Abstract
Fabrics act as fomites for microorganisms, thereby playing a significant role in infection transmission, especially in the healthcare and hospitality sectors. This study aimed to examine the biofilm formation ability of four nosocomial infection–causing bacteria (Acinetobacter calcoaceticus, Escherichia coli, Pseudomonas aeruginosa, and Staphylococcus aureus) on cotton, polyester, polyester-cotton blend, silk, wool, viscose, and nylon, used frequently in the healthcare sector, by qualitative and quantitative methods. The impact of temperature, pH, and relative humidity (RH) on biofilm formation was also assessed. P. aeruginosa and S. aureus were strong biofilm producers, while E. coli produced weak biofilm. Wool (maximum roughness) showed the highest bacterial load, while silk (lowest roughness) showed the least. P. aeruginosa exhibited a higher load on all fabrics, than other test bacteria. Extracellular polymeric substances were characterized by infrared spectroscopy. Roughness of biofilms was assessed by atomic force microscopy. For biofilm formation, optimum temperature, pH, and RH were 30 °C, 7.0, and 62%, respectively. MgCl2 and CaCl2 were the most effective in removing bacterial biofilm. In conclusion, biofilm formation was observed to be influenced by the type of fabric, bacteria, and environmental conditions. Implementing recommended guidelines for the effective disinfection of fabrics is crucial to curb the risk of nosocomial infections. In addition, designing modified healthcare fabrics that inhibit pathogen load could be an effective method to mitigate the transmission of infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Textiles act as potential reservoirs for various pathogens, increasing the risk of nosocomial infections in the hospital environment. Healthcare apparel such as doctor’s coats, surgical gowns, scrubs, bed sheets, pillow covers, curtains, and towels play an inevitable role in the transmission of infection (Goyal et al. 2019). The bacteria adhering to fabrics produce biofilms that are challenging to remove using standard laundry techniques. Biofilm accumulates upon the repeated use of these fabrics, eventually leading to the transmission of infections (Gupta et al. 2019). The National Institute of Health (NIH) delineates that biofilm formation is the cause of 80% of total microbial infections; 60–70% are nosocomial infections caused by biofilms on surfaces (Jamal et al. 2018).
Biofilm, a community of microorganisms, exhibits a higher resistance than their planktonic forms due to its matrix formed of extracellular polymeric substances (EPS) (Sharma et al. 2019). Bacterial adherence can be explained by Derjaguin, Verwey, Landau, and Overbeek (DVLO) forces, which include electrostatic interaction, van der Waal forces, and steric interaction (Garrett et al. 2008). During the growth phase, the adhered cells produce EPS, consisting mainly of polysaccharides, DNA, proteins, and lipids (Chen et al. 2013).
Previous studies have reported a significant number of nosocomial infections in hospitals due to biofilm formation on medical devices (Assefa and Amare 2022; Cangui-Panchi et al. 2022). There are several studies on surface adherence properties and biofilm formation on hard surfaces (Bae et al. 2012; Bhagwat et al. 2021). However, there is a lack of in-depth understanding of how soft surfaces like fabrics influence the process of biofilm formation. This makes it challenging to control infections transmitted through fabric.
Bacterial attachment and biofilm development on textile is influenced by several factors like properties of textile, bacteria, and environmental conditions (Song et al. 2015; Moraes et al. 2018). Higher bacterial adhesion and biofilm formation was reported on hydrophobic and rough surfaces (Zheng et al. 2021). The hydrophobic bacterial surface also promotes strong adhesion to hydrophobic surfaces, whereas hydrophilic bacterial cells prefer hydrophilic surfaces (Kochkodan et al. 2008). Environmental parameters, including temperature, pH, and relative humidity (RH), play a substantial role in fabric-microbe interaction (Dixit et al. 2023). Temperatures beyond the optimal range have an adverse effect on bacterial adherence (Garrett et al. 2008). A change in pH value influences the hydrophobicity of the cell surface (Bunt et al. 1993). Bacterial adhesion and RH are directly correlated, as higher bacterial adhesion was reported in humid environments (Horve et al. 2020). The research on biofilm mitigation majorly focuses on methods to eradicate biofilms on hard surfaces (Feng et al. 2013; del Agustín et al. 2023). These techniques, however, are only partially effective because of the bacterial resistance in biofilms. Thus, to mitigate the infection transmission risk associated with the production of biofilm, understanding the ability of biofilm formation on different fabrics by nosocomial pathogens, and environmental factors that regulate its formation, is essential. There is a research gap in our understanding that fabrics act as a suitable surface for bacterial growth and biofilm formation, and how the bacterial load varies for different fabric types.
The present study aimed to draw a correlation between the type of fabric and environmental conditions on biofilm formation by four bacteria. Fabrics were chosen based on their application in hospitals. Silk was chosen because of earlier reports of its ability to discourage microbial adhesion (Holland et al. 2019). Four bacterial species, viz. Acinetobacter calcoaceticus, Escherichia coli, Pseudomonas aeruginosa, and Staphylococcus aureus, were selected because of their ability to survive on fabrics and their role as potential nosocomial pathogens (Koca et al. 2012; Varshney et al. 2021). This study was undertaken for assessing the capability of selected bacteria to form biofilm on fabrics, by qualitative as well as quantitative methods, and to understand the effect of environmental factors on biofilm development.
Material and methods
Test fabrics and bacteria
Seven fabrics, polyester, cotton, polyester-cotton (70:30) blend, nylon, silk, viscose, and wool, were recorded to be the material of preference for textiles used in hospitals and, thus, selected for the present study. These fabrics were procured from the local market.
Selected bacterial cultures were procured from the culture bank of IIT Delhi, India. Stock cultures were inoculated into Luria-Bertani (LB) broth and incubated overnight at 37 °C under shaking. Experiments were conducted using bacteria in the exponential growth phase. All the experiments were conducted in triplicates.
Scouring of fabrics
Scouring of fabrics was done to remove impurities. The test fabrics were boiled in soda ash (1–2%) and liquid soap solution (5 gpl) for 45 min to scrub the fabrics (Varshney et al. 2020). Following a thorough rinsing with water, samples were dried and ironed. Scoured fabrics were then wrapped in aluminum foil and stored in a sealed plastic bag. Before the experiment, each fabric was autoclaved at 121 °C for 20 min to ensure sterility.
Biofilm formation on fabrics
Confirmatory test for biofilm formation
To confirm biofilm formation on fabrics, approximately 1 × 104 CFU ml−1 of bacterial culture was inoculated in 0.5 l sterile flasks containing Tryptic Soy Broth (TSB) (50 ml) and incubated for 14–16 h under shaking (160 rpm) at 37 °C. Congo Red (CR) dye (0.08%) was then mixed with the bacterial cultures (Arciola et al. 2001). Two hundred microlitres of S. aureus (1.5 × 106 CFU ml−1), P. aeruginosa (1.6 × 106 CFU ml−1), A. calcoaceticus (1.7 × 106 CFU ml−1), and E. coli (2.1 × 106 CFU ml−1) with CR dye was added in each well in a microtiter plate. A brown color of the medium indicated the formation of biofilm on fabrics.
Biofilm quantitation based on Crystal Violet staining
In 96-well flat-bottom microtiter plates, a test for the formation of biofilm was conducted as described by Stepanović et al. (2007). Acetone (10 µl) was added to the wells to fix fabric pieces (0.6 cm diameter) (Fig. S1). Fabric-fixed microtiter plate was sterilized under UV radiation for 30 min. Two hundred microlitre of isolate (S. aureus, P. aeruginosa, A. calcoaceticus, and E. coli) (~ 1.5 × 106 CFU ml−1) was added into the wells followed by incubation of the plate at 37 °C for 48 h. The negative control consisted of sterile TSB. Following incubation, wells were emptied by flicking and washed using PBS (300 µl). After washing, heat fixing of the remaining attached bacteria was done by incubation in a hot air oven for 1 h. Then, 150 µl methanol was added to each well, kept for 20 min, emptied, and kept in an inverted position for overnight drying. Adhered biofilm was stained using 1% Crystal Violet (CV) (150 µl). The stain in the well was removed by washing the plate with sterile water and rinsing till the wells appeared without stain, followed by drying of the plate at room temperature. Then, dye-bound cells were resuspended in 150 µl of ethanol (95%), and plates were covered to minimize evaporation for 30 min. The optical density (OD) of each well was recorded at 570 nm wavelength using a microtiter plate reader (Thermo Scientific, USA). The average OD values were determined for all the negative and tested strains. ODc was calculated (Eq. 1) and the final OD of bacterial strains was determined (Eq. 2).
where ODC is the cutoff value, NC is the negative control, and SD is the standard deviation.
If the reading showed a negative value, it was considered as no biofilm formation (OD ≤ ODc), whereas the positive value represented biofilm formation, weak biofilm producer (ODc < OD ≤ 2 × ODc), moderate biofilm producer (2 × ODc < OD ≤ 4 × ODc), and strong biofilm producer (4 × ODc < OD) (Stepanović et al. 2007).
Quantitative estimation of biofilm by plate count
After biofilm formation, dislodging was done in 500 µl NaCl (0.9%) at 4000 rpm for 2 min (Stepanović et al. 2007; Melo et al. 2017). Diluted cell suspensions were plated on Luria agar (LA) plates, and incubated for 16–18 h at 37 °C. The colonies obtained on the plates were counted to determine the bacterial load on different fabrics.
Production of extracellular polymeric substances (EPS) and their characterization
EPS production by bacteria
A hundred microlitre of each bacterial culture was added to 1 l of fresh LB medium, and incubated at 37 ℃ for 7 days. Thereafter, the culture was centrifuged at 8000 rpm in 50 ml falcon for 20 min. The supernatant was removed, and the falcons containing pellets were filled with double the volume of chilled ethanol (100%). Falcons were kept at 4 ℃ overnight. The supernatant was transferred to a fresh falcon tube followed by centrifugation at 2500 rpm for 20 min. Pellets were dried at 50 ℃ and weighed (Tewari and Sharma 2020).
Infrared spectroscopy of EPS
Fourier-transform infrared spectroscopy (FTIR) (FTIR Nicolet 6700, AZ, USA) was used to identify functional groups in EPS. For sample preparation, EPS (1 mg) was blended with potassium bromide (100 mg), followed by hard-pressing of the sample into a 15 − 16 mm diameter mold. The spectra were documented for a specific range of wave numbers (4000 to 400 cm−1) (Al-Nabulsi et al. 2022). The graphs were obtained in terms of percentage transmittance examined using standards.
Test of stability of biofilm formed on fabrics
After biofilm formation on fabrics in a microtiter plate, liquid culture was discarded from each well followed by washing with 0.9% saline and then treatment with 200 µl of 0.3 M NaCl, 0.21 M CaCl2, 0.21 M MgCl2, 2 M urea, and 0.01 M EDTA (Chen and Stewart 2000). Treatment was followed by incubation at 37 ℃ for 2 h. The wells of the microtiter plate were washed using 0.9% saline and then stained with 1% CV (200 µl). CV was discarded after 5 min and 200 µl of alcohol-acetone (80:20) solution was added in the wells. Alcohol:acetone solution was collected into a fresh microtiter plate and analyzed on a plate reader at 595 nm (Melo et al. 2017).
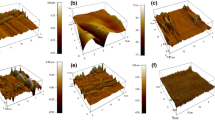
Roughness of fabrics after biofilm formation
Atomic force microscopy (AFM; Asylum Research MFP3D-BIO, UK) was performed for 3D profiling of biofilm formed (nanoscale level) by measuring forces between the surface and a probe at a distance of 0.2–10 nm. The probe tip touches the fabric surface and measures the force between the fabric surface and the probe. Nanoroughness of the control fabric and biofilm formed on fabrics was determined (Mohebi et al. 2017).
Impact of temperature, pH, and RH on biofilm formation
The effect of different environmental factors (temperature, pH, and RH) on the formation of biofilm on fabrics (polyester, cotton, and blend) was studied. Microtiter plates containing fabrics with bacterial cultures were incubated for 48 h at 15 °C, 30 °C, and 45 °C (constant pH 7.0), pH 5.0, 7.0, and 8.0 (constant temperature 30 °C), and RH 22%, 43%, and 62% (30 °C, pH 7.0). RH was maintained in an insulated desiccator using saturated solutions of potassium acetate (approx. 22%), potassium carbonate (approx. 43%), and cobalt chloride (approx. 62%) (Greenspan 1977). The bacterial colonies were counted on LB agar plates to assess the bacterial load on different fabrics.
Statistical analysis
The experimental observations were represented as a mean value with standard deviation. Data analysis was performed by one-way ANOVA using the IBM SPSS software (version 23.0). The statistical significance of the data was calculated by Duncan’s multiple-range test (P < 0.05).
Results
Biofilm formation on fabrics
Detection of biofilm formation on fabrics
The development of dark brown color on the fabrics in the presence of CR dye confirmed biofilm formation by the four bacterial species (Fig. S2). The assessment of biofilm formation showed that P. aeruginosa and S. aureus produced strong biofilm, while A. calcoaceticus and E. coli produced only moderate and weak biofilm, respectively (Table 1).
Quantitative assessment of biofilm formation on fabrics
Among all the fabrics tested, wool showed the highest bacterial biofilm, followed by viscose, blend, cotton, polyester, nylon, and silk (Fig. 1). Among the bacterial species, P. aeruginosa showed the highest count on most fabrics, followed by S. aureus and A. calcoaceticus, while E. coli showed the least count.
Biofilm formation on various fabrics and their bacterial load (CFU cm−2); error bars represent the standard deviations (n = 9). Significant differences within the fabric between different bacterial strains are represented by small letters, and difference between fabrics is denoted by capital letters. PA P. aeruginosa, SA S. aureus, AC A. calcoaceticus, and EC E. coli
EPS production and its characterization
The four bacterial strains produced EPS. Using FTIR, several functional groups were detected in EPS. EPS of the 7-day grown culture of P. aeruginosa was highest and the least for E. coli (Table 2). The CFU count of each bacterial strain was determined in the culture before EPS extraction.
Rheological properties of bacterial EPS revealed that the EPS produced by E. coli, A. calcoaceticus, and S. aureus were non-viscous (< 10 Pa−s) (Fig. 2), while the EPS produced by P. aeruginosa was slightly viscous in nature (> 100 Pa.s). The FTIR spectrum of EPS isolated from the four bacteria showed that it contained a variety of functional groups (Table 3), with carboxylic acid, alkane, sulfonyl chloride, amine salt, primary alcohol, secondary alcohol, aromatic ester, alkene, etc. present in EPS specific to bacteria (Fig. S3). Specific functional groups like C-H bending, -CH3 group, C-O group, aromatic ester, primary alcohol, and C=O stretching delta lactone were present in the EPS of S. aureus. Some functional groups like C-H and O–H stretching were present in EPS of all four bacterial strains.
Biofilm stability on fabrics
Fabrics with biofilm were treated with salts, viz. 0.3 M NaCl, 0.21 M CaCl2, 0.21 M MgCl2, 2 M Urea, and 0.01 M EDTA. The stability of biofilm on fabrics was assessed based on the difference in OD595 between fabrics treated with different salts and control fabrics without treatment (Fig. 3). Biofilm formed by E. coli and A. calcoaceticus on fabrics was found to be least stable when treated with CaCl2 and MgCl2. The stability of S. aureus and P. aeruginosa biofilm on fabrics was least when treated with NaCl and MgCl2.
Roughness of fabrics after biofilm formation
The roughness of sterile fabric and biofilm-formed fabrics was assessed by AFM (Table 4). AFM analysis was done for biofilm formed by S. aureus and E. coli on fabrics. The roughness of wool, viscose, blend, and cotton decreased when the biofilm formation occurred, whereas the roughness of polyester, nylon, and silk increased due to S. aureus and E. coli biofilms.
Optimum temperature, pH, and RH for biofilm formation
P. aeruginosa and S. aureus showed maximum biofilm formation at a temperature of 30 °C, pH 7.0, and RH 62% (Fig. 4). Biofilm formation by bacterial strains was significantly higher on blend fabric, followed by cotton and polyester at 30 °C. P. aeruginosa showed a higher load on all the fabrics, in comparison to S. aureus, irrespective of the environmental conditions.
Bacterial load (CFU cm−2) on different fabrics at variable temperatures (a, b, c 15 °C, 30 °C, and 45 °C, respectively), pH (d, e pH 5 and 8, respectively), and RH (f, g, h 22%, 43%, and 62%, respectively). Error bars denote standard deviations (n = 9). Significant differences between the fabrics (same treatment) are denoted by small letters. PA P. aeruginosa, SA S. aureus
Discussion
Fabrics play a crucial role in the spread of infections as they serve as a reservoir for various microorganisms and pathogens. The heavily contaminated (with infectious agents) hospital fabrics may harbor a microbial load of 106–108 CFU/100 cm2 (Koca et al. 2012). The survival of these bacteria is enhanced due to their persistence within a matrix of EPS; the assemblage thus formed is known as a biofilm.
There are several characteristics of textiles that affect biofilm formation. The type of weave and composition of fabrics are some important parameters (Bajpai et al. 2011; Varshney et al. 2020). The structural characteristics (weave, linear density, properties of warp, and weft thread) of woven fabrics control the permeability of moisture and air, thus influencing microbial load (Rogina-Car et al. 2020). In the present work, plain (cotton, polyester, blend, silk, and nylon) and twill (wool and viscose) woven fabrics were used for assessing the formation of biofilms. Maximum bacterial load was observed on wool (twill type) and minimum on silk (plain) by the four bacteria under similar experimental conditions (Varshney et al. 2020). Twill fabric with higher roughness allows more bacteria to adhere (Premkumar and Thangamani 2017).
The bacterial load on fabric is also associated with surface roughness. It has been reported that a highly rough surface (nanoscale) promotes more bacterial adhesion (Varshney et al. 2021). AFM analysis was done to study the roughness of fabric with and without biofilm. The trend of biofilm formation by the four bacterial species correlated with the roughness of the fabrics. Bacterial strains have different abilities for initial adhesion to various textile types. Previous studies have shown that Staphylococcus spp. adhere strongly to cotton, polyester, and blends in comparison to E. coli (Hsieh et al. 1987). A study of biofilm formation on cotton revealed that P. aeruginosa produced more biofilm than S. aureus (Montagut et al. 2019). A higher bacterial load of P. aeruginosa was observed on all the tested fabrics, compared to other bacteria. In our study, polyester and cotton fabrics promoted weak to strong biofilm formation depending on the bacterial strain. The formation of biofilm on fabrics was assessed by counting the CFU load, which was the highest for P. aeruginosa on fabrics, and the least for E. coli.
Bacterial EPS plays a crucial role in surface adherence, water retention, biofilm formation, cell protection, genetic exchanges, etc. (Costa et al. 2018). The characteristics and production of EPS may vary depending on factors like media composition, temperature, RH, and time. (Mika et al. 2016; Mıdık et al. 2020). In the present study, EPS extraction was done to understand the correlation between biofilm formation and the amount of EPS produced. EPS produced by S. aureus, E. coli, and A. calcoaceticus was non-viscous, while that secreted by P. aeruginosa was slightly viscous and showed viscoelasticity (Di Martino 2018). A higher production of EPS was observed by P. aeruginosa, while E. coli produced the least amount.
Although many studies are reported on bacterial adhesion on surfaces, investigation of the role of EPS in bacterial adhesion on fabrics is not yet clear. In the current study, FTIR analysis of the EPS produced by the four bacterial species revealed several functional groups. Detection of the hydroxyl group (3400 cm−1) and carboxyl group (a peak in the range 1416 to 1631.48 cm−1) showed the presence of polysaccharides in EPS of all bacteria (Kumar et al. 2011). Asymmetrical C‒H stretching (2800–3000 cm−1) showed lipid and sugar content in EPS, which is also present in all bacteria (Kavita et al. 2011). Functional groups such as C‒O‒C and C‒O indicated the presence of alkyl aryl ether and carbohydrates, respectively in P. aeruginosa (Mishra and Jha 2009). Uronic acid was found in E. coli, which was validated by an ester linkage (Bramhachari and Dubey 2006). Stretching of the C=O functional group is the characteristic of proteins (Wang et al. 2014). N–H, C=C, and C-F stretching represent amines, cyclic alkane, and fluoro compounds, respectively, in the EPS (Mishra and Jha 2009; Kavita et al. 2011). The stretching vibrations observed below 1000 cm−1 may represent the presence of phosphate groups of nucleic acids in EPS (Chen et al. 2013). The FTIR data confirmed the presence of polysaccharides, amines, proteins, uronic acid, nucleic acids, etc. in the bacterial EPS. FTIR showed major peaks for polysaccharides in all bacteria, but the composition of polysaccharides may change depending on the type of bacterial strain (Salama et al. 2016). Protein polymer curli and carbohydrate polymer cellulose were the two major constituents in EPS of E. coli, but it can also include DNA, β-1,6-N-acetylglucosamine, and colanic acid (Hufnagel et al. 2015). It contained glucose, galactose, glucuronic acid, arabinose, fucose, etc. as monosaccharides. Carbohydrates are the major components, whereas protein and uronic acids are minor components of EPS. EPS of P. aeruginosa consisted of a neutral branched polysaccharide, which forms a fiber-like network during bacterial colonization and acts as a promoter of bacteria-surface interactions (Di Martino 2018). It also contained cationic polysaccharides consisting of N-acetylglucosamine and N-acetylgalactosamine, which provide structural support to cells and are involved in the initiation of bacterial interactions in biofilms (Vasseur et al. 2005). Biofilm-associated protein (Bap) and phenol soluble modulins (PSMs) are the key components of EPS of S. aureus (Taglialegna et al. 2016). Bap is mainly responsible for bacterial adhesion and production of biofilm (Di Martino 2018). PSMs interact with extracellular DNA to form amyloid fibers, which help move cells during early biofilm formation. EPS of A. calcoaceticus mainly consisted of heptasaccharides (Gudiña et al. 2015).
Bacteria typically have a negative charge because of the existence of carboxylic and phosphate groups on their surface and are reported to adhere mostly on positively charged surfaces (Zheng et al. 2021). Although surface charge density is an important property that determines bacterial adhesion on surfaces, other factors such as EPS components, pili, flagella, and surface properties like roughness, topography, and hydrophobicity also play a role in bacterial adhesion (Kreve and Reis 2021). Several studies reported that bacteria can overcome electrostatic repulsion with negative charge and bind even strongly to negatively charged surfaces due to pili (Zheng et al. 2021). Adherence and growth of bacteria on fabric (negatively charged) despite its negative charge have been reported in several studies (Varshney et al. 2021; Dixit et al. 2023). EPS of bacteria promotes their adhesion on fabrics due to its stabilizing and cross-linking properties. It is reported that small amounts of EPS inhibit bacterial adhesion on surfaces by electrostatic interaction, whereas large amounts enhance cell adhesion due to polymeric interaction (Tsuneda et al. 2003).
A biofilm stability experiment was carried out to confirm the efficiency of various salts in biofilm elimination from fabric. Biofilm removal on fabrics was highest when treated with MgCl2 and CaCl2 for all bacterial strains. Chen and Stewart (Chen and Stewart 2000) also reported NaCl and CaCl2 to be effective in biofilm removal on hard surfaces. The effect of EDTA and urea was the least in biofilm removal from fabrics. Previous studies have also shown moderate to high efficiency of chemicals like EDTA, urea, and MgCl2 for biofilm destabilization on textile surfaces (de Almeida et al. 2016).
The environmental conditions may have a major effect on biofilm formation (Nostro et al. 2012). Variation in the growth temperature of bacteria can affect their ability of biofilm formation. The optimal temperature for the growth of bacteria is linked with an increase in nutrient uptake (Price and Sowers 2004). In addition, temperature can also change the physical properties of bacteria and the binding surface, like low-temperature changes polymer composition on the bacterial surface, which decreases bacterial adhesion (Garrett et al. 2008). In the present study, the ability to form biofilm by S. aureus and P. aeruginosa at various temperatures, pH, and RH was assessed. S. aureus and P. aeruginosa were selected as they were strong biofilm producers. In Delhi, the average temperature varies from 14 to 45 °C (January to June), and an average RH varies from 25 to 68% (April to August) (https://en.wikipedia.org/wiki/climate_of_Delhi; accessed on 22nd July 23). Bacterial load is expected to vary with these variables. The pH range was selected as the pH of the fabric ranges between 4.5 and 7.5 (https://blog.hannainst.com/measuring-surface-ph-of-denim; accessed on 22nd July 23) and most bacteria can grow in this range. Biofilm formation was higher at 30 °C irrespective of bacteria and fabric type. In this study, S. aureus and P. aeruginosa did not form biofilm at lower temperatures (15 °C), and biofilm formation was lower at higher temperatures 45 °C. This may be attributed to the changes in the hydrophobicity of bacteria with temperatures lower or higher than optimum (Hori et al. 2009). This is in agreement with a previous study where a rise in temperature above optimum resulted in reduced (46.4–98.4%) biofilm formation (Hostacká et al. 2010). It is known that optimum temperature increases the rate of enzymatic reactions, which regulate biochemical processes in bacteria, thus enhancing nutrient metabolism, and increasing bacterial growth and biofilm formation (Achinas et al. 2019). An earlier study reported that the hydrophobicity of S. aureus increased with a rise in temperature from 20 to 37 °C, which subsequently led to enhanced adhesion (Khelissa et al. 2017). In the current study, biofilm formation by bacteria differed depending on the surface characteristics, with the maximum on the blend, followed by cotton and polyester, regardless of environmental conditions and type of bacteria. This can be correlated with the surface roughness, which is maximum for blend and least for polyester. In addition, the hydrophilic nature of the fabric surface also promotes bacterial adhesion, thus, cotton, being more hydrophilic, had a higher bacterial load than polyester. In a previous study, S. aureus produced more biofilm on hydrophilic surfaces than on hydrophobic surfaces (Lee et al. 2015). It was observed that changes in pH value impact microbial adherence, the initial stage in biofilm development (McWhirter et al. 2002). Maximum biofilm formation was observed at a neutral pH of 7.0. As reported earlier, biofilm formation by S. aureus was slower at pH values (pH 3 and pH 12), different from the optimum (pH 7), which is consistent with the present study (Zmantar et al. 2010). The alteration in pH value changes the hydrophobicity of the cell surface (Chmielewski and Frank 2003). In addition, a change in pH also causes variations in the zeta potential of bacteria; thus, it affects bacterial adhesion by modifying surface features of the bacterial cells, as also reported for adherence of Staphylococcus epidermidis to surfaces (Nostro et al. 2012).
Another environmental factor that influences bacterial adherence and the development of biofilms is RH. In the present study, biofilm development by S. aureus and P. aeruginosa was maximum at a higher RH value, i.e., 62% followed by 43% and 22% irrespective of the bacterial species. At lower RH, insufficient moisture on surfaces may inhibit bacterial adhesion, growth, and other metabolic activities (Qiu et al. 2022).
Studies focusing on biofilm formation on soft surfaces like fabrics will be beneficial to mitigate the transmission of infections in hospitals, as fabric forms the immediate environment for patients and healthcare staff. The present study used an in vitro microtitre plate assay to understand biofilm formation on fabrics. Although this technique has significantly improved our understanding of the biofilm, it is becoming more apparent that most in vitro techniques insufficiently reflect in vivo conditions.
In the future, the growth of a mixed bacterial community on various fabrics in the presence of body fluids such as sweat and blood would be more realistic, and help us understand how fabrics facilitate the proliferation of bacteria in their presence. Biofilm study under in vivo conditions will provide a more logical understanding of the biofilm formation process. Designing surface-modified fabrics will be advantageous to limit bacterial adhesion on fabrics.
In conclusion, textile surfaces provide a suitable environment for biofilm formation. Several factors influence microbe-textile interaction, including the type of bacteria and textile, and their surface properties. A correlation could be established between the roughness and hydrophobicity of fabrics with microbial load and biofilm formation. Biofilm assay revealed that P. aeruginosa and S. aureus produced strong biofilms, whereas A. calcoaceticus and E. coli produced moderate and weak biofilms, respectively. Optimum values of temperature, pH, and RH promote the formation of biofilm, thus providing a significant contribution in shaping the biofilm. Current findings may help mitigate nosocomial infections in hospitals by using fabrics that inhibit bacterial adhesion and subsequently biofilm formation.
Data availability
All data generated or analyzed during this study are included in this article [and its supplementary information files].
References
Achinas S, Charalampogiannis N, Euverink GJW (2019) A brief recap of microbial adhesion and biofilms. Appl Sci 9:2801–2815
Al-Nabulsi AA, Jaradat ZW, Al Qudsi FR, Elsalem L, Osaili TM, Olaimat AN, Esposito G, Liu SQ, Ayyash MM (2022) Characterization and bioactive properties of exopolysaccharides produced by Streptococcus thermophilus and Lactobacillus bulgaricus isolated from labaneh. LWT 167:113817–113827
Arciola CR, Baldassarri L, Montanaro L (2001) Presence of icaA and icaD genes and slime production in a collection of staphylococcal strains from catheter-associated infections. J Clin Microbiol 39:2151–2156
Assefa M, Amare A (2022) Biofilm-associated multi-drug resistance in hospital-acquired infections: a review. Infect Drug Resist 15:5061–5068
Bae YM, Baek SY, Lee SY (2012) Resistance of pathogenic bacteria on the surface of stainless steel depending on attachment form and efficacy of chemical sanitizers. Int J Food Microbiol 153:465–473
Bajpai V, Bajpai S, Jha MK, Dey A, Ghosh S (2011) Microbial adherence on textile materials: a review. J Environ Res Dev 5:666–672
Bhagwat G, O’Connor W, Grainge I, Palanisami T (2021) Understanding the fundamental basis for biofilm formation on plastic surfaces: role of conditioning films. Front Microbiol 12:1–10
Bramhachari PV, Dubey SK (2006) Isolation and characterization of exopolysaccharide produced by Vibrio harveyi strain VB23. Lett Appl Microbiol 43:571–577
Bunt CR, Jones DS, Tucker IG (1993) The effects of pH, ionic strength and organic phase on the bacterial adhesion to hydrocarbons (BATH) test. Int J Pharm 99:93–98
Cangui-Panchi SP, Nacato-Toapanta AL, Enríquez-Martínez LJ, Reyes J, Garzon-Chavez D, Machado A (2022) Biofilm-forming microorganisms causing hospital-acquired infections from intravenous catheter: a systematic review. Curr Res Microb Sci 3:100175–100186
Chen X, Stewart PS (2000) Biofilm removal caused by chemical treatments. Water Res 34:4229–4233
Chen YP, Zhang P, Guo JS, Fang F, Gao X, Li C (2013) Functional groups characteristics of EPS in biofilm growing on different carriers. Chemosphere 92:633–638
Chmielewski RAN, Frank JF (2003) Biofilm formation and control in food processing facilities. Compr Rev Food Sci Food Saf 2:22–32
Costa OYA, Raaijmakers JM, Kuramae EE (2018) Microbial extracellular polymeric substances: ecological function and impact on soil aggregation. Front Microbiol 9:1636–1650
de Almeida J, Hoogenkamp M, Felippe WT, Crielaard W, van der Waal SV (2016) Effectiveness of EDTA and modified salt solution to detach and kill cells from Enterococcus faecalis biofilm. J Endod 42:320–323
del Agustín MR, Stengel P, Kellermeier M, Tücking KS, Müller M (2023) Monitoring growth and removal of Pseudomonas biofilms on cellulose-based fabrics. Microorganisms 11:892–909
Di Martino P (2018) Extracellular polymeric substances, a key element in understanding biofilm phenotype. AIMS Microbiol 4:274–288
Dixit S, Varshney S, Gupta D, Sharma S (2023) Textiles as fomites in the healthcare system. Appl Microbiol Biotechnol 107:3887–3897
Feng G, Klein MI, Gregoire S, Singh AP, Vorsa N, Koo H (2013) The specific degree-of-polymerization of A-type proanthocyanidin oligomers impacts Streptococcus mutans glucan-mediated adhesion and transcriptome responses within biofilms. Biofouling 29:629–640
Garrett TR, Bhakoo M, Zhang Z (2008) Bacterial adhesion and biofilms on surfaces. Prog Nat Sci 18:1049–1056
Goyal S, Khot SC, Ramachandran V, Shah KP, Musher DM (2019) Bacterial contamination of medical providers’ white coats and surgical scrubs: a systematic review. Am J Infect Control 47:994–1001
Greenspan L (1977) Humidity fixed points of binary saturated aqueous solutions. J Res Natl Bur Stand Sect Phys Chem 81:89–96
Gudiña EJ, Pereira JFB, Costa R, Evtuguin DV, Coutinho JAP, Teixeira JA, Rodrigues LR (2015) Novel bioemulsifier produced by a Paenibacillus strain isolated from crude oil. Microb Cell Fact 14:1–11. https://doi.org/10.1186/s12934-015-0197-5
Gupta P, Bairagi N, Gupta D (2019) Effect of domestic laundering on removal of bacterial contamination from nurses’ white coats. In: Majumdar A, Gupta D, Gupta S (eds) Functional textiles and clothing. Springer Singapore, pp 67–73. https://doi.org/10.1007/978-981-13-7721-1
Holland C, Numata K, Rnjak-Kovacina J, Seib FP (2019) The biomedical use of silk: past, present, future. Adv Healthc Mater 8:1800465–1800490
Hori K, Hiramatsu N, Nannbu M, Kanie K, Okochi M, Honda H, Watanabe H (2009) Drastic change in cell surface hydrophobicity of a new bacterial strain, Pseudomonas sp. TIS1-127, induced by growth temperature and its effects on the toluene-conversion rate. J Biosci Bioeng 107:250–255
Horve PF, Lloyd S, Mhuireach GA, Dietz L, Fretz M, MacCrone G, Van Den Wymelenberg K, Ishaq SL (2020) Building upon current knowledge and techniques of indoor microbiology to construct the next era of theory into microorganisms, health, and the built environment. J Expo Sci Environ Epidemiol 30:219–235
Hostacká A, Ciznar I, Stefkovicova M (2010) Temperature and pH affect the production of bacterial biofilm. Folia Microbiol (praha) 55:75–78
Hufnagel DA, Depas WH, Chapman MR (2015) The biology of the Escherichia coli extracellular matrix. Microbiol Spectr 3:10–1128
Jamal M, Ahmad W, Andleeb S, Jalil F, Imran M, Nawaz MA, Hussain T, Ali M, Rafiq M, Kamil MA (2018) Bacterial biofilm and associated infections. J Chinese Med Assoc 81:7–11
Kavita K, Mishra A, Jha B (2011) Isolation and physico-chemical characterisation of extracellular polymeric substances produced by the marine bacterium Vibrio parahaemolyticus. Biofouling 27:309–317
Khelissa SO, Jama C, Abdallah M, Boukherroub R, Faille C, Chihib N-E (2017) Effect of incubation duration, growth temperature, and abiotic surface type on cell surface properties, adhesion and pathogenicity of biofilm-detached Staphylococcus aureus cells. AMB Express 7:1–13
Koca O, Altoparlak U, Ayyildiz A, Kaynar H (2012) Persistence of nosocomial pathogens on various fabrics. Eurasian J Med 44:28–31
Kochkodan V, Tsarenko S, Potapchenko N, Kosinova V, Goncharuk V (2008) Adhesion of microorganisms to polymer membranes: a photobactericidal effect of surface treatment with TiO2. Desalination 220:380–385
Kreve S, Reis ACD (2021) Bacterial adhesion to biomaterials: What regulates this attachment? A review. Jpn Dent Sci Rev 57:85–96. https://doi.org/10.1016/j.jdsr.2021.05.003
Kumar MA, Anandapandian KTK, Parthiban K (2011) Production and characterization of exopolysaccharides (EPS) from biofilm forming marine bacterium. Brazilian Arch Biol Technol 54:259–265
Lee J, Bae Y, Lee S, Lee S (2015) Biofilm formation of Staphylococcus aureus on various surfaces and their resistance to chlorine sanitizer. J Food Sci 80:M2279–M2286
McWhirter MJ, McQuillan AJ, Bremer PJ (2002) Influence of ionic strength and pH on the first 60 min of Pseudomonas aeruginosa attachment to ZnSe and to TiO2 monitored by ATR-IR spectroscopy. Colloids Surfaces B Biointerfaces 26:365–372
Melo RT, Mendonça EP, Monteiro GP, Siqueira MC, Pereira CB, Peres PABM, Fernandez H, Rossi DA (2017) Intrinsic and extrinsic aspects on Campylobacter jejuni biofilms. Front Microbiol 8:1332–1347
Mıdık F, Tokatlı M, Bagder Elmacı S, Ozcelik F (2020) Influence of different culture conditions on exopolysaccharide production by indigenous lactic acid bacteria isolated from pickles. Arch Microbiol 202:875–885
Mika JT, Thompson AJ, Dent MR, Brooks NJ, Michiels J, Hofkens J, Kuimova MK (2016) Measuring the viscosity of the Escherichia coli plasma membrane using molecular rotors. Biophys J 111:1528–1540
Mishra A, Jha B (2009) Isolation and characterization of extracellular polymeric substances from micro-algae Dunaliella salina under salt stress. Bioresour Technol 100:3382–3386
Mohebi S, Shafiee H-A, Ameli N (2017) Evaluation of enamel surface roughness after orthodontic bracket debonding with atomic force microscopy. Am J Orthod Dentofac Orthop 151:521–527
Montagut AM, Granados A, Lazurko C, El-Khoury A, Suuronen EJ, Alarcon EI, Sebastián RM, Vallribera A (2019) Triazine mediated covalent antibiotic grafting on cotton fabrics as a modular approach for developing antimicrobial barriers. Cellulose 26:7495–7505
Moraes JO, Cruz EA, Souza EGF, Oliveira TCM, Alvarenga VO, Pena WEL, Sant’Ana AS, Magnani M (2018) Predicting adhesion and biofilm formation boundaries on stainless steel surfaces by five Salmonella enterica strains belonging to different serovars as a function of pH, temperature and NaCl concentration. Int J Food Microbiol 281:90–100
Nostro A, Cellini L, Di Giulio M, D’Arrigo M, Marino A, Blanco AR, Favaloro A, Cutroneo G, Bisignano G (2012) Effect of alkaline pH on staphylococcal biofilm formation. APMIS 120:733–742
Premkumar S, Thangamani K (2017) Study of woven and non-woven fabric on water retention property for effective curing of concrete. J Text Inst 108:962–970
Price PB, Sowers T (2004) Temperature dependence of metabolic rates for microbial growth, maintenance, and survival. Proc Natl Acad Sci 101:4631–4636
Qiu Y, Zhou Y, Chang Y, Liang X, Zhang H, Lin X, Qing K, Zhou X, Luo Z (2022) The Effects of ventilation, humidity, and temperature on bacterial growth and bacterial genera distribution. Int J Environ Res Public Health 19:15345–15357
Rogina-Car B, Kovacevic S, Schwarz I, Dimitrovski K (2020) Microbial barrier properties of cotton fabric-influence of weave architecture. Polymers (basel) 12:1570–1587
Salama Y, Chennaoui M, Sylla A, Mountadar M, Rihani M, Assobhei O (2016) Characterization, structure, and function of extracellular polymeric substances (EPS) of microbial biofilm in biological wastewater treatment systems: a review. Desalin Water Treat 57:16220–16237
Sharma D, Misba L, Khan AU (2019) Antibiotics versus biofilm: an emerging battleground in microbial communities. Antimicrob Resist Infect Control 8:1–10
Song F, Koo H, Ren D (2015) Effects of material properties on bacterial adhesion and biofilm formation. J Dent Res 94:1027–1034
Stepanović S, Vuković D, Hola V, Di BG, Djukic S, Ćirkovic I, Ruzicka F (2007) Quantification of biofilm in microtiter plates: overview of testing conditions and practical recommendations for assessment of biofilm production by staphylococci. APMIS 115:891–899. https://doi.org/10.1111/j.1600-0463.2007.apm_630.x
Taglialegna A, Navarro S, Ventura S, Garnett JA, Matthews S, Penades JR, Lasa I, Valle J (2016) Staphylococcal Bap proteins build amyloid scaffold biofilm matrices in response to environmental signals. PLoS Pathog 12:1–34
Tewari S, Sharma S (2020) Rhizobial exopolysaccharides as supplement for enhancing nodulation and growth attributes of Cajanus cajan under multi-stress conditions: a study from lab to field. Soil Tillage Res 198:104545–104555
Tsuneda S, Aikawa H, Hayashi H, Yuasa A, Hirata A (2003) Extracellular polymeric substances responsible for bacterial adhesion onto solid surface. FEMS Microbiol Lett 223:287–292
Varshney S, Pandey P, Gupta D, Sharma S (2020) Role of fabric properties, moisture and friction in transfer of bacteria from fabric to fabric. Text Res J 90:478–485
Varshney S, Sain A, Gupta D, Sharma S (2021) Factors affecting bacterial adhesion on selected textile fibres. Indian J Microbiol 61:31–37
Vasseur P, Vallet-Gely I, Soscia C, Genin S, Filloux A (2005) The pel genes of the Pseudomonas aeruginosa PAK strain are involved at early and late stages of biofilm formation. Microbiology 151:985–997
Wang J, Li Q, Li M-M, Chen T-H, Zhou Y-F, Yue Z-B (2014) Competitive adsorption of heavy metal by extracellular polymeric substances (EPS) extracted from sulfate reducing bacteria. Bioresour Technol 163:374–376
Zheng S, Bawazir M, Dhall A, Kim H-E, He L, Heo J, Hwang G (2021) Implication of surface properties, bacterial motility, and hydrodynamic conditions on bacterial surface sensing and their initial adhesion. Front Bioeng Biotechnol 9:643722–643743
Zmantar T, Kouidhi B, Miladi H, Mahdouani K, Bakhrouf A (2010) A microtiter plate assay for Staphylococcus aureus biofilm quantification at various pH levels and hydrogen peroxide supplementation. New Microbiol 33:137–145
Funding
The work was supported by the Science and Engineering Research Board, Government of India (Grant number: PDF/2021/001456).
Author information
Authors and Affiliations
Contributions
S. D.: funding acquisition; investigation; formal analysis; writing—original draft. S. V.: methodology; investigation. D. G.: supervision; writing—review and editing. S. S.: conceptualization; funding acquisition; project administration; supervision; formal analysis; writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This article does not include any studies with animal or human subjects.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dixit, S., Varshney, S., Gupta, D. et al. Factors affecting biofilm formation by bacteria on fabrics. Int Microbiol 27, 1111–1123 (2024). https://doi.org/10.1007/s10123-023-00460-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10123-023-00460-z