Abstract
Tissue injuries that affect the skin and/or adjacent tissues and are usually over a bony prominence are called pressure injuries. The prevalence of these dysfunctions remains high, and despite technological advances, there is no consensus on the most appropriate treatment. The objective of this review was to evaluate the efficacy of photobiomodulation (PBM), ultrasound, and high-frequency electrophysical agents in the healing of pressure injuries in adults and the elderly. The search was conducted in the PubMed, Embase, Cochrane Library, Web of Science, and PEDro databases; in clinical trial records, a list of references of the selected articles, as well as through manual search (Google), of the last 5 years in humans in English and Portuguese. Nine thousand and sixty-seven studies were identified, 13 pre-selected, and 6 were included in this systematic review. PBM showed similar efficacy to other technologies indicated in other studies in healing pressure injuries. PBM with red wavelength (660 nm) in stages 2 and 3 pressure injuries effectively promoted healing compared to standard care. It was observed that the use of PBM accelerates tissue repair in pressure injuries; therapeutic ultrasound showed similar efficacy to other electrophysical agents but was effective in reducing the area of pressure injuries when comparing pre- and post-intervention. No clinical studies using the high-frequency electrophysical agent have been described in the last 5 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previously known as pressure ulcers, decubitus injuries, or bedsores, tissue injuries that affect the skin and/or adjacent tissues and are usually over a bony prominence are called pressure ulcers [1]. A retrospective study conducted according to hospital databases in the USA and Canada showed that 7.2% of adult patients developed pressure injuries [2]. In Brazil, the rate of pressure injuries in hospitalized patients is 16.9% [3].
These data show that, although advances have been made in the prevention and treatment of pressure injuries (PI), there is still a significant number of people affected by this dysfunction. There is a need for standardization and more research on available treatments.
The available treatments aim to stimulate tissue repair, reestablish, and restore the normality of the tissues. For this objective, some conducts can be used to assist this process, such as the use of electrophysical agents. Currently, the electrophysical agents most discussed in the literature are ultrasound, photobiomodulation, and electrostimulation [4,5,6]. The use of physical therapy resources capable of triggering beneficial effects has been justified because they are considered adjuvants in regeneration, promoting healing in the shortest possible time, with minimal pain, discomfort, and scarring, in a physiological environment conducive to tissue repair and regeneration [7].
Machado et al. [8] described photobiomodulation (PBM) as an amplified light of low radiation power capable of promoting biochemical, bioelectrical, and bioenergetic effects that act at the cellular level by promoting increased metabolism and thus the proliferation, maturation, and locomotion of fibroblasts and lymphocytes, intensifying fibrin resorption, increasing the amount of granulation tissue, and decreasing the release of inflammatory mediators. A systematic review by Petz et al. [9] concludes that red-wave PBM (658 nm) showed efficacy in healing pressure injuries similar to other technologies indicated in other studies and can consider PBM a clinical choice for the treatment of pressure injuries in adults and the elderly.
Another electrophysical agent widely used to accelerate healing is therapeutic ultrasound (US), which stimulates or inhibits biochemical and biophysical activities by delivering energy to the affected tissues, improving bioburden, and inhibiting the excessive inflammatory environment [7]. In addition to this function, the US can increase collagen synthesis by stimulating fibroblasts in the proliferative phase, thereby increasing the tensile strength of tissue undergoing healing [10,11,12]. Research based on this information has revealed that US therapies improve soft tissue healing such as Cullum and Liu [13] describe the use of therapeutic US in venous ulcers. The authors conclude that low-frequency ultrasound is widely used in the literature, however, with studies of low methodological quality. A systematic review that aimed to determine whether the US produces beneficial outcomes in wound healing and which parameters should be used to provide better dose–response showed limited evidence of this resource for wound treatment. The scientific base could not clearly answer the dose–response relationship [14].
High frequency (HF) is an electrophysical agent that has been used for the treatment of pressure injuries. Such device operates with alternating current (high-voltage and low intensity) and glass electrodes that contain vacuum (rarefied air) or gas (neon, xenon, or argon) inside; concomitant to the formation of an electric field, it is argued that the HF generator is capable of producing physiological effects resulting from thermal effects produced by the current when crossing the body, generating local heat production, causing peripheral vasodilatation. The other physiological effect occurs due to the sparking produced by the current as it passes through the electrode, described as ozone. The use of ozone (O3) is essential because it eliminates pathogens and then releases oxygen, activates fibroplasia to elaborate intercellular matrix, the proliferation of keratinocytes, and consequently stimulates healing [13].
The mechanisms of action of electrophysical agent photobiomodulation and therapeutic ultrasound are described in the literature. However, we did not find studies that described its mechanism of action for high-frequency equipment. PBM and US both act in the regulation of Ca2 + channels. Furthermore, the mechanism of action of red and near-infrared PBM has its main pathway through mitochondria, with the absorption of cytochrome C oxidase, generating ATP and NO release. In addition, the ultrastructural alteration thus activates pathways for the regulation of gene expression. The mechanism of action of ultrasound occurs through Integrin via the FAK, which activates two pathways initiated by Pho and PI3K, which also activates the regulation of gene expression (Fig. 1) [15,16,17,18,19].
Schematic of the intracellular and molecular mechanism of action of therapeutic ultrasound (US) and photobiomodulation (PBM; NIR = near-infrared). In the photobiomodulation scheme, photons are taken up by chromophores in the mitochondrial crest via the cytochrome C oxidase photoreceptor. After photon absorption, nitric oxide is released, increasing enzymatic activity and ATP production. In addition, it causes an increase in ROS and cAMP, inducing several transcription factors (NF-kB and AP-1). After photon absorption, the authors describe the possible effects: increase in growth factors, increase in cytokine production, cell proliferation and mobility, anti- and pro-inflammatory effects, pain attenuation, improvement in cell survival, and inhibition of cellular apoptosis [15, 16]. In the US scheme, the mechanical waves generated by the ultrasound stimulate membrane integrin receptors. After stimulation, the subsequent phosphorylation of signaling proteins activates two main pathways such as Rho/ROCK/ERK/MAPK and PI3K/Akt/mTOR. After US stimulation, the authors describe the possible effects: improved proliferation, viability, adhesion, migration, and cellular differentiation [17,18,19]
When it comes to healing chronic wounds, especially pressure injuries, the great challenge is establishing reliable guidelines for treating such pathology because there is still a large gap between what can be done and the best way to treat individuals who present such dysfunction. Thus, the objective of this systematic review was to describe the efficacy of the electrophysical agents most used by physical therapy and the parameters described in the literature to determine the best effectiveness in treating pressure injuries in adults and the elderly.
Methods
The systematic review is registered (PROSPERO) under CRD42020178792 and can be accessed at https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=178792
This systematic review was conducted according to the recommendations of the Cochrane manual proposed by Cochrane, and the PRISMA checklist was used for a better description of the study. The PICOT strategy was used to formulate the research question, which resulted in the following question: What is the efficacy of the electrophysical agent ultrasound, high frequency, and photobiomodulation for the healing of pressure injuries in adults and the elderly?
Inclusion criteria
Inclusion criteria were defined based on the question guiding the review: clinical trials, the search was conducted from 2015 to May 2022, target population (humans, adults, and elderly with pressure injuries aged ≥ 20 years regardless of age, sex, and severity of pressure injuries, in any care setting such as hospital, clinic, outpatient clinic, long-term care facility, or home care); interventions considered were photobiomodulation, ultrasound, and high frequency; the methodological criterion was the description of parameters and the quality of the studies (PEDro scale), language (English and Portuguese). A third evaluator resolved disagreements that may have occurred.
Exclusion criteria
For duplicate or identical articles, only the first publication was included. Articles that were not replicable methodological criteria or did not describe how to apply electrophysical agents were excluded.
Search strategy
Studies were identified through an electronic search of PubMed, Embase, and Web of Science databases from 04/08/2020 to 04/11/2020, and on 05/02/2020, a search of Lilacs and PEDro databases was conducted. Manual searches of studies from 04/20/2021 to 04/29/2021 were conducted and considered reference lists of systematic review articles and their included studies; google scholar and gray literature, through open search.
In order to guide the search strategy, we used the descriptors in Health Sciences (Decs), Medical Subject Headings (MeSH), and between terms, according to the specificity of each database: “Pressure Ulcer”[Mesh]) OR “Skin Ulcer”[Mesh]) AND “Low-Level Light Therapy”[Mesh]) OR “Laser Therapy”[Mesh]) OR “Phototherapy”[Mesh]) OR “Lasers”[Mesh]) OR “Ultrasonics”[Mesh] OR “radio waves”[Mesh]) and (random allocation; randomized clinical trial; controlled trial; clinical trial; clinical trial as topic and 5 years, English and Portuguese and humans). Booleans AND and OR were applied between the terms. On 21/01/2022 and 05/05/2022, we performed a new search with the same strategic search to identify new studies. We identified four studies, one case study, two literature reviews, and one randomized clinical trial [20,21,22,23]. No studies were included as they did not meet the inclusion criteria of this review.
Study selection
The selection of the studies occurred in different phases. It was performed by two independent reviewers (AV and JM) and blinded. In cases of doubt or disagreement, a consensus meeting was held with a third reviewer (KH). In the first phase, the titles and abstracts of the initially selected studies were read, and the eligibility criteria previously defined in the present review were applied. The studies selected in the first phase were read in their entirety in the second phase and the eligibility criteria were applied to confirm their inclusion in the present investigation.
Data collection
Evaluation of methodological quality
Methodological quality was assessed by applying the PEDro scale tool, available at (https://www.pedro.org.au/portuguese/downloads/pedro-scale/), according to the following areas: eligibility criteria, random allocation, concealed allocation, baseline comparability, blinded subjects, blinded therapists, blinded assessors, adequate follow-up, intention-to-treat analysis, between-group comparisons, point estimates, and variability. Studies were classified as having low methodological quality if one of the domains, random sequence generation, participant and personnel concealment, and assignment concealment, was considered to be at high risk of bias.
Data extraction
For data extraction, an independent form was used with the following information: (1) study identification and participant characteristics (inclusion and exclusion criteria, number of participants, sex, age) (Table 1), (2) pressure injury characteristics (location of pressure injury, stage, and duration of pressure injury) (Table 2); and (3) intervention characteristics (including information about the type of intervention and control, specific intervention parameters, and application methods considered relevant, as well as outcome assessment instrument) (Table 3).
Data analysis and presentation
The studies were organized and analyzed descriptively according to the results listed for this review. Due to the heterogeneity of the studies, it was not possible to establish summary measures such as relative risk and mean differences between results.
Results
Identification of studies
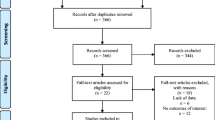
In this systematic review, including individuals with pressure injuries, in the process of detection and selection of studies, we identified 9067 studies in the databases: 2193 in Embase; 1881 in MEDLINE/PubMed; 4956 in Web of Science; 11 in LILACS; 21 in PEDro; 5 in manual search. Using Mendeley, software for bibliographic reference management, 338 articles were found to be duplicates. After reading the titles of 8729, it was seen that 8716 did not meet the inclusion criteria. Therefore, 13 studies were pre-selected. After full reading and consensus meeting, 7 studies were excluded for not meeting the criteria, 2 related to the population, 1 for the intervention, 2 for the type of study described, and 2 for performing only histological analysis without macroscopic analysis. Thus, 6 studies were selected and included in this review (Fig. 2). According to Kappa, the degree of agreement between the reviewers obtained an index of 0.692 for adequacy of the population, 0.769 for adequacy of the intervention, 1.0 for adequacy of the study, and 0.846 for inclusion decision.
As for the clinical characteristics of pressure injury (PI), most of the PI, 82 (48.8%), developed in the buttock region (ischial tuberosity, sacrum, coccyx), four (2.3%) in the trunk, and 27 (16.07%) in the lower extremity, while 11 patients (6.54%) had multiple PI. Romanelli et al. [24] did not describe the clinical characteristics of pressure injuries.
All studies used the classification proposed by the EPUAP-European Pressure Ulcer Advisory Panel and NPUAP-National Pressure Ulcer Advisory Panel: grade IV (loss of tissue thickness with exposure of bone, tendons or muscle, devitalized or necrotic tissue may appear, they are often captivated or fistulized), grade III (total loss of tissue thickness, subcutaneous adipose tissue may be visible, whereas tendons, muscles, and N bone are exposed, and may present some type of devitalized tissue), and grade II (partial loss of dermis thickness presents as a superficial wound with a pink-red bed, without devitalized tissue) [1].
Characteristics of the interventions
As for interventions, the study by Polak et al. [25] compared three experimental groups (A: ultrasound + standard care; B: electrostimulation + standard care; C control: standard care with antiseptics or covered with hydrogel dressings and hydrocolloid wound dressings and antibiotics according to microbiological culture and pressure ulcer smear sensitivity tests). Karsli et al. [10] compared the effectiveness of high-voltage electrical stimulation (HVES) + standard care and ultrasound (US) + standard care in treating pressure injuries of hospitalized patients. Standard care was not described in the article.
In the intervention conducted by Romanelli et al. [24], the effectiveness of photobiomodulation was verified through the use of LED associated with a BioPhotonic gel (LumiHeal™) in the treatment of chronic wounds; of the 33 individuals who participated in the study, 3 had pressure ulcers and received the LED + BioPhotonic gel treatment; the evaluation of the effectiveness of the intervention was done by measuring the wound before and after treatment, with no control group. The study by Ruh et al. [26] investigated the action of the laser for 12 consecutive days on pressure ulcers, assessing the area of the lesion before and after the interventions, and did not report a control group; however, biochemical analysis was performed.
In the research by Bortoli et al. [27], two experimental groups were compared: group 1 papain laser (GLP) AlGaInP (aluminum, gallium, indium, and phosphorus), 660 nm, 4 J/cm2, once a day for 10 days, with the use of dressing with 10% papain solution and group 2 oil laser (GLO) AlGaInP 660 nm, 4 J/cm2, once a day for 10 days, associated with the use of dressing with oil lotion based on essential fatty acids. Chaves et al. [28] compared conventional treatment (cleaning of the lesion with physiological solution, plus a hydrogel-based dressing with alginate) for 4 weeks with conventional daily treatment plus LED application (630 and 940 nm 4 J/cm2) three times a week, totaling 12 sessions; pressure lesions were evaluated by measuring the area and temperature. Follow-up time between studies ranged from 3 to 6 weeks.
As for the parameters of the electrophysical agents (Table 4), a description of 100% of the wavelength was observed for photobiomodulation, and the frequency and emission mode of ultrasound; the energy density (ED) was described in 5 studies not being described in Romanelli et al. [24]; as for the PBM, a variety in the choice of parameters was observed. The power density (PD) was introduced in mW/cm2 and described in all studies, unlike the distance between the application points, which was not described in two studies [24, 28, 29]. The case of dose per diode and dose per tissue was not described in any study.
The duration of treatment was described in all studies, as was the frequency of application, the latter being reported in three studies as daily frequency of application (once a day) at least 5 days a week (Table 4). Another study reported a frequency of 3 times per week, and another, at least one application during the study. Also, in Table 5, other characteristics were observed, and the method of contact with the skin in the case of the ultrasound agent N was reported in one study [9]. In the studies that used PBM, one reported that it kept 5 cm of distance of the light from the skin, the other only described that it used the scanning method, and the third kept 0.5 cm of distance to avoid contact.
Study results
Due to the heterogeneity in the characteristics of the participants (age, location, classification, and duration of pressure injury) and the interventions (irradiation parameters, application methods, and assessment instrument) of the studies, the data were presented descriptively according to the results intended by this review in each study. No studies using the high-frequency electrophysical agent have been described in the last 5 years. Table 5 presents the characteristics of the results of the studies included in this review, the evaluation instruments, and their conclusion; the lesions were evaluated using a planimeter, images captured by a camera, and measured in cm2 and by a conventional ruler. The final area reduction was assessed in all studies.
In the study by Polak et al. [25], after 6 weeks of treatment, the mean reduction in surface area of pressure injuries was significantly lower in all groups, decreasing in the ultrasound group from 10.86 ± 11.59 cm2 at baseline to 3.69 ± 6.23 cm2 after treatment (p < 0.0001), in the electrical stimulation group from 7.48 ± 6.20 to 2.65 ± 4.33 cm2 (p < 0.0001), and in the control group from 9.31 ± 7.27 to 5.33 ± 46.41 cm2 (p < 0.0001). In the research by Karsli et al. [10], the initial averages were 25 and 15 cm2 in the high-voltage electrical stimulation group. In the ultrasound group, the post-treatment values were 17 and 8 cm2, respectively. The percentage changes in the measurements were analyzed, with a decrease of 43% in the electrostimulation group and 63% in the ultrasound group; in intragroup comparisons, a significant reduction was detected comparing pre- and post-treatment: in stage II, electrostimulation group 5 cm2 (20%) and ultrasound group 9 cm2 (40.9%); in stage III, 13 cm2 (52%) of the electrostimulation group and 13 cm2 (59.1%) of the ultrasound group; stage IV, 7 cm2 (28%) of the electrostimulation group and the ultrasound group (0%).
Romanelli et al. [24] assessed the elapsed time to complete wound closure. However, as different wounds were assessed and in the pressure injury group, there were only 3 participants; the N results were interpretable for this category. The wound size of the participants decreased by an average of 78% on day 30, and 100% on day 60 for the pressure injuries. The results of Ruh et al. [26] showed a 50% contraction in irradiated wound diameters after 7 days, as well as increased cell activity at the edge and base of the wound, faster granulation tissue formation, and accelerated wound closure in the irradiated group.
In Bortoli et al. [27], the lesions in the laser plus papain group did not show a significant difference in the treatment performance between the first and the fifth day. Still, a significant difference was observed between the first and the tenth day (F24.8 = 6.885, p < 0.05), equivalent to 39.1% of the wound area, and all wounds showed a decrease in size and improvement in physical appearance during treatment. The average total reduction in the laser plus papain group was 9.50 units of area, which corresponds to a 33% reduction in the lesion area. When evaluating the recovery of the lesions in the laser plus oil group, it was found that there was a significant difference in the performance of the treatment between the first and fifth day (F19.62 = 4.864, p < 0.05) and between the first and tenth day (F19.62 = 5.850, p < 0.05), and the average total reduction of the laser plus oil group was 12.15 area units, corresponding to a 44.5% reduction of the area of the lesions.
In Chaves et al. [28], applying the LED device (630 and 940 nm) at a dose of 4 J/cm2 promoted a higher healing rate in pressure ulcers in the experimental group than in the control group. The pressure lesion area of the group that received LED and conventional treatment decreased over the 12 treatment sessions, while the pressure lesion area of the group that received only conventional treatment increased.
The methodological quality of the studies included in this review was assessed using the PEDro tool, as shown in Table 6.
As for the methodological evaluation performed by the PEDro scale, it was possible to observe that half (50%) of the articles had a higher mean than the world average, which is 5.2 (SD 1.6), considered average; two articles had a mean of 5, and only one article had a mean of 3, considered of low quality [30]. Five of the six studies described that participants were randomized regarding randomized sequence generation. All studies presented a high risk of bias because the participants, the applicators, and the evaluators were not blinded.
Concerning outcomes, only one study did not present sufficient information. The other studies were classified as having a low risk of bias. In the domain of intergroup outcomes, two studies were classified as high risk of bias because the outcomes were not described. Two other studies did not present precision measures as measures of variability for at least one key outcome.
Discussion
In chronic skin lesions, the healing process does not occur adequately or happens slower than expected due to multiple factors [31]. To stimulate the healing of skin lesions, the literature describes the use of physical agents known as therapeutic ultrasound, electrostimulation, negative pressure, photobiomodulation, and high frequency, as adjunctive therapeutic methods to accelerate tissue repair [8, 32,33,34,35,36,37,38]. In this systematic review, we sought to evaluate the effects of photobiomodulation electrophysical agents that include laser and LED, ultrasound, and high frequency in treating pressure injuries.
The six studies included presented the analysis of the efficacy of two physical agents, photobiomodulation (PBM) and ultrasound, in the treatment of pressure injuries, but 2 of the 6 studies did not present a control group, only the analyses before and after treatment, making the analysis of subgroups and meta-analysis impossible. The absence of a control group reduces the reliability of the findings, reducing their use for future studies and the generalizability of the results. In addition, the sample size of the four studies using photobiomodulation was small and heterogeneous. These results corroborate with other reviews, which identified clinical heterogeneity and differences in PBM parameters in the treatment of pressure injuries and ultrasound in other chronic skin wounds [8, 14].
Photobiomodulation (PBM) includes laser and LED (light-emitting diode), the latter being a resource that has biological action mechanisms similar to laser, such as the reduction of inflammatory cells, increased proliferation of fibroblasts, stimulation of angiogenesis, formation of granulation tissue, increased collagen synthesis, and antibacterial action [29, 39, 40]. The irradiation parameters are also similar between LED and laser, with the biological effects depending on the wavelength and dose parameters [29, 39]. For this reason, both laser and LED therapies were included in the present study. In the present review, one study found that LED photobiomodulation + BioPhotonic gel appears to promote healing and accelerate lesion closure. However, the small sample number of pressure injuries makes it impossible to confirm such a statement [24]. Nevertheless, Silveira et al. [40] found that both LED and laser reduce the inflammatory response and oxidative stress, thereby decreasing dermal necrosis and increasing granulation tissue formation, providing an increment in burn wound repair.
The effects of photobiomodulation therapy on cutaneous wounds were addressed in the study by Andrade et al. [26], where several studies demonstrate the beneficial effects of PBM on wound healing in in vitro, in vivo, and clinical studies in humans, accelerating the resolution of such lesions. However, this fact is closely linked to the choice of parameters such as dose, time, and wavelength [41]. These findings corroborate those of the present review, in which the use of PBM showed beneficial effects on the healing of pressure injuries. Still, the application parameters were different among the studies, as well as the way of evaluating the results of the interventions, making it difficult to generalize these results.
The findings of the present systematic review corroborate those of Petz et al. [8], who suggest that in systematic reviews on photobiomodulation, one finds difficulties in addressing a large number of studies with significant sample size and high methodological quality in the treatment of pressure injuries. The small sample size and low methodological quality of the studies reduce the quality of the evidence, leading to imprecise effect estimates and limited confidence in the use of laser for wound area reduction and complete healing and the time required for this to occur [8]. The present study also noted difficulties finding recent studies (last 5 years) with significant sample size and high methodological quality in research using PBM.
According to Petz et al. [8], the divergence of clinical studies using photobiomodulation in pressure injuries, such as the variety of clinical characteristics of PI patients and the clinical characteristics of pressure injuries, limits the evaluation of the effect of this technology. In the studies included in this review, pressure injuries were described in different body parts and classifications according to the National Pressure Ulcer Advisory Panel (NPUAP) [1], with stage III injuries predominating. The divergences found by Petz et al. [8] corroborate the present study. Both the clinical particularities of the individuals and the different characteristics of pressure injuries made data uniformity difficult.
The form of evaluation of the interventions in the studies with PBM and US of the present review differed in each study, using photographs, planimeters, questionnaires, 30 cm ruler, thermography, and healing by spreadsheet. In Petz et al. [8], no study mentioned standardized scales to evaluate the healing process. The use of pressure ulcer scales, such as the PLPH (Pressure Ulcer Scale for Healing) tool and the PSST (Pressure Sore Status Tool), provides uniformity in the magnitude of the measurement of the area (length, width, and depth) of the pressure ulcer [42, 43]. It is possible to assess the quantitative aspects of chronic wound healing and the tissue characteristics through it [44]. The use of standardized, evidence-based scales contributes to a consistent assessment of wound characteristics, and their use is encouraged in clinical settings and recommended in several clinical practice guidelines [45].
Some parameters of the studies that used PBM as intervention N were described, such as energy density, frequency, the distance between points, and irradiation time per point, corroborating the findings of Petz et al. [8] that describe the lack of some important parameters of metrics and their mode of application. The need for standardization in the description of the parameters used in studies is paramount for their reproduction in future studies since the divergence of these parameters can change the biological response, compromising the effect of photobiomodulation, thus not being possible for the reproducibility of studies [8].
In addition to the studies with PBM, 2 studies using ultrasound for the treatment of PI were included. In vitro studies have shown that the existence of leukocytes, production of growth factors and collagen, increased angiogenesis, macrophage reaction, and fibrinolysis are examples of cellular effects induced by such a physical agent [6]. Kavros et al. [46] compared the use of ultrasound in venous lesions with a group that received only standard care, demonstrating in subgroup analysis positive results regarding the use of the electrophysical agent compared with the control. Beheshti et al. [47] demonstrated improvements in lower limb venous lesions with US application compared to standard care, but no difference between high and low frequency. A systematic review has not found sufficient benefit for using ultrasound and photobiomodulation in the treatment of pressure injuries [48]. In the present review, it was possible to observe positive effects regarding the use of US in pressure injuries.
A systematic review by Korelo et al. [35] evaluated whether the US produces beneficial outcomes in wound healing and which parameters provide the best dose–response. Regarding dose–response, there is no agreement among the studies. There is evidence of the US as an adjunctive resource for wound treatment. However, it is not possible to clearly answer the best dose–response relationship. These findings support the findings of the present review, which although demonstrate positive results for the healing of PI pressure injuries, such as the study by Polak et al. [25] that used US in the treatment of PI in the elderly by comparing US + standard care and electrostimulation + standard care. The percentage reduction in PI surface area at the end of treatment, comparing before and after, was significantly greater in the standard care + US group and the standard care + ES group compared to the control group. The groups associated with electrophysical agents did not differ with respect to treatment outcomes. The results show that US and electrostimulation are comparable with respect to their efficacy in reducing the size of PIs in the elderly.
Another study compared the effectiveness of high-voltage electrical stimulation (HVES) with ultrasound [9]. Pressure injuries in the HVES and ultrasound groups were reduced by an average of 43% and 63%, respectively. Changes in wound surface measurements were statistically significant in both groups for all stages, and there was no statistically significant difference between groups. Although the studies show US and electrostimulation intervention methods as promising for PI healing in adults and the elderly, the impossibility of determining the best dose–response to the heterogeneity of the application parameters, the lack of a control group in one of the studies, the evaluation of one of the studies have been only the measurement in cm2, limits the conclusion of which is the best electrophysical agent, may be useful for the healing of pressure injuries.
It can be observed through this systematic review on the effectiveness of electrophysical agents in the treatment of pressure injuries that the difficulty in determining whether such agents are effective or not is due to the lack of methodological rigor in some included studies. It is suggested that new randomized clinical trials be conducted with better methodological conduct and detailed description of the PBM parameters with standardized terminology, homogeneity of the clinical characteristics of the participants, determination of the sample through sample calculation, uniformity in classification, measurement, and evaluation of pressure injuries, as well as the presence of a control group.
Conclusion
This systematic review concludes that PBM showed efficacy in healing pressure injuries similar to other technologies indicated in other studies. PBM with red wavelength (658 nm) at stages 2 and 3 of pressure injuries effectively promoted healing compared to standard care. Although the studies in this review showed heterogeneity regarding participants (comorbidity, age, sample size, clinical characteristics of pressure injuries), interventions (PBM parameters, application methods, and techniques), groups, and comparative outcomes (assessment instrument), PBM may be a choice in practice for the treatment of pressure injuries in adults and the elderly, as no strong evidence was found to refute its clinical application. As for ultrasound, what was observed was the equality of results when compared with electrostimulation and no difference between the interventions and the control group; however, a significant reduction in the areas of the lesions was observed after the use of US when compared before and after interventions to the control group. The scientific production of new randomized clinical trials with a significant number of samples and a better methodological quality may change the confidence in the estimation of the effect of the laser on complete wound healing, time to complete wound healing, and reduction of the pressure lesion area, and therefore the degree of certainty of these results. Thus, the clinical studies available in this systematic review should be considered to guide further trials.
References
Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M (2016) Revised National Pressure Ulcer Advisory Panel pressure injury staging system. J Wound Ostomy Continence Nurs 43(6):585–597. https://doi.org/10.1097/WON.0000000000000281
Kayser SA, Vangilder CA, Ayello EA, Lachenbruch C (2018) Prevalence and analysis of medical device-related pressure injuries: results from the International Pressure Ulcer Prevalence Survey. Adv Skin Wound Care 31(6):276–285. https://doi.org/10.1097/01.ASW.0000532475.11971.aa
Brito PA, Generoso SV, Correia MITD (2013) Prevalence of pressure ulcers in hospitals in Brazil and association with nutritional status-a multicenter, cross-sectional study. Nutrition 29(4):646–649. https://doi.org/10.1016/j.nut.2012.11.008
Pereira ÂL, Bachion MM (2005) Tratamento de feridas: análise da produção científica publicada na Revista Brasileira de Enfermagem de 1970–2003. Rev Bras Enferm 58(2):208–213. https://doi.org/10.1590/s0034-71672005000200016
Qaseem A, Humphrey LL, Forciea MA, Starkey M, Denberg TD (2015) Treatment of pressure ulcers: a clinical practice guideline from the American College of Physicians. Ann Intern Med 162(5):370–379. https://doi.org/10.7326/M14-1568
Oliveira A, Simões S, Ascenso A, Reis CP (2022) Therapeutic advances in wound healing. J Dermatol Treat 33(1):2–22. https://doi.org/10.1080/09546634.2020.1730296
Ennis WJ, Lee C, Plummer M, Meneses P (2011) Current status of the use of modalities in wound care: electrical stimulation and ultrasound therapy. Plastic Reconstr Surg 127(SUPPL. 1 S):93–102. https://doi.org/10.1097/PRS.0b013e3181fbe2fd
Machado RS, Viana S, Sbruzzi G (2017) Low-level laser therapy in the treatment of pressure ulcers: systematic review. Lasers Med Sci 32(4):937–944. https://doi.org/10.1007/s10103-017-2150-9
Petz FFC, Félix JVC, Roehrs H, Pott FS, Stocco JGD, Marcos RL, Meier MJ (2020) Effect of photobiomodulation on repairing pressure ulcers in adult and elderly patients: a systematic review. Photochem Photobiol 96(1):191–199. https://doi.org/10.1111/php.13162
Karsli PB, Gurcay E, Karaahmet OZ, Cakci A (2017) High-voltage electrical stimulation versus ultrasound in the treatment of pressure ulcers. Adv Skin Wound Care 30(12):565–570. https://doi.org/10.1097/01.ASW.0000526606.72489.99
Fyfe MC, Bullock MI (1985) Therapeutic ultrasound: some historical background and development in knowledge of its effect on healing. Aust J Physiother 31(6):220–224
de Oliveira PD, Oliveira DAAP, Martinago CC, Frederico RCP, Soares CP, de Oliveira RF (2015) Effect of low-intensity pulsed ultrasound therapy on a fibroblasts cell culture. Fisioter Pesq 22(2):112–118. https://doi.org/10.0590/1809-2950/12860222022015
Cullum N, Liu Z (2017) Therapeutic ultrasound for venous leg ulcers. Cochrane Database Syst Rev 5:CD001180. https://doi.org/10.1002/14651858.CD001180.pub4
Korelo RIG, Fernandes LC (2017) Ultrassom terapêutico para cicatrização de feridas: revisão sistemática. ConScientiae Saúde 15(3):518–529. https://doi.org/10.5585/conssaude.v15n3.6421
Gupta A (2018) Augmenting wound healing with photobiomodulation therapy, Chap 10; 135–146. In Hamblin MR, Ferraresi C, Huang Y, de Freitas LF, Carroll JD. Low-Level Light Therapy: Photobiomodulation. Tutorial Texts in Optical Engineering Volume TT115; Ed. Spie Press, Bellingham, Washington USA,p. 390.
Mosca RC, Ong AA, Albasha O, Bass K, Arany P (2019) Photobiomodulation therapy for wound care: a potent, noninvasive, photoceutical approach. Adv Skin Wound Care 32(4):157–167. https://doi.org/10.1097/01.ASW.0000553600.97572.d2
de Lucas B, Pérez LM, Bernal A, Gálvez BG (2020) Ultrasound therapy: experiences and perspectives for regenerative medicine. Genes 11(1086):2–20. https://doi.org/10.3390/genes11091086
Yadollahpour A, Mostafa J, Samaneh R, Zohreh R (2014) Ultrasound therapy for wound healing: a review of current techniques and mechanisms of action. J Pure Appl Microbiol 8(5):4071–4085
Leng X, Shang J, Gao D, Wu J (2018) Low-intensity pulsed ultrasound promotes proliferation and migration of HaCaT keratinocytes through the PI3K/AKT and JNK pathways. Braz J Med Biol Res 51(12):e7862. https://doi.org/10.1590/1414-431X20187862
Goyal M, Kothiyal S (2021) Efficacy of deep tissue laser therapy in pressure ulcer healing in patient with quadriplegia: case report. J Physiother Res 11(3):593–598. https://doi.org/10.17267/2238-2704rpf.v11i3.3784
Macedo SPR, Mota MSA, Fagundes CF, de Souza MR, Navarro RS (2021) Effects of photobiomodulation in the treatment of pressure ulcers: integrative review. Res Soc Dev 10(2):e32810212597. https://doi.org/10.33448/rsd-v10i2.12597
Silva JRM, Fernandes MAL, Neiva LM (2021) Comparative analysis of the effects of low power laser on the healing of skin lesions: a systematic review. Braz J Health Rev 4(3):13949–13960. https://doi.org/10.34119/bjhrv4n3-330
Lu Q, Yin Z, Shen X, Li J, Su P, Feng M, Xu X, Li W, He C, Shen Y (2021) Clinical effects of high-intensity laser therapy on patients with chronic refractory wounds: a randomized controlled trial. BMJ Open 11:e045866. https://doi.org/10.1136/bmjopen-2020-045866
Romanelli M, Piaggesi A, Scapagnini G, Dini V, Janowska A, Iacopi E, Scarpa C, Fauverghe S, Bassetto F (2017) EUREKA study - The evaluation of real-life use of a biophotonic system in chronic wound management: an interim analysis. Drug Des Dev Ther 11:3551–3558. https://doi.org/10.2147/DDDT.S142580
Polak A, Taradaj J, Nawrat-Szoltysik A, Stania M, Dolibog P, Blaszczak E, Zarzeczny R, Juras G, Franek A, Kucio C (2016) Reduction of pressure ulcer size with high-voltage pulsed current and high-frequency ultrasound: a randomized trial. J Wound Care 25(12):742–754. https://doi.org/10.12968/jowc.2016.25.12.742
Ruh AC, Frigo L, Cavalcanti MFXB, Svidnicki P, Vicari VN, Lopes-Martins RAB, Leal ECP, De Isla N, Diomede F, Trubiani O, Favero GM (2018) Laser photobiomodulation in pressure ulcer healing of human diabetic patients: gene expression analysis of inflammatory biochemical markers. Lasers Med Sci 33(1):165–171. https://doi.org/10.1007/s10103-017-2384-6
Bortoli I, Prado AL, Kroth A (2016) A efetividade do laser associado a diferentes tipos de curativos na cicatrização de úlceras de pressão. 16 (1), Evidência, Ciência e Biotecnologia 45–58. https://doi.org/10.18593/eba.v16i1.9774
Chaves MEA, Silva FS, Soares VPC, Ferreira RAM, Gomes FSL, Andrade RM, Pinotti M (2015) Evaluation of healing of pressure ulcers through thermography: a preliminary study. Res Biomed Eng 31(1):3–9. https://doi.org/10.1590/2446-4740.0571
Chaves MEA, Piancastelli ACC, Araujo AR, Pinotti M (2014) Effects of low-power light therapy on wound healing. An Bras Dermatol 89(4):616–623
Fitzpatrick RB (2008) PEDro: A physiotherapy evidence database. Med Ref Serv Q 27(2):188–197. https://doi.org/10.1080/02763860802114397
Delavary BM, Van Der Veer WM, Van Egmond M, Niessen FB, Beelen RHJ (2011) Macrophages in skin injury and repair. Immunobiology 216(7):753–762. https://doi.org/10.1016/j.imbio.2011.01.001
Arora M, Harvey LA, Glinsky JV, Nier L, Lavrencic L, Kifley A, Cameron ID (2020) Electrical stimulation for treating pressure ulcers. Cochrane Database Syst Rev 2020(1). https://doi.org/10.1002/14651858.CD012196.pub2
Coltro PS, Ferreira MC, Batista BPSN, Nakamoto HA, Milcheski DA, Tuma Júnior P (2010) Tratamento cirúrgico das feridas complexas: experiência da cirurgia plástica no Hospital das Clínicas da FMUSP TT - Surgical treatment of complex wounds: experience of plastic surgery in the “Hospital das Clínicas – FMUSP”. Rev. Med. (Säo Paulo), 89(3/4), 153–157. http://www.revistas.usp.br/revistadc/article/view/46290/49946
Das Neves LMS, Guirro ECO, Albuquerque FLA, Marcolino AM (2016) Effects of high-voltage electrical stimulation in improving the viability of musculocutaneous flaps in rats. Ann Plast Surg 77(4):e50–e54. https://doi.org/10.1097/SAP.0000000000000621
Korelo RIG, Oliveira JJJ, Souza RSA, Hullek RF, Fernandes LC (2013) Gerador de alta frequência como recurso para tratamento de úlceras por pressão: estudo piloto. Fisioterapia Em Movimento 26(4):715–724. https://doi.org/10.1590/s0103-51502013000400002
Chen C, Hou WH, Chan ES, Yeh ML, Lo HL (2014) Phototherapy for treating pressure ulcers. Cochrane Database Syst Rev 11(7):CD009224. https://doi.org/10.1002/14651858.CD009224.pub2
Al-Wattar WM, Abdulluh BH, Mahmmod AS (2013) Irradiation effect of 780–805nm diode laser on wound healing in mice. J Bagh College Dentistry 25(1):48–52
Hendler KG, Canever JB, de Souza LG, das Neves LMS, Fonseca MCR, Kuriki HU, Aguiar Junior AS, Barbosa RI, Marcolino AM (2021) Comparison of photobiomodulation in the treatment of skin injury with an open wound in mice. Lasers Med Sci 36:1845–1854. https://doi.org/10.1007/s10103-020-03216-7
Silveira PCL, Ferreira KB, Rocha FR, Pieri BLS, Pedroso GS, De Souza CT, Nesi RT, Pinho RA (2016) Effect of low-power laser (LPL) and light-emitting diode (LED) on inflammatory response in burn wound healing. Inflammation 39(4):1395–1404. https://doi.org/10.1007/s10753-016-0371-x
Brauncajs M, Ksiąszczyk K, Lewandowska-Polak A, Gorzela K, Grzegorczyk J (2018) Impact of low-level laser therapy on the dynamics of pressure ulcer-induced changes considering an infectious agent and cathelicidin LL-37 concentration: a preliminary study. Adv Dermatol Allergol 35(6):582–586. https://doi.org/10.5114/ada.2018.77609
Andrade FSSD, Clark RMO, Ferreira ML (2014) Efeitos da laserterapia de baixa potência na cicatrização de feridas cutâneas. Revista Do Colegio Brasileiro de Cirurgioes 41(2):129–133. https://doi.org/10.1590/s0100-69912014000200010
Greatrex-White S, Moxey H (2015) Wound assessment tools and nurses’ needs: an evaluation study. Int Wound J 12(3):293–301. https://doi.org/10.1111/iwj.12100
Santo PFE, de Almeida SA, Silveira MM, Salomé GM, Ferreira LM (2013) Use of the Pressure Ulcer Scale for Healing tool to evaluate the healing of chronic leg ulcers. Rev Bras Cir Plásti 28(1):133–141
Iizaka S, Kaitani T, Sugama J, Nakagami G, Naito A, Koyanagi H, Konya C, Sanada H (2013) Predictive validity of granulation tissue color measured by digital image analysis for deep pressure ulcer healing: a multicenter prospective cohort study. Wound Repair Regen 21(1):25–34. https://doi.org/10.1111/j.1524-475X.2012.00841.x
Bates-Jensen BM, McCreath HE, Harputlu D, Patlan A (2020) Reliability of the Bates-Jensen wound assessment tool for pressure injury assessment: the pressure ulcer detection study. HHS Public Access 27(4):386–395. https://doi.org/10.1111/wrr.12714
Kavros SJ, Liedl DA, Boon AJ, Miller JL, Hobbs JA, Andrews KL (2008) Expedited wound healing with noncontact, low-frequency ultrasound therapy in chronic wounds: a retrospective analysis. Adv Skin Wound Care 21(9):416–423. https://doi.org/10.1097/01.ASW.0000323546.04734.31
Beheshti A, Shafigh Y, Parsa H, Zangivand AA (2014) Comparison of high-frequency and MIST ultrasound therapy for the healing of venous leg ulcers. Adv Clin Exp Med 23(6):969–975. https://doi.org/10.17219/acem/37353
Cullum N, Nelson EA, Flemming K, Sheldon T (2001) Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy. Health Technol Assess 5(9). https://doi.org/10.3310/hta5090
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Registration number
The present study was approved by the PROSPERO and is registered under CRD42020178792 and can be accessed at https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=178792.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vieceli, A.S., Martins, J.C., Hendler, K.G. et al. Effectiveness of electrophysical agents for treating pressure injuries: a systematic review. Lasers Med Sci 37, 3363–3377 (2022). https://doi.org/10.1007/s10103-022-03648-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-022-03648-3