Abstract
Background
The neutrophil-to-lymphocyte ratio (NLR) is associated with clinical outcomes of various cancers. This study aimed to evaluate whether pretreatment NLR can be used as a prognostic factor in patients with metastatic renal cell carcinoma (mRCC) receiving targeted therapy.
Methods
In this single-center retrospective study, the Kaplan–Meier method was used to estimate progression-free survival (PFS) and overall survival (OS) of 373 mRCC patients receiving targeted therapy. The survival outcomes of patients with high (≥2.2) and low (<2.2) pretreatment NLRs were compared by log-rank test, and Cox proportional hazard regression model was used to compare OS and PFS between groups.
Results
The overall median PFS and OS times for all 373 patients were 18.4 and 34.3 months, respectively. Patients with high NLRs had significantly shorter median OS (28.8 vs 410 months, P = 0.005) and PFS (15.4 vs 23.9 months, P = 0.001) than those with low NLRs. After adjusting for confounding variables, each unit increase of NLR was associated with a 40 % increase in mortality (hazard ratio [HR] 1.391; 95 % confidence interval [CI] 1.022–1.894; P = 0.036). High NLR was also an independent predictor of poor PFS (HR 1.544; 95 % CI 1.166–2.045; P = 0.002).
Conclusion
Pretreatment NLR may be an independent prognostic factor for mRCC patients who are receiving targeted therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 30 % of patients with renal cell carcinoma (RCC) have metastatic disease on initial diagnosis [1], and ~20 % of patients with localized RCC relapse with metastasis following surgery [2]. The availability of targeted agents has revolutionized treatment of metastatic RCC (mRCC) and has resulted in a dramatic improvement in prognosis. The identification of novel prognostic markers would facilitate assessment of individual risk and assist clinical decision-making. However, clinical and investigational models that have been shown to accurately predict clinical outcomes of mRCC patients receiving targeted therapy are still lacking.
The association between inflammation and the initiation and development of cancer [3], has led to increased interest in the prognostic value of proinflammatory factors. For example, recent studies have found that C-reactive protein was associated with survival in hepatocellular carcinoma and mRCC treated with sunitinib [4, 5], and with serum albumin in glioblastoma patients [6]. Ito et al. observed that pretreatment C-reactive protein could provide useful prognostic information to help to identify advanced mRCC patients who are most likely to benefit from initial nephrectomy [7]. Additionally, changes in the number of circulating inflammatory cells, such as the lymphocyte-to-monocyte ratio in B-cell lymphoma [8] and the neutrophil-to-lymphocyte ratio (NLR) in RCC, [9] have prognostic value. Despite this evidence, little is known about the predictive value of such variations in mRCC patients receiving targeted therapy. Park et al. reported that an increase in NLR following treatment was an independent predictor of poor prognosis in mRCC patients receiving sunitinib as first-line therapy [10]. Other investigators reported an inverse correlation between increased pretreatment NLR and prognosis in mRCC patients treated with tyrosine kinase inhibitors [11]. Given the relative lack of data and inconsistency of the existing information, we evaluated the prognostic significance of NLR in Chinese mRCC patients, and aimed to provide additional data on the predictive role of NLR in mRCC patients receiving targeted therapy. To the best of our knowledge, this is the first study of its kind in Chinese mRCC patients.
Patients and methods
Study subjects
This retrospective study enrolled 373 consecutive patients with pathologically confirmed mRCC at the Department of Urology of Fudan University Shanghai Cancer Center (FUSCC) between December, 2006 and May, 2014. The Institutional Research Review Board of FUSCC approved the study protocol, and each participant gave written informed consent before inclusion. Patient age, sex, body mass index (BMI), history of cytokine therapy, Eastern Cooperative Oncology Group (ECOG) performance status, International Metastatic Renal Cell Carcinoma Database Consortium prognostic model (IMDC) scores [12], and pathological information were retrieved from our medical records database. Peripheral blood cell counts were performed 1–7 days before the start of targeted therapy.
The first-line targeted agents administered to patients were sorafenib (400 mg, b.i.d.) and sunitinib (50 mg/day, 4 weeks on and 2 weeks off). These agents have been approved by the China Food and Drug Administration for routine treatment of mRCC patients. All patients were advised to visit the doctor for disease assessment every 3 months after the start of treatment, or at any time they experienced discomfort. Drug dosages were reduced in the presence of grade 3–4 adverse effects that reduced a patient’s tolerance. If first-line therapy failed, then another first-line drug, or second-line targeted agent, including axitinib, famitinib or everolimus, was used.
Progression-free survival (PFS) and overall survival (OS) were chosen as efficacy endpoints. PFS was defined as the time between the start of targeted therapy and radiological evidence of disease progression (or death if it occurred before progression). OS was defined as the time between the start of targeted therapy and either death or the date of the last follow-up visit. The NLR was the absolute neutrophil count divided by absolute lymphocyte count recorded as cells × 109 L−1. We used a median NLR value of 2.2 as a cut-off to stratify patients into high NLR (≥2.2) and low NLR (<2.2) groups.
Statistical methods
Continuous variables were reported as medians, and nonparametric Kruskal tests were used to determine the significance of differences. Pearson’s chi-squared tests were used to determine the significance of differences of categorical variables that were expressed as frequencies and percentages. OS and PFS curves were calculated using the Kaplan–Meier method and compared by the log-rank test. We used a Cox proportional hazard regression model to evaluate the relationship between OS and PFS with independent clinical variables, including age, sex, BMI, ECOG score, IMDC, history of cytokine treatment, pathology, Fuhrman grade and NLR. All statistical tests were two-sided, and P values of <0.05 were considered statistically significant. All analyses were performed using STATA software version 12.1 (StataCorp; College Station, TX, USA).
Results
We enrolled 373 mRCC patients (278 male, 95 female) with a median age of 58 years (range 17–90 years). Pathological diagnosis was by renal biopsy in 57 patients, and by surgical excision in 316 patients. On pathological evaluation, there were 317 patients with clear cell RCC (ccRCC) and 56 with non-clear cell RCC (nccRCC), including 29 with papillary RCC, seven with collecting duct RCC, and six with chromophobe RCC. There were three patients with medullary carcinoma, three with Xp11.2 translocation RCC, and eight with unclassified renal cancers. The first-line targeted agents were sorafenib in 217 patients and sunitinib in 156 patients.
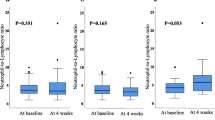
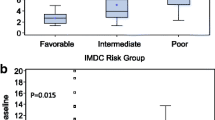
Median (range) peripheral blood cell counts were 6.0 × 109 L−1 (3.1–13 × 109 L−1) for white blood cells, 3.6 × 109 L−1 (1.3–10.2 × 109 L−1) for neutrophils, and 1.7 × 109 L−1 (0.5–4.3 × 109 L−1) for lymphocytes. The demographic and clinical characteristics of the study patients are shown in Table 1. There were no significant differences in age, BMI, ECOG score, IMDC, pathology (ccRCC vs nccRCC), and first-line targeted agents of the high (≥2.2) and low NLR (<2.2) groups. There were more males in the high NLR group than in the low NLR group. Fewer patients in the high NLR group had a history of cytokine treatment than in the low NLR group.
Kaplan–Meier curves of OS and PFS are shown in Fig. 1. The overall median PFS of all 373 patients was 18.4 months, and the median OS was 34.3 months. In the high NLR group, median OS (28.8 months) and PFS (15.4 months) were significantly shorter than in the low NLR group (OS 41.0 months, P = 0.005; PFS 23.9 months, P = 0.001).
The effect of NLR on PFS and OS was determined using a Cox proportional hazard regression model (Table 2). After adjusting for confounding variables, each unit increase of the NLR was associated with a 40 % increase in mortality (hazard ratio [HR] 1.391; 95 % confidence interval [CI] 1.022–1.894; P = 0.036). A high NLR was also an independent predictor of poor PFS (HR 1.544; 95 % CI 1.166–2.045; P = 0.002).
Discussion
In this retrospective study conducted in Eastern China, we revealed a favorable prognosis in mRCC patients with a low NLR who received targeted therapy. Patients with a low pretreatment NLR (<2.2) had significantly longer median OS and PFS than those with a high NLR (≥2.2). Controlling for other clinical and demographic variables that might have affected survival, a high NLR was found to be an independent predictor of poor prognosis in mRCC patients receiving targeted therapy.
The interaction between inflammation and tumor growth has been extensively studied, and the evidence shows that inflammation is associated with all stages of carcinogenesis and is involved through a number of mechanisms [13]. Host inflammatory responses, to a certain extent, reflect microenvironments that can either promote or inhibit tumor development and influence subsequent oncological outcomes. However, the steps by which these interactions between targeted cells and the immune system proceed have yet to be discovered. NLR is an important host inflammatory marker that has been linked to poor prognosis in various cancers [14–16]. The data on the role of NLR in mRCC patients receiving targeted therapy are inconsistent, but Keizman et al. [17] found that NLR ≤3 was an independent predictive factor of increased PFS (HR 0.285) and OS (HR 0.3) in mRCC patients treated with sunitinib. Another study group found that mRCC patients receiving sunitinib with pretreatment NLR ≤2.5 indicated longer cancer-specific survival; however, after adjustment for confounding factors, low NLR did not harbor independent significance. Conversely, post-treatment NLR was significantly associated with favorable prognosis by both univariate and multivariate analysis [10]. NLR was also observed to be an independent prognostic factor in a group of mRCC patients who failed initial therapy with one or two targeted agents and were given everolimus as a second- or third-line targeted agent [18].
In addition, Heng et al. observed that absolute neutrophils greater than the upper limit of normal was an independent adverse prognostic factor in mRCC patients treated with targeted therapy [19]. We also evaluated the prognostic role of absolute neutrophils in our group of patients. The results indicated that there was no difference between the high NLR group and low NLR group in both median OS and PFS (data not shown). We found that only a pretreatment NLR of <2.2 was associated with longer PFS and OS in our group of Chinese mRCC patients given targeted therapy. Our results may have differed from those reported by others because of differences in study design, patient populations and ethnicity, therapeutic regimen, or NLR cut-off. It is well known that targeted therapy has different effects in patients of different ethnic and genetic backgrounds [20, 21]. Compared with patients in Western countries, Chinese mRCC patients given targeted agents seem to have a better prognosis [22]. This might reflect differences in immune cell activity and tumor cell response to targeted therapy. Furthermore, several NLR cut-offs have been used to stratify study groups in various investigations because, to date, there has been no agreed standard cut-off that can be used in similar studies. Therefore, further validation of the NLR as a prognostic marker depends on further studies being conducted using large patient samples, different ethnicities, and unified standards. The underlying mechanisms by which NLR affects RCC response to targeted therapy remains to be elucidated.
In addition to their well-known function in host immunity, peripheral leukocytes greatly affect tumor initiation and progression. Neutrophil activation and migration to tumor tissues can occur in response to increasing tumor burden or aggressive tumor metabolism. Neutrophils that infiltrate tumors produce a variety of bioactive molecules, such as reactive oxygen species and vascular endothelial growth factor, which can stimulate tumor cell proliferation and angiogenesis [23, 24]. Conversely, lymphocytes are thought to confer an antitumor effect by inducing cell apoptosis, suppressing tumor growth and migration and by mediating antibody-dependent cell-mediated cytotoxicity [25, 26]. Hence, neutrophilia may be a marker of overproduction of cytokines associated with tumor-related inflammation, and higher lymphocyte levels might reflect the strength of the antitumor immune response. A combination of neutrophils and lymphocytes, as denoted by the NLR, may thus reflect the balance between tumor-inhibiting and tumor-promoting immune system activities. Consequently, it might serve as a convenient, useful monitor in risk stratification and cancer follow-up.
There are several limitations to our study. First, this was a retrospective study carrying an intrinsic selection bias. Second, patients who failed first-line targeted therapy were switched to different first- or second-line therapeutic strategies. Third, patients with tumors of different histopathological types were included, and not all Fuhrman grades were represented in our study. All these confounding factors may affect the results. Fourth, additional potential prognostic factors, such as history of cytoreductive nephrectomy and C-reactive protein levels, were not included in our analyses. In addition, the NLR differs among individuals owing to the influence of concurrent infection or drugs, which were also not accounted for in the results.
In conclusion, increased pretreatment NLR was associated with shorter PFS and OS in mRCC patients receiving targeted therapy. The results warrant further validation of the NLR as a cost-effective easily measured marker with possible prognostic value in mRCC.
References
Gupta K, Miller JD, Li JZ et al (2008) Epidemiologic and socioeconomic burden of metastatic renal cell carcinoma (mRCC): a literature review. Cancer Treat Rev 34:193–205
Athar U, Gentile TC (2008) Treatment options for metastatic renal cell carcinoma: a review. Can J Urol 15:3954–3966
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674
Shin JH, Kim CJ, Jeon EJ et al (2015) Overexpression of C-reactive protein as a poor prognostic marker of resectable hepatocellular carcinomas. J Pathol Transl Med 49:105–111
Beuselinck B, Vano YA, Oudard S et al (2014) Prognostic impact of baseline serum C-reactive protein in patients with metastatic renal cell carcinoma (RCC) treated with sunitinib. BJU Int 114:81–89
Han S, Huang Y, Li Z et al (2015) The prognostic role of preoperative serum albumin levels in glioblastoma patients. BMC Cancer 15:108
Ito H, Shioi K, Murakami T et al (2012) C-reactive protein in patients with advanced metastatic renal cell carcinoma: usefulness in identifying patients most likely to benefit from initial nephrectomy. BMC Cancer 12:337
Wei X, Huang F, Wei Y et al (2014) Low lymphocyte-to-monocyte ratio predicts unfavorable prognosis in non-germinal center type diffuse large B-cell lymphoma. Leuk Res 38:694–698
Pichler M, Hutterer GC, Stoeckigt C et al (2013) Validation of the pre-treatment neutrophil–lymphocyte ratio as a prognostic factor in a large European cohort of renal cell carcinoma patients. Br J Cancer 108:901–907
Park YH, Ku JH, Kwak C et al (2014) Post-treatment neutrophil-to-lymphocyte ratio in predicting prognosis in patients with metastatic clear cell renal cell carcinoma receiving sunitinib as first line therapy. Springerplus 3:243
Gunduz S, Mutlu H, Uysal M et al (2014) Prognostic value of hematologic parameters in patients with metastatic renal cell carcinoma using tyrosine kinase inhibitors. Asian Pac J Cancer Prev 15:3801–3804
Heng DY, Xie W, Regan MM et al (2013) External validation and comparison with other models of the international metastatic renal-cell carcinoma database consortium prognostic model: a population-based study. Lancet Oncol 14:141–148
Vakkila J, Lotze MT (2004) Inflammation and necrosis promote tumour growth. Nat Rev Immunol 4:641–648
Kaynar M, Yildirim ME, Badem H et al (2014) Bladder cancer invasion predictability based on preoperative neutrophil–lymphocyte ratio. Tumour Biol 35:6601–6605
Dalpiaz O, Ehrlich GC, Mannweiler S et al (2014) Validation of pretreatment neutrophil–lymphocyte ratio as a prognostic factor in a European cohort of patients with upper tract urothelial carcinoma. BJU Int 114:334–339
Chen J, Hong D, Zhai Y et al (2015) Meta-analysis of associations between neutrophil-to-lymphocyte ratio and prognosis of gastric cancer. World J Surg Oncol 13:122
Keizman D, Ish-Shalom M, Huang P et al (2012) The association of pre-treatment neutrophil to lymphocyte ratio with response rate, progression free survival and overall survival of patients treated with sunitinib for metastatic renal cell carcinoma. Eur J Cancer 48:202–208
Santoni M, De Giorgi U, Iacovelli R et al (2013) Pre-treatment neutrophil-to-lymphocyte ratio may be associated with the outcome in patients treated with everolimus for metastatic renal cell carcinoma. Br J Cancer 109:1755–1759
Heng DY, Xie W, Regan MM et al (2009) Prognostic factors for overall survival in patients with metastatic renal cell carcinoma treated with vascular endothelial growth factor–targeted agents: results from a large, multicenter study. J Clin Oncol 27:5794–5799
Pensa M, Swede H, Brockmeyer JA et al (2009) Patterns of HER2 testing in the management of primary breast cancer. Cancer Epidemiol 33:113–117
Garcia-Donas J, Esteban E, Leandro-Garcia LJ et al (2011) Single nucleotide polymorphism associations with response and toxic effects in patients with advanced renal-cell carcinoma treated with first-line sunitinib: a multicentre, observational, prospective study. Lancet Oncol 12:1143–1150
Ye DW, Zhang HL (2014) Critical appraisal of sorafenib in the treatment of Chinese patients with renal cell carcinoma. Onco Targets Ther 7:925–935
Weitzman SA, Gordon LI (1990) Inflammation and cancer: role of phagocyte-generated oxidants in carcinogenesis. Blood 76:655–663
Kusumanto YH, Dam WA, Hospers GA et al (2003) Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis 6:283–287
Mantovani A, Allavena P, Sica A et al (2008) Cancer-related inflammation. Nature 454:436–444
Rosenberg SA (2001) Progress in human tumour immunology and immunotherapy. Nature 411:380–384
Acknowledgments
This study was supported in part by grants from the National Natural Science Foundation of China (Grant No. NSFC 81001131).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
G. - M. Zhang and Y. Zhu contribute equally to the work.
About this article
Cite this article
Zhang, GM., Zhu, Y., Gu, WJ. et al. Pretreatment neutrophil-to-lymphocyte ratio predicts prognosis in patients with metastatic renal cell carcinoma receiving targeted therapy. Int J Clin Oncol 21, 373–378 (2016). https://doi.org/10.1007/s10147-015-0894-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-015-0894-4