Abstract
The radiofrequency treatment (RFD) for sacroiliac joint pain (SIP) is well-established, but there is still scarce evidence on its clinical outcome. The classical monopolar RFD is limited by a high recurrence rate. This might be caused by an incomplete denervation of the dorsal rami. The Simplicity III probe was invented to optimise pain fibre recruitment by its multi-electrode design. However, the clinical superiority of this procedure was never proven. The aim of this study was to illustrate the effectiveness of RFD and to compare both denervation techniques. One hundred twenty-one patients were included, and their clinical course was analysed. Fifty-seven patients received conventional treatment with multiple percutaneous monopolar RFDs (monolesion probe group, MoLG) and 64 patients with the Simplicity III probe (multilesion probe group, MuLG). All patients were followed 1, 3, 6 and 12 s after RFD. Clinical outcome scores were analysed (numeric pain rating scale (NPRS), Roland-Morris Disability Questionnaire, Oswestry Disability Index (ODI), Odom’s criteria, Short Form 36 score). The MuLG showed a clearly advanced improvement concerning the clinically relevant pain relief (≥ 50%) (1 month/3 months /6 months/12 months = 72%, 55%, 36%, 27% vs. 1 month/3 months/6 months/12 months = 39%, 28%, 16%, 11%) as well as an advanced improvement of pain-associated disability and a higher satisfaction rating compared to the MoLG (NPRSMuLG_preop = 8,3; NPRSMuLG_12months = 5.8; NPRSMoLG_preop = 7,7; NPRSMoLG_12months = 5.8; ODIMuLG_preop = 52; ODIMuLG_12months = 42; ODIMoLG_preop = 52; ODIMoLG_12months = 47; ODOMSMuLG_good/excellent = 54%; ODOMSMoLG_good/excellent = 28%). RFD of the SIP with the Simplicity III probe is effective and delivers a distinct pain reduction even after 1 year of treatment. This technique shows clear advantages compared to the conventional monolesion technique and is a useful treatment for patients with recurrent SIP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sacroiliac joint pain (SIP) comprises about 10–25% of all reasons for low back pain. It can either occur primarily or secondarily, following fusion procedures in the lumbosacral region. In most cases, it can be treated conservatively by physiotherapy treatment and does not need further invasive interventions. If conservative management fails, it is difficult to achieve an adequate pain reduction in the long term. Injections with local anaesthetics and corticoids frequently result in a brief, temporary improvement of symptoms. Surgical approaches are discussed controversially. Based on the current literature and experience, they should only be performed, if extensive conservative treatment fails [10, 13,14,15].
The radiofrequency denervation of the SI joint was developed for mid- to long-term pain reduction of SIP. The conventional technique with several monopolar lesions between the dorsal foramina and the sacroiliac joint under oblique anterior-posterior X-ray is an established procedure. However, there are only a few studies with low patient numbers, which show the clinical outcome after this intervention, and in many cases, the results are not satisfying with about 30–60% success rates after 6 months and even less after 12 months [1, 6, 7]. In contrast to pre-existing literature, a multicentre trial from 2017 showed no effect of sacroiliac joint denervation, not even within the early follow-up time [9]. The Simplicity III probe was developed to guarantee the denervation of all pain fibres arising from the dorsal rami. All other published studies demonstrated a high effectiveness of this denervation technique. Nevertheless, the cost of this denervation is very high, and the placement of the probe is pain-intense due to the periosteal placement. There are only a few studies investigating this denervation technique, and a comparison with the classical monolesion denervation was never performed [2, 8, 12]. The aim of our study was to investigate the outcome of both denervation techniques and to compare those techniques concerning their effectiveness in the long term.
Materials and methods
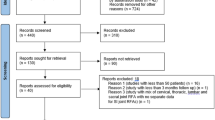
We identified 156 patients with an age of 37–84 years who received an isolated denervation of the sacroiliac joint between 2011 and 2016. All patients suffered from low back pain and presented with pain in the typical area at the lower lumbar spine and gluteal. Inclusion criteria for denervation were a chronic sacroiliac joint pain, which was refractory to conventional pain therapy including physiotherapy, manual therapy and medication with nonsteroidal anti-inflammatory drugs. A certain amount of patients (31%, 37 of 121 patients) received at least one spinal surgery before they developed SIP. Twenty-five patients of these (68%, 25 of 37 patients) received a spinal instrumentation before they developed SIP. All patients received a fluoroscopic guided injection into the sacroiliac joint with local anaesthetic (1 ml Carbostesin 0.5%® or Scandicain® 2%) and 40 mg triamcinolone with additional contrast arthrography, which resulted in a pain reduction of at least 50% on the numeric pain rating scale.
We excluded other sources of low back pain by medical history, physical examinations, x-ray, computed tomography, magnet resonance imaging or myelography and/or different injection techniques. Patients with other sources of low back pain were excluded from our study.
For the sacroiliac joints, a 25-gauge needle was inserted 3 to 10 mm laterally of the sacral foramina S1–3 under fluoroscopy. The correct depth of the needle was confirmed laterally, after which 0.5 ml of 2% lidocaine was injected.
Study design and ethics approval
The prospectively collected data was analysed retrospectively. The ethical approval was given by the local ethics committee (reference number EA2/093/13).
Denervation techniques
For the conventional monopolar denervation, the Neuro N50 system (inomed Medizintechnik GmbH, Emmendingen, Germany) was used. The costs for the new version of this RFD system (LG 2) and a probe for multiple use are 22.676 € in Germany. For every single denervation, a canula (11 €) for insertion of the probe is needed.
For the Simplicity denervation, the NT110 system (Abbott, IL, USA) was used. The costs for the new version of this system (NT2000ix) are 28.500 € in Germany. A Simplicity probe (480 €) is needed for every RFD treatment.
Conventional monolesion SIJ-denervation
The conventional lesions of the dorsal rami were performed with a C-arm in oblique position.
The sacroiliac joint and the dorsal foramen were visualised, and the 18-gauge needle with a length of 100 mm was placed between the dorsal foramen and the SIJ and additionally in the groove between the sacral ala and the superior articular process of S1 to address the dorsal ramus of the nerve root of L5. Local anaesthesia was applied (1 ml Carbostesin 0.5%® or Scandicain® 2%). We performed motor stimulation up to 1.5 V to exclude a motor recruitment of lower extremities. Local anaesthetics were injected, and a monopolar lesion at 85 °C for 60 s was performed.
Denervation in Simplicity technique
The Simplicity denervation was performed in general anaesthesia without relaxation. Two C-arms were used to position the probe. One of the C-arms enabled the anterior-posterior and oblique view, and the other C-arm enabled the lateral view. After disinfection, the percutaneous perforation was located at S4—right below and 1 cm lateral to the posterior foramen. The Simplicity III probe was positioned along the sacral curvature up to the sacral ala (Fig. 1). The three active electrodes should be positioned lateral to the posterior foramen of S1–3 and medial to the SIJ. A motor testing is conducted with up to 3 V at every electrode separately to avoid motor recruitment. Denervation was performed with three monopolar lesions at the single electrodes and two bipolar denervations between the electrodes, 80–85 °C, 60 s each. Afterwards, the probe was removed.
Representative radiographs imaging the placement of the Simplicity III probe. a Anterior-posterior fluoroscopic images illustrate the positioning of the Simplicity III probe on the left side. The probe on the right side is already in the final position. b Anterior-posterior and lateral view showing the final placement of the Simplicity III probe. c Intraoperative 3D O-arm scan showing the ideal location of the Simplicity III probe periosteal and medial to the dorsal edge of the sacroiliac joint
Groups
Patients were divided into two groups according to the RFD technique. Patients, who received a denervation with the classical technique, were assigned to the monolesion probe group (MoLG). Patients, who were treated with the Simplicity technique, were assigned to the multilesion probe group (MuLG).
Clinical outcome measurements
Clinical outcome scores were collected on follow-up appointments in our outpatient department routinely, following our institutional standard protocol.
The patients were examined by a physician in our outpatient department before 1, 3, 6 and 12 months after RFD.
The numeric pain rating scale (NPRS), the Oswestry Disability Index (ODI) and the Roland-Morris Disability Questionnaire (RMDQ) were analysed to evaluate back pain and back pain-related disability.
Moreover, health-related quality of life (HRQOL) was measured with the Short Form 36-item Health Survey Questionnaire (SF-36). To illustrate patient’s satisfaction, Odom’s criteria were evaluated, and the results at the one-year follow up were analysed.
Statistical analysis
The statistical analysis was performed, and graphs were designed using Graphpad Prism 5 (San Diego, CA, USA). After determining the normal distribution and the variances, the Mann-Whitney U test or Student’s t test was performed to compare both groups. To compare mean values at different points in time of each group, ANOVA or Friedman test was conducted. We considered p values below 0.05 as significant.
Results
Out of 156 patients, who received a unilateral (112) or bilateral (44) denervation of the SIJ between 2011 and 2016, 121 completed the regular appointments in our outpatient department and reported their outcome scores. Thirty-five patients were not included in our retrospective analysis, because 26 of them were not living close to the hospital and did not want to attend the regular appointments in our outpatient department, and 9 patients could not be contacted via telephone or mail. Fifty-seven patients received the classical solely monopolar denervation technique (17 with bilateral treatment), and 64 patients received the single strip denervation with the Simplicity III probe (22 with bilateral treatment). All patients that were treated for a recurrent SIJ syndrome before November 2013 received treatment with the classical SIJ denervation technique. Further patients that presented after 2013 received RFD with the Simplicity III probe. The RFD of the MuLG was performed in short general anaesthesia combined with an overnight stay in the hospital.
Both groups have very similar demographic parameters concerning age and gender with a clear female predominance and more than two thirds of women (Table 1).
About 30% suffered from an SIJ pain after spine surgery. Seventy percent suffered from primary SIJ pain (Table 1). In both groups, no complication occurred during or after the procedure or anaesthesia. We found a highly significant difference between the groups concerning x-ray exposure time and operating time in favour of the MuLG (Table 1).
Baseline clinical parameters
The baseline of the clinical parameters measured before treatment was very similar in both groups (NPRSMoLG_preop = 7.7 ± 1.5, NPRSMulG_preop = 8.0 ± 1.2, ODIMoLG_preop = 51.7 ± 9.6, ODIMulG_preop = 51.8 ± 10.4, RMDQMoLG_preop = 15.4 ± 4.8, RMDQMuLG_preop = 16.4 ± 3.3, SF-36MoLG_preop = 27.9 ± 5.9, SF-36MuLG_preop = 28.6 ± 6.6). The scores illustrated no statistical differences (Fig. 2).
Quantification of the outcome scores of the multilesion probe group (MuLG) and the monolesion probe group (MoLG) before treatment and 1, 6 and 12 months after treatment. (values are given as mean ± standard error of the mean (SEM)). a The numeric pain rating scale (NPRS) illustrates an improvement in both groups, but a significant better outcome in the MuLG compared to the MoLG over the entire course. b The Oswestry Disability Index (ODI) shows beneficial result in the MuLG as well with a mean improvement of 10 points after 1 year. c The Roland-Morris Disability Questionnaire illustrates a reduction of pain-associated disability with advantages in the MoLG as well. d Only in the MuLG the denervation resulted in a benefit concerning the health-related quality of life
Clinical outcome parameters
Both groups benefitted from denervation of the SIJ concerning their back pain, back pain-associated disability and quality of life 1 month after RFD. In the course of a year, a clearly beneficial pain score in patients treated with the Simplicity probe was observed, compared to the less successful monolesion approach (Fig. 2a). The RMDQ and the ODI scoring illustrated a superiority of the Simplicity treatment with a significantly better outcome in the whole follow-up course compared to the classic denervation (Fig. 2b, c). This improvement resulted in a significantly higher health-related quality of life even 1 year after RFD in the MuLG only (Fig. 2d). We regarded 50% or more pain relief in the NPRS as a clinical success. This applies to 72% of patients in the MuLG compared to only 39% in the MoLG. Patients of the MuLG were relieved of pain with a reduction of more than 2 points measurable in the NPRS in the course of the total year (Fig. 2). However, a high recurrence was observed in both groups.
Overall, the patient satisfaction 1 year after treatment was considerably higher in the MuLG (Table 1).
Discussion
The main findings of our study are that a radiofrequency denervation of the lateral branches supplying the dorsal part of the SIJ leads to a significant reduction of low back pain or buttock pain in patients with SIP for at least 1 year. However, a high recurrence rate already after 6 months could be illustrated. Patients, who received the RFD with the Simplicity probe, showed an advanced benefit concerning back pain, back pain-associated disability and quality of life compared to the MoLG. Only in the MuLG, a clinically relevant pain reduction (≥ 2 points on the NPRS) lasted for a whole year.
A critical factor for a beneficial outcome in patients with chronic SIP is a conduction of the adequate denervation technique. Very important is a gapless ablation of all nerves arising from the lateral branches of the nerves S1–3 (L5). Therefore, a denervation with the Simplicity III probe is clearly an improvement compared to conventional denervation techniques with a single monolesion probe.
Essential for an adequate performance of articular denervation is the knowledge of the innervation of the treated area. The exact innervation of the SIJ was a matter of discussion for a long time. Many authors suggested that the upper part of the SIJ is frequently innervated by the dorsal rami of L4 and L5, and they claimed to perform a denervation of these nerves additionally to the RFD of the lateral branches of S1–S3 [6, 12]. Cadaveric studies of Roberts et al. determined that the nerves supplying the SIJ from dorso-medial are mainly originating from S1–S3. Only in 8% L5 and in 4% S4 are contributing to the posterior sacral network (PSN), which supplies the dorsal part of the joint. Even if L5 is contributing to the PSN, it firstly unites with the lateral branches of S1 before it joins the PSN [11]. Therefore, L4 does not play any role concerning the innervation of the SIJ, and the L5 dorsal ramus do not need a separated denervation due to its track joining the S1 lateral branch. According to these findings, we did not perform an L5 RFD in the simplicity group and suggested that a S1–S3 RFD results in a complete denervation of the dorsal SIJ. Our encouraging results prove the effectiveness of our technique for the treatment of SIP.
There are many technical approaches to address the SIJ by a denervation of its lateral branches. The most common approaches are the cooled RFD and the classical heated RFD with a monolesion probe [5,6,7]. Some authors performed a stimulation of the pain-associated nerves to optimise the location of denervation [16], but there is no evidence in the literature showing the advantage over nonstimulated approaches. Recently, most of the authors suggest not to select the nerves for denervation, but to technically optimise the completeness of ablation of all lateral branches innervating the dorsal part of the SIJ [6]. Bipolar approaches were invented to increase the likelihood of recruiting all lateral branches. Recently published results are superior to the classical RFD approach in terms of x-ray time, procedure duration and outcome [3]. We present a very simplified approach containing only one probe that enables a gapless denervation by three monopolar radiofrequency ablations and two bipolar ablations resulting in lesions overlapping along the track of the probe. The literature lacks detailed information concerning the advantage of this device compared to the standard denervation techniques.
The outcome of our patient cohort treated with the Simplicity III probe is comparable to the case series reported by Schmidt et al. We could illustrate a reduction of more than 50% back pain relief in the NPRS in 72% of patients 1 month after treatment. The success rate after 6 months was still detectable in 50% of patients. However, a high recurrence rate in the 1-year course is obvious [12]. This can be caused by incomplete ablation, or repair mechanisms like remyelination, collateral sprouting and regeneration of the axons, which result in a reinnervation of the sacroiliac joint [4]. Bellini and Barbieri published extremely positive results describing a significant pain reduction of more than 90% after 1 month, and 36% after one year. After a dramatical, initial relief of pain, they observed a high recurrence rate after 6 and 12 months. Astonishingly, they illustrated a contradictory continuous improvement of pain-associated disability (ODI) in their patient cohort with best scores after 1 year. In our opinion, this is incomprehensible due to the fact that an increase of the NPRS over time always effects the pain-associated disability directly. There was no clarification concerning the patients who received treatment nor an explanation of the discrepancy concerning NPRS and ODI. Hegarty published 12 patients, who received RFD with the Simplicity III probe. He described that his patients benefitted extremely well after one-year follow up compared to previous studies of RFD [8]. He presented a 61% pain reduction after 12 months, and surprisingly, his patients showed a continuous pain improvement over the follow-up course. This continued pain improvement is controversial with regard to the clinical course we determined in our study. We assume that the patients he described were notably younger, did not suffer from advanced degeneration of the SIJ and had no history of spinal surgery, as his manuscript does not contain this information. The patients included in our study represent the very wide range of patients suffering from SIP presenting with back or buttock pain in the outpatient department specialised for spinal diseases. As expected, a significant percentage of our patients have a postsurgical SIP (31%, Table 1).
The need for general anaesthesia combined with higher costs is certainly disadvantages of RFD using the Simplicity III probe. However, it is possible to perform the Simplicity approach with mild sedation in an ambulant setting as well.
The main limitation of our study is the retrospective character. However, we were able to analyse the clinical results of large patient groups compared to previous studies. The patient cohort has a clear female predominance as it is common for patients with SIP [7, 16], and there is a wide range of different ages.
Our study illustrates an improvement of operating time, x-ray time as well as of the clinical outcome 1 year after RFD in patients treated with the multiple lesion probe. This represents a clear advantage compared to a conventional monolesion RFD of the SIJ. However, because of the retrospective character and the low patient numbers, the results have to be considered with caution. The SI joint ablation with the Simplicity probe is simple in use and rarely leads to complications. This denervation technique shows good mid-term results in young patients as well as in old patient with severe degeneration of the SIJ.
References
Aydin SM, Gharibo CG, Mehnert M, Stitik TP (2010) The role of radiofrequency ablation for sacroiliac joint pain: a meta-analysis. PM R 2:842–851. https://doi.org/10.1016/j.pmrj.2010.03.035
Bellini M, Barbieri M (2016) Single strip lesions radiofrequency denervation for treatment of sacroiliac joint pain: two years’ results. Anaesthesiol Intensive Ther 48:19–22. https://doi.org/10.5603/AIT.2016.0004
Cheng J, Chen SL, Zimmerman N, Dalton JE, Lasalle G, Rosenquist R (2016) A new radiofrequency ablation procedure to treat sacroiliac joint pain. Pain Physician 19:603–615
Choi EJ, Choi YM, Jang EJ, Kim JY, Kim TK, Kim KH (2016) Neural ablation and regeneration in pain practice. Korean J Pain 29:3–11. https://doi.org/10.3344/kjp.2016.29.1.3
Cohen SP, Abdi S (2003) Lateral branch blocks as a treatment for sacroiliac joint pain: a pilot study. Reg Anesth Pain Med 28:113–119. https://doi.org/10.1053/rapm.2003.50029
Cohen SP, Hurley RW, Buckenmaier CC, Kurihara C, Morlando B, Dragovich A (2008) Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology 109:279–288. https://doi.org/10.1097/ALN.0b013e31817f4c7c
Ferrante F (2001) Radiofrequency sacroiliac joint denervation for sacroiliac syndrome. Reg Anesth Pain Med 26:137–142. https://doi.org/10.1053/rapm.2001.21739
Hegarty D (2016) Clinical outcome following radiofrequency denervation for refractory sacroiliac joint dysfunction using the Simplicity III probe: a 12-month retrospective evaluation. Pain Physician 19:E129–E135
Juch JNS, Maas ET, Ostelo RWJG, George Groeneweg J, Kallewaard JW, Koes BW, Verhagen AP, Van Dongen JM, Huygen FJPM, Van Tulder MW (2017) Effect of radiofrequency denervation on pain intensity among patients with chronic lowback pain the mint randomized clinical trials. JAMA 318:68–81. https://doi.org/10.1001/jama.2017.7918
Polly DW, Cher DJ, Wine KD, Whang PG, Frank CJ, Harvey CF, Lockstadt H, Glaser JA, Limoni RP, Sembrano JN (2015) Randomized controlled trial of minimally invasive sacroiliac joint fusion using triangular titanium implants vs nonsurgical management for sacroiliac joint dysfunction. Neurosurgery 77:674–691. https://doi.org/10.1227/NEU.0000000000000988
Roberts SL, Burnham RS, Ravichandiran K, Agur AM, Loh EY (2014) Cadaveric study of sacroiliac joint innervation: implications for diagnostic blocks and radiofrequency ablation. Reg Anesth Pain Med 39:456–464. https://doi.org/10.1097/AAP.0000000000000156
Schmidt PC, Pino CA, Vorenkamp KE (2014) Sacroiliac joint radiofrequency ablation with a multilesion probe: a case series of 60 patients. Anesth Analg 119:460–462. https://doi.org/10.1213/ANE.0000000000000282
Smith AG, Capobianco R, Cher D, Rudolf L, Sachs D, Gundanna M, Kleiner J, Mody MG, Shamie AN (2013) Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res 7:14. https://doi.org/10.1186/1750-1164-7-14
Soriano-Baron H, Lindsey DP, Rodriguez-Martinez N, Reyes PM, Newcomb A, Yerby SA, Crawford NR (2015) The effect of implant placement on sacroiliac joint range of motion. Spine (Phila Pa 1976) 40:E525–E530. https://doi.org/10.1097/BRS.0000000000000839
Sturesson B, Kools D, Pflugmacher R, Gasbarrini A, Prestamburgo D, Dengler J (2017) Six-month outcomes from a randomized controlled trial of minimally invasive SI joint fusion with triangular titanium implants vs conservative management. Eur Spine J 26:708–719. https://doi.org/10.1007/s00586-016-4599-9
Yin W, Willard F, Carreiro J, Dreyfuss P (2003) Sensory stimulation-guided sacroiliac joint radiofrequency neurotomy: technique based on neuroanatomy of the dorsal sacral plexus. Spine (Phila Pa 1976) 28:2419–2425. https://doi.org/10.1097/01.BRS.0000085360.03758.C3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bayerl, S.H., Finger, T., Heiden, P. et al. Radiofrequency denervation for treatment of sacroiliac joint pain—comparison of two different ablation techniques. Neurosurg Rev 43, 101–107 (2020). https://doi.org/10.1007/s10143-018-1016-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-018-1016-3