Abstract
A remote cerebellar hemorrhage (RCH) is a spontaneous bleeding in the posterior fossa, which may rarely occurs as a complication of supratentorial procedures, and it shows a typical bleeding pattern defined “the zebra sign.” However, its pathophysiology still remains unknown. We performed a comprehensive review collecting all cases of RCH after supratentorial craniotomies reported in literature in order to identify the most frequently associated procedures and the possible risk factors. We assessed percentages of incidence and 95 % confidence intervals of all demographic, neuroradiological, and clinical features of the patients. Univariate and multivariate analyses were used to evaluate their association with outcome. We included 49 articles reporting 209 patients with a mean age of 49.09 ± 17.07 years and a male/female ratio 130/77. A RCH was more frequently reported as a complication of supratentorial craniotomies for intracranial aneurysms, tumors debulking, and lobectomies. In the majority of cases, RCH occurrence was associated with impairment of consciousness, although some patients remained asymptomatic or showed only slight cerebellar signs. Coagulation disorders, perioperative cerebrospinal fluid drainage, hypertension, and seizures were the most frequently reported risk factors. Zebra sign was the most common bleeding pattern, being observed in about 65 % out of the cases, followed by parenchymal hematoma and mixed hemorrhage in similar percentages. A multivariate analysis showed that symptomatic onset and intake of antiplatelets/anticoagulants within a week from surgery were independent predictors of poor outcome. However, about 75 % out of patients showed a good outcome and a RCH often appeared as a benign and self-limiting condition, which usually did not require surgical treatment, but only prolonged clinical surveillance, unless in the event of the occurrence of complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A remote cerebellar hemorrhage (RCH) is a postoperative complication characterized by spontaneous bleeding in the posterior fossa after supratentorial procedures. It is a relatively rare occurrence with an incidence of approximately 0.08–0.6 % [2].
RCH has been described after different supratentorial craniotomies [11, 45], burr holes for hematomas’ evacuation, or trans-sphenoidal procedures [2].
The typical bleeding pattern is defined as “the zebra sign” which is characterized by blood in the sulci of cerebellar hemispheres and vermis facing the tentorium. It has been reported as an isolated pattern or in association with a intracerebellar hemorrhage (ICH). Since RCH was first described by Yasargil and Yonekawa in 1977 [52], it has intrigued the neurosurgical community due to the uncertainty regarding the pathophysiology, risk factors, best treatment, and outcome.
This paper is the first systematic review of the English literature reporting cases of RCH after supratentorial craniotomies. The aim of this study is to identify which procedures are more frequently associated with RCH and discuss the pathophysiological mechanisms and the possible risk factors.
Materials and methods
Study selection
A comprehensive review of the literature was performed using the keywords “remote AND cerebellar AND (hemorrhage OR stroke)” to search in PubMed and Scopus databases. Search terms were identified by consulting MeSH terms and according to the most common definition adopted by the authors. All studies in the English language reporting on cases of RCH after supratentorial procedures were selected. Review papers, letters, and cases of RCH after infratentorial or spinal procedures were excluded. Two couples of reviewers (CLS/MR and FV/VB) independently abstracted data from the included papers. Any differences were resolved by consensus and discussion with the senior author (DdA). The last search was launched in September 2013. The search strategy followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement where applicable, and this checklist was used in designing and reporting our review.
Variables and risk factors assessment
We evaluated the following variables: demographics, primary disease (intracranial aneurysm (IA), tumor, focal epilepsy, vascular malformation, or other), and surgical procedure (clipping, tumor/malformation resection, hematoma evacuation, lobectomy, bypass, or other). In regard to RCH characteristics, we assessed the following variables: pattern (zebra sign, ICH, or mixed), clinical onset (asymptomatic, cerebellar signs, seizures, impairment of consciousness, or coma), timing of bleeding (immediately after surgery, within 24, 48, 72 h or later than 72 h), and the relationship between side of craniotomy and side of RCH (omolateral, contralateral, bilateral, or midline).
Moreover, we considered the different management strategies adopted by the authors (clinical observation, external ventricular drainage (EVD), sub-occipital decompression (SD)), the clinical status at hospital discharge and at follow-up (assessed by Glasgow Outcome Scale (GOS)). For studies reporting a different outcome scale, a correspondent GOS score was assigned. According to the GOS, patient outcome was dichotomized as follows: “good” in those with good recovery or moderate disability, and “poor” in those with severe disability, vegetative state, or dead.
Finally, we explored the frequency of a number of potential risk factors distinguishing them in: preexisting pathological conditions, intraoperative complications, and surgical maneuvers potentially at risk for RCH; we also analyzed their relationship with outcome.
According to the literature, a zebra sign was defined as alternating hyperdense/hypodense curvilinear, slightly irregular stripes along the cerebellar folia, imitating a zebra’s coat, indicating subarachnoid bleeding [7], whereas an ICH was defined as a hemorrhage within the cerebellar parenchyma.
Statistical analysis
Data were individually extracted for each patient. Percentage of incidence and 95 % of confidence intervals (CI) were calculated for all considered variables and outcomes. For those risk factors with the similar clinical significance, we also assessed their cumulative incidence.
Since we collected data from a large time period and pooled together case reports and case series, we stratified the outcomes according to the year of publication (before and after 2001 at intervals of 4 years), and the sample size (less vs more than ten cases), in order to evaluate selection or publication bias.
Quantitative variables were expressed as mean ± standard deviation and Student’s t test was used to compare their means. Fisher’s exact test (two-sided) was instead used to compare categorical variables.
Two logistic regression models were built in order to assess the independent contribution of those variables significantly associated with outcome at univariate analysis, alternatively introducing the time as variable. Positive (PPV) and negative predictive value (NPV) of the main predictors were also measured, and the receiver operating characteristics curve (ROC) analysis was performed to determine sensitivity and specificity. The associations were considered significant when p < 0.05. The statistical package used was SPSS 13.0 (SPSS Inc., Chicago, IL).
Results
Study selection
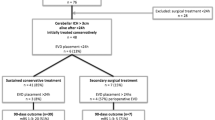
The electronic literature search yielded 154 results; 49 articles (from 1977 to 2013) met our inclusion criteria and were analyzed in detail [1, 3–31, 34–40, 42–54]. Eighteen papers were case reports, and 31 were series including from 2 to 42 patients. Overall, 209 patients were included in the study.
Demographic characteristics
Age was reported in 194 out of 209 patients (92.82 %), and the mean age at diagnosis was 49.09 ± 17.07 years (range 12–80). Sex was reported in 207 out of 209 patients (99.04 %) and the male/female ratio was 130/77 (62.8 vs 37.2 %).
Associated procedures
RCH was a complication more frequently observed after supratentorial craniotomies for treatment of IA (39.2 %), tumors (26.3 %), focal epilepsy (20 %), hematomas (7.1 %), vascular malformations (3.3 %), ischemia (1.4 %), and other diseases (2.3 %). All reported IA (26.8 % ruptured) underwent clipping; tumors were treated with debulking in 92.7 % and lobectomy in 7.3 % of cases; patients with focal epilepsy underwent frontal or temporal lobectomy in 14.3 and 85.7 %, respectively; similarly, vascular malformations underwent selective resection in 85.7 % and lobectomy in 14.3 %; all cerebral hematomas were evacuated through external drainage; three patients affected by cerebral ischemia underwent STA-MCA bypass; different procedures were instead performed in the remaining five patients. Aneurysm clipping (39.2 %; 95 % CI, 32.8–45.9), parenchymal lesion debulking (27.2 %; 95 % CI, 21.6–33.6), and lobectomies (22.4 %; 95 % CI, 17.3–28.6) were the procedures most frequently associated with RCH.
About 6.2 % of RCH (13/209; 95 % CI, 3.6–10.3) occurred, instead, after supratentorial craniectomy or burr holes.
Clinical onset and timing
The clinical status after RCH was described in 197 out of 209 patients (94.5 %). In 57 cases (28.9 %; 95 % CI, 23.0–35.6) RCH was incidentally discovered on postoperative imaging with no associated symptoms; in 88 cases (44.6 %; 95 % CI, 37.9–51.6), it was associated with impairment of consciousness, in 25 (12.6 %; 95 % CI, 8.7–18.0) with cerebellar signs, in 17 (8.6 %; 95 % CI, 5.4–13.3) with seizures, and in 10 (5 %; 95 % CI, 2.7–9.0) evolved in a comatose state.
Timing of the clinical onset was reported in 152 out of 209 patients (72.7 %): 48 (31.5 %; 95 % CI, 24.7–39.3) showed symptoms immediately after surgery, 72 (47.3 %; 95 % CI, 39.5–55.2) within 24 h, 22 (14.4 %; 95 % CI, 9.7–20.9) between 24 and 72 h, and 10 (6.5 %; 95 % CI, 3.6–11.6) later than 72 h from surgery. Overall, 80.4 % (95 % CI, 73.1–86.0) of patients had a clinical onset during the first postoperative day.
RCH characteristics
RCH pattern was reported in 194 out of 209 patients (92.8 %): 126 showed a zebra sign (64.9 %; 95 % CI, 58.0–71.3), 36 an ICH (18.5 %; 95 % CI, 13.7–24.6), and 32 (16.4 %; 95 % CI, 11.9–22.3) a mixed pattern (Fig. 1).
The side of the RCH was reported in 205 out of 209 patients (98 %): 113 were bilateral (55.1 %; 95 % CI, 48.2–61.7), and 92 unilateral (44.9 %; 95 % CI, 38.2–51.7). Among them, 42 (20.4 %; 95 % CI, 15.5–26.5) were omolateral to the supratentorial craniotomy, 45 (21.9 %; 95 % CI, 16.8–28.1) were contralateral, and 5 were located at the midline (2.4 %; 95 % CI, 1.0–5.5). Bilateral localization was about four times more frequent among patients with zebra pattern (Fig. 1).
Treatment and clinical outcome
Data on treatment were reported in 207 out of 209 patients (99 %). Clinical observation was the strategy adopted in 157 cases (75.8 %; 95 % CI, 69.5–81.1); 27 patients (13 % 95 % CI, 9.1–18.3) who showed a progressive impairment of consciousness due to the appearance of hydrocephalus underwent EVD, whereas 23 (11.1 %; 95 % CI, 7.5–16.1) who showed a significant mass effect with cerebellum and brainstem distortion underwent SD. Among the latter, 16/23 (69.5 %) showed ICH or mixed bleeding.
Outcome at discharge was reported in 179 out of 209 cases (85.6 %). According to the GOS, 134 patients (74.8 %; 95 % CI, 68.0–80.6) had a good outcome, whereas 45 (25.1 %; 95 % CI, 19.3–31.9) had a poor outcome. There was no significant difference in mean GOS at discharge between studies reporting less or more than ten cases. A trend of progressive GOS improvement over time was instead evident stratifying the outcome according to the year of publication, with a significant difference between studies published before and after 2001 (Table 1).
Outcome at follow-up (mean 5.2 ± 10 months) was reported in less than half of patients (91 out of 209; 43.5 %): among them, 88 (96.7 %; 95 % CI, 90.7–98.8) showed a good outcome and 3 (3.3 %; 95 % CI, 1.1–9.2) a poor outcome. Twenty-one patients died during postoperative course (11.7 %; 95 % CI, 7.8–17.2). Regardless of the associated procedure, mortality was mainly (17 out of 21 cases, 80.9 %) due to cerebellar ICH causing severe brainstem compression.
Relationship among demographics, RCH characteristics, treatment, and outcome
Table 2 shows the relationship among sex, mean age, RCH characteristics, clinical onset, treatment, and outcome at hospital discharge.
Among the 179 patients whose outcome at discharge was reported, data regarding age were available in 176 (98.3 %), sex in 177 (98.8 %), timing of RCH appearance in 122 (68.1 %), clinical status in 171 (95.5 %), bleeding pattern in 168 (93.8 %), side of hemorrhage in 171 (95.5 %), and mode of treatment in 175 (97.7 %).
Univariate analysis showed that older patients had a significantly worse outcome (p ≤ 0.0001), whereas sex did not seem to affect the prognosis. Ninety-five percent of patients who presented asymptomatic at onset had a good prognosis (p = 0.0006), whereas the timing of RCH appearance did not show association with outcome. Patients showing zebra pattern had a significantly more frequent good outcome (p = 0.0001), inspite of the fact that the majority underwent no surgical treatment. On the other hand, patients showing a pure ICH had a significantly poorer outcome (p = 0.0002). Finally, bilateral localization did not appear to be necessarily related to a worse prognosis.
Risk factors
Percentages of incidence and 95 % CI of potential risk factors are reported in Table 3.
A history of hypertension or epilepsy was reported in approximately one fourth of patients (56/209, 26.7 %, and 49/209, 23.4 %, respectively). About 19.1 % of patients (40/209) were taking antiplatelet/anticoagulant drugs approximately within a week before surgery. Nearly 13.4 % (28/209), instead, suffered from pathologies potentially impairing the coagulation (deficit of factors/platelet, hematologic tumors, radiochemotherapy, anemia, alcohol addiction, chronic kidney failure, etc.).
Perioperative seizures and hypertension peaks were the complications most frequently reported in association with RCH (32/209, 15.3 %, and 28/209, 13.3 %, respectively). Also, hydrocephalus was reported in 10.5 % of patients (22/209) with RCH and pneumocephalus in about 8.1 % (17/209). Finally, thrombotic/hemorrhagic complications occurred in less than 5 % of cases (10/209).
Surgical maneuvers responsible for prolonged CSF leakage, such as the placement of epidural drainages, were performed in approximately one fourth of patients (52/209); a spinal drainage was placed in almost 14 % (29/209); a ventricular/subdural catheter in 11 % (23/209). Overall, at least one drainage was present in about 34 % of patients (71/209).
The presence of at least one risk factor (cumulative risk) for impaired coagulation, hypertension, or seizures was present in about one third of patients (70/209, 33.4 %, and 72/209, 34.3 %), respectively. In particular, assumption of antiplatelet/anticoagulant drugs and factors impairing coagulation appeared significantly associated with poor outcome (Table 2).
Multivariate analysis
A logistic regression model, considering poor outcome at discharge as dependent variable and zebra pattern, symptomatic onset, antiplatelet/anticoagulant intake, and age as covariates, confirmed that symptomatic onset, intake of antiplatelet/anticoagulant drugs, and older age were independently associated with poor outcome (Table 4). Factors potentially impairing coagulation other than antiplatelet/anticoagulant drugs were excluded from the multivariate analysis, as it was postulated that they may have contributed to altering the coagulation properties. Likewise, the surgical treatment was excluded as the majority of patients were managed conservatively and surgery was reserved for only those who showed a more severe clinical picture. Contrariwise, the zebra sign appeared as a more benign hemorrhagic pattern (Table 4). However, when the year of publication was added to the statistical model as an additional covariate, the zebra pattern no more appeared as a significant variable.
Since all significant predictors of good/poor outcome on univariate analysis showed a decreasing trend in their association strength over time, we also built a second model of multivariate analysis only including studies published after 2001. In this new model, only symptomatic onset and advanced age appeared as significant predictors of poor outcome.
Sensitivity for predicting poor outcome was 36 % and specificity was 94.4 %. The PPV was 60.0 % and the NPV of 86.4 %. The ROC curve analysis calculated for these two variables presented an area under the curve of 0.845 (95 % CI, 0.77–0.92).
Discussion
This review shows that RCH after supratentorial craniotomies is a complication more frequently reported for IA clipping, tumors’ resection, and lobectomies for focal epilepsy. Overall, these results reflect those observed in the largest series published in literature [11, 16, 20] and support the hypothesis that procedures with greater CSF leakage have higher risk of postoperative RCH. The main RCH pattern has been in fact described as a predominantly subarachnoid bleeding, which probably originates from ruptured veins as they course through the cerebellar fissure or where they enter the cerebellar parenchyma. An excessive CSF leakage, in fact, may cause cerebellum shift, thus resulting in stretching and tearing of these bridging veins [32, 33]. In contrast with this hypothesis, the majority of patients who have a pattern of zebra hemorrhage do not show associated parenchymal infarction, which would be expected after interruption of these veins [11].
RCH was an incidental finding on postoperative imaging in more than one third of cases (37 %), while in the remaining two thirds, it was associated with progressive impairment of consciousness or cerebellar signs; rapid progression toward coma was found in only a minority of patients.
Hence, RCH represents a fairly benign condition, with good outcome in almost three fourths of all patients (74.8 %, 95 % CI, 68.0–80.6) and in more than 85 % of those with the zebra pattern (85.2 %; 95 % CI, 77.1–90.8).
However, the overall mortality rate reported after RCH is not negligible (11.7 %), but if we consider only that observed in patients with the zebra pattern, the rate is significantly lower (about 1.5 %). Accordingly, zebra hemorrhage and ICH could represent two different nosological entities which do not share the same pathophysiology. Compared to pure ICH, in fact, the zebra pattern appears three times more frequent, usually bilateral, and characterized by a significantly better outcome.
This study also reveals that the influence of bleeding pattern on outcome appears progressively reduced over time, probably due to advances in neurosurgical and intensivistic management.
With regard to possible etiological risk factors, this review shows that alterations of coagulation, hypertensive status, and perioperative CSF drainages are described in more than one third of patients with postoperative RCH, respectively. However, the frequency of a previous history of hypertension in these patients does not significantly differ from that of the general population with the same mean age. Also, since most of the surgical procedures associated with RCH were elective, we could expect that the majority of patients had suspended the anticoagulant/antiplatelet drugs at least a week before surgery. Thus, the association with this factor could only reflect a more general relationship with cardiovascular risk factors.
Finally, this review does not provide sufficient information to validate other different pathophysiological hypotheses, such as the role of the intraoperative head rotation and its influence on jugular outflow [11, 41, 45], or the Papanastassiou’s hypothesis, which proposes that RCH would preferentially occur contralateral to the supratentorial craniotomy as this part of cerebellum, due to CSF leakage, moves posteriorly to abut the transverse sinus, kinking, and obstructing the veins draining from the superior aspect of the hemisphere [36]. In fact, in patients with unilateral RCH (about 42 %), we observed that the percentages of hemorrhages omolateral and contralateral to the side of the craniotomy were approximately the same.
Also, these data cannot certainly establish if the high percentage of RCH reported in patients with a previous history of epilepsy only reflects an association with the procedures of lobectomy or if the occurrence of perioperative seizures (also undetected) may cause venous congestion and subarachnoid bleeding.
Similarly, the relatively high frequency of RCH among patients who underwent large tumor resections only partially corroborates the hypothesis of Konig et al., who suggested that removal of supratentorial space occupying masses may induce a reduction of intracranial pressure and an associated critical increase of transmural venous pressure causing bleeding [25].
This study presents several limitations. First of all, 18 of the included papers were case reports and 18 were case series reporting less than five patients. Also, the reported evidence is observational and noncomparative; in fact, data regarding the denominator were lacking in the majority of the analyzed studies. Therefore, the proportions reported in this review only reflect the published cases and may be influenced by some form of publication bias. On the other hand, the stratification of outcomes according to the sample size did not show significant differences, therefore limiting the impact of a possible selection bias. However, we cannot exclude that the severity of the underlying disease, in addition to the occurrence of a RCH, has affected the outcomes (including mortality) in some cases. In fact, it is noteworthy that the mean percentage of good outcome among patients with RCH has increased over time maybe due to the introduction of a better management, being limited to about 50 % until 2000 and constantly around 80 % in the papers published since 2001 (Table 1).
Moreover, data regarding the variables and short-term outcomes we investigated were not available for all patients and the reported percentages were assessed in subgroups. However, these data were accessible in approximately 90 % of patients we considered. Instead, data regarding follow-up were available only in 43.5 % out of patients and they did not include a reliable evaluation of long-term prognosis.
Furthermore, in regard to patients with ruptured IA, neither it was possible to differentiate the contribution of a the previous SAH on the postoperative RCH, nor its influence on outcome.
Finally, risk factors analyzed in this study has showed a NPV of only 86.4 %, and a PPV not exceeding 60 %.
However, this study has some strengths. We followed a comprehensive systematic review process and extracted all available demographic, clinical, and neuroradiological data in order to improve the knowledge about the RCH characteristics and the associated risk factors. Moreover, so far, this is the only systematic review on this topic.
Conclusions
RCH after supratentorial craniotomy is a fairly benign and frequently self-limiting condition, particularly when it occurs in younger patients and shows a zebra hemorrhage pattern. The presence of ICH, instead, may result in a more severe clinical picture. All available clinical and neuroradiologial data suggest a venous origin of the bleeding. The role of coagulation disorders, perioperative CSF drainages, and hypertension as possible risk infactors appears limited, since their incidence does not exceed about one third out of the reported cases, respectively.
In the opinion of most authors, RCH usually does not require surgical treatment except for cases associated with hydrocephalus or progressive deterioration of consciousness.
The correct interpretation of this hemorrhagic complication far from the field of surgery is therefore mandatory to plan a prolonged clinical surveillance and to identify those cases which may potentially evolve and result in severe neurological impairment.
References
Amini A, Osborn AG, McCall TD, Couldwell WT (2006) Remote cerebellar hemorrhage. AJNR Am J Neuroradiol 27:387–390
Baeesa SS (2012) Remote cerebellar hemorrhage in neurosurgery. Neurosciences (Riyadh) 17:305–308
Bilginer B, Oguz KK, Akalan N, Spencer DD (2008) Remote cerebellar hemorrhage and iliofemoral vein thrombosis after supratentorial craniotomy. Neurocrit Care 8:283–285
Bokhari R, Baeesa S (2012) Remote cerebellar hemorrhage due to ventriculoperitoneal shunt in an infant: a case report. J Med Case Rep 30:222
Borkar SA, Lakshmiprasad G, Sharma BS, Mahapatra AK (2013) Remote site intracranial haemorrhage: a clinical series of five patients with review of literature. Br J Neurosurg 27:735–738
Brisman MH, Bederson JB, Sen CN, Germano IM, Moore F, Post KD (1996) Intracerebral hemorrhage occurring remote from the craniotomy site. Neurosurgery 39:1114–1121
Brockmann MA, Groden C (2006) Remote cerebellar hemorrhage: a review. Cerebellum 5:64–68
Brockmann MA, Nowak G, Reusche E, Russlies M, Petersen D (2005) Zebra sign: cerebellar bleeding pattern characteristic of cerebrospinal fluid loss. Case Rep J Neurosurg 102:1159–1162
Chalela JA, Monroe T, Kelley M, Auler M, Bryant T, Vandergrift A et al (2006) Cerebellar hemorrhage caused by remote neurological surgery. Neurocrit Care 5:30–34
Chitale R, Tjoumakaris S, Gonzalez F, Dumont AS, Rosenwasser RH, Jabbour P (2013) Infratentorial and supratentorial strokes after a cranioplasty. Neurologist 19:17–21
Cloft HJ, Matsumoto JA, Lanzino G, Cail WS (1997) Posterior fossa hemorrhage after supratentorial surgery. AJNR 18:1573–1580
Clusmann H, Kral T, Marin G, Van Roost D, Swamy K, Schramm J (2004) Characterization of hemorrhagic complications after surgery for temporal lobe epilepsy. Zentralbl Neurochir 65:128–134
De Paola L, Troiano AR, Germiniani FM, Coral P, Della Coletta MV et al (2004) Cerebellar hemorrhage as a complication of temporal lobectomy for refractory medial temporal epilepsy: report of three cases. Arq Neuropsiquiatr 62:519–522
Dincer A, Özcan Ü, Kaya D, Usseli MI, Erzen C, Pamir MN (2012) Asymptomatic remote cerebellar hemorrhage: CT and MRI findings. Cerebellum 11:880–886
Figueiredo EG, de Amorim RL, Teixeira MJ (2009) Remote cerebellar hemorrhage (zebra sign) in vascular neurosurgery: pathophysiological insights. Neurol Med Chir (Tokyo) 49:229–233
Friedman JA, Piepgras DG, Duke DA, McClelland RL, Bechtle PS, Maher CO et al (2001) Remote cerebellar hemorrhage after supratentorial surgery. Neurosurgery 49:1327–1340
Gelfenbeyn M, Vasil’ev S, Krylov V (2001) Cerebellar haemorrhage after supratentorial aneurysm surgery with lumbar drainage. Neurosurg Rev 24:214–219
Hara T, Matsuda M, Watanabe S, Nakai K, Yamamoto T, Matsumura A (2013) Remote Cerebellar Hemorrhage after Removal of a Supratentorial Glioma without Perioperative CSF Loss: A Case Report. Case Rep Surg 2013:305039
Honegger J, Zentner J, Spreer J, Carmona H, Schulze-Bonhage A (2002) Cerebellar hemorrhage arising postoperatively as a complication of supratentorial surgery: a retrospective study. J Neurosurg 96:248–254
Huang CY, Lee PH, Lin SH, Chuang MT, Sun YT, Hung YC, Lee EJ (2012) Remote cerebellar hemorrhage following supratentorial craniotomy. Neurol Res 34:422–429
Hyam JA, Turner J, Peterson D (2007) Cerebellar haemorrhage after repeated burr hole evacuation for chronic subdural haematoma. J Clin Neurosci 14:83–86
Jang J-W, Joo S-P, Kim J-H, Kim S-H (2006) Remote Cerebellar Hemorrhage after Supratentorial Aneurysmal Surgery: Report of Six Cases. J Korean Neurosurg Soc 39:370–373
Kaplan SS, Lauryssen C (1999) Cerebellar haemorrhage after evacuation of an acute supratentorial subdural haematoma. British J Neurosurg 13:329–331
Koller M, Ortler M, Langmayr J, Twerdy K (1999) Posterior-Fossa Haemorrhage After Supratentorial Surgery ± Report of Three Cases and Review of the Literature. Acta Neurochir (Wien) 141:587–592
König A, Laas R, Herrmann HD (1987) Cerebellar haemorrhage as a complication after supratentorial craniotomy. Acta Neurochir (Wien) 88:104–108
Kuroda R, Nakatani J, Akai F, Sato M, Kataoka K, Isaka T et al (1994) Remote subarachnoid haemorrhage in the posterior fossa following supratentorial surgery. Clinical observation of 6 cases. Acta Neurochir (Wien) 129:158–165
Lehmann P, Salioub G (2011) Remote cerebellar haemorrhage. Eur J Radiol Extra 77:e29–e33
Li D, Fu C, Xu D, Sun L, Yu W, Zhao C (2013) Remote peritentorial hemorrhage complicating supratentorial aneurysmal surgery: a report of three cases and literature review. Acta Neurochir (Wien) 155:271–276
Mandonnet E, Faivre B, Bresson D, Cornelius J, Guichard JP, Houdart E et al (2010) Supratentorial craniotomy complicated by an homolateral remote cerebellar hemorrhage and a controlateral perisylvian infarction: case report. Acta Neurochir (Wien) 152:169–172
Marquardt G, Setzer M, Schick U, Seifert V (2002) Cerebellar hemorrhage after supratentorial craniotomy. Surg Neurol 57:241–251
Maruyama T, Ishii K, Isono M, Abe T, Fujiki M, Kobayashi H (2004) Remote cerebellar hemorrhage following supratentorial craniotomy-case report. Neurol Med Chir (Tokyo) 44:294–297
Matsushima T, Rhoton AL, de Oliveira E, Peace D (1983) Microsurgical anatomy of the veins of the posterior fossa. J Neurosurg 59:63–105
Matsushima T, Suzuki SO, Fukui M, Rhoton AL Jr, de Oliveira E, Ono M (1989) Microsurgical anatomy of the tentorial sinuses. J Neurosurg 71:923–928
Miranda P, Alén JF, Rivas J, Pérez A, Ramos A (2005) Cerebellar hematoma following transsphenoidal surgery. Acta Radiol 46:184–186
Modesti LM, Hodge CJ, Barnwell ML (1982) Intracerebral hematoma after evacuation of chronic extracerebral fluid collections. Neurosurgery 10:689–693
Papanastassiou V, Kerr R, Adams C (1996) Contralateral cerebellar hemorrhagic infarction after pterional craniotomy: report of five cases and review of the literature. Neurosurgery 39:841–851
Park JS, Hwang JH, Park J, Hamm IS, Park YM (2009) Remote cerebellar hemorrhage complicated after supratentorial surgery: retrospective study with review of articles. J Korean Neurosurg Soc 46:136–143
Paul J, Jhaveri MD, Lewis SL (2011) Teaching neuroimages: remote cerebellar hemorrhage following resection of a supratentorial tumor. Neurology 77:e82–e83
Rezazadeh A, Rohani M, Tahamy SA (2011) Remote cerebellar hemorrhage. Arch Iran Med 14:292–293
Sasani M, Ozer AF, Oktenoglu T, Karaarslan E, Sasani H, Kaner T (2009) Remote cerebellar hemorrhage following resection of a supratentorial tumor: a case report. Cases J 2:7299
Seoane E, Rhoton AL Jr (1999) Compression of the internal jugular vein by the transverse process of the atlas as the cause of cerebellar hemorrhage after supratentorial craniotomy. Surg Neurol 51:500–505
Siu TL, Chandran KN, Siu T (2003) Cerebellar haemorrhage following supratentorial craniotomy. J Clin Neurosci 10:378–384
Smith R, Kebriaei M, Gard A, Thorell W, Surdell D (2014) Remote cerebellar hemorrhage following supratentorial cerebrovascular surgery. J Clin Neurosci 21:673–676
Srikijvilaikul T, Deesudchit T (2007) Cerebellar hemorrhage after supratentorial surgery for treatment of epilepsy: report of two cases. J Med Assoc Thai 90:1221–1224
Toczek MT, Morrell MJ, Silverberg GA, Lowe GM (1996) Cerebellar hemorrhage complicating temporal lobectomy. Rep Four Cases J Neurosurg 85:718–722
Tucker A, Miyake H, Tsuji M, Ukita T, Nishihara K (2007) Remote cerebellar hemorrhage after supratentorial unruptured aneurysmal surgery: report of three cases. Neurol Res 29:493–499
van Calenbergh F, Goffin J, Plets C (1993) Cerebellar hemorrhage complicating supratentorial craniotomy: report of two cases. Surg Neurol 40:336–338
Vogels RL, Verstegen MJ, van Furth WR (2006) Cerebellar haemorrhage after non-traumatic evacuation of supratentorial chronic subdural haematoma: report of two cases. Acta Neurochir (Wien) 148:993–996
Waga S, Shimosaka S, Sakakura M (1983) Intracerebral hemorrhage remote from the site of the initial neurosurgical procedure. Neurosurgery 13:662–665
Yacubian EM, de Andrade MM, Jorge CL, Valério RM (1999) Cerebellar hemorrhage after supratentorial surgery for treatment of epilepsy: report of three cases. Neurosurgery 45:159–162
Yang BP, Yang CW (2005) Remote cerebellar hemorrhage after craniotomy. Pediatr Neurosurg 41:52–53
Yasargil MG, Yonekawa Y (1977) Results of microsurgical extra-intracranial arterial bypass in the treatment of cerebral ischemia. Neurosurgery 1:22–24
Yoshida S, Yonekawa Y, Yamashita K, Ihara I, Morooka Y (1990) Cerebellar hemorrhage after supratentorial craniotomy--report of three cases. Neurol Med Chir (Tokyo) 30:738–743
Ziyal I, Bilginer B, Yavuz K, Turk C, Ozgur C, Benli K (2012) Does ventricular opening promote remote cerebellar haemorrhage? Turk Neurosurg 22:102–104
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Sources of funding
The authors did not receive any funding in conjunction with the generation of this manuscript.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Comments
Adam Tucker, Osaka, Japan
The authors are to be commended for conducting perhaps the largest review to date including an analysis of 209 patients in 49 articles published during 1977 to 2013. Although many of the findings served to confirm results from prior reviews, this study was unique in that it provided a precise statistical analysis of patient characteristics, risk factors, and outcomes. Of note, better outcomes were observed both in studies published after 2001, probably reflecting recent advances in management, and with the zebra pattern (1.5 % mortality), which was usually bilateral. In contrast, there was an overall 11.7 % mortality, with 80.9 % due to brainstem compression from intracerebellar hemorrhage (ICH). Multivariate logistic regression analysis showed that symptomatic onset, antiplatelet/anticoagulation medication, and older age were independently associated with poor outcome, while in univariate analysis timing of remote cerebellar hemorrhage (RCH) appearance, bilateral localization, and sex were unrelated. Because the respective incidences of coagulation disorders, perioperative CSF drainage, and hypertension did not exceed one third of the cases, these risk factors were considered to play a relatively limited etiological role.
RCH is rare postoperative neurosurgical and orthopedic complication with as yet unknown etiology, however, possibly because of recent advances in both neuroimaging and interventional therapy, this entity is beginning to confront neurologists and stroke specialists as well. Aside from a report of two cases of remote cerebellar hemorrhage from the site of craniotomy published in 2015, which found multiple foci of hemorrhage as an additional adverse prognostic factor, there have been few new studies, especially ones pertaining to the etiology of remote cerebellar hemorrhage. However, recent indirect investigations on post-stroke remote cerebral hemorrhage, in particular a 2014 large prospective cohort, found that previous stroke and higher age were independently associated with remote parenchymal hemorrhage, which occurred in 2.2 % (970) of patients from a total group of 43,494 patients treated with intravenous recombinant tissue-type plasminogen activator. Thus, in addition to classical mechanical factors related to CSF over-drainage, cerebellar sag and venous bleeding or hypertensive parenchymal bleeding factors, these data, as well as neuroimaging diagnostic advances in microbleeds, tend to suggest the possibility of previously unconsidered multiple histopathological conditions such as cerebral amyloid angiopathy (CAA), small vessel microangiopathic processes, and other age-related hemorrhagic and or ischemic contributing factors. Prospective studies with incorporation of susceptibility-weighted imaging or other modalities including tissue diagnosis would be useful for clarifying issues of causative mechanisms, prognosis, and could possibly lead to new treatment avenues.
Currently, there are no established guidelines for management of post-procedural remote cerebellar hemorrhage, though recent reports have recommended preventative measures, such as perioperative blood pressure control, management of coagulopathies, avoidance of excessive CSF drainage and inadvertent durotomies, as well as adequate CSF replacement with watertight closure. Finally, although the authors took the ambitious task of dividing remote hemorrhage into a two part review (remote hemorrhage after supratentorial and spinal procedures), it may be constructive to address the relations between the two phenomena within the second part of their review.
References
1. Das KK, Nair P, Mehrotra A, Sardhara J, Sahu RN, Jaiswal AK, Kumar R (2014) Remote cerebellar hemorrhage: Report of 2 cases and review of literature. Asian J Neurosurg. Jul-Sep;9(3):161–4.
2. Gao Y, Churilov L, Teo S, Yan B (2015) Remote intracerebral haemorrhage post intravenous thrombolysis: experience from an Australian stroke centre. J Clin Neurosci. Feb;22(2):352–6.
3. Mazya MV, Ahmed N, Ford GA, Hobohm C, Mikulik R, Nunes AP, Wahlgren N (2014) Remote or extraischemic intracerebral hemorrhage—an uncommon complication of stroke thrombolysis: results from the safe implementation of treatments in stroke-international stroke thrombolysis register. Stroke. Jun;45(6):1657–63.
4. Shiau EL, Yip CM, Fu JH, Lai PH (2013) Remote intracranial parenchymal hemorrhage in susceptibility-weighted imaging. QJM. Jul;106(7):677–8.
5. Shoamanesh A, Yan S, Charidimou A (2015) New Cerebral Microbleeds and Mechanism of Post-Thrombolysis Remote Intracerebral Hemorrhage: "Red Meets White" Revisited. Front Neurol. Sep 15;6:203.
6. Stuart MJ, Tsahtsarlis A, Amato D, Pattavilakom A (2015) Remote cerebellar haemorrhage from site of craniotomy: A report of two cases. Br J Neurosurg. Aug 27:1–3. [Epub ahead of print]
Jack Jallo, Philadelphia, USA
Dr. Sturiale and his group have written an interesting review paper regarding remote cerebellar hemorrhage after supratentorial procedures, describing the incidence of a relatively under recognized complication in neurosurgery. We hope that this paper will help to shed light on this unpredictable complication and further the community’s understanding for the sake of future treatment and prevention.
Rights and permissions
About this article
Cite this article
Sturiale, C.L., Rossetto, M., Ermani, M. et al. Remote cerebellar hemorrhage after supratentorial procedures (part 1): a systematic review. Neurosurg Rev 39, 565–573 (2016). https://doi.org/10.1007/s10143-015-0691-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-015-0691-6