Abstract
Expandable vertebral body replacement cages (VBRs) have been widely used for reconstruction of the thoracolumbar spine following corpectomy. However, their use in the cervical spine is less common, and currently, no expandable cages on the market are cleared or approved by the US Food and Drug Administration for use in the cervical spine. The objective of this study was to perform a systematic review on the use of expandable cages in the treatment of cervical spine pathology with a focus on fusion rates, deformity correction, complications, and indications. A comprehensive Medline search was performed, and 24 applicable articles were identified and included in this review. The advantages of expandable cages include greater ease of implantation with less risk of damage to the end plate, less intraoperative manipulation of the device, and potentially greater control over lordosis. They may be particularly advantageous in cases with poor bone quality, such as patients with osteoporosis or metastatic tumors that have been radiated. However, there is a potential risk of overdistraction, which is increased in the cervical spine, their minimum height limits their use in cases with collapsed vertebra, and the amount of hardware in the expansion mechanism may limit the surface area available for fusion. The use of expandable VBRs are a valuable tool in the armamentarium for reconstruction of the anterior column of the cervical spine with an acceptable safety profile. Although expandable cervical cages are clearly beneficial in certain clinical situations, widespread use following all corpectomies is not justified due to their significantly greater cost compared to structural bone grafts or non-expandable VBRs, which can be utilized to achieve similar clinical outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A cervical corpectomy is most commonly required for decompression of the anterior spine in the treatment of degenerative spondylosis, trauma, primary or metastatic tumors, osteomyelitis, kyphosis or deformity, and ossification of the posterior longitudinal ligament (OPLL). Following corpectomy, reconstruction of the anterior column is required, and various approaches have been used previously.
The use of expandable cages has been described in the literature for over 10 years, but their more popular use has been in posterolateral approaches to the thoracolumbar spine and their use in the cervical spine has been limited [13, 14, 32–34]. Several expandable vertebral body replacement (VBR) devices have previously been cleared as class II devices through the 510(k) pathway for use in the thoracolumbar spine. However, currently, there are no US Food and Drug Administration (FDA) cleared or approved expandable VBR devices for use in the cervical spine. The telescopic plate spacer (TPS) (Biomet Spine, Broomfield, CO) VBR system previously received a Humanitarian Device Exemption approval from the FDA for reconstruction of C3-T2 following surgery for tumors but has since been withdrawn from the market. As such, the other devices described in the literature represent off-label use, and all current use of expandable cages in the cervical spine in clinical practice is off-label use.
The objective of this study was to systematically review the use of expandable cages in the treatment of cervical spine pathology, with a focus on fusion rates, deformity correction, complications, and indications, to help guide surgeons in clinical practice.
Methods
A comprehensive search was conducted using Medline with an attempt to identify all relevant studies documenting the use of expandable cages in the cervical spine. A MEDLINE search was conducted using the search terms “expandable cage,” “expandable vertebral body replacement,” “expandable VBR,” “distractable cage,” “distractable vertebral body replacement,” “distractable VBR,” “distractible cage,” “distractible vertebral body replacement,” OR “distractible VBR,” from January 1, 1990 to October 31, 2014, as expandable cages were not used before this time. The same search terms were then used in a Google Scholar search. Studies describing case reports, case series, retrospective reviews, prospective observational studies, and prospective controlled trials were included, though no prospective controlled trials were identified. Using these search terms, 165 manuscripts were identified. Articles not including cervical spine use and not in English were excluded. Following these exclusions, 24 relevant studies were identified, 20 of which provided clinical data. The citations of the relevant studies were also reviewed, but no further studies meeting the inclusion and exclusion criteria were identified.
Results
A summary of the relevant studies is provided in Table 1 [1–4, 6–10, 23, 27, 29, 30, 36, 38–40, 42, 45, 46]. The manuscripts were grouped based on the type of expandable VBR used. The different VBRs that have been reported in the literature, used in the cervical spine, include the ADD (Ulrich Medical, Germany), ADDplus (Ulrich Medical, Germany), Cervilift (Deltacon GmbH, Werneck, Germany), Synex ECC (Depuy Synthes Spine; Raynham, MA), Tecorp-C (Scient’x-Alphatec Spine, Carlsbad, CA), the Osteotech VBR (Osteotech, Eatontown, New Jersey), and the TPS. The use of the ADD or ADDplus were reported in nine studies, the Synex in two studies, the Tecorp-C in three studies, the TPS in two studies, the cervilift in one study, the Osteotech in one study, and the cage used was not specified in four studies. All patients either had additional placement of an anterior plate, posterior supplemental fixation, both, or a VBR with incorporated anterior fixation such as the ADDplus or TPS was used, except for two patients treated in the study by Alfieri et al. [1] with a VBR alone.
In total, expandable VBRs were used in the cervical spine in 333 patients. The most common indication was degenerative spondylosis, with trauma, osteomyelitis, tumor, deformity, and OPLL also commonly reported. The VBRs were used for reconstruction of one level in 130 patients, two levels in 86 patients, three levels in 19 patients, four levels in 3 patients, and the number of levels was not specified for 95 patients.
Although fusion rates were not reported in eight studies, fusion assessment was generally made by demonstrating no motion on flexion-extension radiographs. Four studies used CT scans for fusion assessment. Using these criteria, reported fusion rates ranged from 79 to 100 % at follow-up of 9–41 months. Nine studies examined sagittal alignment following cage placement and reported improvements in cervical lordosis of 4°–22°.
Subsidence was the most common adverse event noted, and the reported rates of subsidence were 0–43 %, although subsidence predominantly did not require surgical revision. Surgical revision was required for one patient who was a smoker after excessive end plate removal [30]. Arts and Peul [2] reported the highest subsidence rate, at 43 %, with a 20 % reoperation rate for hardware failure, and all these cases involved placement of the TPS device.
Other reported complications included adjacent segment vertebral body fractures requiring surgical revision, transient C5 palsy from overdistraction of the cage, dysphagia that was typically transient, durotomy, and esophageal injury.
Discussion
Over the past 10 years, the use of expandable cages for reconstruction of the cervical spine after corpectomy has increased dramatically. To the best of our knowledge, this is the first manuscript to systematically review the use of expandable or distractible vertebral body replacement devices in the cervical spine.
The classic gold standard for reconstruction of the anterior column of the cervical spine has been tricortical iliac crest autograft, which has a high fusion rate, but has a high complication rate with significant donor site morbidity, with complications or morbidity in up to 90 % [15, 18]. In a recent review, a 19 % complication rate was reported for the iliac crest donor site, with complications including infection, hematoma, fracture, and scarring [12]. Although the use of structural allograft has mitigated some of the these complications, another strategy has been to use fixed cages made out of materials such as titanium mesh, PEEK, or carbon fiber. Lied et al. [26] performed a prospective, non-randomized trial comparing autograft and PEEK interbody cages for anterior cervical discectomy and fusion (ACDF) and found similar clinical outcomes between the two methods, but significant donor site morbidity for the autograft group.
A disadvantage of non-expandable VBRs is that ideal placement can be challenging. These fixed devices or grafts typically are produced with fixed sizes and end plate angles, and the cage must be modified intraoperatively for the ideal fit. If the device is trimmed, it is critical that it is positioned in the correct rotation or a worsening kyphosis could result. The non-expandable VBRs must be tamped into place, and this can potentially lead to increased distraction forces on the vertebral end plates with an increased risk of damage to the end plate and cage subsidence. This risk of end plate damage can also result if the cage must be removed or repositioned intraoperatively. Furthermore, it can be more challenging to improve lordosis with the fixed VBRs.
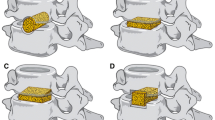
A major advantage of expandable VBRs for cervical spine reconstruction is that the device can be placed easily in its non-expanded state. Although this is potentially more beneficial for posterolateral placement in the thoracolumbar spine, this theoretically reduces the risk of damage to adjacent structures in the neck and potentially reduces the risk of damage to the vertebral end plates during placement. Additionally, the devices are usually provided in a modular system with a range of core diameters (typically 12–16 mm are used in the cervical spine), heights, endcap footprint, size, shape, and angle. This wide range of available options provides significant versatility for the surgeon in creating an ideally sized and contoured construct for the corpectomy defect. The VBRs are typically constructed from titanium, but some variants made of PEEK are available as well. Figure 1 demonstrates representative computed tomography (CT) and radiographs of both titanium and PEEK devices. Additionally, many of the devices are designed for supplementation with an anterior plate or posterior fixation, while some have an incorporated anterior fixation system.
Representative images of cervical expandable cages. a Sagittal CT scan and b lateral radiograph of two-level titanium (radiopaque) cage and anterior plate reconstruction following C7-T1 corpectomy. c Sagittal CT scan and d lateral radiograph of two-level PEEK (radiolucent) cage and anterior plate reconstruction following C5-6 vertebrectomy
The majority of the studies were case series or retrospective reviews solely reporting the results of expandable cage use; only a single group compared the outcomes when using a distractible cage with the use of structural autograft and a fixed PEEK cage [23]. While fusion rates and sagittal alignment were not assessed, they found that there were similar neurologic outcomes regardless of the reconstruction used, though the static PEEK cage had significantly more subsidence than the other two groups.
Biomechanics and supplemental fixation
The cervical spine has a unique biomechanical profile compared to the thoracolumbar spine with significant flexion/extension, lateral bending, axial rotation, and compression/distraction [5, 11]. Additionally, it lacks the support of the rib cage found in the thoracic spine.
Given its unique biomechanics, a major concern with the use of expandable cages is overdistraction of the cage, which could result in neurologic injury or structural damage. In intact human cadavers, Yoganandan et al. [44] applied tensile loads to failure and found a mean failure load of 3.4 kN at a mean distraction of 21.3 mm. They also found that the cervical spine was most sensitive to axial tensile loads, particularly at C6-7, as an explanted O-T3 spine had a significantly lower mean failure load at 1.6 kN at a distraction of 27.1 mm. These data indicate that excessive expansion of the cage with resulting injury is easier in the cervical spine, as a greater distraction is achieved at a significantly lower force. Although no catastrophic failures of the spinal column have been reported in the literature due to overdistraction, two cases of neurologic injury have been reported. For instance, Arts and Peul [2] described a patient with transient C5 palsy from excessive cage distraction, while Shen et al. [34] reported a case with a lumbar nerve root injury from excessive expansion of the cage.
Although expandable VBRs do have several advantages over fixed devices or structural bone grafts, they have not been shown to have a substantially different biomechanical profile. For instance, Kandziora et al. [20] studied the biomechanics of the Synex-C expandable cage in both titanium and PEEK and compared it with tricortical autograft and a titanium mesh cage in a C4 cadaveric corpectomy model. The goal of the reconstruction was to restore the preoperative height. The implants were tested alone, with an anterior plate, and with anteroposterior supplemental fixation. No differences in range of motion or stiffness were noted between the expandable and non-expandable devices, but the expandable cage had a significantly lower motion and higher stiffness than structural autograft in rotation. Adding an anterior plate significantly decreased range of motion and increased stiffness compared to a stand-alone implant for all three types of reconstruction, and adding additional posterior supplemental fixation significantly decreased range of motion further, with up to 102 % greater stiffness than the anterior plate alone. However, this model only assessed a one-level reconstruction, and no angulation of the device end plates was used.
An additional type of fixation included the cages such as the ADDplus or TPS which incorporated anterior fixation screws into the cage. While no biomechanical data is available on these devices, they typically had similar subsidence and fusion rates to the ADD cage with an anterior plate. However, Cabraja et al. [8] reported an 11 % pseudoarthrosis rate requiring revision with the ADD plus and increased subsidence compared to the ADD cage with an anterior plate.
A different study assessed the effects of different fixation combinations in a two-level cervical corpectomy model with a structural allograft reconstruction [35]. They found that combined anterior plating and posterior fixation as well as posterior fixation alone were significantly more rigid than anterior plating alone. However, there was no difference between anterior-posterior supplementation and posterior fixation alone. Similarly, Koller et al. [22] studied the effects of different fixation combinations in a two-level cervical corpectomy model with a distractible cage reconstruction. They found that anterior plating alone had significantly greater range of motion in flexion-extension, lateral bending, and axial rotation than lateral mass screw posterior fixation alone or combined anterior plating and lateral mass screw fixation. The 360° construct was statistically similar to the lateral mass screw only construct except in axial rotation for which the 360° had significantly less motion. These differences have been observed clinically as well, as a 9 % failure rate was observed when a two-level corpectomy was reconstructed with only anterior plate supplementation, and this increased to a 50 % failure rate for a three-level corpectomy reconstructed with only anterior plate supplementation [37].
The substantial improvement in fixation from adding an anterior plate and/or posterior supplementation indicates that even for a one-level corpectomy, some types of supplemental fixation should be used. This was the case in the reviewed literature as all patients had placement of an anterior plate and/or posterior fixation except for two patients. In our own practice, we typically use only an anterior plate for a one-level corpectomy, while for a two-level corpectomy, additional posterior supplemental fixation is often required if there is poor bone quality, especially in patients with metastatic disease. We believe that a VBR spanning three or four levels requires posterior supplementation to allow for adequate construct stability.
Fusion
A concern when using expandable cages is that they may have a lower fusion rate than either structural bone grafts or hollow cages. The large footprint of the expansion system may limit the surface area for fusion at the end plate and may limit the amount of bone graft that can be placed within the cage. A CT scan depicting the channel used for bone graft is presented in Fig. 2. However, in the reviewed manuscripts, based on a combination of flexion-extension radiographs and CT scans, reported fusion rates in the cervical spine for single and multilevel fusions ranged from 79 to 100 % at follow-up of 9–41 months. While it is possible that using CT scans in all of the studies would have yielded lower fusion rates, the results are not substantially different than prior reported literature for structural bone grafts and fixed cages [16, 24, 43, 47].
While fusion rate is a concern following treatment for most spine pathology, it is less of a concern in the treatment of metastatic tumors. For these patients, expandable cages may be an important option as the bone quality is often poor with prior radiation, and some of the concerns for fusion limitations are mitigated due to the patient’s limited lifespan.
Sagittal alignment
An additional advantage of the expandable cages is their improvement of cervical lordosis. Of the studies identified in this review, nine examined sagittal alignment following cage placement and reported improvements in cervical lordosis of 4°–22°. Although no studies compare the effect on lordosis and segmental height of expandable and fixed devices in the cervical spine, several comparative studies have been performed in the thoracolumbar spine. Eleraky et al. [14] compared the effects of expandable and fixed cages following thoracolumbar burst fractures and found that the expandable cages had a mean kyphotic angle correction of 17.5° postoperatively, while the fixed cages had a mean kyphotic angle correction of 14.5° postoperatively. In a separate study comparing expandable cages with polymethylmethacrylate reconstruction following posterior extracavitary corpectomy for thoracolumbar spine metastases, there was a trend toward a reduction in kyphosis for the expandable cage group [13]. Furthermore, Sciubba et al. reported that expandable titanium cages allowed for a 53 % reduction in kyphosis following thoracic vertebrectomy from a posterior approach. Similarly, Sasani et al. [32] described a reduction in thoracic kyphosis and increased lumbar lordosis following reconstruction with an expandable cage following posterior corpectomy for thoracolumbar burst fractures. Although a study is needed to directly compare the effects of expandable versus fixed cages on cervical lordosis, expandable cages generally allowed for a gain in cervical lordosis for both single and multilevel constructs.
Subsidence
Subsidence of the cage is a widely recognized complication both in interbody cages and VBR cages and has been observed at all levels of the spine, although it is not always clinically significant. While rates of subsidence ranged from 0 to 43 % for the patients described in this review, only two studies described patients that required surgical revision. In the first study, the patient with clinically significant subsidence was a smoker and the authors reported excessive removal of the end plate prior to cage placement [30]. The second study reported a 43 % subsidence rate with a 20 % hardware failure rate, which was substantially higher than reported in the other studies. All of the cases requiring revision involved a TPS expandable cage which has a rectangular shape that requires very accurate end plate preparation for proper placement of the device. These cases highlight the importance of proper surgical technique with judicious preparation of the end plates to minimize the risk of subsidence regardless of the implant used.
Biomechanically, several factors may predispose the patient to an increased risk of subsidence. Biomechanical studies simulating normal neck movement with 700 cycles of loading in random directions on fixed vertebral bodies separated by an interbody cage have found increased rates of subsidence up to 1.6 mm for a porous titanium cage [21, 41]. Additionally, Hasegawa et al. [17] found that the end plate-cage interface strength was improved with increasing diameter that better matched the end plate size and that the interface strength was improved with better bone mineral density. Similarly, Jost et al. [19] indicated that the failure load of the end plate cage was more dependent on bone mineral density than cage design in a lumbar interbody model. Furthermore, using a finite element analysis, Polikeit et al. [31] demonstrated that the insertion of a cage changed the normal loading and that the stress was concentrated at the contact point of the cage rather than spread more uniformly across the entire end plate as in the native disc-end plate interface. Finally, in a recent study, another group studied the effect of angular mismatch between the cage and the end plate by cyclically loading constructs with a Synex expandable cage at mismatch angles from 0° to 30°. They observed a significant increase in subsidence with each 10° increase in angular mismatch, thus demonstrating the importance of making sure that the cage end plates are flush against the vertebral body end plate [28].
Showing clinical correlation, Konig and Spetzger [23] found a 32 % subsidence rate when using fixed lordotic PEEK cages for reconstruction following single or multilevel cervical corpectomies, while no subsidence was noted for the expandable cage group (ADDplus) or iliac crest structural autograft group. Contrarily, Lau et al. [25] compared subsidence rates between static and expandable cages throughout the spine in a retrospective cohort analysis and found that expandable cages had an increased odds ratio of subsidence at 1 and 12 months, and there was an increased risk of subsidence at 1 month with osteomyelitis, footplate-to-body ratio <0.5, no posterior fusion or fusion <2 levels above and below the corpectomy. The use of prongs on the cage end plate decreased the risk of subsidence. However, they did not study subsidence rates in the cervical spine separately, and multiple different models of both static and expandable cages were clustered together in the cohorts, so it is unclear if there is an increased risk at different levels of the spine or with certain types of cages.
Given these considerations, expandable cages may offer an advantage in that their modularity and adjustability will make it easier to fit flush against the end plate, and the different end plate footprints may allow for a more uniform stress distribution across the end plate. This will be particularly important in patients with poor bone quality such as patients with osteoporosis or with metastatic disease after prior radiation, who are predisposed to subsidence.
Adjacent segment injury
There have been several reports of adjacent segment vertebral body fractures in the early postoperative period. Zairi et al. [45] described a patient who underwent a C5 corpectomy with an anterior plate but presented 1 month postoperatively with neck pain and right arm weakness and was found to have a C6 fracture with hardware migration and increasing kyphosis. A C6 corpectomy was performed, and an expandable titanium cage was again used with an anterior plate. His sagittal alignment remained stable over the following 2 years, but his right arm weakness did not resolve.
Additionally, Chou et al. [9] presented a case series documenting adjacent segment vertebral body fractures in four patients, two of which involved the cervical spine. One patient had severe myelopathy from degenerative spondylosis and underwent C4-5 corpectomies with an expandable cage and anterior plate reconstruction. However, on postoperative day 1, a C3 fracture was noted and a C3 corpectomy was performed. A longer expandable cage with an anterior plate was then used for the reconstruction. The second patient had a kyphotic deformity following radiation for a foramen magnum meningioma and underwent a C4-6 corpectomy with an expandable cage and anterior plate reconstruction. Posterior supplemental fixation was planned during the hospitalization, but on postoperative day 1, it was noted that the hardware had migrated and a C7 vertebral body fracture was present. A C7 corpectomy was performed. and a longer expandable cage with an anterior plate and posterior supplemental fixation was used.
The authors hypothesized that there were three possible reasons for the adjacent segment fractures noted in their patients. First, the patients had osteoporosis which likely predisposed them to the fracture. Second, the cages can be placed securely without the cage flush against the end plate, due to their expandable design. This would potentially create a stress riser as it would focus the force on the small area of contact rather than spread it throughout the end plate. Finally, the design of the devices allows for substantial force generation with distraction of the spinal segment and compression of the adjacent vertebral body, although these forces have not been quantified in the literature. Given this possible complication, great care must be exercised when placing the devices to verify that the cage is flush with the end plate and to be judicious in the expansion of the cage.
Additional limitations
Although expandable cages offer several advantages over fixed cages, there are some limitations in addition to the smaller surface area for fusion, the added risk of overdistraction with neurologic injury, and the risk of adjacent segment fracture. Although the ADD device has a minimum height of 10 mm, most of the expandable VBRs have a minimum height around 20 mm which may preclude their use in reconstruction of a collapsed vertebral body commonly seen with tumors, osteomyelitis, or trauma. On the other hand, fixed cages and structural bone grafts are available down to much smaller heights as they are also used as interbody devices. Additionally, there is an additional potential failure mechanism with collapse of the expansion device itself. While this is unlikely given the substantially greater stiffness of the devices compared to the vertebral body and this was not reported in any of the reviewed manuscripts, it does represent a theoretical concern when using these devices.
Conclusions
Based on this systematic review, the use of expandable VBRs are a valuable tool in the armamentarium for reconstruction of the anterior column of the cervical spine with an acceptable safety profile. Their predominant advantage is greater ease of implantation with less risk of damage to the end plate, less intraoperative manipulation of the device, and potentially greater control over lordosis. They may be particularly advantageous in cases with poor bone quality, such as patients with osteoporosis or metastatic tumors that have been radiated, as their modularity and customization may allow for less localized stress transfer to the vertebral body and better matching of the end plate angulation to minimize subsidence. Despite their advantages, there is a potential risk of overdistraction, which is increased in the cervical spine, their minimum height limits their use in cases with collapsed vertebra, and the amount of hardware in the expansion mechanism limits the surface area available for fusion. Although expandable cervical cages are clearly beneficial in certain clinical situations, widespread use following all corpectomies is not justified due to their significantly greater cost compared to structural bone grafts or non-expandable VBRs, with similar clinical outcomes.
References
Alfieri A, Gazzeri R, Neroni M, Fiore C, Galarza M, Esposito S (2011) Anterior expandable cylindrical cage reconstruction after cervical spinal metastasis resection. Clin Neurol Neurosurg 113(10):914–917. doi:10.1016/j.clineuro.2011.02.023
Arts MP, Peul WC (2008) Vertebral body replacement systems with expandable cages in the treatment of various spinal pathologies: a prospectively followed case series of 60 patients. Neurosurgery 63(3):537–544. doi:10.1227/01.NEU.0000325260.00628.DC, discussion 544–535
Auguste KI, Chin C, Acosta FL, Ames CP (2006) Expandable cylindrical cages in the cervical spine: a review of 22 cases. J Neurosurg Spine 4(4):285–291. doi:10.3171/spi.2006.4.4.285
Ayhan S, Palaoglu S, Geyik S, Saatci I, Onal MB (2014) Concomitant intramedullary arteriovenous malformation and a vertebral hemangioma of cervical spine discovered by a pathologic fracture during bicycle accident. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deformity So Eur Sect Cervical Spine Res Soc. doi:10.1007/s00586-014-3620-4
Bogduk N, Mercer S (2000) Biomechanics of the cervical spine. I: Normal kinematics. Clin Biomech 15(9):633–648
Burkett CJ, Baaj AA, Dakwar E, Uribe JS (2012) Use of titanium expandable vertebral cages in cervical corpectomy. J Clin Neurosci Off J Neurosurg Soc Australas 19(3):402–405. doi:10.1016/j.jocn.2011.07.030
Cabraja M, Abbushi A, Koeppen D, Kroppenstedt S, Woiciechowsky C (2010) Comparison between anterior and posterior decompression with instrumentation for cervical spondylotic myelopathy: sagittal alignment and clinical outcome. Neurosurg Focus 28(3):E15. doi:10.3171/2010.1.FOCUS09253
Cabraja M, Abbushi A, Kroppenstedt S, Woiciechowsky C (2010) Cages with fixation wings versus cages plus plating for cervical reconstruction after corpectomy—is there any difference? Cen Eur Neurosurg 71(2):59–63. doi:10.1055/s-0029-1246135
Chou D, Lu DC, Weinstein P, Ames CP (2008) Adjacent-level vertebral body fractures after expandable cage reconstruction. J Neurosurg Spine 8(6):584–588. doi:10.3171/SPI/2008/8/6/584
Coumans JV, Marchek CP, Henderson FC (2002) Use of the telescopic plate spacer in treatment of cervical and cervicothoracic spine tumors. Neurosurgery 51(2):417–424, discussion 424–416
Cusick JF, Yoganandan N (2002) Biomechanics of the cervical spine 4: major injuries. Clin Biomech 17(1):1–20
Dimitriou R, Mataliotakis GI, Angoules AG, Kanakaris NK, Giannoudis PV (2011) Complications following autologous bone graft harvesting from the iliac crest and using the RIA: a systematic review. Injury 42(Suppl 2):S3–S15. doi:10.1016/j.injury.2011.06.015
Eleraky M, Papanastassiou I, Tran ND, Dakwar E, Vrionis FD (2011) Comparison of polymethylmethacrylate versus expandable cage in anterior vertebral column reconstruction after posterior extracavitary corpectomy in lumbar and thoraco-lumbar metastatic spine tumors. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deformity Soc Eur Sect Cervical Spine Res Soc 20(8):1363–1370. doi:10.1007/s00586-011-1738-1
Eleraky MA, Duong HT, Esp E, Kim KD (2011) Expandable versus nonexpandable cages for thoracolumbar burst fracture. World Neurosurg 75(1):149–154. doi:10.1016/j.wneu.2010.09.018
Epstein NE (2012) Iliac crest autograft versus alternative constructs for anterior cervical spine surgery: Pros, cons, and costs. Surg Neurol Int 3(Suppl 3):S143–S156. doi:10.4103/2152-7806.98575
Han YC, Liu ZQ, Wang SJ, Li LJ, Tan J (2014) Is anterior cervical discectomy and fusion superior to corpectomy and fusion for treatment of multilevel cervical spondylotic myelopathy? A systemic review and meta-analysis. PLoS One 9(1):e87191. doi:10.1371/journal.pone.0087191
Hasegawa K, Abe M, Washio T, Hara T (2001) An experimental study on the interface strength between titanium mesh cage and vertebra in reference to vertebral bone mineral density. Spine 26(8):957–963
Heneghan HM, McCabe JP (2009) Use of autologous bone graft in anterior cervical decompression: morbidity & quality of life analysis. BMC Musculoskelet Disord 10:158. doi:10.1186/1471-2474-10-158
Jost B, Cripton PA, Lund T, Oxland TR, Lippuner K, Jaeger P, Nolte LP (1998) Compressive strength of interbody cages in the lumbar spine: the effect of cage shape, posterior instrumentation and bone density. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deformity So Eur Sect Cervical Spine Res Soc 7(2):132–141
Kandziora F, Pflugmacher R, Schaefer J, Scholz M, Ludwig K, Schleicher P, Haas NP (2003) Biomechanical comparison of expandable cages for vertebral body replacement in the cervical spine. J Neurosurg 99(1 Suppl):91–97
Kettler A, Wilke HJ, Claes L (2001) Effects of neck movements on stability and subsidence in cervical interbody fusion: an in vitro study. J Neurosurg 94(1 Suppl):97–107
Koller H, Schmidt R, Mayer M, Hitzl W, Zenner J, Midderhoff S, Graf N, Resch H, Wilke HJ (2010) The stabilizing potential of anterior, posterior and combined techniques for the reconstruction of a 2-level cervical corpectomy model: biomechanical study and first results of ATPS prototyping. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deformity So Eur Sect Cervical Spine Res Soc 19(12):2137–2148. doi:10.1007/s00586-010-1503-x
Konig SA, Spetzger U (2014) Distractable titanium cages versus PEEK cages versus iliac crest bone grafts for the replacement of cervical vertebrae. Minim Invasive Ther Allied Technol MITAT Off J Soc Minim Invasive Ther 23(2):102–105. doi:10.3109/13645706.2013.854809
Konig SA, Spetzger U (2014) Experience with a modular PEEK system for cervical vertebral body replacement. J Spinal Disord Tech. doi:10.1097/BSD.0000000000000149
Lau D, Song Y, Guan Z, La Marca F, Park P (2013) Radiological outcomes of static vs expandable titanium cages after corpectomy: a retrospective cohort analysis of subsidence. Neurosurgery 72(4):529–539. doi:10.1227/NEU.0b013e318282a558, discussion 528–529
Lied B, Roenning PA, Sundseth J, Helseth E (2010) Anterior cervical discectomy with fusion in patients with cervical disc degeneration: a prospective outcome study of 258 patients (181 fused with autologous bone graft and 77 fused with a PEEK cage). BMC Surg 10:10. doi:10.1186/1471-2482-10-10
Lu DC, Wang V, Chou D (2009) The use of allograft or autograft and expandable titanium cages for the treatment of vertebral osteomyelitis. Neurosurgery 64(1):122–129. doi:10.1227/01.NEU.0000336332.11957.0B, discussion 129–130
Mohammad-Shahi MH, Nikolaou VS, Giannitsios D, Ouellet J, Jarzem PF (2013) The effect of angular mismatch between vertebral endplate and vertebral body replacement endplate on implant subsidence. J Spinal Disord Tech 26(5):268–273. doi:10.1097/BSD.0b013e3182425eab
Omeis I, Bekelis K, Gregory A, McGirt M, Sciubba D, Bydon A, Wolinsky JP, Gokaslan Z, Witham T (2010) The use of expandable cages in patients undergoing multilevel corpectomies for metastatic tumors in the cervical spine. Orthopedics 33(2):87–92. doi:10.3928/01477447-20100104-12
Payer M (2006) Implantation of a distractible titanium cage after cervical corpectomy: technical experience in 20 consecutive cases. Acta Neurochir 148(11):1173–1180. doi:10.1007/s00701-006-0871-9, discussion 1180
Polikeit A, Ferguson SJ, Nolte LP, Orr TE (2003) Factors influencing stresses in the lumbar spine after the insertion of intervertebral cages: finite element analysis. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deformity So Eur Sect Cervical Spine Res Soc 12(4):413–420. doi:10.1007/s00586-002-0505-8
Sasani M, Ozer AF (2009) Single-stage posterior corpectomy and expandable cage placement for treatment of thoracic or lumbar burst fractures. Spine 34(1):E33–E40. doi:10.1097/BRS.0b013e318189fcfd
Sciubba DM, Gallia GL, McGirt MJ, Woodworth GF, Garonzik IM, Witham T, Gokaslan ZL, Wolinsky JP (2007) Thoracic kyphotic deformity reduction with a distractible titanium cage via an entirely posterior approach. Neurosurgery 60(4 Suppl 2):223–230. doi:10.1227/01.NEU.0000255385.18335.A8, discussion 230–221
Shen FH, Marks I, Shaffrey C, Ouellet J, Arlet V (2008) The use of an expandable cage for corpectomy reconstruction of vertebral body tumors through a posterior extracavitary approach: a multicenter consecutive case series of prospectively followed patients. Spine J Off J N Am Spine So 8(2):329–339. doi:10.1016/j.spinee.2007.05.002
Singh K, Vaccaro AR, Kim J, Lorenz EP, Lim TH, An HS (2003) Biomechanical comparison of cervical spine reconstructive techniques after a multilevel corpectomy of the cervical spine. Spine 28(20):2352–2358. doi:10.1097/01.BRS.0000085344.22471.23, discussion 2358
Thongtrangan I, Balabhadra RS, Le H, Park J, Kim DH (2003) Vertebral body replacement with an expandable cage for reconstruction after spinal tumor resection. Neurosurg Focus 15(5):E8
Vaccaro AR, Falatyn SP, Scuderi GJ, Eismont FJ, McGuire RA, Singh K, Garfin SR (1998) Early failure of long segment anterior cervical plate fixation. J Spinal Disord 11(5):410–415
Viswanathan A, Abd-El-Barr MM, Doppenberg E, Suki D, Gokaslan Z, Mendel E, Rao G, Rhines LD (2012) Initial experience with the use of an expandable titanium cage as a vertebral body replacement in patients with tumors of the spinal column: a report of 95 patients. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deformity So Eur Sect Cervical Spine Res Soc 21(1):84–92. doi:10.1007/s00586-011-1882-7
Waschke A, Kaczor S, Walter J, Duenisch P, Kalff R, Ewald C (2013) Expandable titanium cages for anterior column cervical reconstruction and their effect on sagittal profile: a review of 48 cases. Acta Neurochir 155(5):801–807. doi:10.1007/s00701-013-1655-7, discussion 807
Waschke A, Walter J, Duenisch P, Kalff R, Ewald C (2013) Anterior cervical intercorporal fusion in patients with osteoporotic or tumorous fractures using a cement augmented cervical plate system: first results of a prospective single-center study. J Spinal Disord Tech 26(3):E112–E117. doi:10.1097/BSD.0b013e3182764b37
Wilke HJ, Kettler A, Goetz C, Claes L (2000) Subsidence resulting from simulated postoperative neck movements: an in vitro investigation with a new cervical fusion cage. Spine 25(21):2762–2770
Woiciechowsky C (2005) Distractable vertebral cages for reconstruction after cervical corpectomy. Spine 30(15):1736–1741
Xiao SW, Jiang H, Yang LJ, Xiao ZM (2014) Anterior cervical discectomy versus corpectomy for multilevel cervical spondylotic myelopathy: a meta-analysis. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deformity So Eur Sect Cervical Spine Res Soc. doi:10.1007/s00586-014-3607-1
Yoganandan N, Pintar FA, Maiman DJ, Cusick JF, Sances A Jr, Walsh PR (1996) Human head-neck biomechanics under axial tension. Med Eng Phys 18(4):289–294
Zairi F, Aboukais R, Thines L, Allaoui M, Assaker R (2012) Relevance of expandable titanium cage for the treatment of cervical spondylotic myelopathy. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deformity So Eur Sect Cervical Spine Res Soc 21(8):1545–1550. doi:10.1007/s00586-012-2380-2
Zhang HY, Thongtrangan I, Le H, Park J, Kim DH (2005) Expandable cage for cervical spine reconstruction. J Kor Neurosurg Soc 38:435–441
Zhang Y, Quan Z, Zhao Z, Luo X, Tang K, Li J, Zhou X, Jiang D (2014) Evaluation of anterior cervical reconstruction with titanium mesh cages versus nano-hydroxyapatite/polyamide66 cages after 1- or 2-level corpectomy for multilevel cervical spondylotic myelopathy: a retrospective study of 117 patients. PLoS One 9(5):e96265. doi:10.1371/journal.pone.0096265
Compliance with ethical standards
**This manuscript reflects the views of the authors and should not be construed to represent FDA’s views or policies.
Conflict of interest
Benjamin Elder has no conflict of interest.
Sheng-Fu Lo has no conflict of interest.
Thomas Kosztowski has no conflict of interest.
C. Rory Goodwin has no conflict of interest.
Timothy F. Witham receives research support from Eli Lilly & Co, The Johns Hopkins Neurological Pain Research Institute, and the Gordon and Marilyn Macklin Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Ziya L. Gokaslan, Baltimore, USA
In the article entitled "A systematic review of the use of expandable cages in the cervical spine," the authors present their findings after a systematic review of the literature on the use of expandable cages in cervical spine surgery, evaluating fusion rates, deformity correction, complications, and indications. The authors performed a Medline search and identified 24 relevant studies, of which 20 presented clinically relevant data. The studies included several expandable vertebral body replacements (VBRs), which are detailed. The 333 identified patients either had an additional anterior plate placed or posterior fixation, or both (two patients had stand-alone VBR only). The most common indication was degenerative spondylosis, in addition to trauma, osteomyelitis, tumor, deformity, and OPLL, with levels specified as one-level VBR in 130 patients, two levels in 86 patients, three levels in 19 patients, and four levels in 3 patients. At a follow up of 9–41 months, fusion rates ranged from 79 to 100 % and nine studies reported improvement in cervical lordosis of 4°–22°. Adverse events included subsidence in 0–43 % of cases, with other complications including vertebral body fractures, transient C5 palsy, dysphagia, durotomy, and esophageal injury. The authors conclude that expandable VBRs are a valuable option for reconstruction of the cervical anterior column, with an acceptable safety profile. Limitations of the study include the retrospective nature of the studies and lack of comparison cohorts. Only one study included comparison of cohorts with expandable VBR to other fixed reconstruction methods.
The authors are to be commended for providing a systematic review of the use of expandable VBRs in cervical spine surgery as an alternative to other methods such as autograft, allograft, and fixed cage use. They provide a larger cohort of patients for reporting of outcomes such as fusion rate, deformity correction, and complications associated with expandable VBRs, which can help further delineate their use in clinical practice. The use of expandable cages for anterior cervical reconstruction may become a good option for particular indications, such as patients undergoing surgery for tumor (where concerns for long-term fusion are less given lifespan) and deformity where further lordosis gained by expandable cages can be advantageous, though direct comparisons to fixed replacements are needed.
Rights and permissions
About this article
Cite this article
Elder, B.D., Lo, SF., Kosztowski, T.A. et al. A systematic review of the use of expandable cages in the cervical spine. Neurosurg Rev 39, 1–11 (2016). https://doi.org/10.1007/s10143-015-0649-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-015-0649-8