Abstract
Background
This study evaluated the safety, effectiveness, and feasibility of indocyanine green (ICG) tracing in guiding lymph-node (LN) dissection during laparoscopic D2 radical gastrectomy in patients with advanced gastric cancer (AGC) after neoadjuvant chemotherapy (NAC).
Method
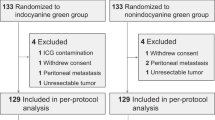
We retrospectively analyzed data on 313 patients with clinical stage of cT1-4N0-3M0 who underwent laparoscopic radical gastrectomy after NAC between February 2010 and October 2020 from two hospitals in China. Grouped according to whether ICG was injected. For the ICG group (n = 102) and non-ICG group (n = 211), 1:1 propensity matching analysis was used.
Results
After matching, there was no significant difference in the general clinical pathological data between the two groups (ICG vs. non-ICG: 94 vs. 94). The average number of total LN dissections was significantly higher in the ICG group and lower LN non-compliance rate than in the non-ICG group. Subgroup analysis showed that among patients with LN and tumor did not shrink after NAC, the number of LN dissections was significantly more and LN non-compliance rate was lower in the ICG group than in the non-ICG group. Intraoperative blood loss was significantly lesser in the ICG group than in the non-ICG group, while the recovery and complications of the two groups were similar.
Conclusion
For patients with poor NAC outcomes, ICG tracing can increase the number of LN dissections during laparoscopic radical gastrectomy, reduce the rate of LN non-compliance, and reduce intraoperative bleeding. Patients with AGC should routinely undergo ICG-guided laparoscopic radical gastrectomy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the fifth most common malignant tumor worldwide and the third highest cause of cancer mortality. Although the 5-year survival rate of patients with early gastric cancer exceeds 90%, for patients with locally advanced gastric cancer (AGC), the 5-year survival rate is low even with radical surgery [1,2,3,4]. In 1994, Kitano et al. [5] reported laparoscopic radical gastrectomy, with the development of minimally invasive equipment and technology, the safety and effectiveness of laparoscopic radical gastrectomy are gradually being recognized [6]. Since the MAGIC trial in 2006, which proved for the first time that preoperative neoadjuvant chemotherapy (NAC) combined with surgery can significantly improve the 5-year overall survival rate of patients with AGC [7], NAC has gradually become an indispensable part of treatment for AGC patients. However, for patients receiving NAC, fibrosis of lymphatic tissue caused by NAC and loss of normal anatomical planes caused by cytotoxicity are technical challenges for laparoscopic lymph-node (LN) dissection [8,9,10]. Although studies have confirmed the safety and feasibility of laparoscopic distal gastrectomy for patients with neoadjuvant gastric cancer, for more technically difficult whole-stomach resections and for inexperienced surgeons, neoadjuvant standard gastric cancer radical resection after chemotherapy is a challenge. In contrast, Taylor et al. [11] found that, due to reasons including tumor downgrading, patients receiving NAC require more LN dissections to truly reflect the prognosis of patients. Therefore, for patients with gastric cancer who have undergone NAC and plan to undergo laparoscopic surgery, surgeons should focus on how to safely complete the operation and complete the standardized and precise LN dissection.
Indocyanine green (ICG) near-infrared light imaging technology, as a new surgical navigation technology, has achieved relatively positive results in sentinel LN dissection and in detecting the location of tumors such as breast cancer and non-small cell lung cancer [11,12,13,14]. Furthermore, in gastric cancer research, prospective studies have reported that ICG can significantly increase the number of LN dissections during laparoscopic radical gastrectomy [15]. However, there is no research to confirm whether ICG technology can also increase the number of LN dissections for patients with AGC who have undergone NAC. To this end, the study is based on a large sample of clinical data from multiple centers, and explores the feasibility of using laparoscopic ICG tracing for LN dissection in patients with AGC receiving NAC, and provides a reference for applying ICG imaging technology in other cavity organs (such as the esophagus and colorectal) after NAC.
Methods
Study design and patient data
We enrolled 329 patients from two hospitals (Fujian Medical University Union Hospital and Qinghai University Affiliated Hospital) with facilities for the electronic storage of clinical data, including medical records, images, and laboratory data, for all consecutive patients with gastric cancer who underwent NAC before gastrectomy between February 2010 and October 2020. Eligible participants were histologically proven to have gastric adenocarcinoma with clinical stageT1–4aN0/+M0 after NAC by a preoperative evaluation according to the 8th staging system of the American Joint Committee on Cancer. The detailed inclusion and exclusion criteria are described in Fig. S1. Preoperative staging was evaluated using computed tomography, optional laparoscopy, or endoscopic ultrasound. The study was approved by the Ethics Committee of Union Hospital affiliated to Fujian Medical University (approval number: 2020WSJK034).
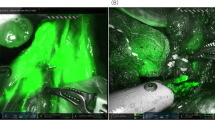
Indocyanine green fluorescence imaging
We used Huang’s subserosal hexa-points maneuver to inject ICG [15]. After preoperative exploration, ICG powder was dissolved in 0.5 mg/mL of sterile water, and the prepared solution (1.5 mL for each point) was injected along the subserosa of the stomach at six specific points along the lesser and greater curvatures of the stomach.
The NOVADAQ fluorescence surgical system (Stryker Corp., Kalamazoo, MI, USA) was used to obtain near-infrared fluorescent images. A simple finger click converted visible light into near-infrared fluorescent images (near-infrared, green fluorescence, and color-segmented fluorescence imaging) without changing equipment. Intraoperatively, the fluorescent mode was switched according to the situation.
Neoadjuvant chemotherapy
The indication for NAC in this study was cT2-4NxM0. NAC was administered to all eligible patients with 2–5 cycles (3 weeks per cycle) of intravenous oxaliplatin (130 mg/m2 on day 1 of each cycle) plus oral S-1 (40–60 mg/m2 twice daily on days 1–14 of each cycle) before surgery. Dose reductions or interruptions were allowed to help patients cope with serious or life-threatening adverse events. Each participant was allowed a maximum of two-dose adjustment. The cumulative time of drug discontinuation of each cycle was not allowed to exceed 2 weeks; drug discontinuance of each cycle should not be more than two times. The premature termination criteria were as follows: disease progression or death; grade 3/4 adverse events still not complete treatment according to the protocol after dose adjustment; patient decision; and researcher decision based on the best interests of the participants. No patients received other forms of perioperative treatment, such as radiotherapy, immunotherapy, or targeted therapy. Response Evaluation Criteria in Solid Tumors (RECIST) [16] guidelines were used to assess the degree of tumor or LN regression after NAC [16].
Standardization of surgical operations
Gastrectomy was performed by a surgeon with experience of > 100 cases of laparoscopic gastrectomy. The abdominal cavity was explored during the operation to check whether the liver, peritoneum, mesenteric, pelvic, and other metastatic gastric serous membranes were invaded. According to the Japanese Gastric Cancer Treatment Guidelines, 5th Edition [17], on the premise that the principles of oncology can guarantee, perform distal gastric or total gastrectomy. The sequence of laparoscopic LN dissection was as follows [18, 19]: (1) total gastrectomy: No. 4d, 6 → No. 7, 9, 11p → No. 8a, 12a, 5 → No. 1 → No. 4sb, 4sa → No. 11d → No. 2; (2) distal gastrectomy: No. 4d, 6 → No. 7, 9, 11p → No. 3, 1 → No. 8a, 12a, 5 → No. 4sb. After LN dissection, a fluorescent mode was used to check for missing LNs within the prescribed range of dissection. If there were missing LNs, remedial dissections were performed. Regarding the regulation of LN dissection outside the scope of D2, the 10th group of LNs underwent selective laparoscopic spleen-preserving splenic hilar LN dissection [20,21,22] when the tumor was located in the greater curvature of the stomach or preoperative imaging assessment showed that splenic hilar LNs were enlarged or during intraoperative imaging of the NO.10 group of LNs. LNs in group 14v were also selectively dissected during intraoperative imaging. The intraoperative images of ICG tracing for the well regression and poor regression groups are shown in Fig. S2.
Definition
Based on the definition of each group of LNs in the Japanese gastric cancer classification [23], the study group’s LN processing method was as follows: after the specimen was isolated, under the fluorescent irradiation produced by the ICG system, the LNs of each group were searched by hand, and the fluorescent and non-fluorescent LNs in each group were collected. After the fluorescent LNs were aliquoted, they were fixed with 10% formalin solution and sent for pathological examination. LN stations with fluorescent LNs were classified as fluorescent stations, and fluorescent LNs in the fluorescent stations were classified as visible LNs. The surgeon checked all specimens and sent them to the pathology department immediately. All pathological examinations were performed in a standard manner.
The LN dissection rate of each group of LNs was defined as the number of patients in whom LNs were detected in each group divided by the total number of patients. In each group of LNs, within the scope of D2 dissection defined by the Japanese gastric cancer protocol, if more than one group of LNs was not detected, the LNs were considered non-compliant [24, 25].
Complications within 30 days after surgery were recorded through hospitalization and discharge summaries, and the severity of the complications was graded according to the Clavien–Dindo scoring system [26]. Estimated blood loss was estimated by calculating the number of gauze pieces and the amount of suction. The operation time definition the time from the start of the skin incision and trocar to the end of abdominal closure.
Statistical analysis
All data were statistically processed using SPSS Statistics for Windows (version 22.0. Chicago, IL, USA) and R language software (version 3.5.3). Continuous variables are represented as means and standard deviations, and categorical variables are presented as numbers and percentages. Continuous variables were analyzed using the t test, while categorical variables were analyzed using the Chi-square test or Fisher’s exact test according to the situation. All tests were two sided, and the significance level was set at P < 0.05. Logistic regression analysis was used to assess the influence of ICG on the number of LN dissections. The propensity scores were calculated using a logistic regression model with the following preoperative factors as covariates: body mass index (BMI), cT, and cN, and a 1:1 (ICG to non-ICG) matching (matched without replacement) with a caliper of 0.01 standard deviation of the estimated logit was performed. The cut-off value of an absolute standardized mean difference above which a meaningful imbalance is indicated is 0.200 [27].
Ethical approval
This study was conducted with the approval of the institutional review boards of all participating hospital.
Results
General information of the study population before and after matching
Before matching, there were 313 patients with AGC who underwent laparoscopic-assisted radical gastrectomy after NAC, and grouped according to whether ICG was injected (ICG group vs. non-ICG group = 102 vs. 211). The two groups of patients differed significantly in terms of body mass index (BMI) and tumor staging (including pT and pN staging and AJCC staging; P < 0.05), but they were comparable in terms of age, gender, Eastern Cooperative Oncology Group score, Body mass index, tumor resection margin, location, surgical procedure, digestive tract reconstruction, tumor size, histological type, and preoperative clinical stage (P > 0.05). According to the 1:1 matching, there were 94 patients in each groups, and the general data between the groups were comparable (P > 0.05, SMD < 0.200, Table 1).
Effect of ICG on the number of LN dissections in all patients
After matching, the total number of LN dissections was significantly higher in the ICG group than in the non-ICG group (40.8 ± 13.7 vs. 31.8 ± 13.5 P < 0.001). In the subgroup analysis, compared with non-ICG group, patients in the ICG group had more D2 LN dissection (39.6 ± 13.2), perigastric LN dissection (21.7 ± 10.7), and extraperigastric LN (19.1 ± 6.7) dissection number (all P < 0.05). The number of LN dissections in the 5–12a subgroup (26.5 ± 10.6) was also significantly higher in ICG group (all P < 0.05), while the number of LN dissections in the 1–4 subgroup was comparable (15.9 ± 7.7 vs. 14.7 ± 8.4, P = 0.308). Furthermore, the number of each subgroup LN dissections in the ICG group was higher than that in the non-ICG group, especially in subgroups 5, 8a, 9, and 12a, were significantly higher than non-ICG group (all P < 0.05, Table 2).
Effect of ICG on the number of LN dissections in patients with different responses to different NAC
After matching, the stratified analysis of NAC according to the RECIST standards showed in patients with non-remission of tumor or LN, including progressive disease (PD) and stable disease (SD), the number of LN dissection in the ICG group was significantly higher than non-ICG group (41.5 ± 12.9 vs. 28.4 ± 12.4, P < 0.001 and 44.9 ± 16.4 vs. 30.4 ± 11.4, P < 0.001, respectively), while in complete response(CR) and partial response(PR) patients, was comparable in two groups (Fig. 1).
Impact of ICG on the non-compliance rate of LNs
The LN dissection rates of subgroup No.12a in total gastrectomy and No.9 in distal gastrectomy in the ICG group were significantly higher than non-ICG group (P < 0.05). However, other subgroup LNs were similar in two groups (all P > 0.05, Supplemental Fig. 3).
The LN non-compliance rate after matching was significantly lower in the ICG group than in the non-ICG group (35.1% vs. 51.1%, P = 0.027). Stratified analysis according to the RECIST standards showed that among patients with non-remission of tumors or LNs after NAC (SD + PD), the LN non-compliance rate was significantly lower in the ICG group than in the non-ICG group (22.4% vs. 56.2%; 23.3% vs. 55.0%, P all < 0.001; Table 3).
Analysis of risk factors for the number of LN dissections
Univariate analysis showed that in patients without ICG injection, cT stage, Tumor remission, LN remission, and Margin affecting the number of LN dissections. Further multivariate analysis showed that non-remission of tumors or LNs affected the number of LN dissections (both P < 0.05; Supplemental Table 1). However, the number of LN dissections in patients who injected ICG was not affected by any factors (P > 0.05; Supplemental Table 2).
Surgery and postoperative recovery
Supplemental Table 3 shows the short-term outcomes after matching. Intraoperative blood loss in the ICG group was significantly lesser than that in the non-ICG group (45.6 ± 19.1 vs. 89.6 ± 89.3 ml, P < 0.001). There were no significant differences in the first exhaust, liquid diet, and postoperative hospital stay (all P > 0.05). After matching, there were 10 complications within 30 days after surgery in the ICG group and 12 in non-ICG group. Overall, there was no difference in the incidence of postoperative complications and Clavien–Dindo grades between the two groups (P > 0.05, Supplemental Table 3). No patients underwent second operations in either group, and no deaths occurred within 30 days after surgery.
Discussion
With the gradual development of laparoscopic technology, further improvement of the accuracy of laparoscopic surgery to efficiently and safely increase the number of LN dissections is a hot topic. In line with this, the safety and effectiveness of the ICG technology used in laparoscopic radical gastrectomy are gradually being recognized [28,29,30,31]. However, in neoadjuvant patients with AGC, fibrosis reaction or cytotoxicity caused by chemotherapy can cause loss of the normal tissue plane. However, evidence regarding whether it will affect LN visualization or tissue discrimination by ICG in these patients is lacking. This study included patients with AGC who underwent laparoscopic radical resection after NAC in two centers in China and analyzed the relationship between ICG injection and the number of LNs dissected and LN non-compliance in detail. Our study shows that ICG can reduce intraoperative blood loss without increasing the operation time and number of complications, and it can guide the surgeon to dissected more LNs during laparoscopic radical gastrectomy after neoadjuvant therapy and reduce the LN non-compliance rate. In particular, for surgical patients with poor chemotherapy effects, the effect is obvious.
The total number of LNs dissected and the LN non-compliance rate are of great significance in radical gastrectomy. Previous studies have confirmed that, regardless of whether the dissected LNs are metastasized, the perigastric LNs are thoroughly dissected during surgery, the number of LNs is detected, and the rate of LN non-conformance is reduced. Accurate staging, selection of appropriate subsequent treatment options, and improvement in prognoses are of great significance. Studies have proven that patients with NAC need more LN dissections to truly reflect the tumor stage and prognosis of patients [11]. Among patients with gastric cancer who did not receive NAC, our center concluded through randomized-controlled trial research that, in the early stage of disease, ICG can guide the surgeon to dissect more LNs and LNs during laparoscopic radical gastrectomy without increasing the operation time and complications, effectively reducing LN inconsistencies in patients undergoing total gastrectomy [15]. However, in patients with AGC receiving NAC, tumor cell metabolism disorder caused by chemotherapy drugs can cause eosinophilic cytoplasm, nuclear enlargement, condensation, cell necrosis, cell dissection and destruction of ducts, neutrophils, and other inflammatory cells. Infiltration and aggregation of monocytes can eventually replace tumor cells with interstitial fibrosis, that is, primary tumors and metastatic LNs shrink due to fibrosis. This phenomenon may block lymphatic drainage [32], and it is inconclusive whether ICG can be used to fully drain lymph fluid in patients with AGC undergoing chemotherapy by visualizing the LNs. We are the first to report this study internationally. The results showed that the average number of LN dissections in patients with AGC who were not injected with ICG and who underwent laparoscopic radical gastrectomy was 31.8, which is equivalent to that reported in international reports [8], but in patients with AGC injected with ICG, this number can reach 40.8; that is, ICG significantly improves the total number of LN dissections in laparoscopic radical gastrectomy. The stratified analysis also showed that the total number of LNs dissected in the ICG group was significantly higher than in the non-ICG group, regardless of the number of LNs in the D2, perigastric, or extragastric ranges. Similarly, the LN non-compliance rate in the ICG group was 35.1%, which was significantly lower than that in the non-ICG group (51.1%). Single- and multi-factor analysis also showed that ICG technology can help surgeons achieve more thorough LN dissection in patients with AGC receiving NAC. We believe this is because the surgeon can clearly visualize blood vessels under the guidance of ICG, which help them confidently and calmly dissect perigastric LNs, ensuring as many LNs as possible are dissected and reducing bleeding caused by vascular damage caused by misjudgment, significantly reducing intraoperative blood loss. We further divided the LNs into subgroups No. 1–4 and No. 5–12a. Intraoperative cleaning of the No. 1–4 subgroups of LNs does not require naked blood vessels, and the removal of subgroups No. 5–12a LNs requires ICG guidance to dissect the perigastric complex blood vessels. The results showed that the number of LN dissections in the No. 1–4 subgroups in the ICG group was comparable to that in the non-ICG group, while the number of LN dissections in the No. 5–12a subgroups was significantly higher than that in the non-ICG group, which confirmed that ICG-guided laparoscopic radical gastric cancer treatment, more LNs are removed during surgery, not because ICG is beneficial to the specimen-sorting LNs, but because ICG helps the surgeon to perform more accurate and effective LN dissection.
This study further showed that the number of LN dissections in the ICG group did not increase in patients with significant tumor or LN regression after NAC, and the LN non-compliance rate was equivalent to that in the non-ICG group. However, ICG can significantly increase the number of LN dissections and reduce the rate of LN non-compliance in patients with tumors or LNs that have not been resolved after chemotherapy. The analysis of risk factors for the number of LN dissections also confirms this result; that is, in patients with tumors and LN remission, ICG was not a factor influencing the increase in the number of LN dissections, but in patients whose tumors and LNs did not shrink, ICG significantly increased the number of LN dissections. Conversely, our analysis also showed that for patients receiving NAC who underwent radical gastrectomy without ICG injection, the number of LN dissections was affected by factors such as cT4, non-remission of tumors after chemotherapy, and LN remission after chemotherapy. In other words, in patients with AGC whose tumors are in the advanced stages after chemotherapy, it is more difficult to clean a sufficient number of LNs during surgery, but after ICG injection, the tumor stage no longer affects the number of LNs dissection. This phenomenon suggests that for patients receiving NAC that has significant effects, fibrosis in the peripheral gastric LNs means that the lymphatic vessels may be blocked, causing poor ICG inflow, resulting in poor intraoperative imaging effects. However, when the tumor or LNs are enlarged after chemotherapy, it is not easy to distinguish the boundary between enlarged LNs and the surrounding tissues, while ICG near-infrared light imaging has good tissue penetration and can effectively identify fatty LNs in the tissues [33, 34]. Because of the different ICG uptake rates, a high-definition laparoscope can collect different signals from different tissues, helping the surgeon to effectively and accurately distinguish between the contours of lymphatic tissue and perigastric blood vessels, fat, pancreas, and other organization to avoid missing LNs, but also, the ICG can better locate the lymph nodes, leading to an increase in the number of lymph nodes dissected in patients with poor chemotherapy effects.
Although this is the first study to evaluate the application of ICG to LN tracing in laparoscopic radical resection after neoadjuvant treatment of malignant tumors, this study has some shortcomings. First, even after very strict matching of underlying factors, there is no guarantee that all confounding factors have been adjusted for in our analysis. To evaluate the accuracy of such studies, it is necessary to perform randomized-controlled trials for further verification. Second, there is currently a lack of long-term follow-up results. In theory, LN dissection under ICG guidance improves accuracy, reducing the spread of tumors in the LNs during the dissection process, and it may increase long-term patient survival. Therefore, further evaluation of ICG imaging technology needs to be conducted in multicenter and long-term follow-up studies. Third, this study was based on a database of Chinese hospitals and skilled surgeons. There are significant differences in the number of gastrectomy performed between the East and the West. Therefore, study results should be further evaluated when applied to other institutions or other regions worldwide. However, we believe that the conclusions obtained in this study provide certain reference values for clinical practice. It is recommended that ICG tracing techniques are routinely performed during laparoscopic radical gastrectomy in patients with ACG who have received NAC.
Overall, ICG tracer technology can increase the number of LN dissections during laparoscopic radical gastrectomy in patients with poor NAC outcomes, reduce the rate of LN non-compliance, and reduce intraoperative bleeding. It is recommended that surgeons should routinely perform ICG-guided laparoscopic radical gastrectomy in patients with AGC who have received NAC.
Data accessibility statement
Huang CM and Yan S had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
Ahn HS, Lee HJ, Hahn S, Kim WH, Lee KU, Sano T, et al. Evaluation of the seventh American Joint Committee on Cancer/International Union Against Cancer Classification of gastric adenocarcinoma in comparison with the sixth classification. Cancer. 2010;116:5592–8.
Sobin LH, Wittekind CH. TNM Classification of Malignant Tumors (6th edn). New York: Wiley-Liss; 2002.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Handbook (7th edn). New York: Springer; 2010.
Ahn HS, Lee HJ, Yoo MW, Jeong SH, Park DJ, Kim HH, et al. Changes in clinicopathological features and survival after gastrectomy for gastric cancer over a 20-year period. Br J Surg. 2011;98:255–60.
Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopyassisted Billroth I gastrectomy. Surg Laparosc Endosc. 1994;4:146–8.
Yu J, Huang C, Sun Y, et al. Effect of laparoscopic vs open distal gastrectomy on 3-year disease-free survival in patients with locally advanced gastric cancer: The CLASS-01 randomized clinical trial. JAMA. 2019;321(20):1983–92. https://doi.org/10.1001/jama.2019.5359.
Cunningham D, Allum WH, Stenning SP, et al. MAGIC trial participants. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11–20.
Li Z, Shan F, Ying X, et al. Assessment of laparoscopic distal gastrectomy after neoadjuvant chemotherapy for locally advanced gastric cancer: a randomized clinical trial. JAMA Surg. 2019;154(12):1093–101. https://doi.org/10.1001/jamasurg.2019.3473.
An JY, Kim KM, Kim YM, Cheong JH, Hyung WJ, Noh SH. Surgical complications in gastric cancer patients preoperatively treated with chemotherapy: their risk factors and clinical relevance. Ann Surg Oncol. 2012;19(8):2452–8. https://doi.org/10.1245/s10434-012-2267-9.
Fujisaki M, Mitsumori N, Shinohara T, et al. Short- and long-term outcomes of laparoscopic versus open gastrectomy for locally advanced gastric cancer following neoadjuvant chemotherapy. Surg Endosc. 2020. https://doi.org/10.1007/s00464-020-07552-1.
Vahrmeijer AL, Hutteman M, van der Vorst JR, van de Velde CJH, Frangioni JV. Image-guided cancer surgery using near-infrared fluorescence. Nat Rev Clin Oncol. 2013;10(9):507–518. https://doi.org/10.1038/nrclinonc.2013.123
Valente SA, Al-Hilli Z, Radford DM, Yanda C, Tu C, Grobmyer SR. Near infrared fluorescent LN mapping with indocyanine green in breast cancer patients: a prospective trial. J Am Coll Surg. 2019;228(4):672–8. https://doi.org/10.1016/j.jamcollsurg.2018.12.001.
Yamashita S, Tokuishi K, Anami K, et al. Video-assisted thoracoscopic indocyanine green fluorescence imaging system shows sentinel LNs in non–small-cell lung cancer. J Thorac Cardiovasc Surg. 2011;141(1):141–4. https://doi.org/10.1016/j.jtcvs.2010.01.028.
Brouwer OR, Klop WMC, Buckle T, et al. Feasibility of sentinel node biopsy in head and neck melanoma using a hybrid radioactive and fluorescent tracer. Ann Surg Oncol. 2012;19(6):1988–94. https://doi.org/10.1245/s10434-011-2180-7.
Chen QY, Xie JW, Zhong Q, et al. Safety and efficacy of indocyanine green tracer-guided LN dissection during laparoscopic radical gastrectomy in patients with gastric cancer: a randomized clinical trial. JAMA Surg. 2020;155(4):300–11. https://doi.org/10.1001/jamasurg.2019.6033.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47. https://doi.org/10.1016/j.ejca.2008.10.026.
Association JGC. Japanese gastric cancer treatment guidelines 2014 (ver 4). Gastric Cancer. 2017;20(1):1–19. https://doi.org/10.1007/s10120-016-0622-4.
Huang CM, Zheng CH. Laparoscopic Gastrectomy for Gastric Cancer. Berlin: Springer; 2015.
Huang CM, et al. Laparoscopic suprapancreatic LN dissection for advanced gastric cancer using a left-sided approach. Ann Surg Oncol. 2015;22:2351.
Huang CM, et al. A 346 case analysis for laparoscopic spleen-preserving No.10 LN dissection for proximal gastric cancer: a single center study. Plos One 2014;9:e108480.
Chen QY, et al. Strategies of laparoscopic spleen-preserving splenic hilar LN dissection for advanced proximal gastric cancer. World J Gastrointest Surg. 2016;8:402–6.
Maezawa Y, et al. Priority of LN dissection for proximal gastric cancer invading the greater curvature. Gastric Cancer. 2018;21:569–72.
Association JGC. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 2011;14:101.
De Steur WO, et al. Quality control of LN dissection in the Dutch Gastric Cancer Trial. Br J Surg. 2015;102:1388–93.
Chen QY, et al. Laparoscopic total gastrectomy for upper-middle advanced gastric cancer: analysis based on LN noncompliance. Gastric Cancer 2019.
Dindo D, et al. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205.
Sabbagh C, Manceau G, Mege D, et al. Is adjuvant chemotherapy necessary for obstructing stage II colon cancer? Results from a propensity score analysis of the french surgical association database. Ann Surg. 2020. https://doi.org/10.1097/SLA.0000000000003832.
Lan Y-T, Huang K-H, Chen P-H, et al. A pilot study of LN mapping with indocyanine green in robotic gastrectomy for gastric cancer. SAGE Open Med. 2017;5(114):2050312117727444. https://doi.org/10.1177/2050312117727444.
Kim T-H, Kong S-H, Park J-H, et al. Assessment of the completeness of LN dissection using near-infrared imaging with indocyanine green in laparoscopic gastrectomy for gastric cancer. J Gastric Cancer. 2018;18(2):161–71. https://doi.org/10.5230/jgc.2018.18.e19.
Tajima Y, Murakami M, Yamazaki K, et al. Sentinel node mapping guided by indocyanine green fluorescence imaging during laparoscopic surgery in gastric cancer. Ann Surg Oncol. 2010;17(7):1787–93. https://doi.org/10.1245/s10434-010-0944-0.
Kwon IG, Son T, Kim H-I, Hyung WJ. Fluorescent lymphography-guided lymphadenectomy during robotic radical gastrectomy for gastric cancer. JAMA Surg. 2019;154(2):150–8. https://doi.org/10.1001/jamasurg.2018.4267.
Hu X. Zhonghua wei chang wai ke za zhi. Chinese J Gastrointest Surg. 2013;16(6):509–12.
Gioux S, et al. Image-guided surgery using invisible near-infrared light: fundamentals of clinical translation. Mol Imaging. 2010;9:237–55.
Schaafsma BE, et al. The clinical use of indocyanine green as a near-infrared fluorescent contrast agent for image-guided oncologic surgery. J Surg Oncol. 2011;104:323–32.
Funding
This work was supported by scientific and technological innovation joint capital projects of Fujian province (2017Y9011, 2017Y9004, and 2018Y9041) and the general project of Startup Fund of Fujian Medical University (2019QH1033).
Author information
Authors and Affiliations
Contributions
Conception and design: Ze-Ning Huang, Cheng-Hao Liu, Wen-Wu Qiu, Su-Yan, and Changming Huang. Provision of study materials or patients: all authors. Collection and assembly of data: all authors. Data analysis and interpretation: Ze-Ning Huang, Cheng-Hao Liu, Wen-Wu Qiu, Su-Yan, Chao-Hui Zheng, and Ping Li. Manuscript writing: all authors. Final approval of manuscript: all authors. Accountable for all aspects of the work: all authors.
Corresponding author
Ethics declarations
Conflicts of interest
There are no conflicts of interest or financial ties to disclose from any of author.
Human rights statement and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or a substitute for it was obtained from all patients for inclusion in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file7 (WMV 82843 KB)
Rights and permissions
About this article
Cite this article
Huang, ZN., Su-Yan, Qiu, WW. et al. Assessment of indocyanine green tracer-guided lymphadenectomy in laparoscopic gastrectomy after neoadjuvant chemotherapy for locally advanced gastric cancer: results from a multicenter analysis based on propensity matching. Gastric Cancer 24, 1355–1364 (2021). https://doi.org/10.1007/s10120-021-01211-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-021-01211-7