Abstract
Purpose
(1) Evaluate radiology resident perception of emergency radiology (ER). (2) Identify potential barriers to pursuing fellowship training or a career in ER among radiology residents.
Materials and methods
A 9-question digital survey was designed using Qualtrics Experience Management software (Qualtrics Inc., Provo, UT) and distributed to all US radiology residents via a multi-pronged distribution approach.
Results
Four hundred fifty-one residents responded out of an estimated national total of 4432 residents (10.2%). Gender proportion was nationally representative (female = 24.5%; p = 0.57), with a slight R1 predominance (p = 0.034). Of the residents, 88.8% were aware that an ER subspecialty exists, 82.0% were aware that ER fellowships exist, but only 51.7% were aware that the American Society of Emergency Radiology (ASER) exists. Nearly a quarter reported no ER division or ER resident rotation. Residents in a program without an ER division or rotation were nearly twice as likely to be unaware of the existence of ER subspecialty, ER fellowships, and ASER compared to others (p = 0.017). The presence of an ER division and rotation significantly increases the knowledge of ASER (65.5% vs. 40.7%, p < 0.001) and increases residents’ ratings of their ER training (p < 0.001). The following factors were ranked as the most important for fellowship choice: (1) personal interest, (2) intellectually stimulating, and (3) work hours. When asked if ER had an appealing work schedule, the mean response was 56 out of 100 (0 = disagree, 100 = agree).
Conclusion
US radiology residents with the greatest exposure to ER during residency are more familiar with ER training, ER career opportunities, and ASER and had a more favorable perception of the field. Subspecialty leaders should focus on ER’s inherent intellectual appeal and reframe its nontraditional schedule as positive (flexible).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Over the past several decades, subspecialty fellowship training in diagnostic radiology has grown in importance, with 90–95% of fourth-year radiology residents pursuing fellowship training [1,2,3]. Subspecialty selection is a complex decision-making process that itself has been the subject of prior research [4, 5]. To our knowledge, there is no literature specifically detailing resident interest in emergency radiology (ER) fellowship training or practice. Even resident awareness of the existence of ER and ER fellowships is far from universal, and not all publications examining the radiology fellowship selection process even include ER as a potential subspecialty of interest [3]. In fact, a recent report by Glover and Patel revealed that ER has the lowest representation in terms of number of training programs and fellowship positions offered of all radiology subspecialty training programs [6]. Consequently, since some residents are not even aware of ER as a fellowship option, they will look to other subspecialties for fellowship training. This reality has obvious and profound implications for the success of the field (Fig. 1).
The purpose of this study was to conduct a national survey to learn what residents know about ER fellowship opportunities, their perceptions of ER as a field and potential career option, and their familiarity with the American Society of Emergency Radiology (ASER) in an effort to uncover potential impediments to attracting candidates to the practice of ER [4]. Furthermore, we identify the most important factors radiology residents consider when selecting subspecialty training and, ultimately, future practice. These data will provide guidance in developing strategies to enhance the appeal of emergency radiology fellowship training and practice, particularly through leveraging the resources of ASER.
Materials and methods
Institutional review board approval was obtained for this study. An anonymous, 9-question digital survey was designed using Qualtrics Experience Management software (Qualtrics Inc., Provo, UT), based in part on the methods undertaken by Arnold et al. [4]. The digital survey was made available to all the US radiology residents via a multi-pronged distribution approach. The American Alliance of Academic Chief Residents in Radiology reviewed the survey and used their email listserv to distribute the survey to their members (with instructions to distribute the survey to all residents under their purview). Similarly, the Association of Program Coordinators in Radiology distributed the survey to their members. Reminders were sent after 1 week in all cases. Since this distribution approach would potentially result in duplicate receipt of the survey across different platforms, residents were instructed to complete the survey only once. The survey was conducted between March 1 and March 30, 2018. The estimated total number of the US radiology residents was compiled via retrospective public data available through the National Residency Matching Program [7]. All available data were included on a question-by-question basis; relevant n for observations within each analysis is provided in the results.
Descriptive and comparative statistical analysis was performed with R (The R Foundation). A variety of comparative statistical tests were used as appropriate to the variable subsets, including Chi-squared test, t tests, and Kolmogorov-Smirnov test for equality in distribution. A linear regression was created to predict the influence of “local ER Division and/or resident rotation” and “reading out with ER faculty” on residents’ rating of their ER training. Due to the non-normality of the residents rating of their ER training, an arcsine square root transformation of the ratings was performed (divided by 100 to be scaled between 0 and 1). Significance level was set at p < 0.05.
Results
Response rate and demographics
There were 451 resident responses (24.5% female) out of an estimated national total of 4432 residents, for a response rate of 10.2%. Responses were divided among residency levels: 30.6% R1, 24.9% R2, 23.4% R3, and 21.1% R4. The proportion of respondents differed by residency level (p = 0.034), in which the number of R1 respondents was somewhat higher than other levels, and R4 was somewhat lower. The proportion of women in our sample did not differ significantly from the national population (sample proportion = 0.245, national proportion = 0.258, p = 0.566), indicating a representative sample with respect to gender (approximately 25% female) [8]. The residents completing the survey were from across the USA, with the following geographic distribution: Northeast 23.1%, Southeast 13.2%, Mid-Atlantic 5.2%, Southwest 7.8%, Northwest 4.7%, Midwest 35.9%, West 10.1%.
Resident perceptions of the ER subspecialty and relationship to ER exposure during training
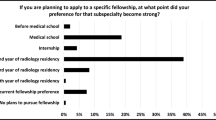
Of the respondents included in the data analysis, 88.8% were aware that an ER subspecialty exists, and 82.0% were aware that ER fellowships exist; however, only 51.7% were aware that ASER exists (for proportion of awareness based on level of training, see Fig. 1). As would be expected, 98.9% (360/364) of residents who were aware that ER fellowships exist were also aware of ER as a radiology subspecialty. Of the residents who were aware that ASER exists, 94.8% (217/229) were also ER-subspecialty- and fellowship-aware. Of residents who answered all three of these questions regarding awareness of ER as a subspecialty and fellowship option and of ASER (n = 444), only 48.9% (217) were aware of all the three entities (ER as a subspecialty, ER fellowships, and ASER), while 9.5% (n = 44) were aware of none. Of particular relevance to the position of ASER as the foremost advocacy organization for ER training and practice, 32.2% (n = 143) were ER-subspecialty- and fellowship-aware, but nonetheless did not know about the existence of ASER. While the vast majority of respondents have some formal training in ER and 57.8% reported that they read out with ER faculty at some point in their training, still over half (52.5%) train at institutions without a dedicated ER division (Fig. 2).
The proportion of residents who had no knowledge of ER as a subspecialty, ER fellowships, or ASER, was significantly higher in the group lacking both an ER division and an ER resident rotation compared to all other respondents (proportions = 0.157 and 0.074, respectively, p = 0.017). Conversely, the proportion of respondents who knew that ASER exists was significantly higher in the group with both an ER division and an ER resident rotation versus all other respondents (proportions = 0.655 and 0.407, p < 0.001).
Regarding the perceived quality of ER training during residency on a sliding scale from 0 to 100 (0 = non-existent, or poor; 100 = excellent), the mean response was 79.8 (SD = 22.2), with a range of 0–100 (median = 85, IQR = 75–95). There is no significant difference between the distribution of the responses in males and females (Kolmogorov-Smirnov test for equality in distribution using bootstrapped p values allowing for ties = 0.35), and their means were similar (mean of males = 80.5, mean of females = 78.4). When isolating residents who reported both “no ER division” and “no ER resident rotation” versus all other subjects and examining their rating of the question “ER is unique enough skill set to warrant it as a separate subspecialty,” we found that they report lower levels of agreement with this statement (p = 0.002, Kolmogorov-Smirnov test for equality distribution based on a bootstrapped p value).
A linear regression was created with the respondents’ ratings of their ER training as the dependent variable; the presence of an ER division and/or rotation and whether the resident read out cases with an ER faculty member were used as independent variables. The reference resident was at a program with neither an ER division nor rotation and who does not read out cases with ER faculty. Compared to the reference resident, those at an institution with both an ER division and ER resident rotation had significantly higher ratings of their ER training (p < 0.001), and, similarly, for ER rotation only (without an ER division) (p < 0.001). Ratings for respondents with an ER division only were higher than neither, but the difference was not significant (p = 0.12). The ratings from respondents who read out cases with an ER faculty member did not differ significantly from those who did not (p = 0.23).
Factors influencing fellowship choice
Residents were asked to rank eight factors influencing fellowship choice (Table 1). The factors most frequently ranked in the top three positions were as follows: personal interest, intellectually stimulating, and work hours.
Residents were asked to rate their agreement with four separate statements from 0 (completely disagree) to 100 (completely agree) with regard to their perception of ER that are presumed to be important in deciding whether to train in or practice ER; the four statements were as follows: “I am confident I could obtain a desirable job after any fellowship,” “I find the shift work nature and schedule of ER appealing,” “The skill set of ER is unique enough to warrant it as a separate subspecialty,” and “Compared to other subspecialties in radiology, ER has a significant impact on patient care.” Responses are graphically displayed as violin density plots (Fig. 3). The violin density plots are widest in areas of most frequent resident response for any given ranking. For example, at the “25” level, which indicates that residents relatively strongly disagreed with the statement in question, the widest plot is the “Appealing schedule” followed by the “ER subspecialty is warranted,” then “Desirable job,” and “ER impacts patient care”. These findings suggest that, while few residents disagree that ER impacts patient care, many perceive the work hours of ER practice to be undesirable, reflecting a potentially significant barrier to selecting ER training and, ultimately, practice.
A violin density plot of the resident responses: wider areas of each plot correspond to a relatively greater number of respondents providing a given rating. Red dots represent residents in programs with no ER division and no ER rotation. Residents were asked to rate their agreement with four separate statements from 0 (completely disagree) to 100 (completely agree) with regard to their perception of a career in ER. The full statements were as follows: “I am confident I could obtain a desirable job after any fellowship,” “I find the shift work nature and schedule of ER appealing,” “The skill set of ER is unique enough to warrant it as a separate subspecialty,” and “Compared to other subspecialties in radiology, ER has a significant impact on patient care.” Note that residents without formal ER exposure (no ER division or rotation) as represented by red dots tend to congregate in the lower range
Discussion
The data presented here provide important insights into what diagnostic radiology residents know about ER fellowship training, practice, and organized ER, and what factors they prioritize in selecting a subspecialty for fellowship training. The most fundamental observation about the first point is that resident knowledge of post-residency training and practice in ER was not universal, with more than one out of 10 being unaware that ER even exists as a unique subspecialty. Fewer still knew that ER fellowship training opportunities exist, and nearly one-half were unfamiliar with ASER. Another notable, but not unexpected, finding in our study is that residents at programs without a formal ER presence (ER division or rotation) tended to be particularly unaware of ER as a subspecialty, ER fellowship training, and ASER. Although nearly half of residents did not know of ASER, of those who did, a high percentage (94.8%) of them reported familiarity with training and career opportunities in the field, as one would anticipate. With respect to resident perception of their training experience in ER during residency, those at institutions with a formal ER presence had a more favorable opinion of their ER training experience than those without such representation. Furthermore, residents without an ER division or rotation were more likely than others to hold a relatively dim view of ER as a legitimate subspecialty.
These findings have clear implications for future ER subspecialty workforce projections: radiology residents without a positive experience in the subspecialty during residency or without formal ER representation at their residency programs are less likely to pursue, or even know about, ER fellowship training or, ultimately, practice. Turning our attention to the factors that residents take into account when selecting a subspecialty for fellowship, we found that “breadth of pathology” and “range of imaging modalities”—arguably the facets most characteristic of ER work—ranked relatively low on the list of resident preferences. These findings suggest that emphasizing head-to-toe, multimodality imaging of the broad range of pathology unique to ER to radiology residents who are undecided on subspecialty training may not be as impactful as might be expected. The subspecialty characteristics of being “intellectually stimulating” and concerning an “area of strong of personal interest” ranked as the top two most important factors in selecting a subspecialty in our survey. These observations are in keeping with those noted in the Arnold et al. study, which reported “area of strong personal interest” and “intellectual challenge” within the top three factors influencing fellowship selection for all respondents. Accordingly, to recruit residents into ER fellowship training and practice, the inherently “interesting” and “intellectually challenging” aspects of ER work need to be emphasized early in residency training. Of course, these facets of ER work are difficult to convey to trainees in programs without an ER division or resident rotation, and we have learned that such a presence is important in forming resident perceptions of the field. In fact, research published by Huang et al. reported that radiology residents rely on fellowship directors and current fellows in their subspecialty of choice in vetting fellowship programs [9]. This transmission of knowledge is most likely to take place when it occurs in-house. It is also noteworthy that, in the Huang et al. study, R1–R3 residents demonstrated relatively little interest in pursuing an ER fellowship (10%), superior to only nuclear medicine (6%) and neurointerventional (8%), and no R4 residents intended on entering an ER fellowship after residency. Expansion of ER divisions into residency training programs currently without one is, therefore, critical to both conveying ER subspecialty knowledge to residents as well as recruiting resident-candidates into ER fellowships and practice.
The matter of resident perception of ER work hours deserves special attention, as the shift work nature of ER practice, with 24-hour continuous coverage in some settings, is unique among the various diagnostic radiology subspecialties. Favorable work hours ranked in third position in our survey, but what is considered favorable to one resident might be unfavorable to another. Some might characterize ER coverage as potentially flexible and, therefore, distinctly appealing. For example, shifts may be regarded as modular and interchangeable, allowing for exchanges with a colleague at mutual convenience. With built-in extra time off to account for working in the evenings, overnight, and on weekends, individual schedules can be constructed ad lib to accommodate personal or professional interests. Emergency radiologists with children may be able to better divide household responsibilities with their partners than is otherwise possible when two income-earners keep traditional work hours. Alternatively, others may view the need to work outside of traditional daytime hours as disruptive, unhealthy, or otherwise onerous. It may be especially challenging to emphasize the positive aspects of ER practice to residents at institutions without an ER division, or whose sole experience with ER-type work arises out of call duty. If understaffed ER divisions are unable to offer the full complement of benefits inherent in shift work, they risk presenting an unsavory reflection of ER practice to residents, potentially discouraging them from pursuing an ER career trajectory. Prior research has identified that certain factors characteristic of ER practice, including cumulative night shift burden without commensurate recovery time, are associated with decreased emergency radiologist satisfaction [10]. Emergency medicine parallels emergency radiology in its dependence on shift work and the need for 24-7 coverage. Data from the emergency medicine literature emphasize the importance of careful attention to physician scheduling to ensure the success and longevity of emergency medicine careers; Rischall et al. reported that 98% of residents felt that shift schedule was a key factor in overall wellness [11, 12]. It is important for radiology departments to ensure that their emergency radiologists are afforded adequate compensation for working off-hours, especially in terms of time away from clinical duty. This not only ensures the well-being of ER faculty and sustainability of the ER division, but it also paints a more appealing picture of ER work to residents, who comprise the pool of potential ER fellows and radiologists.
Understanding resident perception of ER fellowship training and practice, and the factors they take into account when deciding on a subspecialty, comes at a particularly critical time in the evolution of the field. Imaging originating out of emergency departments in the US continues to rise despite a stabilization in medical imaging utilization from all sources combined, signaling a growing need for radiologists with subspecialty expertise in emergency and trauma imaging [13, 14]. The growing demand for ER-trained radiologists is reflected in a review of job postings with the American College of Radiology (ACR) Career Center over a period of 1 year from 2016 to 2017, revealing 78 postings specifically citing ER fellowship training as a requested qualification (authors’ unpublished data). Additional unpublished data from our group estimate that there are only between 10 and 20 conventional pathway ER fellows that complete training annually in the US, revealing a large gap between supply and demand. Our data provide some insight into why this gap exists, and which factors need to be addressed to narrow it. As the face of organized ER, ASER is best suited to ensure the expansion of the ER footprint in residency training programs in the US and, in so doing, advocate for the acceptance of the ER-division institutional model and a reframing of the ER practice schedule as flexible as opposed to burdensome. To achieve this goal, however, it must grow its recognition among residents beyond the current 51.7%.
Limitations
As with many national surveys, our primary limitation is the relatively low response rate. However, to mitigate this issue, we tested our respondent sample for representative fractions of gender and training year. It is possible that residents who took our survey were more likely to have strong opinions about ER; however, we anticipate this to be true for both favorable and unfavorable responses. Those residents who had no knowledge of ER (around 10%) may be underrepresented due to bias. Additionally, although residents were instructed to complete the survey only once, it is possible that residents could have completed the survey multiple times, skewing the data accordingly. The slight overrepresentation of R1s may bias the data in such a way as to overrepresent the proportion of respondents unfamiliar with ASER. While these data provide an overall view of the current landscape of ER fellowship selection and career interest in ER, the survey lacked a certain level of detail that would have allowed for a more informative assessment, such as the influence of specific institutional factors (e.g., Level 1 trauma center, ED volume, residency size, 24/7 faculty coverage, the presence of an ER fellowship); however, we did not include this level of detail in order to avoid lengthening the survey. These additional factors could potentially serve as areas of future investigation.
References
Goodman CJ, Lindsey JI, Whigham CJ, Robinson A (2000) Diagnostic radiology residents in the classes of 1999 and 2000: fellowship and employment. AJR Am J Roentgenol 174(5):1211–1213
Shetty SK, Venkatesan AM, Foster KM, Galdino GM, Lawrimore TM, Davila JA (2005) The radiology class of 2005: postresidency plans. J Am Coll Radiol 2(10):852–858
Baker SR, Luk L, Clarkin K (2010) The trouble with fellowships. J Am Coll Radiol 7(6):446–451
Arnold RW, Goske MJ, Bulas DI, Benya EC, Ying J, Sunshine JH (2009) Factors influencing subspecialty choice among radiology residents: a case study of pediatric radiology. J Am Coll Radiol 6(9):635–642
Gay SB, Resnik CS, Harolds JA, Yousem DM, Lemley DE (2003) The radiology fellowship and fellowship match: current status. Acad Radiol 10(3):303–308
Glover M, Patel TY (2016) The radiology fellowship arms race cannot be won. J Am Coll Radiol 13(4):461–464
National Resident Matching Program. Results and data: main residency match [available from: http://www.nrmp.org/report-archives/
Hammer MM, Shetty AS, Cizman Z, McWilliams SR, Holt DK, Gould JE et al (2015) Results of the 2015 survey of the American alliance of academic chief residents in radiology. Acad Radiol 22(10):1308–1316
Huang J, Patel S, Scruggs R, Levin D (2017) In pursuit of fellowship: results from a 2016 survey of US trainees. Curr Probl Diagn Radiol
Hanna TN, Shekhani H, Lamoureux C, Mar H, Nicola R, Sliker C, Johnson JO (2017) Emergency radiology practice patterns: shifts, schedules, and job satisfaction. J Am Coll Radiol 14(3):345–352
Emergency Physician Shift Work (2017) Ann Emerg Med 70(6):947–948
Rischall ML, Chung AS, Tabatabai R, Doty C, Hart D (2018) Emergency medicine resident shift work preferences: a comparison of resident scheduling preferences and recommended schedule design for shift workers. AEM Educ Train 2(3):229–235
Larson DB, Johnson LW, Schnell BM, Salisbury SR, Forman HP (2011) National trends in CT use in the emergency department: 1995–2007. Radiology 258(1):164–173
Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R (2010) Trends and characteristics of US emergency department visits, 1997–2007. JAMA 304(6):664–670
Funding
The authors (TNH, KDH) are recipients of the 2017–2018 American Society of Emergency Radiology Educational Grant, which was used, in part, to fund this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
IRB statement
This study was reviewed and approved by our institutional IRB.
Conflicts of interests
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Herr, K.D., Risk, B. & Hanna, T.N. Diagnostic radiology resident perspectives on fellowship training and career interest in emergency radiology. Emerg Radiol 25, 653–658 (2018). https://doi.org/10.1007/s10140-018-1633-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-018-1633-8