Abstract
Brain metastases (BM) from lung cancer are among the most common intracranial tumors. Several studies have published scales to estimate the survival of patients with BM. Routine access to molecular diagnostics and modern oncologic treatments, including targeted therapy and immunotherapy, is limited in low- and middle-income countries (LMICs); therefore, incorporating them into recent prognostic scales may diminish the reliability of the scales in LMICs. This retrospective study aimed to determine the survival of 55 patients who were surgically treated for BM from lung cancer at a Brazilian public tertiary teaching hospital between 2012 and 2022. We determined clinical factors associated with survival, and compared observed survival rates with the estimated survival on prognostic scales. The mean overall survival (OS) was 9.3 months (range:0.2–76.5). At univariate analysis, female sex and improved postoperative Karnofsky performance status (KPS) score were associated with longer survival. The median survival did not differ between groups when classified using the Graded Prognostic Assessment (GPA)-2008, Lung-molecular GPA-2017, and Lung-GPA-2021 scales. According to the Diagnosis-Specific (DS)-GPA-2012 scale, there was a significant difference between the groups. In the multivariate Cox regression survival analysis, a higher DS-GPA-2012 and improved postoperative KPS score remained significantly associated with longer survival. In conclusion, this cohort showed a mean OS of < 1 year. Improved KPS score after surgery was associated with increased survival. This cohort DS-GPA scale demonstrated the highest concordance with observed survival, indicating its potential as a valuable tool for patient stratification in surgical treatment decision-making in LMICs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain metastases (BM) are among the most common intracranial tumors, with an incidence comparable to that of primary glial tumors and meningiomas [1,2,3,4]. BM may occur in up to a quarter of malignancy-related patient deaths [5]. Lung cancer is the most common source of BM, with a cumulative incidence in 5 years of up to 29.7% for small cell lung cancer (SCLC) and 12.6% for non-SCLC (NSCLC) [6]. BM are present in up to 15.8% of patients with lung cancer at the time of diagnosis [7]. The symptoms may include headaches, seizures, impaired consciousness, or focal neurological manifestations such as motor, sensory, or speech deficits [8].
In addition to symptom management, treatment of BM may involve radiation therapy, chemotherapy, and surgery. Oncology is currently focusing on advancements in targeted therapy and immunotherapy. For example, mutations in epidermal growth factor receptor (EGFR) or anaplastic lymphoma kinase (ALK) genes in NSCLC can be targeted by tyrosine kinase inhibitors (TKIs), whereas tumors expressing programmed death-ligand 1 (PD-L1) are candidates for immunotherapy with immune checkpoint inhibitors (ICIs) [9, 10]. However, surgical resection of BM is the only treatment promoting immediate resolution of the mass effect, and improving neurological deficits and faster corticosteroid weaning, with the additional advantage of diagnostic confirmation in patients with previously unknown cancers [10, 11].
Treatment decisions involve an assessment of the functional status of the patient to withstand treatment and estimation of prognosis. The Karnofsky performance scale (KPS) is a well-established method for standardizing performance assessment [12], and based on the KPS and additional clinical data, the Radiation Therapy Oncology Group (RTOG) has published a series of tools for prognostic determination in patients with BM. Initially, the Graded Prognostic Assessment (GPA) scale classified patient survival into four prognostic groups regardless of BM origin [13]. GPA was then refined to Diagnosis-Specific GPA (DS-GPA), which separately classify BM according to its five main primary foci [14]. For lung cancer, GPA underwent two additional updates following incorporation of molecular data to enhance prognostic applications in NSCLC: Lung-molGPA in 2017 [15] and LungGPA in 2022 [16].
However, advances in oncological treatments pioneered in developed countries are often delayed in reaching low- and middle-income countries (LMICs), particularly within the public health system where TKIs, ICIs, RS, and even molecular diagnostics are often routinely unavailable. Multicenter Brazilian data show that only 9.2% of patients have access to EGFR testing in the public health system [17], and 38% of the radiotherapy equipment in public hospitals is considered obsolete [18]. In this study, we comprehensively analyzed patients who underwent surgical excision of brain metastases (BMs) from lung cancer at a public hospital. Our objectives were to assess survival outcomes, examine relevant clinical data associated with survival, and compare observed survival rates with prognostic estimates obtained from established scales.
Material and methods
Study design
This observational, retrospective, monocentric study was conducted at a public tertiary referral center and included consecutive patients who underwent surgical resection for lung cancer brain metastasis between June 2012 and December 2021. The study protocol was approved by the local institutional review board (IRB 4.459.416/2020) and conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from the patients or their relatives, if the patients had died.
Participants
We included 55 patients who underwent surgical resection of BM with an anatomopathological report confirming lung cancer as the primary site. All patients were clinically managed according to local protocols, including administration of dexamethasone for symptom relief, anticonvulsants for seizures, and computed tomography for disease staging or restaging. Surgical procedures were performed by the same team, under general anesthesia. Patients were clinically re-evaluated 2–3 weeks after surgery in an outpatient ambulatory clinic. Missing information on deceased patients was obtained from another regional hospital with the assistance of the authors’ hospital social work support.
Variables and outcomes
Medical charts were reviewed for the extraction of clinical data and retrospective application of functional and prognostic scales, including the KPS and many versions of the GPA, including the GPA [13], DS-GPA [14], Lung-molGPA [15], and Lung-GPA [16].
The following patient data were collected: age, sex, smoking status, clinical symptoms at presentation, number and localization of lesions, previous diagnosis of lung cancer, synchronic metastasis (i.e., in other organs), adjuvant therapy (chemotherapy, radiotherapy, or immunotherapy), histologic classification, and surgical complications. Changes in KPS scores were classified as improved, worsened, or unchanged, by comparing the preoperative and postoperative status. The outcome was survival after the index surgery, and the minimum follow-up period was 1 year.
Statistical analysis
The distribution of data was determined using Shapiro–Wilk or Kolmogorov–Smirnov tests. The Mann–Whitney U test was used to compare independent groups with non-parametric data. For variables with a normal distribution, Student’s t-test was used for group comparisons. For more than two groups, the Kruskal–Wallis test followed by the Dunn test was used for nonparametric data, and the ANOVA test followed by the Bonferroni test was used for parametric data. Correlations between variables were evaluated using the Spearman’s rank correlation coefficient for nonparametric data and Pearson’s test for parametric data. Survival curves were constructed using the Kaplan–Meier model for overall survival (OS) and the Cox model for covariable adjustment. Statistical significance was set at 5%. Analyses were performed using GraphPad v. 9.5.0 (GraphPad Software Inc. San Diego, CA, USA) and SPSS v.24.0.0 (Statistical Package for Social Sciences, IBM Corp., Armonk, NY, USA).
Results
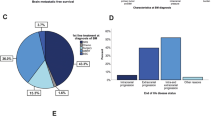
Of the 55 patients, most were male (n = 29, 52.7%) and they had a mean age of 60.9 (± 10.7) years. Of these, 45 (81.8%) of the patients were smokers, and 30 (54.5%) had a single lesion. The frontal lobe was the most common site of BM resection (n = 22, 40.0%), and headache and motor deficits were the most common symptoms (n = 22, 40.0 and n = 20, 36.4%, respectively). Only 13 (23.6%) patients had a history of lung cancer (Table 1). Postoperative chemotherapy and whole-brain radiotherapy were administered to 31 (56.4%) and 28 (50.9%) patients, respectively. Only one patient each underwent stereotactic radiosurgery or received erlotinib, a TKI.
Postoperative complications occurred in 11 (20%) patients including: surgical wound infection (n = 6), cerebrospinal fluid leakage (n = 3), hydrocephalus (n = 2), and intraparenchymal hemorrhage (n = 2). Regarding the postoperative performance status (KPS), 19 (34.5%) patients showed improvement, 20 (36.4%) worsened, and 16 (29.1%) remained unchanged.
Among the prognostic scores that did not utilize molecular information, approximately 10% of the patients each were classified either in the best or worst prognosis groups, respectively, with 80% having intermediate scores. Conversely, in the more recent scores that incorporated molecular data, few or no patients were categorized into the best prognosis groups because molecular investigations were lacking (Table 2).
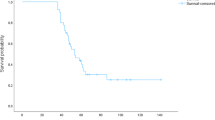
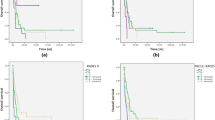
By the end of the follow-up period, only six patients were alive (and only two remained alive beyond 2 years after surgery). Mean survival was 9.3 ± 12 months (min–max: 0.2–76.5, Fig. 1). Univariate analysis revealed that female sex was associated with longer survival (13.6 vs. 5.6 months, p = 0.002). There were no differences in survival with respect to age, smoking status, single metastasis, known primary cancer, postoperative complications, chemotherapy, or radiotherapy. Postoperative performance status was associated with differences in survival; at the mean survival days of 134.3, 270.6, and 443.7 for worsened, unchanged, and improved KPS, respectively (p = 0.002). In Cox regression analysis, differences between the comparison groups also occurred in sex and changes in KPS scores, with longer survival in females and patients with improved postoperative KPS scores (Fig. 1).
Overall survival of patients with surgically removed brain metastasis from lung cancer. Approximately 10% of patients remained alive by the end of the follow-up period. A: Kaplan–Meier survival curve for all patients. B: Cox regression analysis for sex. C: Cox regression analysis for postoperative KPS
The median survival did not differ between the groups classified according to GPA (p = 0.053), Lung-molGPA (p = 0.536), and Lung-GPA (p = 0.660). Using the DS-GPA scale, a significant difference was found in the median survival between the groups (p = 0.021).
Therefore, a survival Cox model was constructed using the following covariates: sex, changes in KPS score, and DS-GPA. In this model, sex was no longer a significant variable for the outcomes (p = 0.243). Higher DS-GPA and improved postoperative KPS scores were significantly associated with longer survival (Table 3).
Discussion
The significant prevalence of lung cancer and its frequent progression to BM, resulting in high mortality rates, have driven significant advancements in the field to enhance patient diagnosis and treatment outcomes. Assessment of prognosis is key to decision-making, especially with the current developments in the understanding of molecular targets of lung cancer and BM. The use of new immunomodulators is changing the life expectancy of these patients; therefore, prognostic assessments are incorporating molecular information. However, routine molecular diagnostics are unavailable in LMICs, and it is unclear whether these updates on prognostic assessment can be reliably used in such settings.
In this study, we found that the OS of patients with lung cancer BM remained short (mean, 9 months), and longer survival is highly associated with higher scores on DS-GPA and improvement in KPS scores after surgery. The classification of our patients according to a more recent prognostic assessment was not helpful in identifying subgroups with longer survival, probably because of the lack of information on the molecular status of the primary tumor, which pushed patient classification to lower grades.
A lack of knowledge of a primary cancer (or a synchronous diagnosis, by some definitions) was observed in 76.4% of our patients and was not associated with a worse prognosis, which is in accordance with most reports [19, 20], despite some disagreement [21]. Chemotherapy and targeted therapy are also associated with better prognosis [21, 22]; however, the former did not show such a relationship in this study.
The observed higher survival rate among female patients, as identified in our study through univariate analysis, aligns with the findings reported in another report focusing on operated BM [23], with statistical significance in multivariate analysis. However, that study included only 41% of patients with lung cancer, accounting for confounding variables. Other studies focusing on lung cancer BM reported on many possible treatment approaches, with only a fraction of surgically managed patients, which adds heterogeneity to interpretation [17, 24].
A KPS score of 70% or above before and after surgery has been associated with lower mortality [19, 20]. Our study showed greater survival with an increase in KPS score postoperatively in patients with BM from lung cancer. Another cohort of neurosurgical patients reported similar findings, albeit with a broader focus on BM originating from various primary diseases [25]. Neurological rehabilitation, adjuvant therapy, and medium- and long-term complications are associated with the functional status and may be responsible for these observed effects. The non-occurrence of surgical complications may be associated with longer survival [19]; however, our complication rate did not differ from that in other reports, and survival was not significantly impaired, as observed by others [26].
Observational surgical studies also point to other prognostic factors such as multiple BM [27], extracranial metastasis, or squamous histology [28], but they are often underpowered. The methodology of recruitment for the RTOG studies, however, allowed them to include much larger groups of participants and analyze the effect of the main prognostic factor on a scale, with survival estimation.
With the continuous evolution of oncological treatment modalities, the integration of molecular data has gained significant relevance in predicting responses to targeted therapy and immunotherapy within the Lung-molGPA and Lung-GPA scales. This inclusion demonstrates a substantial disparity of up to 30 months in the estimated mean survival compared with those of earlier versions of these scales. However, the DS-GPA published in 2012 had the highest similarity of the estimated mean survival with our study, in which a single patient had access to targeted therapy with TKI. With more than 3/4 of our patients without a previous cancer diagnosis, the use of prognostic scales requiring an input of molecular or histological data was impaired.
The scarcity of molecular diagnostic testing [17] and poor radiation therapy infrastructure [18] seen throughout LMICs suggest that our pattern of postoperative care is common and likely has many parallels in less-privileged populations worldwide. Therefore, surgical resection of BM in the context of LMICs plays a key role in treatment, not only for diagnosis and subsequent adjuvant therapy, but also to help increase functionality and survival.
As a retrospective cohort study, the data were registered for other purposes, and the retrospective application of the scales introduced inherent susceptibility to interpretation bias. Despite the relatively small sample size, which is consistent with previous studies, our study maintained the advantage of a more homogeneous population by focusing on a single primary cancer site. Furthermore, a noteworthy strength of our study is the absence of any loss to follow-up, ensuring robust and reliable data integrity. In addition, our study can be used to analyze the real-world conditions and outcomes of a population that may relate to other LMICs, where there are many years of delay in scientific progress to address care in routine clinical practice.
Conclusion
Our study provides a robust analysis of prognostic factors and survival outcomes in a cohort of patients who underwent surgical intervention for lung cancer with brain metastasis at a public tertiary teaching hospital. Our findings underscore the challenging reality of a persistently low OS rate, with an average patient survival of 9.3 months. However, our data revealed crucial determinants of improved survival, including sex and postoperative enhancement in KPS score. Moreover, our comprehensive evaluation of diverse prognostic scales showed that the DS-GPA scale emerged as an unparalleled tool, exhibiting the highest concordance with the observed survival within this cohort. These compelling results not only shed new light on prognostic insights but also offer invaluable guidance for precise patient selection in surgical management.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon request.
References
Baldi I, Engelhardt J, Bonnet C, Bauchet L, Berteaud E, Grüber A, Loiseau H (2018) Epidemiology of meningiomas. Neurochirurgie 64:5–14. https://doi.org/10.1016/j.neuchi.2014.05.006
Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE (2004) Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol 22:2865–2872. https://doi.org/10.1200/JCO.2004.12.149
Nayak L, Lee EQ, Wen PY (2012) Epidemiology of brain metastases. Curr Oncol Rep 14:48–54. https://doi.org/10.1007/s11912-011-0203-y
Porter KR, McCarthy BJ, Freels S, Kim Y, Davis FG (2010) Prevalence estimates for primary brain tumors in the United States by age, gender, behavior, and histology. Neuro Oncol 12:520–527. https://doi.org/10.1093/neuonc/nop066
Gavrilovic IT, Posner JB (2005) Brain metastases: Epidemiology and pathophysiology. J Neurooncol 75:5–14. https://doi.org/10.1007/s11060-004-8093-6
Schouten LJ, Rutten J, Huveneers HA, Twijnstra A (2002) Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer 94:2698–2705. https://doi.org/10.1002/cncr.10541
Cagney DN, Martin AM, Catalano PJ et al (2017) Incidence and prognosis of patients with brain metastases at diagnosis of systemic malignancy: A population-based study. Neuro Oncol 19:1511–1521. https://doi.org/10.1093/neuonc/nox077
Cacho-Díaz B, Lorenzana-Mendoza NA, Chávez-Hernandez JD, González-Aguilar A, Reyes-Soto G, Herrera-Gómez Á (2019) Clinical manifestations and location of brain metastases as prognostic markers. Curr Probl Cancer 43:312–323. https://doi.org/10.1016/j.currproblcancer.2018.06.002
Souza VGP, de Araújo RP, Santesso MR et al (2023) Advances in the molecular landscape of lung cancer brain metastasis. Cancers (Basel) 15:722. https://doi.org/10.3390/cancers15030722
Vogelbaum MA, Brown PD, Messersmith H et al (2022) Treatment for Brain Metastases: ASCO-SNO-ASTRO Guideline. J Clin Oncol 40:492–516. https://doi.org/10.1200/JCO.21.02314
Soffietti R, Abacioglu U, Baumert B et al (2017) Diagnosis and treatment of brain metastases from solid tumors: Guidelines from the European Association of Neuro-Oncology (EANO). Neuro Oncol 19:162–174. https://doi.org/10.1093/neuonc/now241
Vecht CJ, Hovestadt A, Verbiest HB, van Vliet JJ, van Putten WL (1994) Dose-effect relationship of dexamethasone on Karnofsky performance in metastatic brain tumors: A randomized study of doses of 4, 8, and 16 mg per day. Neurology 44:675–680. https://doi.org/10.1212/wnl.44.4.675
Sperduto PW, Berkey B, Gaspar LE, Mehta M, Curran W (2008) A new prognostic index and comparison to three other indices for patients with brain metastases: An analysis of 1,960 patients in the RTOG database. Int J Radiat Oncol Biol Phys 70:510–514. https://doi.org/10.1016/j.ijrobp.2007.06.074
Sperduto PW, Kased N, Roberge D et al (2012) Summary report on the graded prognostic assessment: An accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol 30:419–425. https://doi.org/10.1200/JCO.2011.38.0527
Sperduto PW, Yang TJ, Beal K et al (2017) Estimating survival in patients with lung cancer and brain metastases: An update of the graded prognostic assessment for lung cancer using molecular markers (lung-molGPA). JAMA Oncol 3:827–831. https://doi.org/10.1001/jamaoncol.2016.3834
Sperduto PW, De B, Li J et al (2022) Graded prognostic assessment (GPA) for patients with lung cancer and brain metastases: Initial report of the small cell lung cancer GPA and update of the non-small cell lung cancer GPA including the effect of programmed death ligand 1 and other prognostic factors. Int J Radiat Oncol Biol Phys 114:60–74. https://doi.org/10.1016/j.ijrobp.2022.03.020
Coelho JC, de SouzaCarvalho G, Chaves F et al (2022) Non-small-cell lung cancer with CNS metastasis: Disparities from a real-world analysis (GBOT-LACOG 0417). JCO Glob Oncol 8:e2100333. https://doi.org/10.1200/GO.21.00333
Faroni LD, Rosa AA, Aran V, Ramos RS, Ferreira CG (2021) Access of patients with lung cancer to high technology radiation therapy in brazil. JCO Glob Oncol 7:726–733. https://doi.org/10.1200/GO.20.00622
Antuña AR, Vega MA, Sanchez CR, Fernandez VM (2018) Brain metastases of non-small cell lung cancer: Prognostic factors in patients with surgical resection. J Neurol Surg A Cent Eur Neurosurg 79:101–107. https://doi.org/10.1055/s-0037-1601874
Potthoff AL, Heimann M, Lehmann F et al (2023) Survival after resection of brain metastasis: Impact of synchronous versus metachronous metastatic disease. J Neurooncol 161:539–545. https://doi.org/10.1007/s11060-023-04242-5
She C, Wang R, Lu C et al (2019) Prognostic factors and outcome of surgically treated patients with brain metastases of non-small cell lung cancer. Thorac Cancer 10:137–142. https://doi.org/10.1111/1759-7714.12913
Xu M, Song K, Zhou Z, Yu Z, Lv Y, Xu H (2022) Survival and prognostic factors in patients undergoing the resection of solitary brain metastasis from non-small cell lung cancer: A retrospective cohort study. J Thorac Dis 14:4113–4124. https://doi.org/10.21037/jtd-22-1279
Rotta JM, Rodrigues DB, Diniz JM et al (1992) (2018) Analysis of survival in patients with brain metastases treated surgically: Impact of age, gender, oncologic status, chemotherapy, radiotherapy, number and localization of lesions, and primary cancer site. Rev Assoc Med Bras 64:717–722. https://doi.org/10.1590/1806-9282.64.08.717
Weis LN, Coelho JC, Marks P et al (2016) Non-small lung cancer and brain metastases in Brazil. J Thorac Oncol 11:S204–S205. https://doi.org/10.1016/j.jtho.2016.08.058
Picarelli H, Oliveira ML, Marta GN, Solla DJF, Teixeira MJ, Figueiredo EG (2020) Mortality, morbidity, and prognostic factors in the surgical resection of brain metastases: A contemporary cohort study. J Neurol Surg A Cent Eur Neurosurg 81:279–289. https://doi.org/10.1055/s-0039-1696997
Fuchs J, Früh M, Papachristofilou A et al (2021) Resection of isolated brain metastases in non-small cell lung cancer (NSCLC) patients - Evaluation of outcome and prognostic factors: A retrospective multicenter study. PLOS ONE 16:e0253601. https://doi.org/10.1371/journal.pone.0253601
Huang Y, Chow KKH, Aredo JV, Padda SK, Han SS, Kakusa BW, Hayden Gephart M (2019) Epidermal growth factor receptor mutation status confers survival benefit in patients with non-small-cell lung cancer undergoing surgical resection of brain metastases: A retrospective cohort study. World Neurosurg 125:e487–e496. https://doi.org/10.1016/j.wneu.2019.01.112
Nakao T, Okuda T, Yoshioka H, Fujita M (2020) Clinical outcomes of surgical resection for brain metastases from non-small cell lung cancer. Anticancer Res 40:4801–4804. https://doi.org/10.21873/anticanres.14483
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001.
Author information
Authors and Affiliations
Contributions
Conceptualization: PTHF, PPR. Data curation: FBP, LAR, VGPS. Formal analysis: PTHF. Investigation: FPB, LAR, VGPS, PPR. Project administration: PPR, MAZ, PTHF. Visualization: EOL, ACF, AYF, MAZ. Manuscript draft: FPB. Review and editing: VGPS, PPR, EOL, ACF, AYF, MAZ. Approval of final version: all.
Corresponding author
Ethics declarations
Ethics approval
The study protocol was approved by the local institutional review board (IRB 4.459.416/2020), and conducted in accordance with the Declaration of Helsinki.
Consent
Informed consent was obtained from the patients or their relatives, if the patients had died.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Botta, F.P., Rocha, L.A., de Souza, V.d.G.P. et al. Survival in patients undergoing surgical resection for brain metastasis from lung cancer and utility of different prognostic scales. Neurosurg Rev 46, 184 (2023). https://doi.org/10.1007/s10143-023-02092-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-023-02092-3