Abstract
Background
Previous studies suggested that metabolic syndrome (MetS) might create a pro-cancer environment and increase cancer incidence. However, evidence on the risk of gastric cancer (GC) was limited. This study aimed to evaluate the association between MetS and its components and GC in the Korean population.
Methods
Included were 108,397 individuals who participated in the large-scale prospective cohort study, the Health Examinees-Gem study during 2004–2017. The multivariable Cox proportional was used to estimate hazard ratios (HRs) and 95% confidence intervals (CIs) on the association between MetS and its components with GC risk. Age was used as the time scale in the analyses. The stratified analysis was performed to determine the joint effect of lifestyle factors and MetS on GC risk in different groups.
Results
During the mean follow-up of 9.1 years, 759 cases of newly diagnosed cancer (408 men and 351 women) were identified. Overall, participants with MetS had a 26% increased risk of GC than those without MetS (HR 1.26; 95% CI 1.07–1.47); the risk increased with the number of MetS components (p for trend 0.01). Hypertriglyceridemia, low HDL-cholesterol, and hyperglycemia were independently associated with the risk of GC. The potential joint effect of MetS and current smokers (p for interaction 0.02) and obesity (BMI ≥ 25.0) (p for interaction 0.03) in GC.
Conclusions
In this prospective cohort study, we found that MetS were associated with an increased risk of GC in the Korean population. Our findings suggest that MetS may be a potentially modifiable risk factor for GC risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although gastric cancer (GC) incidence appears to have declined in the past years, GC still ranks fifth for incidence and fourth for cancer mortality, contributing significantly to the worldwide cancer burden [1]. However, the global incidence rate of gastric cancer is not uniformly distributed and varies among geographical regions and ethnicities. The highest GC incidence rates are observed in Eastern Asia and Eastern Europe. Over 70% of new cases and deaths occur in developing countries and are more common in men [2]. GC is a multifactorial disease; infections, lifestyle, and genetic factors have a role in GC risk. Helicobacter pylori (H. pylori) infection may be the most widely recognized cause of GC, but less than 5% of those infected develop GC [3]. Additionally, dietary factors such as salt-preserved foods and lifestyle factors like alcohol consumption and smoking were considered GC risk factors [4], which are also responsible for metabolic disorders. Although many risk factors of GC are deemed preventable in advance, it seems complicated to identify populations that need intervention or to control indicators that need early management.
Metabolic syndrome (MetS) is a cluster of metabolic disorders, including central obesity, elevated blood pressure, fasting plasma glucose, and dyslipidemia [5]. MetS as a chronic inflammatory disease might create a pro-cancer environment and increase cancer incidence. Several epidemiological studies suggest that MetS and its components may independently or in combination increase the risk of several types of cancer, such as pancreatic cancer [6, 7], colorectal cancer [8,9,10], post-menopausal breast cancer [11,12,13], and liver cancer [14] playing a carcinogenic role in cancers. However, the studies on the association between MetS and GC risk are limited and contradictory. Several studies reported the differently affected by gender and region [15,16,17] and proposed irrelevant results [18,19,20]. To our knowledge, few studies are performed based on prospective cohort studies and had limitations of short observation periods and lack enough GC cases to evaluate the results. They also did not consider MetS components combination and lacked information in GC anatomic subsites and histological type.
Therefore, we evaluated the association between MetS and its components and gastric cancer in the Korean population in the present study. Additionally, investigate the joint effect of lifestyle factors on the association of MetS and GC.
Methods
Data source and study population
The Health Examinees (HEXA) study is a large-scale community-based prospective cohort study. HEXA study recruited participants aged 40–69 years from 38 general hospitals and health examination centers in eight regions around Korea [21]. The baseline survey and data collection were conducted between 2004 and 2013. HEXA-G is a sample subset of the HEXA study, after excluding 21 health centers due to differences in quality control and biospecimen collection processes and the short duration of follow-up. HEXA study design and HEXA-G selection criteria have been published elsewhere [21, 22].
Information at recruitment was collected through a self-administered questionnaire that included demographic and lifestyle information, medical history, and dietary factors. Clinical information was tested by blood. In addition, the study linked incident cancer data from the Korea Central Cancer Registry of Korea National Cancer Center until 2018 and death data from Statistics Korea until 2018.
Among 139,267 HEXA-G participants, we excluded those who did not consent for data linkage with the Korea Central Cancer Registry (n = 23,211) and were diagnosed with cancer either before baseline or within the same year of baseline survey (n = 4037); participants with missing information on MetS related variables (n = 3505) were excluded; participants who diagnosed with GC within two lag year after index date were further excluded. Finally, 108,397 participants, including 37,350 men and 71,047 women, were included in the analysis (Fig. 1). The follow-up of the study participants was defined as the period between the time the baseline study was completed until the date of GC diagnosis, death, or the last follow-up date (December 31, 2018).
All participants were provided with written informed consent before entering the study and were followed up according to a standardized study protocol, and all research was performed in accordance with relevant guidelines. The datasets generated and analysed during the current study are not publicly available due to protect the information of cohort participants but are available from the corresponding author upon reasonable request. This study was approved by the Institutional Review Board (IRB) of Seoul National University Hospital (IRB No. E-2009–117-1159, E-2110–004-1257) and the Ethics Committee of the Korean Genome and Epidemiology Study (KoGES) of the Korea National Institute of Health (IRB No. 2014–08-02-3C-A).
Identification of gastric cancer
The primary outcome was the first occurrence of GC based on the International Classification of Diseases, 10th Revision (ICD-10) coded C16.0 to 16.9. We further classified GC by anatomic subsites according to cardia (C16.0) and non-cardia (C16.1–16.6). Histology subtypes were assessed as intestinal and diffuse type according to the International Classification of Diseases for Oncology 3 codes for Lauren classification: Intestinal type GC, 8012, 8021, 8022, 8031, 8032, 8046,8050, 8082, 8143, 8144, 8201, 8210, 8211, 8220, 8221, 8255, 8260, 8261, 8262, 8263, 8310, 8323, 8480, 8481, 8510, 8512, 8570, and 8576; Diffuse type GC, 8020, 8041, 8044, 8141, 8142, 8145, 8490, and 8806 [23].
Definition of metabolic syndrome
We defined MetS and components according to the National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III) and modified the waist circumference based on Korean population criteria [24, 25]. MetS were defined as participants who satisfied at least 3 of the 5 criteria: (1) Abdominal obesity (men ≥ 90 cm; women ≥ 85 cm); (2) Hypertriglyceridemia (≥ 150 mg/dL); (3) Low HDL-cholesterol (men ≤ 40 mg/dL; women ≤ 50 mg/dL); (4) Elevated blood pressure (≥ 130/85 mm Hg); (5) Hyperglycemia (≥ 100 mg/dL). This MetS definition criterion was commonly used in health examination centers in Korea.
Statistical analyses
Baseline characteristics were compared using the Student's t-test and Chi-square test for continuous and categorical variables. The multivariable Cox proportional, using age as the time-scale, were estimated hazard ratios (HRs) and 95% confidence intervals (CIs) on the association of the MetS, number of MetS components, and individual MetS components with GC risk. We performed analyzes on the total and stratified by gender. Furthermore, we assessed the MetS components and GC risk separately by 1 unit increased risk estimation for each component. In addition to quarter cut-points (Waist circumference: ≤ 81.0 cm, 81.0–86.0 cm, 86.0–90.5 cm, and > 90.5 cm in men, ≤ 72.2 cm, 72.2–78.0 cm, 78.0–83.4 cm, and > 83.4 cm in women; Triglycerides: ≤ 72 mg/dL, 72–104 mg/dL, 104–152 mg/dL, and > 152 mg/dL; High-density lipoprotein cholesterol: > 56 mg/dL, 47–56 mg/dL, 41–47 mg/dL, and ≤ 41 mg/dL in men, > 64 mg/dL, 55–64 mg/dL, 47–55 mg/dL, and ≤ 47 mg/dL in women; Systolic blood pressure: ≤ 110 mm Hg, 110–120 mm Hg, 120–131 mm Hg, and > 131 mm Hg; Diastolic blood pressure: ≤ 70 mm Hg, 70–76 mm Hg, 76–81 mm Hg, and > 81 mm Hg; Fasting glucose: ≤ 85 mg/dL, 85–91 mg/dL, 91–99 mg/dL, and > 99 mg/dL), were calculated separately within each component and investigated the linear trend.
We performed two models in our analysis. Model 1 was adjusted for sex, and Model 2 was additionally adjusted for smoking status (current, former or never), alcohol consumption (current, former or never), family history of cancer, education level (middle school or less, high school or college, undergraduate or more), regular exercise (yes or no), and energy intake (kcal/day).
We further analyzed the associations between MetS and GC anatomic subsite and histologic type. Additionally, in this study, we considered a healthy lifestyle, including physical activity (based on a questionnaire of whether performed sweating physical activities at least once per week), normal body weight (less than 25.0 kg/m2), non-smoking, and non-alcohol intake, to investigate the joint effect of lifestyle factors on the association of MetS and GC. Finally, we divided the population into four risk groups based on MetS status and each lifestyle factor. In these analyses, we did not adjust the corresponding factors. Additive interaction was tested using a likelihood ratio test.
All statistical analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC, USA) and were considered statistically significant with p-values less than 0.05.
Results
A total of 759 new GC diagnoses ( 408 men and 351 women) were identified during a mean 9.1-year follow-up.
Characteristics of study subjects
Table 1 shows the characteristics of participants with and without MetS. According to the definitions of the MetS, about 23% of study participants have three or more MetS components. Individuals with MetS were older, less educated, more likely to drink, had a history of diabetes or hypertension and had higher BMI than those without MetS (Table 1). Moreover, men who had MetS were more likely to be smokers, and women who had MetS were more likely to be single (Supplementary Table 1).
MetS and its components and risk of GC
Table 2 shows the association between MetS and GC risk. Overall, participants with MetS had a 26% increased risk of GC than those without MetS (HR 1.26; 95% CI 1.07–1.47), and an increasing number of Mets components showed a significant linear (p for trend 0.01).). Hypertriglyceridemia (HR 1.16; 95% CI 1.00–1.36), low HDL-cholesterol (HR 1.17; 95% CI 1.01–1.37), and hyperglycemia (HR 1.17; 95% CI 1.00–1.37) were independently associated with GC. When the analysis was stratified by gender, the association with GC risk was significantly increased in men (HR 1.30; 95%CI 1.06–1.60) but marginally increased in women (HR 1.24; 95% CI 0.98–1.57) (Table 3). Men (p for trend 0.03) and women (p for trend 0.05) showed a significant linear trend in the number of MetS components. Among men, increased HR for GC was observed in participants with hyperglycemia (HR 1.27; 95% CI 1.04–1.55), marginally increased for abdominal obesity (HR 1.21; 95% CI 0.99–1.48), and low HDL-C (HR 1.21; 95% CI 0.97–1.51). Whereas among women, marginally increased HR of GC was observed in participants with low HDL-C (HR 1.22; 95% CI 0.99–1.52). The risk of GC was examined at the quartile level of individual MetS components, using the first quartile as the reference category (Supplementary Table 2). In total participants, triglycerides (p for trend 0.05) and HDL-cholesterol (p for trend 0.01) showed a positive trend. A positive trend was found for fasting glucose (p for trend 0.03) in men, and HDL-cholesterol (p for trend 0.04) in women.
Furthermore, we evaluated the relationship between combinations of MetS components and GC risk (Supplementary Table 3). The following four combinations were associated with an increased risk of GC: abdominal obesity, hypertriglyceridemia, and low HDL-C (HR 1.49; 95% CI 1.03–2.15); abdominal obesity, hypertriglyceridemia, and elevated blood pressure (HR 1.52; 95% CI 1.01–2.29); abdominal obesity, low HDL-C, and triglycerides (HR 1.94; 95% CI 1.23–3.07); low HDL-C, triglycerides, and elevated blood pressure (HR 1.91; 95% CI 1.05–3.47).
In anatomic subsite analysis, 35 (4%) cases were cardia GC and 821 (96%) cases were non-cardia GC. We found a significant positive association between MetS and non-cardia GC (HR 1.29; 95% CI 1.10–1.50); however, cardia GC seems to be too few cases to assess the association. In histologic type analysis, 192 (21.9%) cases were diffuse-type GC, while 544 (62.0%) cases were intestinal-type GC. We found a significant positive association between MetS and intestinal-type GC (HR 1.29; 95% CI 1.08–1.55) (Supplementary Table 4).
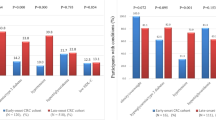
Joint effects between MetS and lifestyle factors on the risk of GC
The assessment of joint effects between MetS and lifestyle factors is presented in Table 4. We found that joint effects of MetS and current smokers, alcohol drinkers, and irregular exercisers independently remained significantly associated with the risk of GC. For the effect of MetS and physical activity, the results showed that the risk of GC increased in participants who had MetS and performed regular exercise (HR 1.37, 95% CI 1.09–1.72) and those with MetS and irregular exercise (HR 1.32, 95% CI 1.05–1.65). For the effect of MetS and BMI, the results showed that the risk of GC was only substantially increased in participants with MetS and obesity (BMI ≥ 25.0) (HR 1.33; 95% CI 1.10–1.60), whereas no significance in MetS and normal BMI. The potential joint effect of MetS and current smokers (p for interaction 0.02) and obesity (BMI ≥ 25.0) (p for interaction 0.03) in GC.
Discussion
In this population-based large-scale prospective cohort study of over a hundred thousand people, we found that MetS were associated with an increased risk of GC in the Korean population. Moreover, GC is independently associated with hypertriglyceridemia, low HDL cholesterol, and hyperglycemia. In addition, smoking status and MetS, BMI and MetS joint effects were strongly related to the risk of GC compared to their individual effects.
Many previous studies reported that obesity, hypertension, hypertriglyceridemia, and hyperglycemia were associated with increased GC risk [26,27,28]. With the prevalence of MetS increasing globally, this public health issue has been paid much attention to in recent decades. However, so far, not many previous studies have investigated the association between MetS and GC risk, and few studies performed by prospective cohort design [26, 27, 29], especially in Asian countries. There is little evidence of the association between metabolic syndrome and the risk of gastric cancer performed in the western population [27, 28, 30]. Moreover, these few cohort studies on the association between MetS and GC have reported inconsistent results with a null [17, 28, 31] or only a positive association in men [30].
In this study, we found that those who have MetS at baseline survey had an increased risk of GC than those without MetS, and having a higher number of MetS components increased the risk of GC. Similar to our findings, in a Norway cohort study, where 192,903 participants were followed for 10.6 years, reported an increased GC risk of 1.44 (1.14–1.82) in individuals with MetS compared to non-MetS [27]. In this study, the sex-specific analyses were also significant for men and women [27]. Furthermore, a 12-year follow-up of 564,596 adults in the European multi-cohorts pooled analysis reported that a higher number of MetS components increased the risk of developing GC (p for trend 0.05) [30]. This study also showed that hyperglycemia, hypertriglyceridemia, and low HDL cholesterol increased GG risk. Other studies supported similar study results for the elevated fasting glucose effect; a Japanese study reported that fasting plasma glucose significantly increased the HR for gastric cancer (HR 3.0. 95%CI 1.5–6.4) [32]. Similarly, in a Norway cohort study, the researchers also found that participants with higher glucose levels had a higher risk of GC [27]. In our meta-analysis of published data, the result also shows a significantly increased risk of GC with high glucose. For other components of MetS, we found that the lower HDL-C was associated with GC, especially showing a trend in women. The potential molecular mechanisms linking HDL-cholesterol to GC remain unclear, and the correlation between them needs further explanation. However, there is consistent evidence that lower HDL-C levels are associated with an increased risk of gastric cancer in women but not in men [16, 33]. A population-based cohort study in Korea found that cholesterol levels, including HDL-C, are inversely related to the risk of gastric cancer among postmenopausal women [34]. Although the exact mechanism of a protective effect of estrogen on gastric cancer is still unclear, it is known that estrogen has anti-inflammatory and anti-oxidant effects [35, 36]. In addition, research reported that estrogen increases the apoptosis of gastric cancer cells [37]. Cholesterol is considered as a major precursor of estrogen, and a possible explanation is that those with high cholesterol level may have relatively high estrogen levels [34]. Other studies have shown that lower HDL-C levels are associated with a higher incidence of gastric dysplasia [38].
An unhealthy lifestyle might play an essential role in mediating the tumorigenesis of MetS. A westernized diet, lack of exercise, frequent drinking, and stress create a complex pro-cancer environment by increasing the prevalence of metabolic diseases [39, 40]. If metabolic syndrome develops first and is left untreated, it creates a pro-cancer environment and significantly increases gastric cancer. In the present study, the HRs increased when MetS and ever smoker, ever drinker and high BMI were jointly assessed for risk of GC compared to MetS who were evaluated alone. Smoking is a well-known risk factor for several cancers; previous studies have reported that MetS and laryngeal cancer were stronger in current smokers than in never smokers suggesting more pronounced effects of MetS on laryngeal cancer [41]. Other studies examined the combined effects of smoking and MetS on the prognosis of patients with colorectal cancer risk and reported that colorectal cancer risk for current smokers with MetS was 1.62 times as high as the sum of risks exposed to each risk factor alone [42]. The extent to which smoking modifies the association between MetS and the risk of GC remains to be elucidated. In previous studies, we have reported the individual effect of alcohol consumption and obesity on the GC risk using the HEXA cohort. The results showed that frequent intake of alcohol increases GC risk [22], and obesity is associated with an increased risk of GC [43]. Alcohol is thought to exert its carcinogenic effect via reactive oxygen production; it acts in the same pathway as the MetS. Few previous studies have shown that physical activity is inversely related to GC [44, 45]. The reasons for these inconsistent findings are hard to verify. Measurement of physical activity is complex, and at least some of the mixed results are likely explained by differences in exposure measurement and intensity cut-offs [44].
The mechanisms linked to MetS and the risk of GC remain uncertain. Several previous studies reported that MetS were considered an additive or synergistic factor in promoting cancer, including GC [30, 46]. Specifically, these components may promote cancer development by generating reactive oxygen species, increasing hormone production/bioavailability, including estrogen, insulin-like growth factor-1, insulin, and adipokines; and providing an energy-rich environment [47,48,49]. The association between the MetS and the risk of cancer mechanism proposed by most previous studies focused on obesity and insulin resistance. It is accepted that insulin resistance is generally considered the primary mechanism responsible for many manifestations of MetS [50, 51]. Since obesity, inflammation, and insulin resistance are interrelated, when a variety of metabolic abnormalities combination work together, the risks of energy imbalance, inflammation, insulin sensitivity, angiogenesis, lipid metabolism, cell proliferation, and atherosclerosis will have a multiplier effect, which may lead to an increased risk of gastric cancer.
Furthermore, impaired insulin secretion and insulin resistance increased the production of reactive oxygen species. More significant oxidative stress causes DNA damage, leading to mutational changes in oncogenes and tumor suppressor genes, which may be related to gastric carcinogenesis [52]. Hyperglycemia and consequent elevated insulin-like growth factors (IGF) are involved in the development of stomach tissues [53]. Long fluctuation in glucose levels increases oxidative stress, endothelial dysfunction, and subclinical inflammation [54], possibly promoting gastric organ damage. Moreover, previous research has demonstrated that insulin enhances the stimulatory effects of epidermal growth factors on the proliferation of cultured gastric epithelial cells, which may predispose the gastric mucosa to genetic or epigenetic changes and, thereby, to the development of carcinogenesis [55]. Scarce glucose might result from the overexpression of glucose transporters and type II hexokinase, which are both confirmed in gastric cancer tissues [56].
One of the strengths of this study is that it was a large-scale prospective cohort study, which included representative participants from the Korean population. Furthermore, this cohort study was linked with death data from Statistics Korea, which could more accurately assess the follow-up period and provide more accurate results. At present, few cohort studies could consider the vital state of follow-up.
A limitation of the present study is that the well-established risk factor for gastric cancer is chronic infection with H.pylori. However, this study did not consider the effect of H.pylori on the association between MetS and gastric cancer development due to the loss of data about H.pylori infection. Although we were unable to determine whether the increased risk of GC in MetS was due to H.pylori, the correlation between MetS and H.pylori infection may be etiologically linked to GC since MetS components have been reported to increase GC risk independently of H.pylori infection in the Japanese population [57]. However, in the Korean population, no endoscopic differences were found in the proportions of H.pylori infection between glucose levels [58]. Moreover, regarding obesity, although BMI may play a modest role in developing GC among individuals with H.pylori infection, a significant association between BMI and GC risk has been reported only in H.pylori uninfected individuals in Korean Multi-Center Cohort study [59]. The authors described that BMI could play a modest role in the development of GC compared to H.pylori infection. In addition, although the relationship between hypertension and gastric cancer is not well known, the considered changes in the stomach's mucosa in patients with portal hypertension [60]. Gastric vascular congestion in portal hypertension gastropathy may suppress H.pylori colonization [61]. However, evidence indicated that gastric disease caused by blood pressure abnormalities such as gastric vascular congestion are not associated with the possibility of H.pylori infection [62]. Therefore independently of H.pylori infection, explaining the MetS and its components and GC risk are clinically meaningful. In addition, in this study, regular exercise combined with MetS, whether done or not, increases the risk of GC. That may be due to possible misclassficaition of the definition of physical activity. In this study, physical activity was investigated using interviewer-administered questionnaires. Information concerning regular exercise was based on who answered about performing regular sweating physical activities [21]. When considering the problem of “frequent” frequency, the minimum range is once or twice a week. With the questionnaire and definition, more people are likely to be defined as ‘regular exercise’ than they performed. Furthermore, we could not consider some related confounders, dietary factors such as salty food, due to lack of data. Subsequent research needs further research. Finally, the association between medication use and development of the metabolic syndrome is increasingly being recognized for several common medications [63]. Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs), for example, have been shown to slightly improve insulin resistance while having no effect on circulating lipids or body weight. In the present study, we lacked information on specific Mets components medication intake, which may affect the association of gastric cancer risk. Thus, future research is warranted to clarify the effect of MetS components medication use and gastric cancer risk.
In conclusion, MetS were associated with an increased risk of GC in the Korean population. Our findings suggest that MetS may be a potentially modifiable GC risk factor. We also recommend that smoking cessation and body mass index control are necessary while managing and intervening in MetS to prevent GC risk.
Data availability
Data from the Health Examinees (HEXA) study is part of the Korean Genome and Epidemiology Study (KoGES), conducted by Korea Disease Control and Prevention Agency (KDCA; formerly Korea Centers for Disease Control and Prevention), Republic of Korea. The Korea Central Cancer Registry (KCCR) data is provisioned by the KDCA in cooperation with the National Cancer Center of Korea as a part of the KoGES. The dataset used for the analysis in this study is maintained and managed by the Division of Population Health Research at the National Institute of Health, which is a part of the Korea Disease Control and Prevention Agency. The Health Examinees Study dataset has been merged with the cancer registry data provided by the National Cancer Center of Korea in a collaborative agreement. It contains some personal data that may potentially be sensitive to the patients, even though researchers are provided with an anonymized dataset that excludes resident registration numbers. Other researchers may request access to the data by contacting the following individuals at the Division of Population Health Research, National Institute of Health, Korea Disease Control and Prevention Agency: Director Dr. Kyoungho Lee (khlee3789@korea.kr).
References
Uncategorized References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2020. https://doi.org/10.3322/caac.21660.
Etemadi A, Safiri S, Sepanlou SG, Ikuta K, Bisignano C, Shakeri R, et al. The global, regional, and national burden of stomach cancer in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease study 2017. Lancet Gastroenterol Hepatol. 2020;5(1):42–54. https://doi.org/10.1016/s2468-1253(19)30328-0.
LA Kidd M, Atherton JC, Louw JA. Heterogeneity in the Helicobacter pylori vacA and cagA genes: association with gastroduodenal disease in South Africa? Gut. 1999;45(4):499–502.
World Cancer Research Fund/American Institute for Cancer Research. The Continuous Update Project Expert Report 2018. Diet, Nutrition, Physical Activity and Cancer: Colorectal Cancer. http://wcrf.org/sites/default/files/Color ectal-cancer-report.pdf. wcrforg/sites/default/files/Colorectal-cancer-reportpdf. Accessed October 23, 2020.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–5. https://doi.org/10.1161/CIRCULATIONAHA.109.192644.
Xia B, He Q, Pan Y, Gao F, Liu A, Tang Y, et al. Metabolic syndrome and risk of pancreatic cancer: a population-based prospective cohort study. Int J Cancer. 2020;147(12):3384–93. https://doi.org/10.1002/ijc.33172.
Johansen D, Stocks T, Jonsson H, Lindkvist B, Bjorge T, Concin H, et al. Metabolic factors and the risk of pancreatic cancer: a prospective analysis of almost 580,000 men and women in the Metabolic Syndrome and Cancer Project. Cancer Epidemiol Biomark Prev. 2010;19(9):2307–17. https://doi.org/10.1158/1055-9965.EPI-10-0234.
Nagel G, Bjorge T, Jaensch A, Peter RS, Haggstrom C, Lang A, et al. Metabolic factors and the risk of small intestine cancers: Pooled study of 800 000 individuals in the metabolic syndrome and cancer project. Int J Cancer. 2021;149(1):66–74. https://doi.org/10.1002/ijc.33530.
Kim J, Park EY, Park E, Lim MK, Oh JK, Kim B. Metabolic syndrome and colorectal cancer risk: results of propensity score-based analyses in a community-based cohort study. Int J Environ Res Public Health. 2020. https://doi.org/10.3390/ijerph17228687.
Pais R, Silaghi H, Silaghi AC, Rusu ML, Dumitrascu DL. Metabolic syndrome and risk of subsequent colorectal cancer. World J Gastroenterol. 2009;15(41):5141–8. https://doi.org/10.3748/wjg.15.5141.
Wani B, Aziz SA, Ganaie MA, Mir MH. Metabolic syndrome and breast cancer risk. Indian J Med Paediatr Oncol. 2017;38(4):434–9. https://doi.org/10.4103/ijmpo.ijmpo_168_16.
Bjorge T, Lukanova A, Jonsson H, Tretli S, Ulmer H, Manjer J, et al. Metabolic syndrome and breast cancer in the me-can (metabolic syndrome and cancer) project. Cancer Epidemiol Biomark Prev. 2010;19(7):1737–45. https://doi.org/10.1158/1055-9965.EPI-10-0230.
Lee JA, Yoo JE, Park HS. Metabolic syndrome and incidence of breast cancer in middle-aged Korean women: a nationwide cohort study. Breast Cancer Res Treat. 2017;162(2):389–93. https://doi.org/10.1007/s10549-017-4131-x.
Jinjuvadia R, Patel S, Liangpunsakul S. The association between metabolic syndrome and hepatocellular carcinoma: systemic review and meta-analysis. J Clin Gastroenterol. 2014;48(2):172–7. https://doi.org/10.1097/MCG.0b013e3182a030c4.
Yoo H, Kim H, Lee JH, Lee KS, Choi MJ, Song HR, et al. Study on the relevance of metabolic syndrome and incidence of gastric cancer in Korea. Int J Environ Res Public Health. 2019. https://doi.org/10.3390/ijerph16071101.
Li F, Du H, Li S, Liu J. The association between metabolic syndrome and gastric cancer in Chinese. Front Oncol. 2018;8:326. https://doi.org/10.3389/fonc.2018.00326.
Ko S, Yoon SJ, Kim D, Kim AR, Kim EJ, Seo HY. Metabolic risk profile and cancer in Korean Men and Women. J Prev Med Public Health. 2016;49(3):143–52. https://doi.org/10.3961/jpmph.16.021.
Lindkvist B, Almquist M, Bjorge T, Stocks T, Borena W, Johansen D, et al. Prospective cohort study of metabolic risk factors and gastric adenocarcinoma risk in the Metabolic Syndrome and Cancer Project (Me-Can). Cancer Causes Control. 2013;24(1):107–16. https://doi.org/10.1007/s10552-012-0096-6.
Osaki Y, Taniguchi S, Tahara A, Okamoto M, Kishimoto T. Metabolic syndrome and incidence of liver and breast cancers in Japan. Cancer Epidemiol. 2012;36(2):141–7. https://doi.org/10.1016/j.canep.2011.03.007.
Matthews CE, Sui X, LaMonte MJ, Adams SA, Hebert JR, Blair SN. Metabolic syndrome and risk of death from cancers of the digestive system. Metabolism. 2010;59(8):1231–9. https://doi.org/10.1016/j.metabol.2009.11.019.
Health Examinees Study G. The Health Examinees (HEXA) study: rationale, study design and baseline characteristics. Asian Pac J Cancer Prev. 2015;16(4):1591–7. https://doi.org/10.7314/apjcp.2015.16.4.1591.
Lee HW, Huang D, Shin WK, de la Torre K, Song M, Shin A, et al. Frequent low dose alcohol intake increases gastric cancer risk: the Health Examinees-Gem (HEXA-G) study. Cancer Biol Med. 2022. https://doi.org/10.20892/j.issn.2095-3941.2021.0642.
Anderson WF, Rabkin CS, Turner N, Fraumeni JF Jr, Rosenberg PS, Camargo MC. The changing face of noncardia gastric cancer incidence among US Non-Hispanic Whites. J Natl Cancer Inst. 2018;110(6):608–15. https://doi.org/10.1093/jnci/djx262.
Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract. 2007;75(1):72–80. https://doi.org/10.1016/j.diabres.2006.04.013.
Hong AR, Lim S. Clinical characteristics of metabolic syndrome in Korea, and its comparison with other Asian countries. J Diabetes Investig. 2015;6(5):508–15. https://doi.org/10.1111/jdi.12313.
Hu D, Peng F, Lin X, Chen G, Zhang H, Liang B, et al. Preoperative metabolic syndrome is predictive of significant gastric cancer mortality after gastrectomy: the Fujian Prospective Investigation of Cancer (FIESTA) Study. EBioMedicine. 2017;15:73–80. https://doi.org/10.1016/j.ebiom.2016.12.004.
Lin Y, Ness-Jensen E, Hveem K, Lagergren J, Lu Y. Metabolic syndrome and esophageal and gastric cancer. Cancer Causes Control. 2015;26(12):1825–34. https://doi.org/10.1007/s10552-015-0675-4.
van Kruijsdijk RC, van der Graaf Y, Peeters PH, Visseren FL, Second Manifestations of Adsg. Cancer risk in patients with manifest vascular disease: effects of smoking, obesity, and metabolic syndrome. Cancer Epidemiol Biomark Prev. 2013;22(7):1267–77. https://doi.org/10.1158/1055-9965.EPI-13-0090.
Yang K, Zhang Y, Saito E, Rahman MS, Gupta PC, Sawada N, et al. Association between educational level and total and cause-specific mortality: a pooled analysis of over 694 000 individuals in the Asia Cohort Consortium. BMJ Open. 2019;9(8):e026225. https://doi.org/10.1136/bmjopen-2018-026225.
Stocks T, Bjorge T, Ulmer H, Manjer J, Haggstrom C, Nagel G, et al. Metabolic risk score and cancer risk: pooled analysis of seven cohorts. Int J Epidemiol. 2015;44(4):1353–63. https://doi.org/10.1093/ije/dyv001.
Inoue M, Noda M, Kurahashi N, Iwasaki M, Sasazuki S, Iso H, et al. Impact of metabolic factors on subsequent cancer risk: results from a large-scale population-based cohort study in Japan. Eur J Cancer Prev. 2009;18(3):240–7. https://doi.org/10.1097/CEJ.0b013e3283240460.
Yamagata H, Kiyohara Y, Nakamura S, Kubo M, Tanizaki Y, Matsumoto T, et al. Impact of fasting plasma glucose levels on gastric cancer incidence in a general japanese population: the Hisayama Study. Diabetes Care. 2005;28(4):789–94. https://doi.org/10.2337/diacare.28.4.789.
Kim EH, Lee H, Chung H, Park JC, Shin SK, Lee SK, et al. Impact of metabolic syndrome on oncologic outcome after radical gastrectomy for gastric cancer. Clin Res Hepatol Gastroenterol. 2014;38(3):372–8. https://doi.org/10.1016/j.clinre.2013.11.009.
Lim JH, Shin CM, Han K, Yoo J, Jin EH, Choi YJ, et al. Nationwide cohort study: cholesterol level is inversely related with the risk of gastric cancer among postmenopausal women. Gastric Cancer. 2022;25(1):11–21. https://doi.org/10.1007/s10120-021-01241-1.
Pfeilschifter J, Köditz R, Pfohl M, Schatz H. Changes in proinflammatory cytokine activity after menopause. Endocr Rev. 2002;23(1):90–119. https://doi.org/10.1210/edrv.23.1.0456.
Kalaitzidis D, Gilmore TD. Transcription factor cross-talk: the estrogen receptor and NF-κB. Trends Endocrinol Metab. 2005;16(2):46–52. https://doi.org/10.1016/j.tem.2005.01.004.
Freedman ND, Chow WH, Gao YT, Shu XO, Ji BT, Yang G, et al. Menstrual and reproductive factors and gastric cancer risk in a large prospective study of women. Gut. 2007;56(12):1671–7. https://doi.org/10.1136/gut.2007.129411.
Jung MK, Jeon SW, Cho CM, Tak WY, Kweon YO, Kweon YO, Kim SK, Choi YH, et al. Hyperglycaemia, hypercholesterolaemia and the risk for developing gastric dysplasia. Dig Liver Dis. 2008;40(5):361–5. https://doi.org/10.1016/j.dld.2007.12.002.
Schmidt DR, Patel R, Kirsch DG, Lewis CA, Vander Heiden MG, Locasale JW. Metabolomics in cancer research and emerging applications in clinical oncology. CA Cancer J Clin. 2021;71(4):333–58. https://doi.org/10.3322/caac.21670.
Lee J, Go TH, Min S, Koh SB, Choi JR. Association between lifestyle factors and metabolic syndrome in general populations with depressive symptoms in cross-setional based cohort study of Ansung-Ansan. PLoS ONE. 2022;17(3):e0262526. https://doi.org/10.1371/journal.pone.0262526.
Kim SY, Han KD, Joo YH. Metabolic syndrome and incidence of laryngeal cancer: a Nationwide Cohort Study. Sci Rep. 2019;9(1):667. https://doi.org/10.1038/s41598-018-37061-0.
Chen DZ, Ji FY, Xu QM, Wu XX, Cai C, Zhang LJ, et al. Interaction of smoking and metabolic syndrome in increasing the recurrence risk of colorectal cancer in a Chinese male cohort: a retrospective study. Sci Rep. 2018;8(1):972. https://doi.org/10.1038/s41598-018-19322-0.
Lee HW, Huang D, Shin WK, de la Torre K, Yang JJ, Song M, et al. Obesity at early adulthood increases risk of gastric cancer from the Health Examinees-Gem (HEXA-G) study. PLoS ONE. 2022;17(2):e0260826. https://doi.org/10.1371/journal.pone.0260826.
Campbell PT, Sloan M, Kreiger N. Physical activity and stomach cancer risk: the influence of intensity and timing during the lifetime. Eur J Cancer. 2007;43(3):593–600. https://doi.org/10.1016/j.ejca.2006.11.011.
Gunathilake MN, Lee J, Jang A, Choi IJ, Kim YI, Kim J. Physical activity and gastric cancer risk in patients with and without Helicobacter pylori infection in a korean population: a hospital-based case-control study. Cancers (Basel). 2018. https://doi.org/10.3390/cancers10100369.
Yoo S, Oh S, Park J, Cho SY, Cho MC, Son H, et al. Effects of metabolic syndrome on the prevalence of prostate cancer: historical cohort study using the national health insurance service database. J Cancer Res Clin Oncol. 2019;145(3):775–80. https://doi.org/10.1007/s00432-019-02842-1.
de Luca COJ. Inflammation and insulin resistance. FEBS Lett. 2008;582(1):97–105.
Saetang J, Sangkhathat S. Diets link metabolic syndrome and colorectal cancer development (Review). Oncol Rep. 2017;37(3):1312–20. https://doi.org/10.3892/or.2017.5385.
Alicka M, Marycz K. The effect of chronic inflammation and oxidative and endoplasmic reticulum stress in the course of metabolic syndrome and its therapy. Stem Cells Int. 2018. https://doi.org/10.1155/2018/4274361.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuniga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):122. https://doi.org/10.1186/s12933-018-0762-4.
Fahed G, Aoun L, BouZerdan M, Allam S, BouZerdan M, Bouferraa Y, et al. Metabolic syndrome: updates on pathophysiology and management in 2021. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms23020786.
Simone S, Gorin Y, Velagapudi C, Abboud HE, Habib SL. Mechanism of oxidative DNA damage in diabetes: tuberin inactivation and downregulation of DNA repair enzyme 8-oxo-7,8-dihydro-2’-deoxyguanosine-DNA glycosylase. Diabetes. 2008;57(10):2626–36. https://doi.org/10.2337/db07-1579.
Yi HK, Hwang PH, Yang DH, Kang CW, Lee DY. Expression of the insulin-like growth factors (IGFs) and the IGF-binding proteins (IGFBPs) in human gastric cancer cells. Eur J Cancer. 2001;37(17):2257–63. https://doi.org/10.1016/S0959-8049(01)00269-6.
Giri B, Dey S, Das T, Sarkar M, Banerjee J, Dash SK. Chronic hyperglycemia mediated physiological alteration and metabolic distortion leads to organ dysfunction, infection, cancer progression and other pathophysiological consequences: an update on glucose toxicity. Biomed Pharmacother. 2018;107:306–28. https://doi.org/10.1016/j.biopha.2018.07.157.
Cevenini A, Orru S, Mancini A, Alfieri A, Buono P, Imperlini E. Molecular signatures of the insulin-like growth factor 1-mediated epithelial-mesenchymal transition in breast, lung and gastric cancers. Int J Mol Sci. 2018. https://doi.org/10.3390/ijms19082411.
Xiao S, Zhou L. Gastric cancer: metabolic and metabolomics perspectives (Review). Int J Oncol. 2017;51(1):5–17. https://doi.org/10.3892/ijo.2017.4000.
Ikeda F, Doni Y, Yonemoto K, Ninomiya T, Kubo M, Shikata K, et al. Hyperglycemia increases risk of gastric cancer posed by Helicobacter pylori infection: a population-based cohort study. Gastroenterology. 2009;136(4):1234–41. https://doi.org/10.1053/j.gastro.2008.12.045.
Yang HJ, Kang D, Chang Y, Ahn J, Ryu S, Cho J, et al. Diabetes mellitus is associated with an increased risk of gastric cancer: a cohort study. Gastric Cancer. 2020;23(3):382–90. https://doi.org/10.1007/s10120-019-01033-8.
Jang J, Cho EJ, Hwang Y, Weiderpass E, Ahn C, Choi J, et al. Association between body mass index and gastric cancer risk according to effect modification by Helicobacter pylori infection. Cancer Res Treat. 2019;51(3):1107–16. https://doi.org/10.4143/crt.2018.182.
Ghosh P, Miyai K, Chojkier M. Gastric adenocarcinoma inducing portal hypertension: a rare presentation. World J Gastroenterol. 2007;13(6):960–3. https://doi.org/10.3748/wjg.v13.i6.960.
Hu JK, Li XM, Gu BH, Zhang F, Li YM, Chen H. Helicobacter pylori and portal hypertensive gastropathy. Hepatobiliary Pancreat Dis Int. 2018;17(6):578–80. https://doi.org/10.1016/j.hbpd.2018.10.007.
Jun YK, Kim JW, Kim BG, Lee KL, Jung YJ, Kim W, et al. Helicobacter pylori infection is not associated with portal hypertension-related gastrointestinal complications: a meta-analysis. PLoS ONE. 2022;17(1):e0261448. https://doi.org/10.1371/journal.pone.0261448.
Wofford MR, King DS, Harrell TK. Drug-induced metabolic syndrome. J Clin Hypertens (Greenwich). 2006;8(2):114–9. https://doi.org/10.1111/j.1524-6175.2006.04751.x.
Acknowledgements
This study was supported by the National Genome Research Institute, Korea Centers for Disease Control and Prevention, and by a grant from the Seoul National University Hospital.
Funding
This work was supported by the Research Program funded by the Korea Centers for Disease Control and Prevention [grant number 2004-E71004-00; 2005-E71011-00; 2005-E71009-00; 2006-E71001-00; 2006-E71004-00; 2006-E71010-00; 2006E71003-00; 2007-E71004-00; 2007-E71006-00; 2008-E7100600; 2008-E71008-00; 2009-E71009-00; 2010-E71006-00; 2011E71006-00; 2012-E71001-00; 2013-E71009-00]. This funding source had roles in study design and data collection.
Author information
Authors and Affiliations
Contributions
DH and DK conceived and designed the study. DH performed the data analysis and drafted the first manuscript. AS, J-KL, and DK collected the data and obtained study funding. W-KS, Kde la T, H-WL, S M, AS, J-KL, and DK provided a critical review of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflicts of interest were disclosed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, D., Shin, WK., De la Torre, K. et al. Association between metabolic syndrome and gastric cancer risk: results from the Health Examinees Study. Gastric Cancer 26, 481–492 (2023). https://doi.org/10.1007/s10120-023-01382-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-023-01382-5