Abstract
The introduction of flow diverters (FDs) has represented a paradigm shift in the management of unruptured cerebral aneurysms (UCA). Flow Re-direction Endoluminal Devices (FREDs) and Pipeline Embolization Devices (PEDs) have gained widespread popularity. We aimed to investigate the cumulative incidence of aneurysm occlusion. A total of 195 patients with 199 UCAs were analyzed retrospectively. The outcomes were aneurysmal occlusion during the follow-up, a modified Rankin Scale score of 0–2 at 90 days, additional treatment, major stroke, and steno-occlusive events of FD. Propensity score-matched analysis was performed, controlling for age, sex, aneurysmal size, and location of the internal carotid artery (ICA) aneurysm. Non-ICA aneurysms were excluded from matching. During the follow-up period (median, 366 days), complete and satisfactory aneurysmal occlusions were observed in 128 (68%) and 148 (78%) of 189 UCAs in the unmatched cohort. The 142 (71 each) propensity score-matched cohort was complied. The FRED group had a higher cumulative incidence of ICA aneurysm occlusion (complete: HR 2.7, 95% CI 1.4–5.1, p = 0.0025; satisfactory: HR 2.4, 95% CI 1.1–5.2, p = 0.025). The proportion of additional treatment was significantly smaller in the FRED group (OR 0.077, 95% CI 0.010–0.57, p = 0.0007). Other outcomes showed no significant differences. Propensity score-matched analysis indicated that FRED might have a higher cumulative incidence of aneurysmal occlusion in the treatment of unruptured ICA aneurysms. Whether a cumulative incidence of aneurysmal occlusion may differ by the type of FDs warrants further investigation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The introduction of a flow diverter (FD), an endovascular technique used to treat cerebral aneurysms by reconstructing the parent vessel, has represented a paradigm shift in the management of unruptured cerebral aneurysms (UCA). FDs change the flow dynamics at the interface between the parent artery and the aneurysm, resulting in flow stasis and thrombosis in the aneurysm sac, as well as endoluminal reconstruction of the parent artery by endothelial formation along the FD surface [12, 19]. Although a few studies assessing different FDs have been published [6, 8], the relationship between the time course of follow-up imaging and cumulative incidence of aneurysm closure has not been well documented. In addition, the differences in the treatment results of these FDs remain unknown. This study aimed to compare the clinical and radiological results, including the cumulative incidence of aneurysm closure, in patients with UCA treated with the Flow-Re-direction Endoluminal Device (FRED; MicroVention, Aliso Viejo, California, USA) or the Pipeline Embolization Device (PED; Medtronic Inc., Dublin, Ireland).
Methods
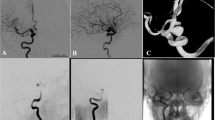
The study was reported based on criteria from the Strengthening the Reporting of Observational Study in Epidemiology statement [23]. The study protocol was approved by the Institutional Ethics Committee (No. 3229). Consent was obtained from all patients. Between December 2015 and January 2022, 1222 patients with 1291 UCAs were treated at our single institute. Among them, 1027 patients with 1092 UCAs did not meet the inclusion criteria (Fig. 1). FD placement was performed by a certificated and experienced neurosurgeon (S.Y). Finally, a total of 195 patients with 199 UCAs treated by FRED or PED were included and retrospectively analyzed.
Clinical data were obtained through a review of the patients’ medical records, such as age, sex, smoking history (never or current/past), daily alcohol consumption, and preoperative modified Rankin scale (mRS) [22]. The following data were also collected: medical history, medications (antiplatelet agents and statins), platelet aggregability, P2Y12 reaction units, aspirin reaction units, aneurysm morphology (location, size, shape, and branches from aneurysm sac, and whether aneurysm was growing), whether UCAs undertook previous treatment, whether the aneurysm was thrombosed, type of FD, and adjunctive coiling. FRED indications were defined as follows: dome size ≥ 5 mm; neck ≥ 4 mm or dome/neck ratio < 2; and aneurysm location from the petrous segment in the internal carotid artery (ICA) to the proximal anterior and middle cerebral artery, basilar artery, and vertebral artery. PED indications were the same as those of FRED except for dome size ≥ 10 mm and aneurysm location from the petrous to superior hypophyseal segments in the ICA. The selection of FRED or PED was at the discretion of the treating physician.
Platelet aggregability (adenosine disphosphate and collagen) was measured and classified into 1 to 9 using aPRP313M platelet aggregation analyzer (TAIYO Instruments, Osaka, Japan) 2 days prior to treatment, and P2Y12 and aspirin reaction units were measured using a Verify system (Accriva Diagnostics, San Diego, CA) on the day of the procedure. If platelet aggregability could not be suppressed sufficiently (value of adenosine disphosphate or collagen 7 to 9), 20 mg prasugrel or 200 mg cilostazole was administered one day before the procedure. If platelet aggregability was too suppressed (value of adenosine disphosphate or collagen 1 to 3), clopidogrel or aspirin dosages were decreased.
Outcomes
The primary and secondary outcome was complete and satisfactory aneurysmal occlusion during the follow-up period. Other secondary outcomes were an mRS score of 0–2 at 90 days and additional treatment for an FD-treated aneurysm. Complete and satisfactory aneurysmal occlusions [9, 17, 18] were defined using the Raymond-Roy occlusion classification [15] I and I/II based on digital subtraction angiography or no apparent aneurysm dome filling and only aneurysm neck filling on magnetic resonance angiography [24], respectively. The mRS score was evaluated at 90 days by telephone interviews with the patient or family members or during a physical examination in those who were able to visit our hospital. The safety outcome was major stroke (≥ 4 points on the National Institutes of Health Stroke Scale) and steno-occlusive events of FD. Safety outcome was evaluated periprocedurally (in-hospital stay) and during follow-up (after hospital discharge).
Statistical analysis
Statistical analyses were performed using JMP Pro (version 15.2; SAS Institute, Cary, NC). Variables were expressed as mean ± standard deviation (SD), median (interquartile range [IQR], 25th–75th percentile), or number of cases (%). Categorical variables were analyzed using Fisher’s exact test. Pearson chi-square tests were used to assess associations between categorical variables, complemented by adjusted residual analysis. The normality of data was evaluated by the Shapiro–Wilk test. Normally distributed continuous variables were compared by the Student t test, whereas non-normally distributed variables were analyzed using the Mann–Whitney U test. Because treatment indication of FRED and PED was different, as stated above, propensity score matching was performed using age, sex, aneurysm size, and internal carotid artery (ICA) aneurysm location. Non-ICA aneurysms were excluded from matching. Because the number of cases with FRED was fewer than those with PED, the cases with PED were matched to those with FRED using a 1:1 matching technique [1, 21].
At first, clinical and radiological characteristics were compared between FRED and PED groups. Second, the Kaplan–Meier method was used to assess the relationship between the time course of the follow-up imaging and the cumulative incidence of complete and satisfactory aneurysmal occlusions by FD type. Differences were considered significant at p < 0.05.
Results
Patient and aneurysm characteristics
One hundred sixty-six patients were female (85%), and the mean age was 62 ± 12 years. A preoperative mRS score of 0 to 2 was observed in 191 patients (98%). Dual antiplatelet agents were prescribed in 178 patients (91%) (aspirin and clopidogrel: 142 (73%), aspirin and prasugrel: 34 (17%), clopidogrel and cilostazol: 2 (1.0%)), and 17 patients (8.7%) took triple antiplatelet agents (aspirin, clopidogrel, and cilostazol: 12 (6.2%), aspirin, prasugrel, and cilostazol: 5 (2.6%)). Fifty-three patients (27%) received statins. Forty-three patients (22%) were administered prasugrel instead of clopidogrel according to values of platelet aggregability. Other patients’ characteristics are shown in Table 1.
The median aneurysm size and neck length were 10 mm (IQR 6.7–15 mm) and 6.3 mm (IQR 4.6–8.2 mm), respectively. Seventeen aneurysms (8.5%) underwent previous treatment; coiling, 10 (5.0%), stent assist coiling, 4 (2.0%), and surgical treatment, 3 (1.5%). Branch from aneurysm sac was observed in 10 (5.1%) aneurysms, and the median procedure time was 74 min (IQR 60–90 min). Other aneurysm characteristics are shown in Table 1.
Unmatched cohort
The proportion of female sex was significantly smaller, and that of smoking history was larger in the FRED group (p = 0.0002 and p = 0.0096). Median P2Y12 reaction units and base value of Verify Now were significantly lower in the FRED group (p = 0.022 and p < 0.0001). The value of platelet aggregability by adenosine diphosphate was significantly higher, and that by collagen was lower in the FRED group (p = 0.036 and p = 0.049). Other patients’ characteristics showed no significant difference between the two groups. The median size of the aneurysm and neck length was significantly smaller in the FRED group (p < 0.0001). The proportion of ICA was significantly smaller, and that of the vertebral artery and basilar artery was larger in the FRED group by residual analysis (p < 0.01). The proportion of saccular aneurysms was significantly smaller in the FRED group (p = 0.0040). Other aneurysm characteristics showed no significant difference between the two groups.
Among 104 PEDs, 9 (8.7%) were PED-shield (Medtronic Neurovascular, Irvine, CA). During the median follow-up period (366 days (IQR 210–552 days)), complete and satisfactory aneurysmal occlusions were observed in 128 (68%) and 148 (78%) of 189 aneurysms, respectively. The median follow-up period was significantly shorter in the FRED group (353 days (IQR 184–403 days) vs. 379 (IQR 358–711) days, p < 0.001). Among the 189 aneurysms, conventional angiography, magnetic resonance angiography, and computed tomography angiography were used for 132 (70%), 54 (29%), and 3 (1.6%) aneurysms, respectively.
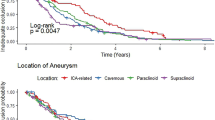
The proportion of complete and satisfactory aneurysmal occlusions showed no significance between the two groups (p = 0.68 and 0.33). The log-rank test revealed that FRED was significantly related to complete and satisfactory aneurysmal occlusions (p < 0.0001 and p < 0.0001). The FRED group had a higher cumulative incidence of complete and satisfactory aneurysm occlusion (complete: HR 3.4, 95% CI 1.8–6.4, p = 0.0001; satisfactory: HR 3.1, 95% CI 1.5–6.4, p = 0.0026) (Table 2).
Other secondary and safety outcomes showed no significant difference between the two groups. The proportion of steno-occlusive events was marginally higher in the FRED group. Major stroke (n = 4) was intraoperative aneurysm rupture (n = 2) and aneurysm rupture after the FD treatment (n = 2), and aneurysm rupture was the cause of mortality.
Propensity score-matched cohort
The median base value of Verify Now and the value of platelet aggregability by collagen were significantly lower in the FRED group (p < 0.0001 and p = 0.0016) (Table 3).
Other patients’ characteristics showed no significant difference between the two groups. Locations of ICA aneurysms were paraclinoid (n = 112, 79%), cavernous (n = 24, 17%), and petrous portion (n = 6, 4.2%). No aneurysm characteristics showed a significant difference between the two groups in a matched cohort.
The proportion of aneurysm occlusion showed no significant difference between the two groups (Table 4).
The log-rank test revealed that FRED was significantly related to complete and satisfactory aneurysmal occlusions (p = 0.0051 and p = 0.0010) (Fig. 2). The FRED group had a higher cumulative incidence of complete and satisfactory aneurysm occlusion (complete: HR 2.7, 95% CI 1.4–5.1, p = 0.0025; satisfactory: HR 2.4, 95% CI 1.1–5.2, p = 0.025). The proportion of additional treatment was significantly smaller in the FRED group (p = 0.0007). Other secondary and safety outcomes showed no differences.
Discussion
To our knowledge, this is the first study to compare two different FDs using the Kaplan–Meier method. The results of the present study indicate that the FRED group had a higher cumulative incidence of complete and satisfactory aneurysm occlusion than the PED group in patients with unruptured ICA aneurysms. Additional treatment was less frequently observed in the FRED group, and no significant differences were identified in the good clinical outcome at 90 days and safety outcomes.
FD type and aneurysm occlusion
FDs provide a non-invasive modality of UCA treatment that is difficult to treat via other endovascular and surgical techniques. Currently, many FDs are available for clinical use. The FRED has a unique structure of dual-layer stents: an outer layer of 16 wires with a higher radial force and an inner layer of 48 wires [13]. The PED is a 48-strand braided mesh that provides 30–35% surface coverage at a nominal diameter.
Aneurysm occlusion by FDs has traditionally been proposed to occur by two main principles: intra-aneurysmal thrombosis via disruption of blood flow and endothelial formation at the aneurysmal neck [7]. As the lower aneurysmal flow velocities were related to shorter occlusion times in FD treatment [4], FRED structure might have an impact on aneurysmal flow velocities. In addition, the spacing between the two layers of FRED could disrupt the flow, increase stasis, trap activated platelets, and serve as a nidus for further thrombus accumulation [5]. Although Szikora et al. observed the lack of intra-aneurysmal thrombosis and endothelial formation in fusiform aneurysms [20], FRED was related to a high cumulative incidence of aneurysm occlusion even at a high proportion of fusiform aneurysm in the FRED group in the present study. Although the proportion of aneurysm occlusion showed no significant difference, FRED may demonstrate a high angiographic occlusion rate at an early stage in patients with unruptured ICA aneurysms.
Hemorrhagic, ischemic, and steno-occlusive events
The incidence of periprocedural and post-operative stroke showed no significant difference between FRED and PED. All steno-occlusive events (n = 4, 2.0%) were observed in the FRED group, and the difference was marginally significant. In this regard, a previous study indicated that the FRED may sometimes be associated with occasional unexplained acute or subacute thromboses unrelated to platelet aggregability, which may be related to the fact that FRED is the device shown to generate significant fibrin and have a greater platelet response [10]. Since there are neither randomized studies nor guidelines on antiplatelet regimens and on testing of individual response to antiplatelet medications during neurovascular procedures, there is currently no standard antiplatelet medication protocol resulting in heterogeneous antiplatelet regimens [11]. Our results showed that some values of Verify Now and platelet aggregability showed differences between patients treated via FRED and PED, but the proportion of switch from clopidogrel to prasugrel was almost similar. Pre-procedural evaluation of Verify Now and platelet aggregation have failed to demonstrate benefits in clinical outcomes in the endovascular treatment of aneurysms [2, 3, 16]. However, as platelet agent administration was modified according to platelet aggregability testing, the rate of major ischemic stroke might be low in the present series.
Limitations
This study has some limitations. First, our study had a retrospective design with inherent limitations leading to potential ascertainment bias, despite the relatively large number of UCA cases treated by FRED and PED. Second, the PED group included two types of PEDs. PED with Shield Technology refers to a surface modification in which a synthetic phosphorylcholine polymer is covalently bonded to the Pipeline braid, which has been shown to decrease thrombogenicity [5, 10, 14]. Because PED with Shield Technology was used in 9 of 104 PED cases (8.7%), this might have influenced the present result even though acceleration of endothelial formation has yet to be clinically demonstrated [19]. Third, as stated above, the indication of FRED and PED differs. Therefore, it was inevitable that there would be residual confounding and selection biases in the comparisons between FRED and PED, even though we constructed propensity score–matched cohorts were constructed to account for the factors associated with the selection of FD. Fourth, the duration of follow-up differed between the two groups. In this regard, aneurysm occlusion was observed early in the FRED group using the Kaplan–Meier method, although the follow-up period was significantly shorter in the FRED group. Fifth, there are institutional differences in indication for each device. Although these differences are partially mitigated by the propensity score matching but not eliminated. Sixth, the generalizability of single-center experiences can be limited due to different populations of patients and different comorbidities. Finally, although a recent study indicated that magnetic resonance angiography can be used as a first-line non-invasive imaging modality during follow-up, especially for patients treated with a PED [24], there is no definitive classification of aneurysm occlusion in FD treatment. As noted above, the results of the present study should be further clarified using an independent cohort.
Conclusion
The present study indicated that FRED might have a higher cumulative incidence of complete and satisfactory aneurysmal occlusions compared to PED, although the proportion of those events showed no significance between FRED and PED in patients with unruptured ICA aneurysms. Whether a cumulative incidence of aneurysmal occlusion may differ by the type of FDs warrants further investigation.
Data availability
The data that support the findings of this study are available from the corresponding author, S.Y., upon reasonable request.
References
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28:3083–3107
Bender MT, Lin LM, Colby GP, Lubelski D, Huang J, Tamargo RJ, Coon AL (2017) P2Y12 hyporesponse (PRU>200) is not associated with increased thromboembolic complications in anterior circulation Pipeline. J Neurointerv Surg 9:978–981
Brasiliense LB, Stanley MA, Grewal SS, Cloft HJ, Sauvageau E, Lanzino G, Miller D, Kallmes DF, Hanel R (2016) Silent ischemic events after pipeline embolization device: a prospective evaluation with MR diffusion-weighted imaging. J Neurointerv Surg 8:1136–1139
Chung B, Mut F, Kadirvel R, Lingineni R, Kallmes DF, Cebral JR (2015) Hemodynamic analysis of fast and slow aneurysm occlusions by flow diversion in rabbits. J Neurointerv Surg 7:931–935
Girdhar G, Andersen A, Pangerl E, Jahanbekam R, Ubl S, Nguyen K, Wainwright J, Wolf MF (2018) Thrombogenicity assessment of pipeline flex, pipeline shield, and FRED flow diverters in an in vitro human blood physiological flow loop model. J Biomed Mater Res A 106:3195–3202
Griessenauer CJ, Enriquez-Marulanda A, Xiang S, Hong T, Zhang H, Taussky P, Grandhi R, Waqas M, Tutino VM, Siddiqui AH, Levy EI, Ogilvy CS, Thomas AJ, Ulfert C, Mohlenbruch MA, Renieri L, Limbucci N, Parra-Farinas C, Burkhardt JK, Kan P, Rinaldo L, Lanzino G, Brinjikji W, Spears J, Muller-Thies-Broussalis E, Killer-Oberpfalzer M, Islak C, Kocer N, Sonnberger M, Engelhorn T, Ghuman M, Yang VX, Salehani A, Harrigan MR, Radovanovic I, Pereira VM, Krings T, Matouk CC, Chen K, Aziz-Sultan MA, Ghorbani M, Schirmer CM, Goren O, Dalal SS, Koch MJ, Stapleton CJ, Patel AB, Finkenzeller T, Holtmannspotter M, Buhk JH, Foreman PM, Cress M, Hirschl R, Reith W, Simgen A, Janssen H, Marotta TR, Dmytriw AA (2021) Comparison of PED and FRED flow diverters for posterior circulation aneurysms: a propensity score matched cohort study. J Neurointerv Surg 13:153–158
Griessenauer CJ, Gupta R, Shi S, Alturki A, Motiei-Langroudi R, Adeeb N, Ogilvy CS, Thomas AJ (2017) Collar sign in incompletely occluded aneurysms after pipeline embolization: evaluation with angiography and optical coherence tomography. AJNR Am J Neuroradiol 38:323–326
Griessenauer CJ, Thomas AJ, Enriquez-Marulanda A, Deshmukh A, Jain A, Ogilvy CS, Kocer N, Engelhorn T, Mohlenbruch M, Holtmannspotter M, Janssen H, Finkenzeller T, Reith W, Sonnberger M, Buhk JH, Schirmer CM, Killer-Oberpfalzer M (2019) Comparison of Pipeline Embolization Device and Flow Re-Direction Endoluminal Device flow diverters for internal carotid artery aneurysms: a propensity score-matched cohort study. Neurosurgery 85:E249–E255
Guimaraens L, Vivas E, Saldana J, Llibre JC, Gil A, Balaguer E, Rodriguez-Campello A, Cuadrado-Godia E, Ois A (2020) Efficacy and safety of the dual-layer flow-diverting stent (FRED) for the treatment of intracranial aneurysms. J Neurointerv Surg 12:521–525
Hagen MW, Girdhar G, Wainwright J, Hinds MT (2017) Thrombogenicity of flow diverters in an ex vivo shunt model: effect of phosphorylcholine surface modification. J Neurointerv Surg 9:1006–1011
Iosif C, Camilleri Y, Saleme S, Caire F, Yardin C, Ponomarjova S, Boncoeur-Martel MP, Mounayer C (2015) Diffusion-weighted imaging-detected ischemic lesions associated with flow-diverting stents in intracranial aneurysms: safety, potential mechanisms, clinical outcome, and concerns. J Neurosurg 122:627–636
Kadirvel R, Ding YH, Dai D, Rezek I, Lewis DA, Kallmes DF (2014) Cellular mechanisms of aneurysm occlusion after treatment with a flow diverter. Radiology 270:394–399
Kocer N, Islak C, Kizilkilic O, Kocak B, Saglam M, Tureci E (2014) Flow Re-direction Endoluminal Device in treatment of cerebral aneurysms: initial experience with short-term follow-up results. J Neurosurg 120:1158–1171
Marosfoi M, Clarencon F, Langan ET, King RM, Brooks OW, Tamura T, Wainwright JM, Gounis MJ, Vedantham S, Puri AS (2018) Acute thrombus formation on phosphorilcholine surface modified flow diverters. J Neurointerv Surg 10:406–411
Mascitelli JR, Moyle H, Oermann EK, Polykarpou MF, Patel AA, Doshi AH, Gologorsky Y, Bederson JB, Patel AB (2015) An update to the Raymond-Roy Occlusion Classification of intracranial aneurysms treated with coil embolization. J Neurointerv Surg 7:496–502
Miller TR, Wessell A, Jindal G, Malhotra A, Simard JM, Gandhi D (2022) The utility of platelet inhibition testing in patients undergoing Pipeline embolization of intracranial aneurysms. J Neurointerv Surg 14(1):neurintsurg-2021-017681. https://doi.org/10.1136/neurintsurg-2021-017681
Piano M, Valvassori L, Lozupone E, Pero G, Quilici L, Boccardi E, Group FIR (2019) FRED Italian Registry: a multicenter experience with the flow re-direction endoluminal device for intracranial aneurysms. J Neurosurg 1–8. https://doi.org/10.3171/2019.1.JNS183005
Pierot L, Spelle L, Berge J, Januel AC, Herbreteau D, Aggour M, Piotin M, Biondi A, Barreau X, Mounayer C, Papagiannaki C, Lejeune JP, Gauvrit JY, Derelle AL, Chabert E, Costalat V (2019) SAFE study (Safety and efficacy Analysis of FRED Embolic device in aneurysm treatment): 1-year clinical and anatomical results. J Neurointerv Surg 11:184–189
Ravindran K, Salem MM, Alturki AY, Thomas AJ, Ogilvy CS, Moore JM (2019) Endothelialization following flow diversion for intracranial aneurysms: a systematic review. AJNR Am J Neuroradiol 40:295–301
Szikora I, Turanyi E, Marosfoi M (2015) Evolution of flow-diverter endothelialization and thrombus organization in giant fusiform aneurysms after flow diversion: a histopathologic study. AJNR Am J Neuroradiol 36:1716–1720
Taniguchi T, Morimoto T, Shiomi H, Ando K, Kanamori N, Murata K, Kitai T, Kawase Y, Izumi C, Miyake M, Mitsuoka H, Kato M, Hirano Y, Matsuda S, Nagao K, Inada T, Murakami T, Takeuchi Y, Yamane K, Toyofuku M, Ishii M, Minamino-Muta E, Kato T, Inoko M, Ikeda T, Komasa A, Ishii K, Hotta K, Higashitani N, Kato Y, Inuzuka Y, Maeda C, Jinnai T, Morikami Y, Sakata R, Kimura T, Investigators CAR (2015) Initial surgical versus conservative strategies in patients with asymptomatic severe aortic stenosis. J Am Coll Cardiol 66:2827–2838
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
Xiang S, Fan F, Hu P, Yang K, Zhai X, Geng J, Ji Z, Lu J, Zhang H (2021) The sensitivity and specificity of TOF-MRA compared with DSA in the follow-up of treated intracranial aneurysms. J Neurointerv Surg 13:1172–1179
Author information
Authors and Affiliations
Contributions
Matsukawa designed the concept, collected the data, analyzed and interpreted the data, drafted the paper, and performed statistical analysis. Uchida performed statistical analysis, contributed to administrative, technical, and material support, and reviewed the submitted version of the manuscript. Rajbhandari collected the data and reviewed the submitted version of the manuscript. Shirakawa contributed to administrative, technical, and material support and reviewed the submitted version of the manuscript. Yoshimura collected the data, designed the concept, interpreted the data, critically revised the paper, supervised, and reviewed the submitted version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study protocol was approved by the institutional ethics committee (No. 3229).
Competing interest
H. Matsukawa received a lecture fee from Daiichi-Sankyo and consulting services fee from B. Braun. K. Uchida received a lecture fee from Daiichi-Sankyo, Bristol-Myers Squibb, Stryker, and Medtronic. S. Yoshimura received a lecture fee from Stryker, Medtronic, Johnson & Johnson, and Kaneka Medics. The remaining authors have no conflicts of interest to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Matsukawa, H., Uchida, K., Rajbhandari, S. et al. Difference in the cumulative incidence of aneurysmal occlusion by Flow Re-direction Endoluminal Device and Pipeline Embolization Device in the treatment of unruptured internal carotid artery aneurysms: a propensity score-matched cohort study. Neurosurg Rev 46, 125 (2023). https://doi.org/10.1007/s10143-023-02026-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-023-02026-z