Abstract
The use of intraoperative MRI (iMRI) increases extent of resection in transsphenoidal pituitary surgery. Microsurgical and endoscopic techniques have been established as equal and standard surgical methods. The object of the current study was to evaluate the additional value of iMRI for resection of invasive pituitary adenomas. We conducted a retrospective monocenter study of all consecutive patients treated with invasive pituitary adenomas graded as Knosp III-IV at our department after the introduction of iMRI in 2008. Out of 315 transsphenoidal surgeries for pituitary adenomas, 111 met the criteria for analysis. Patients treated with endoscopic or microsurgical technique were included. iMRI was performed at surgeons’ discretion, when maximal safe resection was assumed. Detailed volumetric tumor analysis using semiautomatic segmentation software (Brainlab Elements) before surgery, during surgery, and after surgery was performed. Additionally, demographic data, additional resection, endocrinological outcome as well as complications were evaluated. Postoperative tumor volume as measured in the follow-up MRI 3 months after surgery was significantly lower compared with intraoperative tumor volume (p < 0.001). The difference was statistically significant for both surgical techniques (p < 0.001). No significant difference was found between both techniques in intraoperative and postoperative tumor volume (p = 0.395 and p = 0.329 respectively). Additional tumor resection was performed in 56 cases (50.5%). We found no significant difference between microsurgical and endoscopic techniques regarding additional resection after iMRI (p = 0.512). New diagnosed permanent diabetes insipidus was found in 10 patients (10.5%, 10/95). New hypopituitarism was seen in 22.1% (21/95) cases and according to multivariate logistic regression was significantly associated with microsurgical technique (p = 0.035). Visual improvement was achieved in 76.8% (N = 53/69, p < 0.001) of patients with visual impairment before surgery. Revision surgery as the consequence of cerebrospinal fistula was performed in eight cases (7.2%). Meningitis was documented in three patients (2.7%). One patient died as a consequence of intraoperative vascular injury. Intraoperative MRI after maximal safe resection significantly improves the overall extent of resection in invasive pituitary adenomas independent of the surgical technique employed. Simultaneously, iMRI-assisted transsphenoidal surgery results in excellent visual recovery with low-risk profile for surgical complications for both endoscopic as well as microsurgical technique. Endoscopic technique might be related to the lower incidence of new hypopituitarism after surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Invasion into cavernous sinus is a relevant independent negative prognostic factor for gross total resection (GTR) and recurrence in pituitary adenomas surgery [10, 13, 14]. Since GTR is related to the longer progression-free survival (PFS), different visualization techniques have been established to achieve this goal [21]. Intraoperative MRI (iMRI) is routinely available at many centers. Schwartz et al. showed that iMRI and endoscopy have a complementary role in transsphenoidal surgery [18].
The endoscopic technique became more common in the transsphenoidal pituitary surgery in the last two decades and lead to the development of extended midline approaches, which allow resection of tumors beyond the classic microsurgical corridor [17]. Nevertheless, our previously published data suggest that the routine use of iMRI might lead to a larger extent of resection (EoR) in microsurgical as well as in endoscopic resection of pituitary adenoma [6]. GTR is challenging in invasive pituitary adenomas and often tumor remnants are unachievable even with endoscopic technique. iMRI might help to define resectable tumor borders which are sometimes not clear during primary resection in invasive growing adenomas.
In this study, we have evaluated the influence of iMRI on EoR in transsphenoidal pituitary surgery of invasive adenomas graded as Knosp III and IV. Furthermore, we have compared iMRI-assisted endoscopic and iMRI-assisted microsurgical technique, which was for invasive adenomas according to our knowledge not published so far. Demographic data, surgical technique, residual tumor volume in iMRT and 3 months after surgery as well as complications and pituitary function were involved in the analysis.
Methods
Patients and follow-up
Patients treated at our center between 2008 and 2018 were assessed retrospectively. Invasive pituitary adenomas were graded according to criteria published by Knosp et al [10]. Adenomas graded Knosp III-IV were included in the further analysis. Invasion of the cavernous sinus on preoperative MRI images was used for the stratification. Invasion of the sphenoid sinus only was not a criterion of tumor invasiveness. Follow-up assessment was performed up to 3–12 months after surgery including clinical and endocrine evaluation. Endocrine function was evaluated in cooperation with endocrinologists in multidisciplinary approach before and after surgery. Preservation, worsening, or improvement of pituitary function were reexamined in 4–6 weeks and in 3–6 months after surgery. Additionally, to the monitoring of baseline pituitary hormone levels, hypoglycemic test was commonly used for determination of cortisol and GH dynamics. For statistical analysis, new hypopituitarism was defined as worsening of endocrine function of one or more pituitary axes after surgery. Additionally, new permanent diabetes insipidus was involved as an additional parameter in the analysis. Despite relatively low number of functional adenomas, remission in patients with acromegaly was defined as a normal IGF-1 level and either suppressed GH less than 0.4 ng/ml during an oral glucose tolerance test or GH level less than 1.0 ng/ml in random examination. Remission in Cushing disease was defined either if cortisol substitution was necessary or if morning cortisol level was within normal range with positive suppression after low-dose dexamethasone exposure. Furthermore, visual deficit due to chiasm compression was documented before surgery. Visual field testing was done regularly before and after the surgery. Improvement, stable state and worsening of visual alterations were evaluated.
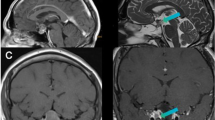
OR setup and MRI
An intraoperative 1.5 T MRI Espree scanner is available (Espree, Siemens AG, Erlangen, Germany) at our department as a one-room solution since October 2008. The analysis of intraoperative residual tumor was performed on thin slice (2 mm) high-resolution coronar and sagittal T2 and contrast-enhanced T1 images using Brainlab Elements software (BrainLab AG, Feldkirchen, Germany). Postoperative MRI was performed 3 months after surgery. Pre- and postoperative MRI images were performed either with the intraoperative scanner or with 1.5 T MRI Symphony system (Siemens AG, Erlangen, Germany).
MRI volumetric assessment
Preoperative MRI images included coronar T2-weighted turbo spin echo as well as coronar and sagittal T1 plain and contrast-enhanced sequences. Tumor volume was measured after image fusion using the above-mentioned software. Tumor borders were segmented semiautomatically on coronar and sagittal T2 and T1 images with gadolinium enhancement. Intraoperative MRI image data as well as MRI data 3 months after surgery were used for the analysis. In case tumor remnants were difficult to evaluate, additional MRI images 1 year after the surgery were analyzed. GTR was defined if no tumor-suspected remnants were found.
Surgical procedure
Endoscopic transsphenoidal approach has been performed by two neurosurgeons at our clinic since 2015. Binasal transsphenoidal approach has been performed in all endoscopic cases. Rigid 0°, 30°, and 45° endoscopes with four hands technique and navigation system were used intraoperatively. In the case of invasive adenomas with skull-base infiltration extended endoscopic approaches in cooperation with ENT surgeons was performed. Skull base reconstruction was performed with fibrin-coated sponge in the case of small or no intraoperative cerebrospinal fluid leak (CSF). Large defects were sealed using multilayer technique with abdominal subcutaneous fat graft and fibrin coated sponge or a Hadad flap according to the internal protocol. [8] Transsphenoidal microsurgical adenomectomy was performed by four experienced neurosurgeons. The microsurgical procedure was performed with unilateral transnasal paraseptal approach.
Surgical complications
Postoperative meningitis was assumed when antibiotic treatment was initiated because of typical clinical signs of meningeal inflammation even if no pathogen was isolated. CSF fistula was considered a complication if a lumbar drain not related to surgical procedure or revision surgery was necessary. Furthermore, intra- and postoperative bleeding, thromboembolic complications and permanent or transient new neurological deficits were included.
Data analysis
Statistical analysis was performed using SPSS 21.0 (Lead Technologies, INC, Charlotte, USA). Descriptive statistics as well as Mann–Whitney U, Wilcoxon, and Fisher exact tests were used for the analysis. Multivariate regression model for new hypopituitarism after surgery was built. Influencing variables were preoperative tumor volume, surgical technique, additional resection, age, and recurrent surgery. The study was conducted according to the international Declaration of Helsinki. The approval of the local ethic committee has been obtained (Nr.365/18).
Results
General characteristics
Out or 315 transsphenoidal iMRI-assisted surgeries, 119 surgeries treating invasive growing pituitary adenoma were identified. Patients who underwent transcranial surgery or endoscopic-assisted microsurgical resection were excluded from the analysis. A total number of 111 transsphenoidal surgeries were finally enrolled in the study. Demographic data are summarized in Table 1. Most patients were males treated for symptomatic non-functioning pituitary adenoma (Table 1).
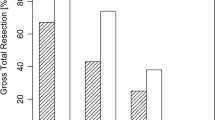
Extent of resection
The mean initial tumor volume is summarized in Table 1 and was slightly higher in the microsurgical cohort but without significant difference if compared to endoscopic cohort (p = 0.885). We found significant difference between tumor volume after primary resection measured by iMRI and tumor volume found in 3 months follow up (p < 0.001, Table 2, Figs. 1, 2). Furthermore, the significant difference was achieved independent of the surgical technique employed (Table 2). Additional tumor resection was performed in more than half of procedures (Table 2). Interestingly, we identified no significant difference in additional resection between both surgical techniques (Table 2). Considering EoR before intraoperative MRI scanning, GTR was achieved in almost 1/3 of all cases and additional GTR rate was significantly improved after additional tumor resection following iMRI scanning (Table 2). Finally, EoR was evaluated separately for both surgical techniques, and no significant difference of tumor volumes in intraoperative and postoperative measurements was found between the techniques (Table 2and Fig. 2). Interestingly, in the subgroup analysis of patients without additional tumor resection with intraoperative tumor remnant, we found significantly lower tumor volume in the follow-up MRI scans (p = 0.001).
Endocrine outcome
Only patients with systematic endocrine evaluation were analyzed. Based on that 95 patients were enrolled in the final analysis. Hypopituitarism affecting one or more pituitary axes prior to surgical treatment was documented in 61/109 patients (56%). New hypopituitarism was documented in 22.1% (N = 21/95) cases and was significantly associated with microsurgical technique (p = 0.035). The statistical significance was confirmed by multivariate regression analysis (p = 0.039, OR 3.5, CI95% 1.066–11.409) Newly diagnosed permanent diabetes insipidus (DI) was found in 10.5% (N = 10) and was significantly higher in patients treated by microsurgical technique (N = 9, p = 0.033). Considering functioning adenomas, only one patient with acromegaly (1/12, 8.3%) presented with remission after surgery according to the defined criteria. Two patients could not be enrolled in the analysis due to incomplete data. In the subgroup analysis of patients with permanent DI in 80% (N = 8), Knosp IV grade was present, and 40% (N = 4) were recurrences. Furthermore, 80% (N = 8) of patients in this cohort had partial or complete pituitary insufficiency before surgery. Mean tumor volume in this cohort was quite large with 14.3 cm3 (range 4.0–29.1 cm3), and mean age was 63 years (range 50–72 years). All tumors in this cohort were non-functioning adenomas.
Visual impairment and outcome
Considering visual deficits, 69 patients presented with visual disturbances related to chiasm compression prior to surgical treatment. Visual improvement was achieved in 76.8% (N = 53, p < 0.001) We found no significant difference in regard to surgical technique (p = 0.565). In one case (0.9%) visual impairment developed after surgery.
Complications
Revision surgery as the consequence of cerebrospinal fistula was performed in eight cases (7.2%). No statistically significant difference was found between microsurgical (N = 4, 6.1%) and endoscopic (N = 4, 8.9%) technique. Meningitis was observed in three cases (2.7%). One patient suffered permanent palsy of oculomotor nerve (0.9%) after surgery, and in one case, hydrocephalus was noted and needed additional treatment. Pulmonary embolism without hemodynamic effect treated with anticoagulation occurred in two cases (1.8%). One patient died as the consequence of intraoperative vascular injury.
Discussion
The focus of our study was to analyze the influence of iMRI on the EoR as well as its influence on further complications and endocrine outcome in the surgical treatment of invasive pituitary adenomas. According to our results, iMRI significantly increases EoR of invasive pituitary adenomas independently of the surgical technique employed. Furthermore, we demonstrated that patients treated by iMRI-assisted endoscopic approach suffer less often from new hypopituitarism or diabetes insipidus after surgery. Our study group has already postulated this tendency in an earlier publication, though there we could analyze only a small number of patients graded Knosp III and IV. [15] Based on our data, we decided to extend the former analysis and focus on invasive adenomas and could confirm this trend as well as the low risk for complications resulting from iMRI or surgery itself on a significantly larger patient sample.
Despite the benign nature of pituitary adenomas, the recurrence rate in published long-term series with up to 20% is relatively high. Furthermore, the recurrent adenomas typically show more aggressive growth pattern with infiltration of parasellar structures. From that point of view, the maximal safe resection is of utmost importance in order to reduce additional treatments and enable safer radiation therapy if necessary [16]. Moreover, there are implications in the literature that GTR is associated with postoperative recovery of hypopituitarism. [2, 22] Furthermore, Sylvester et al. showed that GTR is related to longer PFS and simultaneously iMRI-assisted endoscopic resection resulted in significantly improved EoR compared with microsurgical technique [21]. Our results advocate that the routine use of iMRI might help to achieve higher EoR in invasive adenomas graded Knosp III and IV. Interestingly, according to our data, this advantage persists even if endoscopic technique is used. Endoscopy became more common in the pituitary adenoma surgery [9, 17]. One advantage of this technique is better visualization of intra-, supra- ,and partially even parasellar structures [9, 17]. Nevertheless, complex structure and altered anatomy in the case of invasive pituitary adenomas might lead to difficult anatomical orientation. iMRI seems to help to identify the surgically resectable tumor and results in better EoR. Additionally, iMRI allows intraoperative upgrade of the navigation which helps to improve the orientation if anatomical landmarks are not clear. iMRI became more common in the surgical treatment of pituitary adenomas. Zaidi et al. confirmed recently that iMRI results in higher GTR rates. [23] If compared with our study, only 27 patients without focus on invasive adenomas were analyzed in this study. Similarly, Serra et al. showed on 50 patients harboring pituitary adenoma that iMRI increases EoR rates and decrease tumor remnants. In contrast to our study, only 16 patients with invasive adenomas graded with Knosp 3 and 4 were evaluated. [19] Finally, Buchfelder et al. confirmed these results recently, reviewing the literature dealing with iMRI-assisted resection of pituitary adenomas [4].
Considering invasive pituitary adenomas, we found no significant difference between both surgical techniques in regard to volumetric EoR. iMRI might compensate limitations of microsurgical approach resulting from tubular view as published by our study group [6]. However, the possibility of extended midline approaches is definitely the domain of endoscopy. The primary surgical goal for the treatment of invasive pituitary adenomas is typically maximal safe resection. Complex anatomy and high risk for vascular injury are common limitations of GTRs. While iMRI seems to play a less important role in adenomas graded as Knosp 0–2 treated by endoscopic technique, its value in the resection of invasive adenomas Knosp III-IV is considerably higher. [15] Considering the natural involution of small tumor remnants as proposed by Berkmann et al., we performed a subgroup analysis of patients without additional resection after iMRI despite tumor remnant identified in intraoperative scan and found significantly lower tumor remnant in the follow-up examination [3]. This data confirms results published by Berkmann et al. and might even point out the important role of iMRI in the transsphenoidal pituitary surgery in regard to achieve smaller tumor remnants which are more prone to further involution.
Early and correct identification of pituitary gland is of utmost importance in order to preserve its function. In this regard, iMRI might confirm localization of pituitary gland during surgery if anatomical relations are not clear. Moreover, iMRI could help to predict further functionality of pituitary gland and identify possible intraoperative injuries or other intraoperative complications. Based on our data, we can confirm that endoscopic approach seems to be beneficial for the function of pituitary gland. iMRI and endoscopic technique might have a synergistic effect in this regard. The advantage of endoscopic technique was confirmed even in multivariate logistic analysis. Surgically induced new hypopituitarism rate is documented in the literature between 2.1 and 14.6% [12]. Our incidence of new hormonal deficiency is higher, but we have evaluated selected group of patients with invasive adenomas which are more challenging considering the surgical treatment. Furthermore, they typically reach large volume as confirmed by our data and initial tumor volume is simultaneously an important risk factor for new hypopituitarism after surgery [12]. Considering new diabetes insipidus, our data are comparable with the published literature [12]. Interestingly, similarly as for hypopituitarism, we found that microsurgical technique was associated with much higher rates of postoperative permanent diabetes insipidus than endoscopic technique. In the subgroup analysis of patients with DI, patients with considerably large Knosp IV adenomas dominated as a possible explanation of relatively higher number of DI occurrence. Furthermore, almost half of the patients had tumor recurrence and most of them had complete or some extent of pituitary insufficiency before surgery.
One of the most important indications for the resection of pituitary adenomas are visual disturbances. We can confirm that transsphenoidal pituitary surgery of invasive adenomas results in significant improvement of visual impairment, if it is the consequence of chiasm compression. Simultaneously, we did not find any significant difference between surgical technique used. iMRI leads to higher EoR but its effect on optic function seems to be low because adequate decompression of the optic nerve will mostly be achieved prior to iMRI. Our data indicate that both surgical techniques are adequate for safe and effective decompression of chiasm. Mortini et al. evaluated 788 patients and showed visual normalization in 40.5% and visual improvement in 51.2% after treatment of large invasive adenomas [14]. Our data are congruent, with these results as well as with the current literature [6, 7, 12].
Generally, the risk profile of transsphenoidal pituitary surgery is low as confirmed by our data. Infection rate is very low, despite longer time needed for iMRI-assisted surgery. These findings are congruent with the literature [5, 12, 20]. We did not find other negative effects of longer time needed for anesthesia. Similarly, we did not find any relevant difference considering CSF between microsurgical and endoscopic technique and similar results are comparable with current literature. [1, 11, 14, 17]
Limitations
The retrospective character as well as no comparable cohort treated without iMRI might have biased our data. The availability of iMRI might have led to a change in operative strategy with intraoperative scanning performed before the surgeon would stop the resection were iMRI not available. The number of functioning adenomas is too small to draw any conclusions for this group of patients. A prospective randomized study would be needed to confirm our data.
Conclusion
Intraoperative MRI results in significantly higher EoR in the transsphenoidal pituitary surgery of invasive pituitary adenomas independently of surgical technique. Routine use of iMRI is not related to higher infection rates or other complications and leads to excellent visual improvement in patients with chiasm compression before the surgery. Endoscopic technique might be beneficial for pituitary function but further studies are needed to confirm its potential benefit.
References
Ammirati M, Wei L, Ciric I (2013) Short-term outcome of endoscopic versus microscopic pituitary adenoma surgery: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 84:843–849. https://doi.org/10.1136/jnnp-2012-303194
Bellut D, Hlavica M, Muroi C, Woernle CM, Schmid C, Bernays RL (2012) Impact of intraoperative MRI-guided transsphenoidal surgery on endocrine function and hormone substitution therapy in patients with pituitary adenoma. Swiss Med Wkly 142:w13699. https://doi.org/10.4414/smw.2012.13699
Berkmann S, Schlaffer S, Buchfelder M (2013) Tumor shrinkage after transsphenoidal surgery for nonfunctioning pituitary adenoma. J Neurosurg 119:1447–1452. https://doi.org/10.3171/2013.8.JNS13790
Buchfelder M, Schlaffer S-M (2016) Intraoperative magnetic resonance imaging for pituitary adenomas. Front Horm Res 45:121–132. https://doi.org/10.1159/000442328
Charalampaki P, Ayyad A, Kockro RA, Perneczky A (2009) Surgical complications after endoscopic transsphenoidal pituitary surgery. J Clin Neurosci 16:786–789. https://doi.org/10.1016/j.jocn.2008.09.002
Coburger J, König R, Seitz K, Bäzner U, Wirtz CR, Hlavac M (2014) Determining the utility of intraoperative magnetic resonance imaging for transsphenoidal surgery: a retrospective study. J Neurosurg 120:346–356. https://doi.org/10.3171/2013.9.JNS122207
Dehdashti AR, Ganna A, Karabatsou K, Gentili F (2008) Pure endoscopic endonasal approach for pituitary adenomas: early surgical results in 200 patients and comparison with previous microsurgical series. Neurosurgery 62:1006–1015
Hadad G, Bassagasteguy L, Carrau RL, Mataza JC, Kassam A, Snyderman CH, Mintz A (2006) A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope 116:1882–1886. https://doi.org/10.1097/01.mlg.0000234933.37779.e4
Jho HD, Alfieri A (2001) Endoscopic endonasal pituitary surgery: evolution of surgical technique and equipment in 150 operations. Minim Invasive Neurosurg 44:1–12. https://doi.org/10.1055/s-2001-13590
Knosp E, Steiner E, Kitz K, Matula C (1993) Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33:610–617 – discussion 617–8
Komotar RJ, Starke RM, Raper DMS, Anand VK, Schwartz TH (2011) Endoscopic endonasal compared with microscopic transsphenoidal and open transcranial resection of giant pituitary adenomas. Pituitary 15:150–159. https://doi.org/10.1007/s11102-011-0359-3
Magro E, Graillon T, Lassave J, Castinetti F, Boissonneau S, Tabouret E, Fuentes S, Velly L, Gras R, Dufour H (2016) Complications related to the endoscopic endonasal transsphenoidal approach for nonfunctioning pituitary macroadenomas in 300 consecutive patients. World Neurosurg 89:442–453. https://doi.org/10.1016/j.wneu.2016.02.059
Micko ASG, Wöhrer A, Wolfsberger S, Knosp E (2015) Invasion of the cavernous sinus space in pituitary adenomas: endoscopic verification and its correlation with an MRI-based classification. J Neurosurg 122:803–811. https://doi.org/10.3171/2014.12.JNS141083
Mortini P, Losa M, Barzaghi R, Boari N, Giovanelli M (2005) Results of transsphenoidal surgery in a large series of patients with pituitary adenoma. Neurosurgery 56:1222–1233. discussion 1233. https://doi.org/10.1227/01.NEU.0000159647.64275.9D
Pala A, Knoll A, Brand C, Etzrodt-Walter G, Coburger J, Wirtz CR, Hlavac M (2017) The value of intraoperative MRI in endoscopic and microsurgical transsphenoidal pituitary adenoma resection. World Neurosurgery 102:144–150. https://doi.org/10.1016/j.wneu.2017.02.132
Pomeraniec IJ, Dallapiazza R, Xu Z, Jane J, Jane J Jr, Sheehan JP (2015) 115 early vs late gamma knife radiosurgery following transsphenoidal resection for nonfunctioning pituitary macroadenomas. Neurosurgery 62:202. https://doi.org/10.1227/01.neu.0000467077.55355.a9
Schaberg MR, Anand VK, Schwartz TH, Cobb W (2010) Microscopic versus endoscopic transnasal pituitary surgery. Curr Opin Otolaryngol Head and Neck Surg 18:8–14. https://doi.org/10.1097/MOO.0b013e328334db5b
Schwartz TH, Stieg PE, Anand VK (2006) Endoscopic transsphenoidal pituitary surgery with intraoperative magnetic resonance imaging. Oper Neurosurg 58:ONS–44–ONS–51. https://doi.org/10.1227/01.NEU.0000193927.49862.B6
Serra C, Burkhardt J-K, Esposito G, Bozinov O, Pangalu A, Valavanis A, Holzmann D, Schmid C, Regli L (2016) Pituitary surgery and volumetric assessment of extent of resection: a paradigm shift in the use of intraoperative magnetic resonance imaging. Neurosurg Focus 40:E17. https://doi.org/10.3171/2015.12.FOCUS15564
Starke RM, Raper DMS, Payne SC, Vance ML, Oldfield EH, Jane JA (2013) Endoscopic vs microsurgical transsphenoidal surgery for acromegaly: outcomes in a concurrent series of patients using modern criteria for remission. J Clin Endocrinol Metab 98:3190–3198. https://doi.org/10.1210/jc.2013-1036
Sylvester PT, Evans JA, Zipfel GJ, Chole RA, Uppaluri R, Haughey BH, Getz AE, Silverstein J, Rich KM, Kim AH, Dacey RG, Chicoine MR (2015) Combined high-field intraoperative magnetic resonance imaging and endoscopy increase extent of resection and progression-free survival for pituitary adenomas. Pituitary 18:72–85. https://doi.org/10.1007/s11102-014-0560-2
Webb SM, Rigla M, Wägner A, Oliver B, Bartumeus F (1999) Recovery of hypopituitarism after neurosurgical treatment of pituitary adenomas. J Clin Endocrinol Metab 84:3696–3700. https://doi.org/10.1210/jcem.84.10.6019
Zaidi HA, De Los Reyes K, Barkhoudarian G, Litvack ZN, Bi WL, Rincon-Torroella J, Mukundan S, Dunn IF, Laws ER (2016) The utility of high-resolution intraoperative MRI in endoscopic transsphenoidal surgery for pituitary macroadenomas: early experience in the advanced multimodality image guided operating suite. Neurosurg Focus 40:E18. https://doi.org/10.3171/2016.1.FOCUS15515
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was conducted according to the International Declaration of Helsinki. The approval of the local ethics committee has been obtained (Nr.365/18).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hlaváč, M., Knoll, A., Etzrodt-Walter, G. et al. Intraoperative MRI in transsphenoidal resection of invasive pituitary macroadenomas. Neurosurg Rev 42, 737–743 (2019). https://doi.org/10.1007/s10143-019-01102-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-019-01102-7