Abstract
Purpose
To investigate if the presence of systemic inflammatory response syndrome (SIRS) in patients with urinary tract obstruction at time of presentation to the emergency department correlates with a subsequent positive urine culture and to determine if it could be used as a tool to predict the urgency of a percutaneous nephrostomy (PCN). The secondary aim of the study was to assess the incidence of in-hour and after-hour emergent PCNs performed in a tertiary center which has both interventional radiological and urological expertise.
Methods and materials
Emergent adult PCN cases referred from the emergency department between 2011 and 2016 were identified retrospectively. Urine culture results, clinical features of SIRS, timing of procedure, and radiological findings were analyzed.
Results
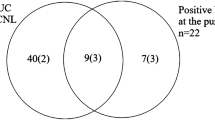
A total of 110 patients met the inclusion criteria. There were a total of 60 male and 50 female patients with a mean age of 62 (age range 18–99 years). Ninety-two (83%) PCN patients were referred and performed on after-hours with the remaining 18 patients performed in-hours. There were 53 (48%) patients that met the criteria for obstruction with SIRS and 57 (52%) patients with obstruction without SIRS. The number of after-hours PCN performed in both groups was equal at 46 patients each. The most common cause of obstruction in the SIRS group was stone related in 31 (58%) patients. Whereas, the most common cause of obstruction in the non-SIRS group was due to malignancy in 26 (45%) cases. An elevated temperature and heart rate were the most common features of SIRS at 96 and 83% respectively in the SIRS group. An organism was isolated in 35 (67%) out of the 52 urine culture results obtained for the SIRS group. No organism was isolated in 42 (95%) out of the 44 urine culture results obtained in the non-SIRS group. Statistical analysis using Fisher’s test revealed that the association between obstruction without SIRS and a negative urine culture result was statistically significant (p < 0.0001).
Conclusion
A large percentage (50%) of PCN cases performed after-hours could have been performed during daytime hours instead due to the absence of infection. This would be in line with the practices of some centers that consider an infected obstructed kidney as the only absolute indication for emergent decompression overnight. The study also demonstrates that the absence of a SIRS in a patient with urinary tract obstruction correlates well with a negative urine culture result from the nephrostomy specimen which has a high negative predictive value for excluding pyonephrosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary tract obstruction is the hindrance of normal urine flow that can happen anywhere along the urinary tract between the kidneys and the urethral meatus. This can be due to calculi, tumors, strictures, or anatomical abnormalities via an extrinsic or intrinsic process which invariably lead to hydronephrosis.
There is no comprehensive published epidemiological data available on the incidence of urinary tract obstruction as it varies with different population groups. In an emergency department setting, it is extrapolated that the annual incidence of urolithiasis is 16 per 10,000 population [1]. Urolithiasis has been described as the most common cause of upper urinary tract obstruction in adults, followed by pelvic malignancies [2].
The two main complications of new onset urinary tract obstruction are infection and acute renal failure. The management of this is prompt decompression of the obstructed collecting systems.
The European Association of Urology recommends that either percutaneous nephrostomy (PCN) or retrograde stent insertion is appropriate for decompression and that choice should be guided by local expertise and resources [3]. PCN is an emergent radiological intervention that was first described by Goodwin in 1955 [4] as a procedure for temporary urinary drainage. A needle is used to access the renal pelvis under ultrasound or fluoroscopic guidance through the skin in order to insert a catheter to allow drainage of urine from the obstructed system. On the other hand, retrograde ureteral stents are devices used by urologists. They are placed with cystoscopy guidance in an operating room setting with patients under general anesthesia. The goal of these procedures is to re-establish patency of the ureters.
Retrospective studies have shown that the safety and efficacy of retrograde stenting of an infected obstructed kidney is comparable to that of PCN with an overall failure rate of 4 and 2.5% respectively [5]. However, PCN is a more favorable procedure in cases of severe sepsis as it can be done under local sedation omitting the need for an anesthetist or the use of anesthetic agents which may depress the cardiovascular system. The microbiology yield from urine culture following a PCN was found to be superior to retrograde stenting [6]. Moreover, there is also a theoretical higher risk of worsening sepsis due to instrumentation of the collecting system associated with retrograde stenting [7].
An infected obstructed kidney is considered by some centers to be the only absolute indication for emergent decompression regardless of time of day or night. This is because mortality rates associated with septic shock could approach 40% [8]. Furthermore, decompression has been shown to improve mortality by up to 50% [9]. It also reduces renal parenchymal loss secondary to pyonephrosis [10].
On the other hand, decompression in cases of non-infected urinary tract obstruction is generally less urgent. A PCN can be placed during daytime hours for urinary tract obstruction without evidence of infection as the kidney is not acutely threatened [11]. Biochemical abnormalities, e.g., hyperkalemia associated with renal failure can be corrected medically in the first instance [12]. Furthermore, recovery of renal function has been shown to be favorable if relief of obstruction is not delayed beyond 2 weeks [13].
There is currently no single clinical parameter which is able to differentiate between an infected obstructed kidney and a non-infected but obstructed kidney at time of presentation. This is an important issue as it is needed to determine the timing or urgency for decompression. The gold standard for the diagnosis of infection is a positive urine culture directly obtained from the involved kidney [14]. However, these results are not available immediately and will take 24–48 h to return. The micturating urine sample may not reflect the urine conditions from the upper renal tract proximal to the obstruction. The urine sample from the upper renal tract can only be assessed during decompression. Some patients may have been given antibiotics prior to presentation which may alter the urine culture results. The European Society of Urology recommends using a combination of history, physical examination, imaging, and lab findings to guide diagnosis [15].
Systemic inflammatory response syndrome (SIRS) is used to define a clinical response to a non-specific insult on the body. It consists of parameters that include temperature, heart rate, respiratory rate, and white cell count level. We hypothesize that patients requiring urgent decompression can be identified using the systemic inflammatory response syndrome criteria. This is because SIRS is often present in systemic infection [16]. However, SIRS is nonspecific and can also be seen in cases of inflammation, ischemia, or trauma.
The aim of this retrospective study was to investigate if the presence of SIRS in patients with urinary tract obstruction at time of presentation to the emergency department correlates with a subsequent positive urine culture and to determine if it could be used as a tool to predict the urgency of a PCN. The secondary aim of the study was to assess the incidence of in-hour and after-hour emergent PCNs performed in a tertiary center which has both interventional radiological and urological expertise.
Methods
Local institutional low risk ethics approval was obtained (17-000-553Q). A retrospective review of an electronic database of PCN cases performed in the radiology department between Jan 2011 and June 2016 from a single tertiary center was undertaken. All consecutive emergent adult PCN cases referred from the emergency department were included in the study. These included subjects with single kidneys or kidney transplants. Inpatient referrals and subjects under the age of 16 were excluded from the study.
The definition on an in-hour procedure was any PCN case performed between Monday and Friday from 8 am to 6 pm. An after-hour procedure was defined as any PCN case performed between Monday and Friday from 6 pm to 8 am the following day as well as on the weekends.
Patient details, such as age, sex, and timing of procedure, were recorded. Data collected included vital signs on presentation (heart rate, blood pressure, respiratory rate, and temperature), laboratory markers (total white cell count and urine culture results), and radiological findings (cause of obstruction). Only urine culture specimens obtained from the upper renal tract during decompression were included in the study to minimize the incidence of false positive and negative results. The administration of pre-decompression antibiotics was also recorded. This was defined as receiving antibiotics between the time of presentation to the emergency department and prior to a PCN.
The PCN cases were then divided according to the presence or absence of clinical features of systemic inflammatory response syndrome at the time of presentation. This was defined as the presence of two or more of the following variables: temperature > 38 (Celsius) or < 36, total white cell count > 12 (× 109/L) or < 4, respiratory rate > 30 (breaths/min), heart rate > 90 (beats/min).
Test for significance of association between the presence and absence of SIRS at time of presentation and subsequent urine culture results were done via Fisher’s test using GraphPad Scientific Software Calculator. All statistical analysis and graphical figures produced were undertaken using Microsoft Office Excel Version 15.33.
Results
A total of 110 adult patients met the final inclusion criteria for emergent PCN cases referred from the emergency department. There was a total of 60 male and 50 female patients with a mean age of 62 (age range 18–99 years) (Fig. 1 and Table 1).
There were 53 (48%) patients that met the criteria for obstruction with SIRS and 57 (52%) patients with obstruction without SIRS.
In the obstruction with SIRS group, 46 (88%) patients had a PCN performed after-hours with 7 (12%) patients performed in-hours. The main cause of obstruction was due to ureteric calculi (58%) (Table 2). An elevated temperature and heart rate were the most common features of SIRS at 96 and 83% respectively. Eighteen (34%) patients fulfilled two of the criteria for SIRS, 20 (38%) patients fulfilled three criteria, and 15 (28%) patients fulfilled all four criteria for SIRS. Ten (18%) patients met the criteria for severe sepsis with a systolic blood pressure of less than 90 mmHg (Fig. 2). Forty-four (83%) patients received antibiotics prior to decompression.
Urine culture results were obtained from 52 (98%) out of the 53 patients who had obstruction with SIRS. An organism was isolated in 35 (67%) out of the 52 urine culture results with Escherichia coli being the most common organism in 18 (50%) patients (Table 1).
In the obstruction without SIRS group, 46 (79%) patients had a PCN performed after-hours with 11 (21%) patients performed in-hours. The most common cause of obstruction was due to malignancy in 26 (45%) patients. Fifteen (26%) patients received antibiotics prior to decompression. Urine culture results were obtained from 44 (77%) out of the 57 patients who had obstruction without SIRS. No organism was isolated in 42 (95%) out of the 44 urine culture results. Of the two patients (5%) in which an organism was isolated from the urine culture, one patient had received antibiotics prior to hospitalization which may account for the absence of SIRS due to partial treatment of the infection. In the other patient, there was a low clinical suspicion of an infection on the initial presentation as the patient was asymptomatic.
There was one unsuccessful nephrostomy due to difficulty accessing the pelvicalyceal system. The patient underwent successful ureteric stenting under cystoscopic guidance the following day. There were no immediate complications reported from any of the emergent PCNs, such as hemorrhage or loss of kidney.
Statistical analysis using Fisher’s test revealed that the association between the presence of SIRS at time of presentation and a subsequent positive urine culture was significant (sensitivity 94% and specificity 71%; p < 0.001) (Table 3). There was also a significant difference in the rate of antibiotics administered pre-decompression between the SIRS and non-SIRS group (86 vs 26%; p < 0.01).
Discussion
Recent onset urinary tract obstruction with and without infection is an indication for decompression to reduce the complication rate of septicemia and acute kidney impairment.
According to the SEPSIS KILLS program in Australia, up to 23% of presentations to ED with sepsis can be traced to a urinary tract source [17] and that up to 80% of cases of urosepsis are due to obstructive uropathy [18].
Eighty-eight percent of patients who had obstruction with SIRS and 79% of patients who had obstruction without SIRS underwent urgent decompression after-hours in our study. It is always preferable for PCN procedures to be performed during in-hours where there is generally more medical support from a resource and manpower perspective. In a study by Lewis and Patel, an increased incidence of major complications during PCN placement such as hemorrhage and worsening sepsis occurred after-hours (5.7%) versus during in-hours (1.8%) [19]. Various studies have also shown that fatigue associated with extended working hours leads to increased medical errors which can directly impact patient care [20].
Our study showed that the presence of SIRS was highly sensitive (94%, p < 0.001) for a subsequent positive urine culture. The absence of SIRS had a high negative predictive value (95%, p < 0.001) for excluding infection in patients presenting with a urinary tract obstruction. Therefore, SIRS may be useful as a tool to predict infection which may help determine the urgency of a PCN. Despite the significant increase in rate of antibiotics administered pre-decompression in the SIRS group, this does not seem to have impacted the likelihood of a positive urine culture result.
Most (83%) of all the emergent PCNs performed in our study were referred and performed after-hours. A large percentage (50%) of PCNs performed after-hours did not meet the criteria for SIRS on presentation.
In the absence of SIRS in patients with a urinary tract obstruction, it seems reasonable to delay performing a PCN for urinary tract obstruction to daytime hours only as the presence of a urine infection is unlikely. As mentioned earlier, recovery of renal function is generally favorable if the relief of obstruction is not delayed beyond 2 weeks.
By performing more placement in-hours, the operator and support staff are generally more alert and better equipped for the procedures. It also allows for additional staffing and support from the urology and intensive care units should a complication arise. In addition to that, it has a direct impact on radiology trainees who need adequate exposure and experience in PCN placements. This represents a significant loss of training opportunities for the radiology trainees as the after-hour PCN placements are mainly performed by consultant interventional radiologists. In addition, the after-hour procedure becomes costly, as the interventional team which includes the radiologist, radiographer, and generally two angiography suite nurses is being called back at penalty rates.
The limitations of this study were the small number of subjects recruited from a single institution. It would also be helpful to obtain data from the urology department to assess the number of retrograde stentings being performed during in-hours and after-hours for these two groups of patients to allow comparison so that a better model of care can be established.
Conclusion
In conclusion, this study shows that the absence of SIRS in patients presenting with a urinary tract obstruction has a high negative predictive value (95%) which aids in excluding infection. A large percentage of the PCNs performed after-hours in this study did not meet the criteria for SIRS and could have been performed during daytime hours instead. Therefore, SIRS could be used as a tool to help determine the urgency of a PCN which may indeed improve the workflow of a busy tertiary radiology department.
References
Sierakowski R, Finlayson B, Landes RR, Finlayson CD, Sierakowski N (1978) The frequency of urolithiasis in hospital discharge diagnoses in the United States. Investig Urol 15(6):438–441
Lameire N, Van Biesen W, Vanholder R. Acute renal failure. Lancet (London, England) 2005; 365(9457):417–430
Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, Knoll T, Lingeman JE, Nakada SY, Pearle MS, Sarica K, Türk C, Wolf JS Jr, EAU/AUA Nephrolithiasis Guideline Panel (2007) 2007 guideline for the management of ureteral calculi. J Urol 178(6):2418–2434
Goodwin WE, Casey WC, Woolf W (1955) Percutaneous trocar (needle) nephrostomy in hydronephrosis. J Am Med Assoc 157(11):891–894
Ahmad I, Saeed Pansota M, Tariq M, Shahzad Saleem M, Ali Tabassum S, Hussain A (2013) Comparison between double J (DJ) ureteral stenting and percutaneous nephrostomy (PCN) in obstructive Uropathy. Pakistan J Med Sci 29(3):725–729
Pearle MS, Pierce HL, Miller GL, Summa JA, Mutz JM, Petty BA et al (1998) Optimal method of urgent decompression of the collecting system for obstruction and infection due to ureteral calculi. J Urol 160(4):1260–1264
Ramsey S, Robertson A, Ablett MJ, Meddings RN, Hollins GW, Little B (2010) Evidence-based drainage of infected hydronephrosis secondary to ureteric calculi. J Endourol 24(2):185–189
Wagenlehner FM, Lichtenstern C, Rolfes C, Mayer K, Uhle F, Weidner W, Weigand MA (2013) Diagnosis and management for urosepsis. Int J Urology: Off J Japan Urol Assoc 20(10):963–970
Borofsky MS, Walter D, Shah O, Goldfarb DS, Mues AC, Makarov DV (2013) Surgical decompression is associated with decreased mortality in patients with sepsis and ureteral calculi. J Urol 189(3):946–951
Liu J-J, Shortliffe LMD. 50- renal abscess and other complex renal infections A2 Long SS. Principles and practice of pediatric infectious diseases (fourth edition). London: Content Repository Only!; 2012 p 343-5.e1
Dagli M, Ramchandani P (2011) Percutaneous nephrostomy: technical aspects and indications. Semin Interv Radiol 28(4):424–437
Regalado SP (2006) Emergency percutaneous nephrostomy. Semin Interv Radiol 23(3):287–294
Lucarelli G, Ditonno P, Bettocchi C, Grandaliano G, Gesualdo L, Selvaggi FP, Battaglia M (2013) Delayed relief of ureteral obstruction is implicated in the long-term development of renal damage and arterial hypertension in patients with unilateral ureteral injury. J Urol 189(3):960–965
Papagiannopoulos D, Whelan P, Ahmad W, Rybak J, Hota B, Deane L, Nehra A (2016) Procalcitonin is a strong predictor of urine culture results in patients with obstructing ureteral stones: a prospective, pilot study. Urol Annals 8(3):277–280
Grabe MB-JT, Botto H et al (2015) Guidelines on urological infections 2015. European Association of Urology
(1992) American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Critical care medicine 20(6):864–874
Burrell AR, McLaws ML, Fullick M, Sullivan RB, Sindhusake D (2016) SEPSIS KILLS: early intervention saves lives. Med J Aust 204(2):73.e1–73.e7
Dreger NM, Degener S, Ahmad-Nejad P, Wobker G, Roth S. Urosepsis—etiology, diagnosis, and treatment. Deutsches Arzteblatt international 2015; 112(49):837–847; quiz 48
Lewis S, Patel U (2004) Major complications after percutaneous nephrostomy—lessons from a department audit. Clin Radiol 59(2):171–179
Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, Lilly CM, Stone PH, Lockley SW, Bates DW, Czeisler CA (2004) Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med 351(18):1838–1848
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Local institutional low risk ethics approval was obtained (17-000-553Q).
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Koh, D., Lau, K.K. & Teoh, E. Are all urgent nephrostomies that urgent?. Emerg Radiol 25, 381–386 (2018). https://doi.org/10.1007/s10140-018-1598-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-018-1598-7