Abstract
To explore the relationship between postoperative motor deficits and the duration of reduced motor-evoked potentials (MEPs) in patients with middle cerebral artery (MCA) aneurysm. This study included 285 cases of MCA aneurysm treated with clipping surgery with MEP monitoring. The effects of MEP changes on postoperative motor function were assessed, and the key time point for minimizing the incidence of postoperative motor dysfunction was found through receiver operating characteristic (ROC) curve analysis. Motor dysfunction was significantly associated with the occurrence of MEP changes, and patients with irreversible changes were more likely to suffer motor dysfunction than were those with reversible changes. The critical duration of MEP changes that minimized the risk of postoperative motor dysfunction was 8.5 min. This study revealed that MEP monitoring is an effective method for preventing ischemic brain injury during surgical treatment of MCA aneurysm and proposes a critical cutoff for the duration of MEP deterioration of 8.5 min for predicting postoperative motor dysfunction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intracranial aneurysm is defined as a localized dilation of a cerebral arterial wall and occurs in 3–5% of the general population [1, 2]. Aneurysm rupture is the most lethal complication of intracranial aneurysm and the major cause of subarachnoid hemorrhage. Aneurysm ranks as the third leading cause of acute cerebrovascular accidents, behind cerebral thrombosis and hypertensive cerebral hemorrhage, and the relevant mortality and morbidity are still high, even with modern treatment approaches.
Neurosurgical clipping and endovascular coiling are the optimal therapeutic options for intracranial aneurysm currently [2]. However, both therapies are invasive and associated with a high risk of postoperative neurological dysfunction. Previous studies have shown that, compared with coiling, neurosurgical clipping leads to a higher incidence of postoperative neurological deficits, primarily due to ischemic brain injury induced by surgical procedures such as prolonged occlusion or inappropriate retraction [6, 8, 10]. Thus, various assistant techniques have been developed for aneurysm surgery for the purposes of detecting ischemic changes early and adjusting relevant procedures in a timely manner. Intraoperative neurophysiological monitoring (IONM) is one such technique, and multiple studies have verified that IONM parameters including motor-evoked potential (MEP) and somatosensory-evoked potential (SSEP) are useful and reliable for predicting and preventing ischemic brain injury during aneurysm surgery [3, 13]. In general, MEP is considered to offer better diagnostic accuracy than SSEP [15].
The sensitivity of MEP monitoring for detecting decreased cerebral blood flow during aneurysm surgery has been validated previously [4], and a warning criterion based on the decrease in MEP amplitude for predicting postoperative neurological dysfunction also has been established (a decrease in amplitude by more than 50%). In 2019, our research team first proposed a threshold value for the duration of MEP deterioration for predicting postoperative motor deficits in aneurysm patients [9], but it was found to be insufficiently precise. An ideal indicator for predicting postoperative motor deficits must be more individualized according to aneurysm characteristics, for instance, aneurysm location. Logically, we can expect the tolerance time to ischemia to vary among cortices supplied by different arteries, and thus, the threshold value for the duration of MEP deterioration should also differ according to aneurysm location. In the current study, we chose middle cerebral artery (MCA) aneurysm, which is the most common aneurysm type surgically treated in our hospital, as an entry point to investigate the specific association between the duration of MEP deterioration and aneurysm location. The relationship between postoperative motor deficits and the duration of MEP deterioration was explored.
Materials and methods
Patients
A total of 285 cases treated with MCA aneurysm clipping surgery with MEP monitoring by the same neurosurgical team at Beijing Tiantan Hospital from January 2016 to July 2018 were enrolled in the study. Cases were included only if they lacked (1) preoperative motor dysfunction; (2) abnormal preoperative MEP; (3) preoperative seizures, cerebral infarction hemiplegia; and (4) cardiac pacemakers and other metal implants. The study was approved by the ethics committee of our hospital.
All patients provided informed consent for participation in the study.
Anesthesia
Total intravenous anesthesia was generally induced with propofol (150 mg) and sufentanil (25 μg) and maintained with propofol (4–6 mg/kg/h) and remifentanil (0.05–0.2 μg/kg/min). The muscle relaxant cis-acurium bromide (20 mg) was used only during endotracheal intubation and scalp incision. Throughout the operation, the patient’s temperature, blood pressure, heart rate, blood oxygen concentration, partial pressure of carbon dioxide, and other relevant parameters were continuously monitored by the anesthesiologist.
IONM
IONM was performed by one of two experienced IONM technicians, and SSEPs and MEPs of extremities were monitored in all patients. For MEP monitoring, the stimulation sites were C1 (left) and C2 (right) according to the International EEG Electrode Placement 10–20 System Standard, and the recorded sites included the abductor pollicis brevis and abductor hallucis muscles. The stimulation and recording electrodes were corkscrew and needle electrodes, respectively. MEPs were generally obtained by 8-pulse trains, with a stimulus intensity of 100–400 V, a stimulus interval of 50–500 μs, and a stimulus frequency of 250–500 Hz. The band-pass filter range was 30–3000 Hz, with a notch filter at 50 Hz, and the analysis time was 50–100 ms.
MEPs were recorded once after anesthesia and again before opening the dura mater to obtain baseline values. After opening of the dura mater, MEPs were routinely recorded approximately every 5 min and should be recorded more frequently for critical procedures such as temporary occlusion and clip adjustment. A reduction in MEP amplitude by more than 50%, excluding anesthetic and physiological effects, was considered a significant change requiring early warning and intervention. Once a warning is reported, the surgeon should take appropriate measures, such as releasing the temporary occlusion or adjusting the clip placement, to restore MEP amplitude and prevent ischemic injury. Changes in MEPs were subdivided into reversible and irreversible changes based on whether the significant reduction or disappearance of MEP amplitude was restored to more than 50% of the baseline value. For a reversible change, the duration of the MEP change was also recorded.
Clinical evaluation and postoperative follow-up
All patients were followed up at 1 week and 3 months after surgery, and their motor function was evaluated using the Karnofsky Performance Scale (KPS). A higher KPS score indicates a better prognosis, and vice versa. Motor deficits that resolved within 3 months post-surgery were defined as short-term motor dysfunction, whereas those that were not resolved within 3 months after surgery were defined as long-term motor dysfunction. The postoperative evaluation of all patients was performed by two experienced neurosurgeons.
Statistical analysis
All statistical analyses were performed using SPSS software version 22.0 (SPSS Inc., Chicago, IL, USA) and GraphPad Prism (version 8.0.1 for Windows, GraphPad Software, San Diego, CA, USA). Continuous variables were represented as the mean ± standard deviation (SD), and categorical variables were represented as frequency and rate. A p value < 0.05 was considered statistically significant. Chi-square test, Student t test, Mann-Whitney U test, or Fisher exact test were used for comparisons of the two groups, as appropriate.
To further analyze the relationship between postoperative motor dysfunction and the duration of MEP deterioration, receiver operating characteristic (ROC) curve analysis was conducted to determine an optimal duration associated with the minimum probability of postoperative motor dysfunction. The effects of various parameters on motor dysfunction were analyzed by multivariate logistic regression analysis.
Results
Clinical and demographic characteristics of MCA aneurysm patients
MEP changes during surgery for MCA aneurysm repair were observed in 63 (22.11%) patients, whereas no changes in MEP changes were found in 222 (77.89%) patients. The characteristics of the patients categorized according to the occurrence of MEP changes are summarized in Table 1. The gender and age of patients did not differ between the groups, but the incidence of aneurysm rupture was significantly higher among patients with MEP changes. Moreover, the incidence of MEP changes was significantly higher in patients who experienced aneurysm rupture. However, whether the aneurysm ruptured or not had no effect on short-term motor dysfunction (8/42 versus 24/243, p < 0.05 chi-square test) and long-term motor dysfunction (4/42 versus 19/243, p < 0.05 chi-square test).
Among the 63 patients with MEP changes, 49 showed reversible changes and 14 showed irreversible changes. No statistically significant differences in gender, age, or the incidence of aneurysm rupture were observed between patients with reversible and irreversible changes in MEPs (Table 2).
Intraoperative MEP changes and postoperative motor dysfunction
Of the 63 MCA aneurysm patients who experienced significant MEP changes during surgery, 22 (34.92%) had short-term and 16 (25.40%) had long-term motor dysfunction. Of the 222 patients who showed no MEP changes during surgery, 10 (4.50%) had short-term and 7 (3.15%) had long-term motor dysfunction. Overall, patients with intraoperative MEP changes were more likely to suffer short-term and long-term motor dysfunction than those without (p < 0.05 and p < 0.05, respectively, chi-square test, Table 3).
Of the 63 patients with intraoperative MEP changes, 49 showed reversible changes and 14 showed irreversible changes. Among the 49 patients with reversible changes, short-term and long-term motor dysfunction were observed in 11 (22.45%) and 6 (12.24%) patients, respectively. Among the 14 patients with irreversible changes in MEPs, short-term motor dysfunction could be identified in 11 (78.57%) patients, whereas 10 (71.43%) showed long-term motor dysfunction. From these outcomes, patients with irreversible changes were at greater risk for suffering both short-term and long-term motor dysfunction (p < 0.05 and p < 0.05, respectively, chi-square test, Table 4).
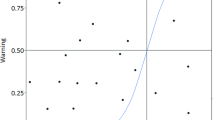
Subsequently, the relationship between the duration of MEP deterioration and postoperative motor deficits was explored in patients with reversible intraoperative MEP changes. In the 11 patients with short-term motor dysfunction, the mean duration of MEP deterioration was 27.64 min (range, 3–97 min), which was significantly longer than that in the 38 patients who did not experience short-term motor dysfunction (7.66 min [range, 1–29 min], p < 0.05, Mann-Whitney U test). From the ROC curve analysis, the critical duration of MEP deterioration for predicting short-term motor dysfunction was determined to be 8.5 min (area under the curve (AUC) = 0.855, 95% confidence interval [CI] 0.699–1.000, Fig. 1a). In the 6 patients with long-term motor dysfunction, the duration of MEP deterioration was also significantly longer than that among the 43 patients without long-term motor dysfunction (26.50 min versus 10.14 min, p < 0.05, Mann-Whitney U test), and the threshold duration of MEP deterioration associated with the minimum risk of long-term motor dysfunction was also 8.5 min (AUC = 0.857, 95% CI 0.740–0.973, Fig. 1b). Among the 49 patients with reversible intraoperative MEP changes, 25 patients experienced intraoperative MEP deterioration for less than 8.5 min. Among these 25 patients, only 1 case (4%) suffered short-term motor dysfunction, which was resolved within 3 months, and none (0%) suffered long-term motor dysfunction. In contrast, among the other 24 patients who experienced intraoperative MEP deterioration for more than 8.5 min, 10 (41.67%) developed short-term motor dysfunction and 6 (25%) suffered long-term motor dysfunction. Thus, the longer duration of MEP deterioration was associated with greater incidence rates of both short-term motor dysfunction (41.67% versus 4%, p < 0.05, chi-square test) and long-term motor dysfunction (25% versus 0%, p < 0.05, chi-square test).
Intraoperative MEP changes and KPS score
KPS scores were compared between the patients with and without intraoperative MEP changes at the 1-week follow-up (short-term) and 3-month follow-up (long-term). At the 1-week follow-up, patients without MEP changes had a significantly higher mean KPS score than those with MEP changes (97.48 ± 10.55 versus 78.25 ± 26.81, p < 0.05, t test, Table 3). At the 3-momth follow-up, the result was the same (98.60 ± 6.48 versus 87.94 ± 20.33, p < 0.05, t test, Table 3). Moreover, patients with reversible MEP changes had a higher KPS than those with irreversible MEP changes at both the 1-week and 3-month follow-ups (p < 0.05 and p < 0.05, respectively, t test, Table 4).
Risk factors for postoperative motor dysfunction
Multivariate binary logistic regression analysis was used to determine whether interoperative MEP deterioration was an independent predictor of the different forms of postoperative dysfunction. The results showed that patients with intraoperative MEP changes had higher risks of short-term motor dysfunction and long-term motor dysfunction than patients without MEP changes. Other factors such as gender, age, and aneurysm characteristics were not found to be independent predictors of postoperative dysfunction. The results are presented in Table 5. For patients with reversible changes in MEP, a duration of MEP deterioration of less than 8.5 min was also an independent predictor of dysfunction compared with a duration of more than 8.5 min (OR 13.88, 95% CI 1.48–130.49, p < 0.05).
Discussion
Relationship between intraoperative MEP changes and postoperative motor dysfunction
Determining the relationship between intraoperative MEP changes and postoperative motor dysfunction was the main research objective of the current study, and the study yielded three results, which follow a progression. First, patients with intraoperative MEP changes had a significantly higher risk of postoperative motor dysfunction than those without, which was not unexpected. Second, patients with irreversible MEP changes were more likely to suffer postoperative motor dysfunction than those with reversible changes, which also was not surprising. Third, a critical threshold value for the duration of MEP deterioration of 8.5 min could minimize the incidence of postoperative motor dysfunction in MCA aneurysm patients, which is established here for the first time and is clinically meaningful.
In the early 1990s, the introduction of multi-pulse electrical stimulation made possible the application of MEP monitoring during surgery for the protection of patients’ motor function. For decades, MEP monitoring has been generally used in a variety of surgery types, including aneurysm surgery, spinal surgery, and carotid endarterectomy, to monitor motor pathway integrity and predict postoperative motor status [9, 11, 14]. MEP changes generally indicate possible ischemia in critical sites (e.g., motor cortex or spinal cord) induced by improper surgical procedures, and thus, could quickly prompt the surgeon to make corresponding countermeasures to change the adverse situation for the purpose of avoiding postoperative dysfunction.
In a study by Szelenyi et al. in 2006, MEP changes were shown to reliably predict postoperative motor deficits, with irreversible changes resulting in postoperative motor dysfunction in all cases (3/3, 100%) and reversible changes also leading to poor motor outcome (3/8, 37.5%) [13]. Consistently, in 2017, Choi et al. reported that 1 patient with irreversible MEP changes (100%) and 2 of 5 with transient MEP changes (40%) experienced postoperative motor dysfunction [3]. In the current study, the incidence rates of postoperative motor dysfunction were 71.4% (10/14) and 12.2% (6/49) in patients with irreversible and reversible MEP changes, respectively. Moreover, patients with irreversible MEP changes experienced markedly worse motility and quality of life than those with reversible MEP changes, according to KPS scores. Notably, our study had a significantly larger sample size than previous studies, which makes the results more generalizable. Overall, the relevant studies to date unanimously indicate that patients with irreversible MEP changes have an increased risk of postoperative motor dysfunction. Jones et al. showed that ischemic infarction occurs when blood flow is reduced to a certain threshold in animal models [7], and Horiuchi et al. suggested that intraoperative MEP monitoring can indicate a lack of cerebral blood flow [5]. Thus, we can infer that irreversible MEP changes indicate a reduction in blood supply so rapid and severe that it cannot be tolerated by the motor cortex and will eventually lead to acute ischemic infarction. In addition, reversible MEP changes may represent an intermediate ischemic state that the motor cortex can tolerate.
However, the extent of the decrease in blood flow is not the only factor that could cause ischemic infarction. The role of the duration of ischemia is also critical. Suzuki et al. reported 4 cases with postoperative motor deficits that showed reversible MEP changes for 8, 10, 12, and 16 min intraoperatively, and these durations were higher than the average MEP deterioration duration in patients without motor dysfunction [12]. Szelenyi et al. found that MEP deterioration for more than 10 min was associated with a high risk of postoperative hemiparesis based on data from 4 patients [13]. Most recently, our research team identified a threshold value (13 min) for the duration of MEP deterioration for predicting postoperative motor deficits in aneurysm patients [9]. By comparison, here we obtained a much shorter critical value (8.5 min) in MCA aneurysm patients. Such results successfully validate our hypothesis that the threshold values for MEP deterioration duration should vary for aneurysms with different locations and characteristics. As the blood supply for the motor cortex is mainly provided by the MCA, the cortex should be less tolerable of ischemia in MCA aneurysm surgery. Additionally, the poor collateral circulation of the MCA should not be ignored, as the ability of contralateral compensation is weak when ischemic injury occurs. Overall, this study expanded our past findings and represents a first step toward an individualized prediction system for postoperative deficits in aneurysm patients.
Limitations
The current study was limited its retrospective nature, and prospective clinical trials should be designed to verify the results.
Conclusion
The results of the current study revealed that MEP monitoring is an effective method for preventing ischemic brain injury during MCA aneurysm surgery and propose a critical value for the duration of MEP deterioration (8.5 min) for predicting postoperative motor dysfunction in MCA aneurysm patients.
References
Brisman JL, Song JK, Newell DW (2006) Cerebral aneurysms. N Engl J Med 355:928–939. https://doi.org/10.1056/NEJMra052760
Chalouhi N, Hoh BL, Hasan D (2013) Review of cerebral aneurysm formation, growth, and rupture. Stroke 44:3613–3622. https://doi.org/10.1161/STROKEAHA.113.002390
Choi HH, Ha EJ, Cho WS, Kang HS, Kim JE (2017) Effectiveness and limitations of intraoperative monitoring with combined motor and somatosensory evoked potentials during surgical clipping of unruptured intracranial aneurysms. World neurosurgery 108:738–747. https://doi.org/10.1016/j.wneu.2017.09.096
Guo L, Gelb AW (2011) The use of motor evoked potential monitoring during cerebral aneurysm surgery to predict pure motor deficits due to subcortical ischemia. Clin Neurophysiol 122:648–655. https://doi.org/10.1016/j.clinph.2010.09.001
Horiuchi K, Suzuki K, Sasaki T, Matsumoto M, Sakuma J, Konno Y, Oinuma M, Itakura T, Kodama N (2005) Intraoperative monitoring of blood flow insufficiency during surgery of middle cerebral artery aneurysms. J Neurosurg 103:275–283. https://doi.org/10.3171/jns.2005.103.2.0275
Hwang JS, Hyun MK, Lee HJ, Choi JE, Kim JH, Lee NR, Kwon JW, Lee E (2012) Endovascular coiling versus neurosurgical clipping in patients with unruptured intracranial aneurysm: a systematic review. BMC Neurol 12:99. https://doi.org/10.1186/1471-2377-12-99
Jones TH, Morawetz RB, Crowell RM, Marcoux FW, FitzGibbon SJ, DeGirolami U, Ojemann RG (1981) Thresholds of focal cerebral ischemia in awake monkeys. J Neurosurg 54:773–782. https://doi.org/10.3171/jns.1981.54.6.0773
Li H, Pan R, Wang H, Rong X, Yin Z, Milgrom DP, Shi X, Tang Y, Peng Y (2013) Clipping versus coiling for ruptured intracranial aneurysms: a systematic review and meta-analysis. Stroke 44:29–37. https://doi.org/10.1161/STROKEAHA.112.663559
Li Z, Fan X, Wang M, Tao X, Qi L, Ling M, Guo D, Qiao H (2019) Prediction of postoperative motor deficits using motor evoked potential deterioration duration in intracranial aneurysm surgery. Clinical neurophysiology : official journal of the International Federation of Clinical Neurophysiology 130:707–713. https://doi.org/10.1016/j.clinph.2019.02.010
Lindgren A, Vergouwen MD, van der Schaaf I, Algra A, Wermer M, Clarke MJ, Rinkel GJ (2018) Endovascular coiling versus neurosurgical clipping for people with aneurysmal subarachnoid haemorrhage. Cochrane Database System Rev 8:CD003085. https://doi.org/10.1002/14651858.CD003085.pub3
Malcharek MJ, Hesse J, Hesselbarth K, Thoma K, Wegner C, Sablotzki A, Hennig G, Gille J (2019) Warning criteria for MEP monitoring during carotid endarterectomy: a retrospective study of 571 patients. J Clin Monit Comput:1–7. https://doi.org/10.1007/s10877-019-00345-5
Suzuki K, Kodama N, Sasaki T, Matsumoto M, Konno Y, Sakuma J, Oinuma M, Murakawa M (2003) Intraoperative monitoring of blood flow insufficiency in the anterior choroidal artery during aneurysm surgery. J Neurosurg 98:507–514. https://doi.org/10.3171/jns.2003.98.3.0507
Szelenyi A, Langer D, Kothbauer K, De Camargo AB, Flamm ES, Deletis V (2006) Monitoring of muscle motor evoked potentials during cerebral aneurysm surgery: intraoperative changes and postoperative outcome. J Neurosurg 105:675–681. https://doi.org/10.3171/jns.2006.105.5.675
Thirumala PD, Crammond DJ, Loke YK, Cheng HL, Huang J, Balzer JR (2017) Diagnostic accuracy of motor evoked potentials to detect neurological deficit during idiopathic scoliosis correction: a systematic review. J Neurosurg Spine 26:374–383. https://doi.org/10.3171/2015.7.SPINE15466
Thomas B, Guo D (2017) The diagnostic accuracy of evoked potential monitoring techniques during intracranial aneurysm surgery for predicting postoperative ischemic damage: a systematic review and meta-analysis. World Neurosurg 103(829–840):e823. https://doi.org/10.1016/j.wneu.2017.04.071
Funding
This work was supported by Capital Foundation of Medical Developments, grant number 2018-2-1075, Principle Investigator: Professor Hui Qiao.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The current study was approved by the ethical committee of our hospital.
Informed consent
Informed consent was obtained for all enrolled patients.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dongze Guo and Xing Fan are co-first authors.
Rights and permissions
About this article
Cite this article
Guo, D., Fan, X., You, H. et al. Prediction of postoperative motor deficits using intraoperative motor-evoked potentials in middle cerebral artery aneurysm. Neurosurg Rev 44, 495–501 (2021). https://doi.org/10.1007/s10143-020-01235-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-020-01235-0