–1111. doi:10.1097/sla.0000000000001593
Baumgartner J et al (2014) Predictors of progression in high-grade appendiceal or colorectal peritoneal carcinomatosis after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol 22:1716–1721
Elias D, Gilly F, Boutitie F et al (2010) Peritoneal colorectal carcinomatosis treated with surgery and perioperative intraperitoneal chemotherapy: retrospective analysis of 523 patients from a multicentric French study. J Clin Oncol 28(1):63–68. doi:10.1200/jco.2009.23.9285
Nikolic S et al (2014) Survival prognostic factors in patients with colorectal peritoneal carcinomatosis treated with cytoreductive surgery and intraoperative hyperthermic intraperitoneal chemotherapy: a single institution experience. Eur J Surg Oncol (EJSO) 40:S163
Sluiter NR, de Cuba EMS, Kwakman R, et al (2016) Versican and vascular endothelial growth factor expression levels in peritoneal metastases from colorectal cancer are associated with survival after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Clin Exp Metastasis 33:297–307
de Cuba E, de Hingh IHJT, Sluiter NR, et al (2016) Angiogenesis-related markers and prognosis after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for metastatic colorectal cancer. Ann Surg Oncol 23:1601–1608
Szkandera J, Pichler M, Absenger G et al (2014) The elevated preoperative platelet to lymphocyte ratio predicts decreased time to recurrence in colon cancer patients. Am J Surg 208(2):210–214
Choi W, Cleghorn M, Jiang H et al (2015) Preoperative neutrophil-to-lymphocyte ratio is a better prognostic serum biomarker than platelet-to-lymphocyte ratio in patients undergoing resection for nonmetastatic colorectal cancer. Ann Surg Oncol 22(S3):603–613
Roxburgh C, McMillan D (2010) Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol 6(1):149–163
Ding P, An X, Zhang R et al (2010) Elevated preoperative neutrophil to lymphocyte ratio predicts risk of recurrence following curative resection for stage IIA colon cancer. Int J Colorectal Dis 25(12):1427–1433
Mallappa S, Sinha A, Gupta S et al (2011) Pre-operative neutrophil lymphocyte ratio greater than 5 is a prognostic factor for recurrent colorectal cancer. Int J Surg 9(7):495
He W, Yin C, Guo G et al (2011) Initial neutrophil lymphocyte ratio is superior to platelet lymphocyte ratio as an adverse prognostic and predictive factor in metastatic colorectal cancer. Med Oncol 30(1)
Sugarbaker P (1995) Peritonectomy procedures. Ann Surg 221:29–42
Jacquet P, Sugarbaker P (1996) Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. Cancer Treat Res 82:359–374
Zhou X et al (2014) Prognostic value of PLR in various cancers: a meta-analysis. PLoS One 9:e101119
Glehen O et al (2004) Intraperitoneal chemohyperthermia and attempted cytoreductive surgery in patients with peritoneal carcinomatosis of colorectal origin. Br J Surg 91:747–754
Glehen O (2004) Cytoreductive surgery combined with perioperative intraperitoneal chemotherapy for the management of peritoneal carcinomatosis from colorectal cancer: a multi-institutional study. J Clin Oncol 22:3284–3292
Shen P et al (2004) Cytoreductive surgery and intraperitoneal hyperthermic chemotherapy with mitomycin C for peritoneal carcinomatosis from nonappendiceal colorectal carcinoma. Ann Surg Oncol 11:178–186
Royal R, Pingpank J (2008) Diagnosis and management of peritoneal carcinomatosis arising from adenocarcinoma of the colon and rectum. Semin Oncol 35:183–191
Verwaal V, van Tinteren H, van Ruth S, Zoetmulder F (2004) Predicting the survival of patients with peritoneal carcinomatosis of colorectal origin treated by aggressive cytoreduction and hyperthermic intraperitoneal chemotherapy. Br J Surg 91:739–746
Jacquet P, Sugarbaker PH (1996) Current methodologies for clinical assessment of patients with peritoneal carcinomatosis. J Exp Clin Cancer Res. 15:49–58
Pelz J, Stojadinovic A, Nissan A, Hohenberger W, Esquivel J (2009) Evaluation of a peritoneal surface disease severity score in patients with colon cancer with peritoneal carcinomatosis. J Surg Oncol 99:9–15
Gilly F, Carry P, Sayag A, Brachet A (1994) Regional chemotherapy (with mitomycin C) and intra-operative hyperthermia for digestive cancers with peritoneal carcinomatosis. Hepatogastroenterology 41:124–129
Ng J, Ong W, Chia C et al (2016) Prognostic relevance of the peritoneal surface disease severity score compared to the peritoneal cancer index for colorectal peritoneal carcinomatosis. Int J Surg Oncol (article ID 24951311–7)
Templeton A, Ace O, McNamara M et al (2014) Prognostic role of platelet to lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Cancer Epidemiol Biomark Prev 23(7):1204–1212
He W, Yin C, Guo G et al (2013) Initial neutrophil lymphocyte ratio is superior to platelet lymphocyte ratio as an adverse prognostic and predictive factor in metastatic colorectal cancer. Med Oncol 30(1):439
Szkandera J et al (2014) The elevated preoperative platelet to lymphocyte ratio predicts decreased time to recurrence in colon cancer patients. Am J Surg 208:210–214
Kwon H, Kim S, Oh S et al (2012) Clinical significance of preoperative neutrophil-lymphocyte versus platelet-lymphocyte ratio in patients with operable colorectal cancer. Biomarkers 17(3):216–222
Terauchi M, Kajiyama H, Yamashita M, Kato M et al (2007) Possible involvement of TWIST in enhanced peritoneal metastasis of epithelial ovarian carcinoma. Clin Exp Metastasis 24(5):329–339
Kokenyesi R, Murray K, Benshushan A et al (2003) Invasion of interstitial matrix by a novel cell line from primary peritoneal carcinosarcoma, and by established ovarian carcinoma cell lines: role of cells’ matrix adhesion molecules, proteinases, and E-cadherin expression. Gynecol Oncol 89(1):60–72
Pocard M, Debruyne P, Bras-Gonasalves R et al (2001) Single alteration of p53 or E-cadherin genes can alter the surgical resection benefit in an experimental model of colon cancer. Dis Colon Rectum 44(8):1106–1112
Meyers M (1973) Distribution of intra-abdominal malignant seeding: dependency of dynamics of flow of ascitic fluid. Invest Radiol 8(4):289
Jonjic N (1992) Expression of adhesion molecules and chemotactic cytokines in cultured human mesothelial cells. J Exp Med 176(4):1165–1174
Bittinger F, Klein C, Skarke C et al (1996) PECAM-1 expression in human mesothelial cells: an in vitro study. Pathobiology 64(6):320–327
Radziwon-Balicka A, Medina C, O’Driscoll L et al (2012) Platelets increase survival of adenocarcinoma cells challenged with anticancer drugs: mechanisms and implications for chemoresistance. Br J Pharmacol 167(4):787–804
Battinelli E, Markens B, Italiano J (2011) Release of angiogenesis regulatory proteins from platelet alpha granules: modulation of physiologic and pathologic angiogenesis. Blood 118(5):1359–1369
Gay L, Felding-Habermann B (2011) Contribution of platelets to tumour metastasis. Nat Rev Cancer 11(2):123–134
Gasic G, Gasic T, Stewart C (1968) Antimetastatic effects associated with platelet reduction. Proc Natl Acad Sci USA 61(1):46–52
Nieswandt B, Hafner M, Echtenacher B et al (1999) Lysis of tumor cells by natural killer cells in mice is impeded by platelets. Cancer Res 59(6):1295–1300
Seo A, Lee H, Kim E et al (2013) Tumour-infiltrating CD8+ lymphocytes as an independent predictive factor for pathological complete response to primary systemic therapy in breast cancer. Br J Cancer 109(10):2705–2713
Fogar P, Sperti C, Basso D et al (2006) Decreased total lymphocyte counts in pancreatic cancer: an index of adverse outcome. Pancreas 32(1):22–28
Esquivel J, Sugarbaker PH (1998) Elective surgery in recurrent colon cancer with peritoneal seeding: when to and when not to proceed. Cancer Ther 1:321–325
Acknowledgements
We thank Mr. Mrinal Kumar for helping in statistical analysis, and Ms. Thakshayeni Skanthakumar and Ms. Tuty Muliana Bte Ismail for assisting with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest or financial ties to disclose.
About this article
Cite this article
Bong, T.S.H., Tan, G.H.C., Chia, C. et al. Preoperative platelet–lymphocyte ratio is an independent prognostic marker and superior to carcinoembryonic antigen in colorectal peritoneal carcinomatosis patients undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Int J Clin Oncol 22, 511–518 (2017). https://doi.org/10.1007/s10147-017-1092-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-017-1092-3