Abstract
In the present study, we investigated the types and ratio of posterior clinoid process (PCP) pneumatization in paranasal sinus multidetector computed tomography (MDCT). Paranasal MDCT images of 541 subjects (227 males, 314 females), between 15 and 65 years old, were included into the study. Pneumatization of anterior clinoid process and pneumatization types (I, II, or III) were evaluated in the males and females. PCP pneumatization was detected in 20.7 % of the males and 11.5 % of the females. Right, left, and bilateral PCP pneumatizations were detected in 7.9, 5.7, and 7.0 % of the males and 2.9, 3.2, and 4.5 % of the females, respectively. PCP pneumatization of the males is significantly higher than the females. The most detected type of pneumatization was type I (61.2 %) for all groups. In right, left, and bilateral pneumatizations separately, type I pneumatization was the most detected pneumatization type with the ratio of the 70.4, 65.2, and 50.0 %, respectively. In males, type I (61.7 %), and similarly in females, type I (60.6 %) pneumatization were detected more. Type II and type III pneumatizations were detected in decreasing order in both groups. In younger subjects, pneumatization of posterior clinoid process was found as higher, and in older subjects, PCP pneumatization was found as lower. Sclerosis process related to the aging may be responsible for the lower pneumatization ratios in older subjects. Structure of the surrounding regions of PCP is important for surgical procedures related to cavernous sinus, basilar apex aneurysms, and mass lesions. Preoperative radiological examinations are useful for operative planning. Any anomalies to PCP can cause unnecessary injury to the neurovascular complex structure around the cavernous sinus or postclinoidectomy CSF fistulas. Posterior clinoidectomies should be avoided in patients with type III PCP pneumatization to prevent CSF fistulas.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The anterior, middle, and posterior clinoid processes (PCPs) in the sphenoid bone contribute to the boundary of the sella turcica. The posterior boundary is formed by a square-shaped plate of bone called the dorsum sellae, the superolateral angles of which are raised to form the posterior clinoid processes [1, 2]. Variations in PCPs are important in intracranial neurosurgery. The PCP deepens the sella turcica and gives an attachment to the tentorium cerebelli. Therefore, any anomalies of the PCP may be responsible for the altered attachment of the tentorium cerebelli. Internal carotid artery, superior petrosal sinus, and oculomotor and trochlear nerves are critical structures which are located closely to the PCPs. To work in the upper basilar region, the posterior aspect of the pituitary fossa, the cavernous sinus, and the internal carotid artery, the anatomy of the clinoid processes should be known in detail [2].
The sphenoid body has a chondral origin. Ossification centers are the presphenoid (between the lesser wings) and the basisphenoid (between the greater wings) [3–5]. Ossification of the PCPs begins after about 4 years of age. The size of the dorsum sellae increases until puberty [2, 6–8].
In this study, we investigated the types and ratio of PCP pneumatization and discussed the importance of it in neurosurgical approaches. The definition of the PCP pneumatization is performed for the first time in the literature, and we made the classification similar to the classification of anterior clinoid process pneumatization reported by Abuzayed et al. [9].
Materials and methods
This retrospective study was conducted in December 2015 in Kırıkkale University, Faculty of Medicine, according to the principles of the Declaration of Helsinki. Computed tomography images were obtained from archive of the Kırıkkale University, Faculty of Medicine, Radiodiagnostic Department. Approval of the local ethics committee of the Kırıkkale University, Faculty of Medicine, was taken (date: November 17, 2015, no. 25/10)
Subjects
In this study, paranasal computed tomography (CT) images of 541 subjects (227 males, 314 females), between 15 and 65 years old, selected from a digital radiology database of all cranial CT in the Kırıkkale University, Faculty of Medicine, Radiodiagnostic Department, were included. The age of the males was 36.79 (mean) ± 13.25 years (ranged from 15.0 to 65.0), and age of the females was 33.69 (mean) ± 13.00 years (ranged from 15.0 to 65.0). Inclusion and exclusion criteria are shown in Table 1.
Technical considerations of multidetector computed tomography (MDCT)
All of the scans were obtained with routine paranasal computed tomography imaging in the supine position, with no contrast or sedation being used for the procedures. The images were acquired using a 64-slice CT (MSCT; Brilliance 64, Philips Medical System, Best, the Netherlands). All of the scans were obtained using the following parameters: tube voltage = 120 kV, effective mAs = 350, slice thickness = 1.00 mm, field of view (FOV) = 180 mm, and image matrix = 768 × 768. The images were transferred to a commercially available workstation, and the raw data was reconstructed using bone algorithms. After scanning, the coronal, axial, and sagittal images were reconstructed with a slice thickness of 1.00 mm.
The following image analyses were performed:
-
1.
Pneumatization of posterior clinoid process (PCP): It is evaluated as absent or present (right, left, bilateral).
-
2.
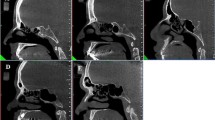
Type of posterior clinoid process pneumatization: Type I, type II, or type III (Figs. 1, 2, 3, 4, and 5). The definition of PCP pneumatization is performed for the first time in the literature, and we made the classification similar to the classification of anterior clinoid process pneumatization reported by Abuzayed et al. [9]:
-
(a)
Type I, in which less than 50 % of the PCP is pneumatized.
-
(b)
Type II, in which more than 50 % but not to totally pneumatized.
-
(c)
Type III, in which the PCP is totally pneumatized.
-
(a)
Measurements were performed in males and females.
Statistical analysis
SPSS for Windows 16.0 (SPSS Inc., an IBM Company, Chicago, IL). Chi-squared test and Spearman’s correlation rho efficient test were used.
p value <0.05 was considered as statistically significant.
Results
Posterior clinoid pneumatization (PCP) in males and females is presented in Table 1. In males, PCP pneumatization was detected in 20.7 % of the subjects, and in females, it was detected in 11.5 % of the subjects. Right, left, and bilateral ACP pneumatization were detected in 7.9, 5.7, and 7.0 % of males and 2.9, 3.2, and 4.5 % of the females, respectively (p < 0.05) (Table 2).
Types of the posterior clinoid process pneumatization according to the sides are shown in Table 2. The most detected type of pneumatization was type I (61.2 %) for all groups. In right, left, and bilateral pneumatizations separately, type I pneumatization was the most detected pneumatization type with the ratio of the 70.4, 65.2, and 50.0 %, respectively. Type II pneumatizations were detected in the second order, and type III pneumatizations were detected in the third order (p > 0.05) (Table 3).
Types of the anterior clinoid process pneumatization in males and females are shown in Table 3. In males, type I (61.7 %), and in females, type I (60.6 %) pneumatizations were detected more. Type II and type III pneumatizations were detected in decreasing order in both groups (p > 0.05) (Table 4).
Spearman correlation rho efficient test results showed that in younger subjects, pneumatization of posterior clinoid process was found as higher, and in older subjects, PCP pneumatization was found as lower (p = 0.036, r = −0.090). In older subjects, the type of PCP pneumatization got lower and type I pneumatization was detected most (p = 0.033, r = −0.092).
PCP pneumatization was significantly higher in males compared to females (p = 0.001, r = 0.137).
Discussion
The degree of the pneumatization in the sphenoid sinuses may change from absent to broad [10]. Pneumatization reaches out into the surrounding bones and also in the anterior and posterior clinoid process [11, 12]. As the pneumatization increase, the bone over the optic nerve, vidian nerve, or carotid arteries can be thin or absent. In this condition, these vital structures can be exposed to the iatrogenic traumas [13].
Anterior clinoid process pneumatization was reported in a lot of studies in the literature [14–18]. However, PCP pneumatization has not been reported yet. In the present study, PCP pneumatization was detected in 20.7 % of the males and 11.5 % of the females. Right, left, and bilateral PCP pneumatizations were detected in 7.9, 5.7, and 7.0 % of the males and 2.9, 3.2, and 4.5 % of the females, respectively. PCP pneumatization of the males is significantly higher than the females. The most detected type of pneumatization was type I (61.2 %) for all groups. In right, left, and bilateral pneumatizations separately, type I pneumatization was the most detected pneumatization type with the ratio of the 70.4, 65.2, and 50.0 %, respectively. In males, type I (61.7 %), and similarly in females, type I (60.6 %) pneumatizations were detected more. Type II and type III pneumatizations were detected in decreasing order in both groups. In younger subjects, pneumatization of posterior clinoid process was found as higher, and in older subjects, PCP pneumatization was found as lower.
The PCP is an anatomic boundary to tumors situated in the retrosellar territory and interpeduncular cistern region [19, 20], and its expulsion could encourage presentation of these areas [21]. The PCPs and the dorsum sellae are the primary bony structures that obscure the view of the upper 2/5 of the basilar artery [22]. Therefore, resection of the PCP is an important surgical stage in aneurysms of the basilar bifurcation. Furthermore, in highly located or giant aneurysms, removal of the PCP is required [23–25].
PCP is very important in operations relevant to internal carotid artery in which PCP is usually drilled. It is also defined as clinoidectomy. Nutik [26] described the reach into the dorsum sella and the cavernous sinus by PCP clinoidectomy. They have suggested this method for basillary artery tip aneurysms. Related to the surgical techniques, third cranial nerve and posterior communicating artery injury can occur. Additionally, bleeding from carotid artery and/or cavernous venous plexus may happen after PCP clinoidectomy [27, 28]. Because of these risks, PCP clinoidectomy ought not to be performed if there is type III PCP pneumatization. Because in this type of PCP pneumatization, CSF fistula develops in all cases. In these cases, high pterional approach should be used to operate the supraclinoid and paraclinoid aneurysms. We recommend that paranasal CT slides be evaluated in detail during the preoperative period to detect any PCP pneumatization. To prevent CSF fistulas, posterior clinoidectomies should be avoided in patients with type III PCP pneumatization [18].
Because of the anatomic variations of PCP and superficial petrosal sinus, surgeons need to have good anatomic information about internal carotid artery and tentorium cerebelli. The literature related to PCP abnormalities is less. The clinical significance of PCP pneumatization can be said that transclinoidal surgery may pose a lot of risks during clinoidectomy process including the drilling of the PCP. For example, to reach the basilar artery and to expose it, PCP pneumatization has a great importance. Clinoidectomy provides a wider area to access oculomotor nerve and the carotid artery. There is little literature on the upper front area of the posterior fossa; therefore, this region has remained hidden.
In neurosurgical procedures, to enter the trochlear, oculomotor, or cavernous sinus regions, the distance between the PCP and these structures should be measured preoperatively to avoid complications. Any bone bridge that connects to the surrounding structures to PCP has been recognized as being particularly dangerous for clinoidectomy operations. Preoperative cranial CT planning is advised in advance of such operations. PCP’s dural layer may be strained because of abnormalities involving this region. Resection of the abnormal PCP may cause unnecessary tears in the dura. At this time, the internal carotid artery, oculomotor, and trochlear nerves are also injured accidentally. Before the operations for basilar aneurysm under the PCP, a detailed plan should be performed before the surgery.
In this study, we presented the ratio of PCP pneumatization which is higher in males and in younger subjects. When getting older, possible sclerosis process may cause lower PCP pneumatization rates.
Conclusion
Structure of the surrounding regions of PCP is important for the surgical procedures related to cavernous sinus, basilar apex aneurysms, and mass lesions. Preoperative radiological examinations are useful for operative planning. Any anomalies to PCP can cause unnecessary injury to the neurovascular complex structure around the cavernous sinus or postclinoidectomy CSF fistulas. Posterior clinoidectomies should be avoided in patients with type III PCP pneumatization to prevent CSF fistulas.
References
Standring S, Ellis H, Berkovitz BKB et al (eds) (2005) The anatomical basis of clinical practice. In: Gray’s anatomy. Elsevier Churchill Livingstone, New York. p 462
Tang CT, Baidya NB, Tseng KY, Ma HI (2012) Posterior clinoid process as a landmarker in current endoscopic-assisted neurosurgical approaches. Formos J Surg 45:45–50
Tubbs RS, Salter EG, Oakes WJ (2007) Quantitation of and measurements utilizing the sphenoid ridge. Clin Anat 20:131–134
Kier EL, Rothman SLG (1976) Radiologically significant anatomic variations of the developing sphenoid in humans. In: Bosma JF (ed) Development of the Basicranium. Department of Health, Education, and Welfare, Bethesda, pp. 107–140
Arey LB (1965) Developmental anatomy, 7th edn. W.B. Saunders Co, Philadelphia, p. 306
Gordon MB, Bell AL (1922) A roentgenographic study of the sella turcica in normal children. New York State J Medic 22:54–59
Mahmoud ME-S (1958) The sella in health and disease: the value of the radiographic study of the sella turcica in the morbid anatomical and tomographic diagnosis of intracranial tumors. Brit J Radiol 31:1–100
Berger PE, Harwood-Nash DC, Fitz CR (1976) The dorsum sella in infancy and childhood. Pediatr Radiol 4:214–220
Abuzayed B, Tanriover N, Biceroglu H, Yuksel O, Tanriover O, Albayram S, Akar Z (2010) Pneumatization degree of the anterior clinoid process: a new classification. Neurosurg Rev 33:367–374
Kinnman J (1977) Surgical aspects of the anatomy of the sphenoidal sinuses and the sella turcica. J Anat 124:541–553
Yune H, Holden R, Smith J (1975) Normal variations and lesions of the sphenoid sinus. Am J Roentgenol 124:129–138
Fujioka M, Yung L (1978) The sphenoid sinuses: radiographic patterns of normal development and abnormal findings in infants and children. Radiology 129:133–139
Liu S, Wang Z, Zhou B (2002) Related structures of the lateral sphenoid wall anatomy studies in CT and MRI. Lin Chuang Er Bi Yan Hou Ke Za Zhi 16:407–409
Bolger WE, Butzin CA, Parsons DS (1991) Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope 101:56–64
Vidic B (1968) The postnasal development of the sphenoidal sinus and its spread into the dorsum sellae and posterior clinoid processes. Am J Roentgenol Radium Therapy, Nucl Med 104:177–183
Sirikci A, Bayazit YA, Bayram M et al (2000) Variations of sphenoid sinus and related structures. Eur Radiol 10:844–848
Birsen U, Gulsah B, Yasemin K et al (2006) Risky anatomic variations of sphenoid sinus for surgery. Surg Radiol Anat 28:195–201
Burulday V, Muluk NB, Akgül MH, Kaya A, Öğden M (2016) Presence and types of anterior clinoid process pneumatization, evaluated by multidetector computerized tomography. Clin Invest Med 39(3):E105–E110
Dolenc VV (2003) Surgical management of a meningioma in the retrosellar region. Acta Neurochir 145(3):220
Kassam AB, Prevedello DM, Thomas A et al (2008) Endoscopic endonasal pituitary transposition for a transdorsum sellae approach to the interpeduncular cistern. Neurosurgery 62(3suppl 1):57–72 discussion 72-54
Salma A, Wang S, Ammirati M (2010) Extradural endoscope-assisted subtemporal posterior clinoidectomy: a cadaver investigation study. Neurosurgery 67(3 Suppl Operative):ons43–ons48 discussion ons48
Gonzalez LF, Amin-Hanjani S, Bambakidis NC, Spetzler RF (2005) Skull base approaches to the basilar artery. Neurosurg Focus 19(2):E3
Figueiredo EG, Zabramski JM, Deshmukh P, Crawford NR, Preul MC, Spetzler RF (2006) Anatomical and quantitative description of the transcavernous approach to interpeduncular and prepontine cisterns. Technical note. J Neurosurg 104(6):957–964
Bambakidis NC, Gonzalez LF, Amin-Hanjani S et al (2005) Combined skull base approaches to the posterior fossa. Technical note. Neurosurg Focus 19(2):E8
Chanda A, Nanda A (2002) Anatomical study of the orbitozygomatic transsellar-transcavernous-transclinoidal approach to the basilar artery bifurcation. J Neurosurg 97(1):151–160
Nutik SL (1998) Pterional craniotomy via a transcavernous approach for the treatment of low-lying distal basilar artery aneurysms. J Neurosurg 89:921–926
Dolenc VV, Skrap M, Sustersic J et al (1987) A transcavernous-transsellar approach to the basilar tip aneurysms. Br J Neurosurg 1(2):251–259
Seoane E, Tedeschi H, de Oliveira E, Wen HT, Rhoton AL Jr (2000) The pretemporal transcavernous approach to the interpeduncular and prepontine cisterns: microsurgical anatomy and technique application. Neurosurgery 46(4):891–898 discussion 898-9
Author contributions
Veysel Burulday: Planning, designing, data collection, and literature survey.
Mehmet Hüseyin Akgül: Planning, designing, data collection, and literature survey.
Nuray Bayar Muluk: Planning, designing, literature survey, statistical analysis, and writing.
Mehmet Faik Ozveren: Literature survey.
Ahmet Kaya: Data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study is retrospective. Ethics committee approval was obtained, and there is no need to take informed consent because the data was evaluated retrospectively.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There are no funds for this article.
Rights and permissions
About this article
Cite this article
Burulday, V., Akgül, M.H., Muluk, N.B. et al. Evaluation of posterior clinoid process pneumatization by multidetector computed tomography. Neurosurg Rev 40, 403–409 (2017). https://doi.org/10.1007/s10143-016-0794-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-016-0794-8