Abstract
Aneurysmal subarachnoid hemorrhage (aSAH) may lead to cerebral vasospasm, significantly associated with morbidity and mortality. In double-blind, placebo-controlled phase 3 studies, clazosentan reduces cerebral vasospasm-related morbidity and all-cause mortality in patients with aSAH. There are no reports about the clinical efficacy of clazosentan combination therapy with some other drugs. Initially, we explored the efficacy of clazosentan combination therapy with cilostazol, statin, and antiepileptic drugs. Subsequently, we assessed the add-on effect of fasudil to clazosentan combination therapy for aSAH patients. This multicenter, retrospective, observational cohort study included Japanese patients with aSAH between June 2022 and March 2023. The primary outcome was the ordinal score on the modified Rankin Scale (mRS; range, 0–6, with elevated scores indicating greater disability) at discharge. Among the 47 cases (women 74.5%; age 64.4 ± 15.0 years) undergoing clazosentan combination therapy, 29 (61.7%) resulted in favorable outcomes. Overall, vasospasm occurred in 16 cases (34.0%), with four cases (8.5%) developing vasospasm-related delayed cerebral ischemia (DCI). Both hypotension and vasospasm-related DCI were related to unfavorable outcome at discharge. Fasudil were added in 18 (38.3%) cases. Despite adding fasudil to clazosentan combination therapy, the incidence of aSAH-related vasospasm did not decrease. Added-on fasudil to combination therapy related to pulmonary edema, vasospasm, and vasospasm-related DCI, and unfavorable outcomes. Clazosentan combination therapy could potentially result in favorable outcomes for aSAH patients to prevent post-aSAH vasospasm-related DCI. The add-on effect of fasudil to combination therapy did not demonstrate a significant impact in reducing aSAH-related vasospasm or improving outcomes at discharge.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cerebral vasospasm is a significant cause of morbidity following aneurysmal subarachnoid hemorrhage (aSAH) [10, 17]. Angiographic vasospasm is observed in 70% of aSAH cases [6]. Approximately 40% of patients with cerebral vasospasm develop delayed ischemic neurological deficits, and 50% exhibit delayed cerebral ischemia (DCI) [8]. Cerebral vasospasm may be present as early as 24 h after onset but often begins 3–4 days after aneurysm rupture and peaks 7–10 days later before spontaneously resolving after 21 days.
The pathogenesis of cerebral vasospasm is not fully understood. Cerebral vasospasm may be caused by the degradation of blood products in the subarachnoid and perivascular spaces [49]. Current management strategies include the administration of nimodipine [9], ozagrel sodium [29], fasudil hydrochloride hydrate (“fasudil”) [33, 38], statins [32], and cilostazol [37]. However, their therapeutic efficacy is unsatisfactory [7].
Previous studies have suggested that endothelin-1, a potent and persistent endogenous vasoconstrictor, plays a role in the development of cerebral vasospasm [51]. After aSAH onset, the concentration of endothelin increases in the cerebral arteries, thereby increasing the sensitivity to endothelin-1 and intracellular calcium concentration [19].
Clazosentan, a selective endothelin receptor antagonist, inhibits endothelin-mediated cerebral vasospasm [2]. Several trials have been conducted to evaluate the efficacy and safety of clazosentan for preventing or modulating cerebral vasospasm in patients with aSAH [12, 23,24,25, 41]. Clazosentan was recently assessed in placebo-controlled, randomized, double-blind studies in adult Japanese patients with aSAH and showed a significant reduction in cerebral vasospasm-related morbidity and all-cause mortality within six weeks post-aSAH [11].
There are no reports about the clinical efficacy of clazosentan in combination therapy with some other drugs for the prevention of aSAH-related vasospasm. In this study, initially we investigate the efficacy of clazosentan combination therapy with cilostazol, statin, and antiepileptic drugs (AEDs). Subsequently we evaluate the add-on effect of fasudil to clazosentan combination therapy in aSAH patients.
Methods
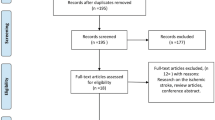
This multicenter, retrospective, observational cohort study used data from patients with aSAH to investigate real-world data of clazosentan in combination therapy regimens.
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of Kariya Toyota General Hospital (approval number: 846). All experiments were performed following the STROBE guidelines. The requirement for informed consent was waived because the analysis used anonymous clinical data obtained after each patient had agreed to treatment by providing written consent. Furthermore, we applied the opt-out method to obtain approval for this study using a poster approved by the Institutional Review Board.
Study design and population
The study populations were enrolled at the Department of Neurosurgery of three hospitals, including Kariya Toyota General Hospital, Handa City Hospital, and Tosei General Hospital, from June 2022 to March 2023. According to American Heart Association/American Stroke Association guidelines, aSAH was diagnosed by head CT, CT angiography (CTA), or digital subtraction angiography [5].
The inclusion criteria were as follows: (1) spontaneous aneurysmal SAH; (2) surgical clipping or coil embolization performed within 24 h after onset; and (3) clazosentan was administered during the perioperative period. The exclusion criteria were: (1) non-aneurysmal or traumatic SAH; (2) non-surgical intervention; and (3) clazosentan was not administered.
Clinical data collection
We used a data registration sheet. This sheet included the following information: age, sex, body mass index (BMI), comorbidities (hypertension, diabetes mellitus, dyslipidemia), past medical history (any stroke, heart disease, renal disease), smoking history, modified Rankin Scale (mRS) score before onset, World Federation of Neurosurgical Societies (WFNS) grade, Fisher group, preoperative laboratory data, preoperative cardiac function (left ventricular ejection fraction), preoperative respiratory complications, aneurysm site, surgical procedure, cerebrospinal fluid drainage, intraoperative fluid balance, intraoperative urine output, postoperative management (medication, laboratory data, fluid balance per 24 h, and urine output per 24 h), angiographic cerebral vasospasm, vasospasm-related DCI, and mRS at discharge. The difference between the concentration of serum albumin (⊿Alb), sodium (⊿Na), hemoglobin (⊿Hb), and hematocrit (⊿Hct) at the onset and lowest value in the postoperative two weeks was calculated.
Therapeutic protocol
All patients underwent microsurgical clipping or coil embolization within 24 h of onset. Postoperative medical therapy was typically initiated on postoperative day (POD) 1, including cilostazol (200 mg/day), pitavastatin (2 mg/day), and antiepileptic drugs (levetiracetam 1000 mg/day or perampanel hydrate 2 mg/day). These drugs were used for two or three postoperative weeks. Intravenous clazosentan administration (10 mg/h) was continued from POD 1 to POD 14. Given that the choice to incorporate fasudil (30 mg*3/day) or ozagrel sodium (80 mg/day) was at the attending physician's discretion, these drugs were concurrently administered with the initiation of postoperative clazosentan.
Enteral feeding or oral intake was initiated on POD 1. Head computed tomography (CT) angiography was performed in patients who had undergone surgical clipping, and digital subtraction angiography (DSA) was performed in patients who underwent coil embolization. Brain magnetic resonance imaging (MRI) and MR angiography were performed on POD 5, 10, and 15. Chest radiography was performed daily in the first postoperative week. Fluid balance was measured every 24 h until POD 15. If the daily fluid balance was negative, 500 mL extracellular fluid loading was delivered during this period. In the case of pulmonary edema, furosemide (20–40 mg/day) or tolvaptan (7.5 mg–15 mg/day) was occasionally administered. In the case of hypotension, if urine output was within normal limits, dobutamine (1–5mcg/kg/min) or norepinephrine (0.05–0.3mcg/kg/min) treatment was initiated. When pulmonary edema was sufficient to increase oxygen demand even with diuretic use, clazosentan was discontinued rather than non-invasive positive pressure ventilation or ventilator management. Clazosentan was also discontinued if hypotension did not improve with dobutamine or norepinephrine administration.
Image assessment
Independent neurosurgeons or radiologists blinded to the clinical information reviewed consecutive imaging studies. Based on the initial preoperative CT angiography, angiographic cerebral vasospasm was defined as inner artery reduction ≥ 50%.
Outcomes
The primary outcome was the ordinal score on the modified Rankin Scale (mRS; range, 0 [no symptoms] to 6 [death] with elevated scores indicating greater disability) at discharge. Outcomes on the mRS were defined as favorable (0–2) or unfavorable (5–6). The secondary outcome was vasospasm and vasospasm-related DCI. DCI was described as a new high-intensity region on MRI between 4 and 20 days after SAH. It was assumed to be a recent infarction if it was not visible on admission and the immediate postoperative CT scans. MRI and CT angiography/DSA confirmed the cause of DCI related to cerebral vasospasm according to the following criteria [46, 47]:
-
1.
No other cause underlying permanent or temporary focal neurological impairment, such as hypoxia, electrolyte imbalance, infection, hydrocephalus, or seizure.
-
2.
The Glasgow Coma Scale score decreased by at least two points.
-
3.
No brain injury related to the treatment itself.
In previous studies, treatment-associated adversities like hypotension and pulmonary edema were documented [11, 12]. Such adverse events were also evaluated as safety outcomes in our current study.
Statistical analysis
We used SPSS for Windows version 20.0 (IBM, Chicago, IL, USA) for all statistical analyses. Continuous variables are presented as the mean ± standard deviation, and categorical variables are described as percentages. The risk factors for vasospasm, pulmonary edema, hypotension, vasospasm-related DCI, and unfavorable outcome (mRS 5–6) were evaluated using the chi-square test or Mann–Whitney U test. Binary logistic regression analysis was performed to calculate the odds ratio (OR) and corresponding confidence interval (CI). Receiver operating characteristic (ROC) curves were plotted to determine the threshold value of each parameter for predicting pulmonary edema, hypotension, vasospasm, and vasospasm-related DCI. The sensitivity and specificity of each parameter were calculated to identify the optimal threshold values.
Statistical significance was set at p < 0.05. A model with an area under the ROC curve (AUC) score of more than 0.7 was evaluated as adequate or better.
Results
Patient characteristics
We used clazosentan for 47 patients with aSAH (women: 35, men: 12; age 64.4 ± 15.0 years) from June 2022 to March 2023. Patient characteristics are presented in Table 1. The mean body mass index was 22.5 ± 3.8 kg/m2. Hypertension was observed in 20 cases (42.6%), diabetes mellitus in 1 case (2.1%), and dyslipidemia in 6 cases (12.8%), and a positive smoking history was reported in 11 cases (23.4%). The median WFNS grade was 2 (IQR: 2–4), and that of the Fisher group was 3. Aneurysms were located in the anterior communicating artery (14 cases, 29.8%), internal carotid artery-posterior communicating artery (13 cases, 27.7%), middle cerebral artery (12 cases, 25.5%), and vertebral artery/basilar artery (4 cases, 8.5%). These aneurysms were treated surgically (32 cases, 68.1%) or endovascularly (15 cases, 31.9%). Cerebral fluid drainage was required in 26 cases (55.3%).
Primary and secondary outcomes
Postoperative management information and clinical outcomes are presented in Table 2. Among the 47 cases, 29 (61.7%) obtained favorable outcomes, and 9 (19.1%) had unfavorable outcomes at discharge. Vasospasms occurred in 16 cases (34.0%), but vasospasm-related DCI was only reported in 4 cases (8.5%).
Univariate risk factors for unfavorable outcomes, vasospasm, and vasospasm-related DCI were assessed, and multivariate analysis was performed (Table 3). Unfavorable outcomes were significantly related to hypotension (OR 16.111, 95% CI 1.659–156.501; p = 0.017), and associated to vasospasm-related DCI (OR 9.000, 95% CI 0.982–82.496; p = 0.052).
The risk factors for vasospasm were higher BMI (OR 4.976, 95% CI 1.183–20.923; p = 0.029), positive fluid balance (OR 1.017, 95% CI 1.002–1.033; p = 0.028), lower urine output within the first postoperative week (OR 1.027, 95% CI 1.000–1.055; p = 0.050), and lower urine output within the first two postoperative weeks (OR 0.973, 95% CI 0.946–1.000; p = 0.049). The risk factors for vasospasm-related DCI were clazosentan discontinuation (OR 294.105, 95% CI 0.356–∞; p = 0.029), positive fluid balance within the first postoperative week (OR 0.977, 95% CI 0.950–1.006; p = 0.038), and positive fluid balance within the first two postoperative weeks (OR 1.025, 95% CI 0.996–1.055; p = 0.027).
ROC curves were plotted to determine the threshold value of each parameter for predicting vasospasm and vasospasm-related DCI. The sensitivity and specificity of each parameter were calculated to identify the optimal threshold values (Table 4).
To assess the vasospasm risk factors, the cut-off value for fluid balance within the first postoperative week was –25 mL (AUC 0.706, 95% CI 0.544–0.867; p = 0.027, sensitivity 0.867, specificity 0.552). The AUCs for the BMI, urine output within the first postoperative week, total urine output, and minimum albumin level were 0.610 (95% CI 0.431–0.790; p = 0.235), 0.580 (95% CI 0.409–0.752; p = 0.386), 0.591 (95% CI 0.420–0.762; p = 0.328), and 0.699 (95% CI 0.526–0.871; p = 0.032), respectively. Therefore, these parameters were unsuitable for the prediction of vasospasm.
To ingestigate the vasospasm-related DCI, the cut-off value for total fluid balance was 130 ml (AUC 0.762, 95% CI 0.548–0.976; p = 0.086, sensitivity 0.750, specificity 0.738). The AUC for fluid balance within the first postoperative week was 0.696 (95% CI 0.478–0.914; p = 0.198), which was unsuitable for predicting vasospasm-related DCI.
Fluid balance during the first postoperative week and the first two weeks were 58.9 ± 500.1 mL and -0.3 ± 540.1 mL, respectively. Urine output in the first postoperative week and during the first two weeks were 1657.3 ± 669.3 mL and 1726.8 ± 680.2 mL, respectively. The lowest serum albumin, sodium, hemoglobin, and hematocrit levels in the first two postoperative weeks were 2.61 ± 0.46 g/dL, 135.1 ± 4.1 mEq/L, 9.4 ± 1.4 g/dL, and 28.2 ± 4.0%, respectively. The ⊿Alb was 1.58 ± 0.44 g/dL, ⊿Na was 4.4 ± 5.0 mEq/L, ⊿Hb was 3.8 ± 1.6 g/dL, and ⊿Hct was 11.4 ± 4.1%.
Safety outcomes
Pulmonary complications were observed in 19 cases (40.4%) and hypotension in 16 cases (34.0%). Clazosentan was discontinued owing to pulmonary complications in 8 cases (17.0%). Smoking history was significantly related to clazosentan discontinuation (p = 0.049). The reasons for clazosentan discontinuation were respiratory complication (7 cases), hypotension (3 cases), and brain edema (1 case).
Univariate risk factors for pulmonary edema and hypotension were assessed, and multivariate analysis was performed (Table 3). ROC curves were plotted to determine the threshold value of each parameter for predicting pulmonary edema, hypotension, vasospasm, and vasospasm-related DCI. The sensitivity and specificity of each parameter were calculated to identify the optimal threshold values (Table 4).
Older age (OR 1.105, 95% CI 1.019–1.199; p = 0.016), clazosentan discontinuation (OR 29.255, 95% CI 1.321–647.981; p = 0.033), positive fluid balance (OR 1.003, 95% CI 1.000–1.006, p = 0.029), and lower serum albumin levels (OR 0.001, 95% CI 0–0.164; p = 0.010) were significant independent risk factors for pulmonary edema. ROC analysis showed that the AUC was 0.791 (95% CI 0.644–0.937; p = 0.001), and the optimal cut-off value with the maximum sensitivity and specificity for age at pulmonary edema occurrence was 67 years old (sensitivity 0.889, specificity 0.821).
The optimal cut-off value with the highest sensitivity and specificity in the ROC curve for total fluid balance was -50 mL (AUC 0.804, 95% CI 0.678–0.929; p = 0.001, sensitivity 0.889, specificity 0.607). The cut-off value of the minimum serum albumin level was 2.65 g/dL (AUC 0.915, 95% CI 0.828–1.000; p < 0.001, sensitivity 1.000, specificity 0.786).
Lower BMI (OR 0.599, 95% CI 0.373–0.963, p = 0.034), higher WFNS grade (OR 6.274, 95% CI 1.687–23.329; p = 0.006), lower urine output within the first postoperative week (OR 0.995, 95% CI 0.991–0.998; p = 0.005), lower serum albumin levels (OR 0.014, 95% CI 0–0.818; p = 0.040), higher serum sodium levels (OR 1.906, 95% CI 1.064–3.412; p = 0.030), and lower delta hematocrit levels (OR 0.236, 95% CI 0.071–0.784; p = 0.018) were significant independent risk factors for hypotension.
The cut-off value for BMI was 21.1 kg/m2 (AUC 0.706, 95% CI 0.551–0.862; p = 0.022, sensitivity 0.687, specificity 0.767). The cut-off value for urine output within the first postoperative week was 1350 mL (AUC 0.773, 95% CI 0.639–0.907; p = 0.003, sensitivity 0.687, specificity 0.800). The cut-off value for the minimum serum albumin level was 2.65 g/dL (AUC 0.772, 95% CI 0.632–0.912; p = 0.003, sensitivity 0.875, specificity 0.667). The AUCs for the minimum serum sodium and delta hematocrit levels were 0.692 (95% CI 0.537–0.847; p = 0.034) and 0.603 (95% CI 0.424–0.782; p = 0.091), respectively. Hence, these parameters were not suitable for the prediction of hypotension.
Add-on effect of fasudil to clazosentan combination therapy
Fasudil was incorporated into clazosentan combination therapy, resulting in "multidrug therapy" in 18 cases (38.3%). As depicted in Table 5, when comparing clazosentan combination therapy with multidrug therapy, a discrepancy in the patients' baseline characteristics was observed. Multidrug therapy was more prevalent in patients with higher BMI (p = 0.021). Microsurgical clipping was executed in patients utilizing clazosentan combination therapy (p = 0.024). The postoperative fluid balance was significantly higher in the multidrug therapy group (p = 0.022). Multidrug therapy was associated with a probable increase in unfavorable outcomes (13.8% vs. 27.8%, p = 0.274), aSAH-related vasospasm (24.1% vs. 44.4%, p = 0.202), vasospasm-related DCI (3.4% vs. 16.7%, p = 0.150). In multidrug therapy, continuous administration of clazosentan proved challenging (6.9% vs. 33.3%, p = 0.053) due to complications associated with pulmonary edema (31.0% vs. 55.6%, p = 0.130).
Representative case
A 68-year-old man was brought to the hospital by ambulance with a disturbance of consciousness. Head CT showed a massive SAH due to a ruptured anterior communicating artery aneurysm (Fig. 1A, B). He was classified as WFNS grade 5 and Fisher group 3. Chest radiography revealed aspiration pneumonia (Fig. 1 C). Endovascular treatment was performed, and cilostazol and levetiracetam were administered from POD 1. Chest radiography revealed that aspiration pneumonia improved on POD 2 (Fig. 2A). On the same day, extubation was performed, and clazosentan, fasudil, statins, and cilostazol were administered. His respiratory condition gradually worsened from POD 5 (Fig. 2B) because of pulmonary edema; ozagurel was administered from POD 6, and clazosentan was discontinued on POD 7. The pulmonary disease improved from POD 8 (Fig. 2C), and the patient did not require oxygen. Cerebrospinal fluid drainage using an indwelling spinal catheter was continued from POD 1 to POD 14. During the first two postoperative weeks, head MRI/MRA did not detect vasospasm (Fig. 2D–F). The patient was transferred to a rehabilitation hospital with an mRS score of 2.
Radiological clinical course. (A) Chest radiography showing improvement in aspiration pneumonia on postoperative day (POD) 2. (B) Pleural effusion and pulmonary edema were observed on POD 5. (C) After clazosentan discontinuation, the pulmonary condition improved smoothly on POD 8. (D–F) Head magnetic resonance angiography showing no vasospasm on POD 5, 10, and 15
Discussion
To our knowledge, this is the first report to assess the real-world data of clazosentan use in combination with other therapeutic drugs, such as ozagrel sodium, fasudil, cilostazol, statins, and AEDs.
In our study, although vasospasm occurred in one-third of cases, the incidence rate of vasospasm-related DCI was less than 10%, and about two-thirds had favorable outcomes. Pulmonary edema and hypotension occurred in about one-third of cases. Hypotension and vasospasm-related DCI were poor prognostic factors unrelated to older age or disease severity at aSAH onset.
Although fasudil was added to clazosentan combination therapy, the incidence of aSAH-related vasospasm did not decrease. On the contrary, the addition of fasudil seemed to generate a positive in–out balance and could potentially contribute to the emergence of pulmonary edema complications. Further, the inclusion of fasudil was associated with an uptick in the incidence of cerebral vasospasm, vasospasm-related DCI, and unfavorable outcomes.
Vasospasm, DCI, and outcomes
In our study, vasospasm occurred when urine output was low despite a daily positive balance in slightly obese patients. On the other hand, vasospasm-associated DCI occurred when a positive balance continued daily, regardless of urine output. In one-third of cases, vasospasm was observed, but less than 10% developed DCI. Previous studies estimated the incidence of vasospasm-related DCI to be 30% [5, 13]. Previous placebo-controlled, randomized, and double-blind studies showed that 10.7%–18.6% of unfavorable outcomes occurred within six weeks [11]. In our study, the incidence rates of vasospasm-related DCI and unfavorable outcomes were lower than those in previous reports.
There was no significant add-on effect of fasudil to clazosentan combination therapy in preventing aSAH-related vasospasm. On the contrary, the addition of fasudil seemed to generate a positive in–out balance and could potentially contribute to the emergence of pulmonary edema complications. Further, the inclusion of fasudil was associated with an uptick in the incidence of cerebral vasospasm, vasospasm-related DCI, and unfavorable outcomes. In case of clazosentan administration in patients with aSAH, it may be advisable not to use it with fasudil. If there are cases of difficulty maintaining patients on clazosentan, using fasudil as a switch drug in such cases may be feasible.
The mechanism of DCI
Both DCI and vasospasm result from physiological changes such as early brain injury, microcirculation disturbances, microthrombosis, neuroinflammation, and cortical spreading depolarization (CSD) [13].
Recent research has recognized neuroelectrical disturbances, especially CSD and epileptiform activity, as critical contributors to the onset of DCI following aSAH. These disturbances can lead to detrimental effects, such as escalated metabolic demand, reversed neurovascular coupling inducing arteriolar vasoconstriction, microthrombus generation from platelet activation, and neuroinflammatory reactions, all potentially leading to DCI [35]. Some antiepileptic drugs have been reported to counteract both CSDs and epileptiform discharges, thus mitigating DCI [18]. Consequently, for this study, we opted to employ levetiracetam or perampanel—both reported as beneficial—as the foundational antiepileptic medications to enhance patient prognosis [36].
Accumulating evidence suggests that inflammation, particularly neuroinflammation, is associated with secondary outcomes following aSAH, including DCI and vasospasm [22, 26]. The multifaceted effects of statins, encompassing their anti-inflammatory properties, have been documented. Statins have demonstrated improvement in cerebral vasomotor reactivity, cerebral blood flow, and fibrinolytic activity [40]. The diminished endothelial nitric oxide synthase (eNOS) and endothelial function following SAH could be amplified by statin administration through activation of the phosphatidylinositol 3-kinase/Akt pathways, thereby mitigating vasospasm and enhancing cerebral vasomotor reactivity and patient outcomes [31, 34]. Given these considerations, statins were administered due to their projected beneficial effects, such as antioxidative, eNOS-inducing, endothelial cell-stabilizing, and anti-inflammatory properties in the treatment of cerebral vasospasm and DCI.
Cilostazol exhibited multifaceted effects on DCI reduction, encompassing the alleviation of angiographic vasospasm, enhancement of microcirculation [32], and attenuation of CSD through microcirculatory vasodilatation, which is mediated by both cyclic adenosine monophosphate and the upregulation of eNOS [16]. Moreover, cilostazol's mechanisms in inhibiting cerebral vasospasm pathogenesis predominantly involve several components: the suppression of lipid peroxidation [15], the decrease of reactive oxygen species [30], the induction of NO production [16], the prevention of endothelial damage [14, 50], and the hindrance of vascular smooth muscle proliferation [50]. Thus, in this study, we administered cilostazol to preempt microcirculation disturbances, microthrombosis, and CSD.
Hypotension
In healthy subjects, clazosentan has vasodilatory effects and slightly decreased systolic and diastolic blood pressure. However, this effect was not reported as clinically important [43, 44]. On the other hand, previous clinical studies of clazosentan reported that hypotension occurred in 10%–15% of patients [11, 12, 23,24,25]. In our study, 34% of cases showed hypotension. Therefore, perioperative combination therapy with clazosentan may lead to hypotension.
Cardiopulmonary dysfunction sometimes occurs after aSAH and is related to catecholamine release and sympathetic overstimulation [4, 42, 48]. Patients with a higher WFNS grade for aSAH are more likely to have complications of cardiopulmonary dysfunction. Echocardiography may show wall motion abnormality, and one of the most typical findings is apical ballooning and Takotsubo cardiomyopathy [20, 21, 27]. Treating stress cardiomyopathy with inotropes like milrinone or dobutamine could improve cardiac output and brain perfusion [4]. In our study, in slightly emaciated patients with a higher WFNS grade, if the serum albumin levels decrease despite a decrease in urine output during the perioperative period, these patients were likely to have hypotension. The clinical effects of dobutamine or norepinephrine to prevent hypotension while on perioperative clazosentan combination therapy must be evaluated.
Fluid retention
Fluid retention, mainly pulmonary edema, occurred in 40% of our cases (almost all had respiratory impairment requiring oxygen supplementation) and required diuretics. Previous clinical studies on clazosentan reported that respiratory complications occurred in 10–25% of patients [11, 12, 23,24,25]. In our study, respiratory failure did not improve despite diuretic use, leading to clazosentan discontinuation in approximately 15% of cases. Pulmonary edema occurred in cases with a positive fluid balance, with decreased serum albumin levels reflecting increased intravascular volume. It is essential to avoid managing older patients with a positive fluid balance day after day because of the possibility of respiratory compromise due to fluid retention. In this study, perioperative aSAH treatment management was primarily handled with euvolemia; however, if the fluid balance was positive on each postoperative day, pulmonary complications would likely occur with clazosentan. Intraoperative fluid balance has not been extensively discussed in managing patients with aSAH. Brandstrup et al. compared surgical patients who were given infusions to compensate for preoperative fluid deficits with those where surgeons focused solely on the intraoperative fluid balance. When patients undergoing surgery are given excessive infusions to compensate for fluid deficits, the fluid not excreted intraoperatively remains for at least six days after surgery, leading to complications such as heart failure and pulmonary edema [6].
Clazosentan is a peripheral vasodilator and may also increase capillary permeability. Excessive intraoperative and postoperative fluid infusions may result in pulmonary edema. Furthermore, some reports showed that positive fluid balance within the early postoperative phase was related to DCI and poor outcomes [1, 45]. For infusion management, it may be necessary to consider total fluid balance during surgery. However, the fluid balance may not precisely reflect blood or plasma volume. Some reports showed that measurement of the extravascular lung water index, cardiac index, and pulmonary vascular permeability index using an invasive device was useful for identifying pulmonary edema in patients with aSAH [28, 29, 39]. Other less invasive monitoring parameters may be useful, such as body weight changes, cardiac output, and oxygen consumption. Further investigation will be needed on perioperative fluid management in patients with aSAH.
Limitations
This study has some limitations. First, numerous drugs were used to prevent vasospasm; therefore, these results cannot be attributed to clazosentan alone. However, in clazosentan combination therapy, it should be noted that vasospasm-related DCI occurred in only less than 10% of patients, regardless of aSAH severity or patient age. Second, this report is a small, retrospective study of patients with aSAH who underwent surgical treatment. A large, prospective cohort trial will be needed to evaluate the effectiveness of clazosentan in daily practice.
Conclusion
We first evaluated the efficacy of clazosentan in real clinical practice. Although vasospasm occurred in one-third of cases, the incidence rate of vasospasm-related DCI was less than 10%, and about two-thirds had favorable outcomes. Pulmonary edema and hypotension occurred in about one-third of cases. Hypotension and vasospasm-related DCI were poor prognostic factors unrelated to older age or disease severity at aSAH onset. Next, we investigated the add-on effect of fasudil on clazosentan. Adding fasudil to clazosentan combination therapy did not reduce the incidence rate of aSAH-related vasospasm. On the contrary, the addition of fasudil seemed to generate a positive in–out balance and could potentially contribute to the emergence of pulmonary edema complications. Further, the inclusion of fasudil was associated with an uptick in the incidence of cerebral vasospasm, vasospasm-related DCI, and unfavorable outcomes. Clazosentan may increase the risk of complications, such as hypotension and pulmonary edema. Perioperative fluid balance management may be critical for preventing unfavorable outcomes.
Data availability
The datasets used or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Anetsberger A, Gempt J, Blobner M et al (2020) Impact of goal-directed therapy on delayed ischemia after aneurysmal subarachnoid hemorrhage: randomized controlled trial. Stroke 51:2287–2296. https://doi.org/10.1161/STROKEAHA.120.029279
Barth M, Capelle HH, Münch E et al (2007) Effects of the selective endothelin A (ET(A)) receptor antagonist clazosentan on cerebral perfusion and cerebral oxygenation following severe subarachnoid hemorrhage - preliminary results from a randomized clinical series. Acta Neurochir (Wien) 149:911–918. https://doi.org/10.1007/s00701-007-1249-3
Brandstrup B, Tønnesen H, Beier-Holgersen R, Hjortsø E, Ørding H, Lindorff-Larsen K et al (2003) Danish Study Group on Perioperative Fluid Therapy. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg 238:641–648. https://doi.org/10.1097/01.sla.0000094387.50865.23
Bruder N, Rabinstein A, Participants in the International Multidisciplinary Consensus Conference on the Critical Care Management of Subarachnoid Hemorrhage (2011) Cardiovascular and pulmonary complications of aneurysmal subarachnoid hemorrhage. Neurocrit Care 15:257–269. https://doi.org/10.1007/s12028-011-9598-4
Connolly ES, Rabinstein AA, Carhuapoma JR et al (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American stroke association. Stroke 43:1711–1737. https://doi.org/10.1161/STR.0b013e3182587839
Crowley RW, Medel R, Kassell NF, Dumont AS (2008) New insights into the causes and therapy of cerebral vasospasm following subarachnoid hemorrhage. Drug Discov Today 13:254. https://doi.org/10.1016/j.drudis.2007.11.010
Dayyani M, Sadeghirad B, Grotta JC et al (2022) Prophylactic Therapies for Morbidity and Mortality After Aneurysmal Subarachnoid Hemorrhage: A Systematic Review and Network Meta-Analysis of Randomized Trials. Stroke 53(6):1993–2005. https://doi.org/10.1161/STROKEAHA.121.035699
de Oliveira JG, Beck J, Ulrich C, Rathert J, Raabe A, Seifert V (2007) Comparison between clipping and coiling on the incidence of cerebral vasospasm after aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. Neurosurg Rev 30:22–31. https://doi.org/10.1007/s10143-006-0045-5
DorhoutMees SM, Rinkel GJ, Feigin VL et al (2007) Calcium antagonists for aneurysmal subarachnoid hemorrhage. Cochrane Database Syst Rev 2007:CD000277. https://doi.org/10.1002/14651858.CD000277.pub3
Dorsch NW (2002) Therapeutic approaches to vasospasm in subarachnoid hemorrhage. Curr Opin Crit Care 8:128–133. https://doi.org/10.1097/00075198-200204000-00007
Endo H, Hagihara Y, Kimura N et al (2022) Effects of clazosentan on cerebral vasospasm-related morbidity and all-cause mortality after aneurysmal subarachnoid hemorrhage: two randomized phase 3 trials in Japanese patients. J Neurosurg 137:1707–1717. https://doi.org/10.3171/2022.2.JNS212914
Fujimura M, Joo JY, Kim JS, Hatta M, Yokoyama Y, Tominaga T (2017) Preventive effect of clazosentan against cerebral vasospasm after clipping surgery for aneurysmal subarachnoid hemorrhage in Japanese and Korean patients. Cerebrovasc Dis 44:59–67. https://doi.org/10.1159/000475824
Geraghty JR, Testai FD (2017) Delayed cerebral ischemia after subarachnoid hemorrhage: beyond vasospasm and towards a multifactorial pathophysiology. Curr Atheroscler Rep 19:50. https://doi.org/10.1007/s11883-017-0690-x
Hashimoto A, Tanaka M, Takeda S, Ito H, Nagano K (2015) Cilostazol Induces PGI2 Production via Activation of the Downstream Epac-1/Rap1 Signaling Cascade to Increase Intracellular Calcium by PLCε and to Activate p44/42 MAPK in Human Aortic Endothelial Cells. PloS one 10(7):e0132835. https://doi.org/10.1371/journal.pone.0132835
Ito H, Fukunaga M, Suzuki H, Miyakoda G, Ishikawa M, Yabuuchi Y, Taki W (2008) Effect of cilostazol on delayed cerebral vasospasm after subarachnoid hemorrhage in rats: evaluation using black blood magnetic resonance imaging. Neurobiol Dis 32(1):157–161. https://doi.org/10.1016/j.nbd.2008.07.004
Ito H, Hashimoto A, Matsumoto Y, Yao H, Miyakoda G (2010) Cilostazol, a phosphodiesterase inhibitor, attenuates photothrombotic focal ischemic brain injury in hypertensive rats. J Cereb Blood Flow Metab: official journal of the International Society of Cerebral Blood Flow and Metabolism 30(2):343–351. https://doi.org/10.1038/jcbfm.2009.220
Kassell NF, Torner JC, Jane JA, Haley EC Jr, Adams HP (1990) The international cooperative study on the timing of aneurysm surgery part 2: surgical results. J Neurosurg 73:37–47. https://doi.org/10.3171/jns.1990.73.1.0037
Klass A, Sánchez-Porras R, Santos E (2018) Systematic review of the pharmacological agents that have been tested against spreading depolarizations. J Cereb Blood Flow Metab: official journal of the International Society of Cerebral Blood Flow and Metabolism 38(7):1149–1179. https://doi.org/10.1177/0271678X18771440
Kramer A, Fletcher J (2009) Do endothelin-receptor antagonists prevent delayed neurological deficits and poor outcomes after aneurysmal subarachnoid hemorrhage?: a meta-analysis. Stroke 40:3403–3406. https://doi.org/10.1161/STROKEAHA.109.560243
Lee VH, Oh JK, Mulvagh SL, Wijdicks EF (2006) Mechanisms in neurogenic stress cardiomyopathy after aneurysmal subarachnoid hemorrhage. Neurocrit Care 5:243–249. https://doi.org/10.1385/NCC:5:3:243
Lee VH, Connolly HM, Fulgham JR, Manno EM, Brown RD Jr, Wijdicks EF (2006) Tako-tsubo cardiomyopathy in aneurysmal subarachnoid hemorrhage: an underappreciated ventricular dysfunction. J Neurosurg 105:264–270. https://doi.org/10.3171/jns.2006.105.2.264
Lucke-Wold BP, Logsdon AF, Manoranjan B, Turner RC, McConnell E, Vates GE, Huber JD, Rosen CL, Simard JM (2016) Aneurysmal Subarachnoid Hemorrhage and Neuroinflammation: A Comprehensive Review. Int J Mol Sci 17(4):497. https://doi.org/10.3390/ijms17040497
Macdonald RL, Kassell NF, Mayer S et al (2008) Clazosentan to overcome neurological ischemia and infarction occurring after subarachnoid hemorrhage (CONSCIOUS-1): randomized, double-blind, placebo-controlled phase 2 dose-finding trial. Stroke 39:3015–3021. https://doi.org/10.1161/STROKEAHA.108.519942
Macdonald RL, Higashida RT, Keller E et al (2011) Clazosentan, an endothelin receptor antagonist, in patients with aneurysmal subarachnoid hemorrhage undergoing surgical clipping: a randomized, double-blind, placebo-controlled phase 3 trial (CONSCIOUS-2). Lancet Neurol 10:618–625. https://doi.org/10.1016/S1474-4422(11)70108-9
Macdonald RL, Higashida RT, Keller E et al (2012) Randomized trial of clazosentan in patients with aneurysmal subarachnoid hemorrhage undergoing endovascular coiling. Stroke 43:1463–1469. https://doi.org/10.1161/STROKEAHA.111.648980
McMahon CJ, Hopkins S, Vail A, King AT, Smith D, Illingworth KJ, Clark S, Rothwell NJ, Tyrrell PJ (2013) Inflammation as a predictor for delayed cerebral ischemia after aneurysmal subarachnoid haemorrhage. J Neurointerv Surg 5(6):512–517. https://doi.org/10.1136/neurintsurg-2012-010386
Murthy SB, Shah S, Rao CP, Bershad EM, Suarez JI (2015) Neurogenic stunned myocardium following acute subarachnoid hemorrhage: pathophysiology and practical considerations. J Intensive Care Med 30:318–325. https://doi.org/10.1177/0885066613511054
Mutoh T, Kazumata K, Terasaka S, Taki Y, Suzuki A, Ishikawa T (2014) Early intensive versus minimally invasive approach to postoperative hemodynamic management after subarachnoid hemorrhage. Stroke 45:1280–1284. https://doi.org/10.1161/STROKEAHA.114.004739
Obata Y, Takeda J, Sato Y, Ishikura H, Matsui T, Isotani E (2016) A multicenter prospective cohort study of volume management after subarachnoid hemorrhage: circulatory characteristics of pulmonary edema after subarachnoid hemorrhage. J Neurosurg 125:254–263. https://doi.org/10.3171/2015.6.JNS1519
Ota H, Eto M, Kano MR, Ogawa S, Iijima K, Akishita M, Ouchi Y (2008) Cilostazol inhibits oxidative stress-induced premature senescence via upregulation of Sirt1 in human endothelial cells. Arterioscler Thromb Vasc Biol 28(9):1634–1639. https://doi.org/10.1161/ATVBAHA.108.164368
Pluta RM, Thompson BG, Dawson TM, Snyder SH, Boock RJ, Oldfield EH (1996) Loss of nitric oxide synthase immunoreactivity in cerebral vasospasm. J Neurosurg 84(4):648–654. https://doi.org/10.3171/jns.1996.84.4.0648
Shen J, Zhu K, Zhu K, Zhou H, Tian H, Yu G (2019) Efficacy of statins in cerebral vasospasm, mortality and delayed cerebral ischemia in patients with aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis of randomized controlled trials. World Neurosurg 131:e65–e73. https://doi.org/10.1016/j.wneu.2019.07.016
Shibuya M, Suzuki Y, Sugita K et al (1992) Effect of AT877 on cerebral vasospasm after aneurysmal subarachnoid hemorrhage: results of a prospective placebo-controlled double-blind trial. J Neurosurg 76:571–577. https://doi.org/10.3171/jns.1992.76.4.0571
Sugawara T, Ayer R, Jadhav V, Chen W, Tsubokawa T, Zhang JH (2008) Simvastatin attenuation of cerebral vasospasm after subarachnoid hemorrhage in rats via increased phosphorylation of Akt and endothelial nitric oxide synthase. J Neurosci Res 86(16):3635–3643. https://doi.org/10.1002/jnr.21807
Suzuki H, Kawakita F, Asada R, Nakano F, Nishikawa H, Fujimoto M (2022) Old but Still Hot Target, Glutamate-Mediated Neurotoxicity in Stroke. Transl Stroke Res 13(2):216–217. https://doi.org/10.1007/s12975-021-00958-6
Suzuki H, Miura Y, Yasuda R, Yago T, Mizutani H, Ichikawa T, Miyazaki T, Kitano Y, Nishikawa H, Kawakita F, Fujimoto M, Toma N (2022) Effects of New-Generation Antiepileptic Drug Prophylaxis on Delayed Neurovascular Events After Aneurysmal Subarachnoid Hemorrhage. Transl Stroke Res. https://doi.org/10.1007/s12975-022-01101-9.Advanceonlinepublication.10.1007/s12975-022-01101-9
Suzuki S, Sayama T, Nakamura T et al (2011) Cilostazol improves outcome after subarachnoid hemorrhage: a preliminary report. Cerebrovasc Dis 32:89–93. https://doi.org/10.1159/000327040
Suzuki Y, Shibuya M, Satoh S, Sugimoto Y, Takakura K (2007) A postmarketing surveillance study of fasudil treatment after aneurysmal subarachnoid hemorrhage. Surg Neurol 68:126–132. https://doi.org/10.1016/j.surneu.2006.10.037
Tagami T, Kuwamoto K, Watanabe A, Unemoto K, Yokobori S, Matsumoto G, Yokota H, SAH PiCCO Study Group (2014) Optimal range of global end-diastolic volume for fluid management after aneurysmal subarachnoid hemorrhage: a multicenter prospective cohort study. Crit Care Med 42:1348–1356. https://doi.org/10.1097/CCM.0000000000000163
Tseng MY, Czosnyka M, Richards H, Pickard JD, Kirkpatrick PJ (2005) Effects of acute treatment with pravastatin on cerebral vasospasm, autoregulation, and delayed ischemic deficits after aneurysmal subarachnoid hemorrhage: a phase II randomized placebo-controlled trial. Stroke 36(8):1627–1632. https://doi.org/10.1161/01.STR.0000176743.67564.5d
Vajkoczy P, Meyer BS, Raabe A et al (2005) Clazosentan (AXV-034343), a selective endothelin A receptor antagonist, in the prevention of cerebral vasospasm following severe aneurysmal subarachnoid hemorrhage: results of a randomized, double-blind, placebo-controlled, multicenter phase IIa study. J Neurosurg 103:9–17. https://doi.org/10.3171/jns.2005.103.1.0009
van der Bilt IA, Hasan D, Vandertop WP, Wilde AA, Algra A, Visser FC et al (2009) Impact of cardiac complications on outcome after aneurysmal subarachnoid hemorrhage: a meta-analysis. Neurology 72:635–642. https://doi.org/10.1212/01.wnl.0000342471.07290.07
van Giersbergen PL, Dingemanse J (2007) Effect of gender on the tolerability, safety and pharmacokinetics of clazosentan following long-term infusion. Clin Drug Invest 27:797–802. https://doi.org/10.2165/00044011-200727110-00006
van Giersbergen PL, Dingemanse J (2007) Tolerability, pharmacokinetics, and pharmacodynamics of clazosentan, a parenteral endothelin receptor antagonist. Eur J Clin Pharmacol 63:151–158. https://doi.org/10.1007/s00228-006-0117-z
Vergouw LJM, Egal M, Bergmans B et al (2020) High early fluid input after aneurysmal subarachnoid hemorrhage: combined report of association with delayed cerebral ischemia and feasibility of cardiac output-guided fluid restriction. J Intensive Care Med 35:161–169. https://doi.org/10.1177/0885066617732747
Vergouwen MDI, Vermeulen M, van Gijn J et al (2010) Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: proposal of a multidisciplinary research group. Stroke 41:2391–2395. https://doi.org/10.1161/STROKEAHA.110.589275
Vergouwen MDI, Vermeulen M, Coert BA, Stroes ES, Roos YB (2008) Microthrombosis after aneurysmal subarachnoid hemorrhage: an additional explanation for delayed cerebral ischemia. J Cereb Blood Flow Metab 28:1761–1770. https://doi.org/10.1038/jcbfm.2008.74
Wartenberg KE, Schmidt JM, Claassen J, Temes RE, Frontera JA, Ostapkovich N et al (2006) Impact of medical complications on outcome after subarachnoid hemorrhage. Crit Care Med 34:617–623. https://doi.org/10.1097/01.ccm.0000201903.46435.35. (quiz 24)
Weir B, Macdonald RL, Stoodley M (1999) Etiology of cerebral vasospasm. Acta Neurochir Suppl 72:27–46. https://doi.org/10.1007/978-3-7091-6377-1_3
Yamaguchi-Okada M, Nishizawa S, Mizutani A, Namba H (2009) Multifaceted effects of selective inhibitor of phosphodiesterase III, cilostazol, for cerebral vasospasm after subarachnoid hemorrhage in a dog model. Cerebrovasc Dis (Basel, Switzerland) 28(2):135–142. https://doi.org/10.1159/000223439
Zimmermann M, Seifert V (2004) Endothelin receptor antagonists and cerebral vasospasm. Clin Auton Res 14:143–145. https://doi.org/10.1007/s10286-004-0186-y
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
The authors declare that they have not received funding.
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design: S.M., T.A., T.N., Y.A., R.S.
Acquisition, analysis, and interpretation of data: S.M., T.F., S.O., S.S., N.K.
Drafting a significant portion of the manuscript or figures: S.M.
Supervision: R.S.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Institutional Review Board of Kariya Toyota General Hospital (approval number: 846), and all procedures were conducted in accordance with the Declaration of Helsinki.
Consent to participate
All experiments were performed according to the relevant guidelines and regulations. Patients were not required to provide informed consent for this study because the analysis used anonymous clinical data obtained after each patient had agreed to treatment by written consent. Furthermore, we used a poster to apply the opt-out method to obtain approval for this study. The Institutional Review Board of Kariya Toyota General Hospital approved the poster.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muraoka, S., Asai, T., Fukui, T. et al. Real-world data of clazosentan in combination therapy for aneurysmal subarachnoid hemorrhage: a multicenter retrospective cohort study. Neurosurg Rev 46, 195 (2023). https://doi.org/10.1007/s10143-023-02104-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-023-02104-2