Abstract
The unruptured intracranial aneurysm treatment score (UIATS) was published in April 2015 as a multidisciplinary consensus regarding treatment of unruptured intracranial aneurysms (UIA). As a tertiary center with focus on vascular neurosurgery, we aimed to investigate whether our treatment decision-making in patients with UIA has been in accordance with the recently published UIATS. A retrospective analysis of patients admitted to our center with UIA was performed. UIATS was applied to all identified UIA. Three decision groups were defined: (a) UIATS favoring treatment, (b) UIATS favoring observation, and (c) UIATS inconclusive. These results were then compared to our clinical decisions. Spearman’s rank-order correlation (ρ) was run to determine the relationship between the UIATS and our clinical decisions. Cases of discrepancies between UIATS and our clinical decisions were then examined for complications, defined as periprocedural adverse events in treated aneurysms, or aneurysm rupture in untreated aneurysms. Ninety-three patients with 147 UIA were included. A total of 118/147 (80.3%) UIA were treated. In 70/118 (59.3%), UIATS favored treatment, in 18/118 (15.3%), it was inconclusive, and in 30/118 (25.4%), it favored observation. A total of 29/147 (19.7%) UIA were not treated. In 15/29 (51.7%), UIATS favored observation, in 9/29 (31%), it favored treatment, and in 5/29 (17.2%), it was inconclusive (ρ = 0.366, p < 0.01). Discrepancies between UIATS and our clinical decisions did not correlate with complications (ρ = 0.034, p = 0.714). Our analysis shows that our more intuitive clinical decision-making has been in line with UIATS. Our treatment decisions did not correlate with an increased rate of complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
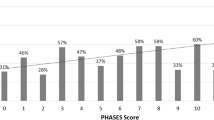
Aneurysmal subarachnoid hemorrhage (aSAH) is a devastating disease with significant morbidity (up to 60% at 6 months) and high mortality (40–50%) [1, 12]. With the advancement of diagnostic tools and the increasing frequency of cranial imaging, more and more unruptured intracranial aneurysms (UIA) have been detected, and it is estimated that approximately 3% of the general population harbors one [30]. The increase in UIA detection offers an opportunity for treatment with the aim to prevent aSAH. However, there are no clear criteria to predict which UIA will rupture, and when. Different risk factors for rupture of UIA have been identified, such as aneurysm size and morphology [5, 6, 9, 10, 17]. Greving et al. [5] developed the so-called PHASES score in 2014 to predict the risk of rupture of intracranial aneurysms. The following risk factors for aneurysm rupture were identified: population (North American, Japanese, and Finnish), hypertension, age, size of aneurysm, earlier aSAH from another aneurysm, and site of aneurysm. Based on a simple addition of risk factors, the 5-year cumulative aneurysm rupture risk could be estimated, which should relieve the treatment decision-making in the clinical setting. However, an important point of criticism towards the PHASES score is that it fails to acknowledge the aneurysm treatment risk. It has been determined that UIA treatment risk increases with patient age, as well as with aneurysm size and aneurysm complexity [11, 19], making these parameters equivocal when employed on their own to guide UIA treatment. In 2015, Etminan et al. [4] published the UIA treatment score (UIATS), a multidisciplinary consensus designed to support the clinical decision-making process (treatment vs. observation) in patients with UIA. By taking into consideration patient-related, aneurysm-related, and treatment-related risk factors identified by 39 world-renowned cerebrovascular specialists, this tool is the first one to incorporate all these aspects into one relatively simple formula. The score is based on theoretical data and personal experience rather than empirical data, and it has to be validated both in prospective studies and daily clinical setting. As a tertiary neurosurgical center in Germany with a focus on aneurysm (ruptured and unruptured) management, it was our aim to determine whether our clinical practice was in accordance with the newly published UIATS.
Materials and methods
We conducted a retrospective analysis of patients admitted to the Göttingen University Hospital harboring saccular UIA from January 2011 to May 2016. Unruptured infectious, traumatic, fusiform, and dissecting aneurysms and flow-related aneurysms in arteriovenous malformation and dural arteriovenous fistulas were excluded [4]. Decision-making at our center was guided by an interdisciplinary consensus between interventional neuroradiology and neurosurgery specialists. Previously established risk factors for UIA rupture such as aneurysm size (> 0.7 cm), morphology, location, current hypertension, previous aSAH, familial history, and multiple UIA were considered. UIA of the basilar artery were mainly treated endovascularly, while aneurysms of the middle cerebral artery were preferably treated surgically. Younger patients were preferably treated surgically, except for aneurysms of the basilar artery. If the UIA was suitable for both treatment modalities, patient preference played a crucial role in our aneurysm treatment decision-making. Surgically treated UIA underwent post-operative computed tomography (CT) and CT-angiography to confirm complete UIA occlusion and to exclude treatment associated complications. DynaCT (flat-panel angiographic computed tomography) scans were performed 3 years after the clipping of the aneurysm [23]. Additionally, in surgically treated patients, DynaCT was performed every 5 years until the age of 70 years for detection of possible de novo UIA. Endovascularly treated UIA underwent follow-up at 6 months with digital subtraction angiography (DSA), and yearly with magnetic resonance angiography (MRA). Untreated UIA underwent yearly follow-up with MRA.
The UIATS was applied to all saccular UIA. According to the UIATS [4], familial aneurysms were considered when two or more first-degree relatives were previously diagnosed with a UIA or aSAH. Current cigarette smoking was defined for adults who had smoked 100 cigarettes in their lifetime and smoked cigarettes at the time of clinical presentation. Hypertension was defined as systolic blood pressure greater than 140 mmHg and/or diastolic blood pressure greater than 90 mmHg. Current drug or alcohol use was defined as recent (within 1 year of clinical presentation) cocaine or amphetamine exposure, or heavy alcohol consumption (> 300 g/week ethanol). Chronic or malignant disease, neurocognitive disorders, and psychiatric disorders resulting in impairment of the patient’s ability to live alone were considered. Concomitant coagulopathies and thrombophilic diseases were also included. Aneurysm size was defined as the greatest aneurysm diameter, while aneurysm lobulation was defined as irregular daughter sac-like protrusion(s) of the aneurysm wall. Aspect ratio represents the ratio of aneurysm dome dimension and neck width, and size ratio was the largest aneurysm diameter divided by parent artery diameter. A complex aneurysm was defined as wide neck (greater than the diameter of the parent artery), significant lobulations, calcifications, intra-aneurysm thrombus, proximal vessel tortuosity/stenosis, branch artery incorporated into the neck or aneurysm sac, and very small aneurysm diameter (< 3 mm).
Factors favoring UIA treatment were scored with positive points, while factors against treatment were scored with negative points. A simple sum of all points was then performed to obtain the total UIATS. Because the UIATS takes into consideration aneurysm-related factors, and because some patients harbor more than one single aneurysm, the UIATS was calculated for each UIA. Results were subsequently divided into three groups: (a) UIATS favoring treatment (cumulative positive sum), (b) UIATS favoring observation (cumulative negative sum), and (c) UIATS non-conclusive (cumulative sum of 0).
Furthermore, we gathered data regarding periprocedural complications, defined as adverse events associated with UIA treatment. These included wound infections, post-operative hemorrhage, or new neurological deficits. Rupture of untreated UIA was also considered a complication in the observational group.
Statistical analysis
The results of the UIATS were compared to the clinical decisions made in our patient cohort, and Spearman’s rank-order correlation was run to determine the relationship between the UIATS and our clinical decisions. The cases in which UIATS was inconclusive were not considered for statistical analysis. Discrepancies between the UIATS and the clinical decisions made were then examined for associated complications. Our aim was to elucidate whether our decision to treat or not to treat UIA actually endangered our patients. Statistical analysis was performed using IBM® SPSS® Statistics Version 21.
Results
Patient-related risk factors
A total of 93 patients, 65 (70%) females and 28 (30%) males, harboring 147 UIA were included. Mean age was 57 years (range 36–84). When analyzing patient-specific risk factors, 24/93 (25.8%) patients had already suffered an aSAH. A positive family history was observed in 6/93 (6.5%). Ethnic risk factors were not identified in our cohort. Current smoking was reported by only 9.7% (9/93) of the patients. All patients denied current drug or alcohol abuse. Arterial hypertension was the most commonly observed risk factor (66/93, 71%). Polycystic kidney disease was observed in 1/93 (1.1%) patients. Most patients (48/93, 51.6%) had multiple aneurysms. Reduced quality of life due to fear of aneurysm rupture was also an important factor for 41/93 (44.1%) patients. Neurocognitive disorders, coagulopathies, and psychiatric disorders were observed in 10/93 (10.8%), 1/93 (1.1%), and 5/93 (5.4%) cases, respectively.
Aneurysm-related risk factors
Of the 147 aneurysms, 3 (2%) caused cranial nerve deficits, 4 (2.7%) exerted mass effect, 4 (2.7%) produced thromboembolic events, and 9 (6.1%) correlated with epilepsy. Aneurysm location is illustrated on Fig. 1. Most aneurysms were located in the middle cerebral artery (75/147, 51%). Similarly, most aneurysms (58/147, 39.5%) were rather small, with a diameter between 4.0 and 6.9 mm. An aspect ratio > 1.6 or irregularity was observed in 68/147 (46.3%) and 55/147 (37.4%), respectively. The remaining aneurysm-related risk factors are listed on Fig. 1.
Aneurysm-related risk factors by category, as stratified in the UIATS. a Aneurysm diameter, stratified according to the UIATS risk groups. b Aneurysm location, stratified in the three risk groups defined in the UIATS and “other.” c Other aneurysm-related risk factors considered in the UIATS by incidence in our cohort
Treatment-related risk factors
Most of the patients in our cohort were relatively young (between 40 and 60 years). Most aneurysms (80/147, 54.4%) were < 6.0 mm and deemed easy to treat (126/147, 85.7%), thus rendering the treatment-related risk rather low.
Treatment
In our cohort, 118/147 (80.3%) of UIA were treated; this accounted for 80/93 (86%) patients being treated. As mentioned above, the majority of our patients harbored multiple aneurysms (48/93, 51.6%). Of these, 39/48 (81.3%) underwent treatment. The most common treatment modality was surgical (105/118, 89%). In 70/118 (59.3%) of treated UIA, the UIATS favored treatment. In 18/118 (15.3%), the UIATS was non-conclusive, while in 30/118 (25.4%), the UIATS favored observation. On the other hand, 29/147 (19.7%) UIA were not treated. In 15/29 (51.7%) of these cases, the UIATS favored observation, while in 9/29 (31%), the UIATS favored treatment. In 5/29 (17.2%), the UIATS was non-conclusive. For statistical purposes, inconclusive cases were excluded from the analysis. Spearman’s rank-order correlation coefficient was 0.366, indicating a positive correlation between our decision-making and the UIATS recommendations. This correlation was statistically significant (p < 0.01). These results are summarized in Fig. 2.
Complications
Complications were defined as adverse events associated with UIA treatment or rupture of untreated UIA. Accordingly, complications were observed in a total of 13/93 (14%) patients, or in 13/147 (8.8%) of UIA analyzed.
Only 2/80 (2.5%) of all patients exhibited permanent deficits, namely hemiplegia due to post-operative infarctions. Other complications observed were transient oculomotor palsy (1/80, 1.3%), post-operative delirium (2/80, 2.5%), intraoperative rupture (1/80, 1.3%), transient hemiparesis (1/80, 1.3%), seizures (1/80, 1.3%), transient aphasia (1/80, 1.3%), and transient vasospasm (3/80, 3.8%). In one case (1/80, 1.3%), the surgery was aborted due to a dermoid cyst covering the aneurysm base. No rupture (0/13, 0%) was observed in the untreated group (13/93, 14%). Four (4/13, 30.8%) complications were observed in treated patients where the UIATS suggested observation. These were permanent right hemiplegia, transient aphasia, post-operative delirium, and intraoperative rupture. Two (2/13, 15.4%) of the complications were observed in treated patients where the UIATS was inconclusive, and 7/13 (53.8%) complications were observed in treated patients in whom the UIATS favored treatment. Overall, complications were not increasingly observed when discrepancies between UIATS and our clinical decisions existed. As illustrated on Fig. 3, a statistically significant correlation between discrepancies and complications could not be found (correlation coefficient 0.034, p = 0.714).
Discussion
The natural history of UIA is an elusive one, as randomized controlled studies are lacking for this pathology. Several clinicians deem the development of such trials as unethical, because the lack of treatment of UIA could result in a devastating aSAH. Therefore, data from observational studies constitute the best source of information for evaluating UIA [16, 31]. Expectedly, there are numerous sources of bias, and many questions remain unanswered, such as the following: Which UIA will rupture? When is the rupture risk of a given UIA larger than the treatment risk? Which intervention should be undertaken, once it has been decided to treat a UIA?
Which UIA will rupture? Patient-related risk factors
One of the most relevant studies for the assessment of UIA natural history is the International Study of Unruptured Intracranial Aneurysms (ISUIA) [8] from North America and Europe. This study has a retrospective arm including 1449 patients with 1937 UIA, and a prospective one with 4060 patients with 6221 UIA. According to this study, arterial hypertension and previous aSAH were found to be important in defining the probability of future aneurysm rupture. Specifically, patients with a previous aSAH had a rupture rate of 0.5% per year for aneurysms less than 10 mm in diameter, which was higher than that for similar-sized aneurysms in patients without a history of aSAH. In regards to patient-related risk factors, age has been found to inversely correlate with UIA rupture [13, 28]. Other comorbidities, such as autosomal dominant polycystic kidney disease (ADPKD) predispose individuals to developing more UIA. A recent systematic review by Cagnazzo et al. [2] demonstrated that the ADPKD population has a higher UIA prevalence (11%), with a comparable rupture rate to the general population. Nevertheless, more de novo aneurysms were observed in this cohort, so that a higher cumulative rupture risk has been speculated. Cigarette smoking and alcohol consumption (per 100 g/week) were significant predictors of aneurysm rupture in a study performed by Juvela et al. [9] in 142 patients harboring 181 untreated UIA between 1956 and 1978 in Finland. A prospective analysis by Korja et al. [10] yielded similar results in a Finnish population. Here, an annual rupture risk of 1.6% was observed, and cigarette smoking and female sex were predictors of aneurysm rupture. Cocaine and methamphetamine consumption has also been linked to aSAH, and it has been postulated that these substances may also lead to UIA rupture [21, 22].
Which UIA will rupture? Aneurysm-related risk factors
The retrospective arm from the ISUIA revealed that UIA located in the posterior circulation including the posterior communicating artery also exhibited a higher risk of rupture. Another relevant study was the Unruptured Cerebral Aneurysm Study (UCAS) [18], with 5720 prospectively analyzed Japanese patients. Here, the rupture risk of UIA was estimated at 0.95% per year. In a multivariate analysis, UIA diameter (> 7 mm), location (posterior or anterior communicating arteries), and the presence of a daughter sac were predictors of aneurysm rupture. Hishikawa et al. [6] also showed in a Japanese cohort that aneurysms larger than 7 mm and posterior communicating artery locations were independent predictors of UIA rupture in elderly patients. Additionally, Ujiie et al. [29] suggested that aspect ratios > 1.6 correlated with greater rates of UIA rupture. Rahman et al. [24] also demonstrated that the ratio between aneurysm size and parent artery diameter correlates with UIA rupture in a prospective study of 40 matched patients with UIA or ruptured aneurysms. A recently published study by Mocco et al. [15] further underscored these findings. The latter is based on the prospective arm of the ISUIA, and the authors conclude that size ratio is an important predictor of rupture, in addition to greatest diameter and posterior location. All these studies consistently found aneurysm size (> 7 mm) and location (posterior circulation, anterior communicating artery) to be strong predictors of rupture. On the other side, we know from studies with ruptured intracranial aneurysms that ruptured aneurysms are often smaller than 7 mm [3, 14]. A recently published study reported that 40% of all ruptured aneurysms were smaller than 5 mm. Although the aneurysm size is a strong predictor of aneurysm rupture, it is important to consider different risk factors during the treatment decision-making process of UIA. The UIATS includes not only the patient- and treatment-related risk factors but also the aneurysm treatment risks.
When is the rupture risk of a given UIA larger than the treatment risk? UIA treatment decision
All the aforementioned data provide an estimation of aneurysm rupture risk, and previous efforts have been made to incorporate these into a score to guide treatment decisions. The PHASES score was based on the pooled data from 8382 patients in six prospective cohort studies with UIA. It was developed to calculate the 5-year absolute aneurysm rupture risk under consideration of established risk factors for aneurysm rupture previously evaluated in those six prospective cohort studies. However, the data considered in the PHASES score were subject to attrition bias, as treatment of the UIA was left to physician’s discretion [5]. Therefore, the produced data about the rupture rate derives from patients that neurosurgeons or neuroradiologists did not consider suitable to treat. Additionally, treatment-related risk was not accounted for in this model. The UIATS [4], on the contrary, offers a comprehensive scoring system that attempts to objectivize patient-related, aneurysm-related, and treatment-related risk factors. It is based on a consensus of multidisciplinary specialists with high expertise in managing UIA. Therefore, the UIATS should be considered as an “advice” from a multidisciplinary group, rather than a mathematical model to predict UIA rupture. Since the UIATS is based on objective criteria, it should allow a more reliable appreciation of the risk factors for aneurysm rupture and aneurysm treatment and therefore facilitates an objective consultation of patients with UIA independent on the specialty of the treating physician.
However, one of the limitations of the UIATS is that it was based on the analysis of only 30 cases with UIA. Even though the authors argue these to be representative cases, some patient groups might have been underrepresented. Therefore, the UIATS may not be suitable for all patients with UIA. The other limitation might be that in the hands of highly specialized experts, UIA treatment yields better results leading to underestimation of the treatment risk. Our study is the first one performed to further validate the UIATS, as the score was applied to 147 UIA reflecting the daily clinical practice of a tertiary center in Germany.
We found a statistically significant agreement of our clinical decisions for the management of UIA with the resulting recommendation from the UIATS in our patient population. Nevertheless, the correlation coefficient, while positive at ρ = 0.366, does not reveal a perfect linear relationship between the UIATS score and our clinical decisions. Therefore, a prospective validation of the UIATS with a larger patient population is necessary in order to determine its applicability in daily clinical practice.
Which intervention should be undertaken?
Lastly, even though the UIATS provides an expert-based recommendation on whether or not to treat an UIA, the question of how to treat the UIA is unanswered. The ISAT (international subarachnoid aneurysm trial) [17] has been a landmark study guiding decision-making in the treatment of ruptured intracranial aneurysms, but a comparable study for UIA is still missing. The TEAM trial [25] was initiated in 2011 to elucidate whether endovascular occlusion of UIA was superior to conservative management. However, because of slow enrollment, this trial was never completed. The strongest evidence comes from a recent meta-analysis [26], which suggests that endovascular coiling and surgical clipping bear similar risk ratios of death, bleeding, cerebral ischemia, occlusion of aneurysm, and quality of life in patients with UIA. Nevertheless, this recommendation is rather broad and must be regarded carefully; aneurysm location, morphology, and complexity are a few of the many factors that may make a given UIA more amenable to one treatment modality or another. For instance, Smith et al. [27] argue that middle cerebral artery UIA should be treated surgically, based on their meta-analysis from 2015. Conversely, Naggara et al. [20] demonstrated in another meta-analysis that satisfactory occlusions of UIA were obtained in 86.1% of cases treated endovascularly, while Hwang et al. [7] argue in their systematic review that coiling is a better procedure for treatment of UIA in regards to short-term disability and complications. In our cohort, most patients were treated surgically, with a low complication rate. It could be proposed that our study supports surgical clipping of UIA, but this recommendation would be burdened by bias, as our center is specialized in cerebrovascular surgery and our study was retrospective in nature, not powered and/or designed to answer this question. Furthermore, the decision concerning the aneurysm treatment modality was made after interdisciplinary case discussion with the neuroradiologists at our institution. The majority of aneurysms included in our cohort were located in the middle cerebral artery. As illustrated in the literature, these aneurysms have been deemed more amenable to surgical treatment than to endovascular one. This is one of the reasons why most lesions underwent surgical clipping. In light of the lacking data from randomized clinical trials, the authors recommend UIA treatment based on center expertise.
Limitations and strengths
Because of its retrospective nature, our study is subject to several biases. On the one hand, treatment decisions were made on an individual basis relying on a panel of experts, and not on an objective, quantifiable algorithm. Therefore, our decisions were subject to selection bias. Furthermore, in patients with multiple UIA, treatment decision might have been influenced by surgical accessibility to multiple lesions, and not necessarily by risk of rupture. Securing a lesion “en passant” might have skewed both the percentage of UIA treated and the treatment modality employed. Additionally, this might have led to misestimating discrepancies between UIATS and treatment decisions. That being said, the criteria employed by our panel of experts were similar to the factors considered in the UIATS. On the other hand, complications such as aneurysm rupture in untreated patients might have been underrepresented, since those patients could have been admitted to other centers without our knowledge.
Nevertheless, our study was the first one performed to evaluate the applicability of the UIATS in daily clinical practice. As seen, there was a statistically significant correlation between our decision-making and the UIATS recommendations. The correlation coefficient, however, was rather low at ρ = 0.366. Bearing this in mind, the UIATS should continue to be used with caution. The discrepancies observed between the UIATS recommendation and our clinical decisions did not show a statistically significant correlation with complications (periprocedural adverse effects or rupture) and, accordingly, did not contribute to poorer outcome. Even in experienced hands, decision-making in patients harboring UIA/UIAs remains a difficult one due to multiplicity of factors influencing aneurysm rupture and risk of aneurysm treatment. The UIATS does not consider all possible factors but covers a lot of relevant aneurysm-related, patient-related and treatment-related risk factors building a supportive algorithm for clinical decision-making in this patient population.
Conclusion
As we stand, there are still no randomized controlled trials to sufficiently support the treatment decision-making in patients with UIA. Nevertheless, several risk factors for UIA rupture have been consistently identified in different cohort studies and meta-analyses, as evinced in our discussion. While no mathematical model currently exists to predict UIA rupture risk and/or treatment benefits, aSAH is a devastating and potentially avoidable complication of UIA. In a scientific environment where unequivocal evidence is missing, the UIATS represents a good surrogate to guide clinical decision-making, as it considers patient-related, aneurysm-related, and treatment-related factors. Our study provides support of its use, as the UIATS encompasses all the established risk factors for aneurysm rupture and provides the clinician with the recommendation of a panel of cerebrovascular experts. That being said, the decision to treat UIA remains an individual one, without a reliable predictor, and one should employ the UIATS with caution.
References
Bonita R, Thomson S (1985) Subarachnoid hemorrhage: epidemiology, diagnosis, management, and outcome. Stroke 16(4):591–594. https://doi.org/10.1161/01.STR.16.4.591
Cagnazzo F, Gambacciani C, Morganti R, Perrini P (2017) Intracranial aneurysms in patients with autosomal dominant polycystic kidney disease: prevalence, risk of rupture, and management. A systematic review. Acta Neurochir 159(5):811–821. https://doi.org/10.1007/s00701-017-3142-z
Choi J, Park H (2017) The incidence and characteristics of patients with small ruptured aneurysms (<5 mm) in subarachnoid hemorrhage. J Korean Neurosurg Soc 60(4):424–432. https://doi.org/10.3340/jkns.2016.0910.003
Etminan N, Brown R, Beseoglu K, Juvela S, Raymond J, Morita A, Torner J, Derdeyn C, Raabe A, Mocco J, Korja M, Abdulazim A, Amin-Hanjani S, Salman R, Barrow D, Bederson J, Bonafe A, Dumont A, Fiorella D, Gruber A (2015) The unruptured intracranial aneurysm treatment score—a multidisciplinary consensus. Neurology 85:1–9
Greving J, Wermer M, Brown RJ, Morita A, Juvela S, Yonekura M, Ishibashi T, Torner J, Nakayama T, Rinkel G, Algra A (2014) Development of the PHASES score for prediction of risk of rupture of intracranial aneurysms: a pooled analysis of six prospective cohort studies. Lancet Neurol 13(1):59–66. https://doi.org/10.1016/S1474-4422(13)70263-1
Hishikawa T, Date I, Tokunaga K, Tominari S, Nozaki K, Shiokawa Y, Houkin K, Murayama Y, Ishibashi T, Takao H, Kimura T, Nakayama T, Morita A (2015) Risk of rupture of unruptured cerebral aneurysms in elderly patients. Neurology 85(21):1879–1885. https://doi.org/10.1212/WNL.0000000000002149
Hwang J, Hyun M, Lee H, Choi J, Kim J, Lee N, Kwon J, Lee E (2012) Endovascular coiling versus neurosurgical clipping in patients with unruptured intracranial aneurysm: a systematic review. BMC Neurol 22(12):99
International study of unruptured intracranial aneurysms investigators (1998) Unruptured intracranial aneurysms—risk of rupture and risks of surgical intervention. N Engl J Med 339(24):1725–1733
Juvela S, Poussa K, Lehto H, Porras M (2013) Natural history of unruptured intracranial aneurysms—a long-term follow-up study. Stroke 44(9):2414–2421. https://doi.org/10.1161/STROKEAHA.113.001838
Korja M, Lehto H, Juvela S (2014) Lifelong rupture risk of intracranial aneurysms depends on risk factors—a prospective Finnish cohort study. Stroke 45(7):1958–1963. https://doi.org/10.1161/STROKEAHA.114.005318
Kotowsi M, Naggara O, Darsaut T, Nolet S, Gevry G, Kouznetsov E, Raymond J (2013) Safety and occlusion rates of surgical treatment of unruptured intracranial aneurysms: a systematic review and meta-analysis of the literature from 1990 to 2011. J Neurol Neurosurg Psychiatry 84(1):42–48. https://doi.org/10.1136/jnnp-2011-302068
Lantigua H, Ortega-Gutierrez S, Schmidt J, Lee K, Badjatia N, Agarwal S, Claassen J, Connolly E, Mayer S (2015) Subarachnoid hemorrhage: who dies, and why? Crit Care 19(1):309–315. https://doi.org/10.1186/s13054-015-1036-0
Lee E, Lee H, Hyun M (2012) Rupture rate for patients with untreated unruptured intracranial aneurysms in South Korea during 2006-2009. J Neurosurg 117(1):53–59. https://doi.org/10.3171/2012.3.JNS111221
Lee G, Eom K, Lee C, Kim D, Kang S (2015) Rupture of very small intracraial aneurysms: incidence and clinical characteristics. J Cerebrovasc Endovasc Neurosurg 17(3):217–222. https://doi.org/10.7461/jcen.2015.17.3.217
Mocco J, Brown R, Torner J, Capuano A, Fargen K, Raghavan M, Piepgras D, Meissner I, Lii J (2017) Aneurysm morphology and prediction of rupture: an international study of unruptured intracranial aneurysms analysis. Neurosurgery. https://doi.org/10.1093/neuros/nyx226
Mocco J, Komotar R, Lavine S, Meyers P, Connolly E, Solomon R (2004) The natural history of unruptured intracranial aneurysms. Neurosurg Focus 17(5):E3
Molyneux A, Kerr R, Yu L, Clarke M, Sneade M, Yarnold J, Sandercock P (2005) International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms. Lancet 366(9488):809–817. https://doi.org/10.1016/S0140-6736(05)67214-5
Morita A, Kirino T, Hashi K (2012) The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med 366(26):2474–2482. https://doi.org/10.1056/NEJMoa1113260
Naggara O, Lecler A, Oppenheim C, Meder J, Raymond J (2012) Endovascular treatment of intracranial unruptured aneurysms: a systematic review of the literature on safety with emphasis on subgroup analyses. Radiology 263(3):828–835. https://doi.org/10.1148/radiol.12112114
Naggara O, White P, Guilbert F, Roy D, Weill A, Raymond J (2010) Endovascular treatment of intracranial unruptured aneurysms: systematic review and meta-analysis of the literature on safety and efficacy. Radiology 256(3):887–897. https://doi.org/10.1148/radiol.10091982
Nanda A, Vannemreddy P, Polin R, Willis B (2000) Intracranial aneurysms and cocaine abuse: analysis of prognostic indicators. Neurosurgery 46(5):1063–1067. https://doi.org/10.1097/00006123-200005000-00006
Oyesiku N, Colohan A, Barrow D, Reisner A (1993) Cocaine-induced aneurysmal rupture: an emergent negative factor in the natural history of intracranial aneurysms? Neurosurgery 32(4):518–525. https://doi.org/10.1227/00006123-199304000-00005
Psychogios MN, Wachter D, Mohr A, Schramm P, Frölich AM, Jung K, Rohde V, Knauth M (2011) Feasibility of flat panel angiographic CT after intravenous contrast agent application in the postoperative evaluation of patients with clipped aneurysms. AJNR Am J Neuroradiol 32(10):1956–1962. https://doi.org/10.3174/ajnr.A2611
Rahman M, Smietana J, Hauck E, Hoh B, Hopkins N, Siddiqui A, Levy E, Meng H, Mocco J (2010) Size ratio correlates with intracranial aneurysm rupture status: a prospective study. Stroke 41(5):916–920. https://doi.org/10.1161/STROKEAHA.109.574244
Raymond J, Darsaut T, Molyneux A (2011) A trial on unruptured intracranial aneurysms (the TEAM trial): results, lessons from a failure and the necessity for clinical care trials. Trials 12(1):64. https://doi.org/10.1186/1745-6215-12-64
Ruan C, Long H, Sun H, He M, Yang K, Zhang H, Mao B (2015) Endovascular coiling vs. surgical clipping for unruptured intracranial aneurysm: a meta-analysis. Br J Neurosurg 29(4):485–492. https://doi.org/10.3109/02688697.2015.1023771
Smith T, Cote D, Dasenbrock H, Hamade Y, Zammar S, El Tecle N, Batjer H, Bendok B (2015) Comparison of the efficacy and safety of endovascular coiling versus microsurgical clipping for unruptured middle cerebral artery aneurysms: a systematic review and meta-analysis. World Neurosurg 84(4):942–953. https://doi.org/10.1016/j.wneu.2015.05.073
Sonobe M, Yamazaki T, Yonekura M, Kikuchi H (2010) Small unruptured intracranial aneurysm verification study: SUAVe study, Japan. Stroke 41(9):1969–1977. https://doi.org/10.1161/STROKEAHA.110.585059
Ujiie H, Tachibana H, Hiramatsu O, Hazel A, Matsumoto T, Ogasawara Y, Nakajima H, Hori T, Takakura K, Kajiya F (1999) Effects of size and shape (aspect ratio) on the hemodynamics of saccular aneurysms: a possible index for surgical treatment of intracranial aneurysms. Neurosurgery 45(1):119–129
Wiebers D (2003) Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 362(9378):103–110. https://doi.org/10.1016/S0140-6736(03)13860-3
Vlak M, Algra A, Brandenburg R, Rinkel G (2011) Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: a systematic review and meta-analysis. Lancet Neurol 10(7):626–636. https://doi.org/10.1016/S1474-4422(11)70109-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was performed in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study (retrospective analysis), formal consent is not required. Upon admission, patients at our institution sign a treatment contract, in which the use of anonymized patient data for research purposes is consented to.
Rights and permissions
About this article
Cite this article
Hernández-Durán, S., Mielke, D., Rohde, V. et al. The application of the unruptured intracranial aneurysm treatment score: a retrospective, single-center study. Neurosurg Rev 41, 1021–1028 (2018). https://doi.org/10.1007/s10143-018-0944-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-018-0944-2