Abstract
Evaluate the effects of antimicrobial photodynamic therapy (aPDT) and photobiomodulation (PBM) as alternatives in the treatment of mastitis in sheep. A total of 100 sheep were evaluated, and four teats with clinical mastitis and 16 teats with subclinical mastitis were selected. Milk was collected for isolation and identification of microorganisms. They were grown on TSA, EMB, and MacConkey agar for 24 h, and the microorganisms were identified by Gram stain and biochemical tests. The ceilings were subdivided into four groups: G1, treatment with photosensitizer; G2, treatment with PBM (diode laser λ = 660 nm); G3, aPDT with methylene blue, and G4, control group. Milk samples were collected before, 24 and 48 h after treatments. Cases of subclinical mastitis presented coagulase-negative Staphylococcus and Streptococcus spp, and clinical mastitis had Escherichia coli grow from the samples. The treatments decrease the total bacterial count of negative coagulase Staphylococcus, Streptococcus spp, and Escherichia coli. Comparing the treatments, aPDT stood out, as it was able to photoinactivate all bacteria. Treatment with methylene blue photosensitizer, PBM, and aPDT induced the initial microbial reduction, but aPDT was more effective 48 h after treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sheep farming is an important income-generating livestock activity in Brazil, where it is in constant expansion. To maintain high gains in the sector, it is essential to implement health care measures for the herd, considering that lack thereof predisposes to the occurrence of many infectious diseases, and one of them is mastitis [1, 2].
Some of the predisposing factors to the occurrence of mastitis or inflammation of the mammary gland are problems related to inadequate hygiene and sanitary management of the Manuscript File. Click here to view linked References animals. This disease causes physical, chemical, and microbiological changes in milk [3].
Mastitis is caused by the proliferation of microorganisms that can penetrate the site, mainly through penetration following the relaxation of the teat sphincter, which occurs after the lamb is suckled or after milking [4].
Mastitis can present clinically or subclinically. The clinical form is characterized by changes such as edema of the mammary gland, increased temperature, pain, and the presence of lumps in the milk [5]. Subclinical mastitis, in turn, is the biggest concern in farming, as there are no visible signs in the udder or the milk, but it causes a high drop in milk yield and the consequent poor lactation of the lamb, besides the risk of transmission to healthy animals [6].
In view of the numerous losses caused by the disease, control, prevention, and treatment measures must be implemented, and the most used treatment of mastitis is based on the use of antimicrobials [7], and the worldwide concern about microbial resistance opens up an opportunity for new treatment modalities [8].
One of such therapeutic alternatives is aPDT. The technique is based on the use of an agent known as photosensitizer (PS), which, upon absorbing a specific wavelength that allows absorption, promotes local oxidative stress through two types of reaction, known as type-I and type-II mechanisms [9].
In type-I reaction, PS transfers H electrons or atoms to the medium in which it is found, allowing the formation of reactive oxygen species such as superoxide anion, hydroxyl radical, and hydrogen peroxide. In type-II reaction, the PS transfers energy to the oxygen molecule, forming singlet oxygen, a potent oxidizer. In both cases, the result is the creation of a local environment that favors oxidative stress, leading to cell death [9].
The technique has been used with clinical success in dentistry, dermatology, and veterinary medicine, among other areas, both for antimicrobial purposes and in the treatment of neoplasms [10, 11].
Moreira et al. [12] employed the technique to treat subclinical mastitis in cattle, using toluidine blue associated with red-emitting LED and described its success in microbial control. Thus, aPDT has been widely used as an alternative to conventional treatments for localized lesions. The advantage of this method is that it does not involve the use of antimicrobials, which prevents the development of microbial resistance [13, 14].
The use of radiation with red light wavelengths can exert beneficial effects on irradiated tissues in a therapy known as PBM, or low-level laser therapy, which reduces local inflammation and promotes analgesia and tissue restoration [15]. Wang et al. [16] developed a model of lipopolysaccharide (LPS)-induced mastitis in rats in which they demonstrated that the LPS-induced secretion of IL-1β and IL-8 decreased significantly after PBM (650 nm, 2.5 mW, 30 mW/cm2).
PBM also inhibited the expression of intercellular adhesion molecule-1 (ICAM-1) and attenuated the decrease in the expression of CD62L induced by LPS and the increase in the expression of CD11b. In this context, the present study proposes to examine the effects of aPDT and PBM on microbial reduction in clinical and subclinical mastitis to open up the possibility of using these therapies as alternatives for the treatment of clinical and subclinical mastitis in sheep.
Materials and methods
Samples origin and general procedures
This study was approved by the Ethics Committee on Animal Use—CEUA/Universidade Brasil (approval no. 1900019). The experiment was carried out on a farm located in Santa Fé do Sul, São Paulo, Brazil.
One hundred sheep (200 teats) were examined for the diagnosis of clinical and subclinical mastitis. The evaluation for the detection of clinical mastitis consisted of observing the udder and performing the strip-cup test. Subclinical mastitis was evaluated by performing the California mastitis test (CMT) on all udder halves.
The strip-cup test was performed by collecting the first three milk jets, which were directed to the strip cup so that changes such as yellow color or the presence of lumps or pus could be observed.
For the CMT, the teats were cleaned with a disinfectant solution and then dried with a paper towel. The milk was collected from each teat (about 2 mL), disregarding the first jets until it reached the mark on the paddle used for the test. Two milliliters of the reagent was added to this sample, which was then homogenized for 20 s. The result of CMT is based on gel formation, and only strongly positive results (+ + +) were considered.
Before treatments, milk samples were collected after antisepsis of the teats using cotton soaked in 70° alcohol, followed by the discard of the first jets. The milk was collected directly in sterile bottles with a lid, which was subsequently labeled, stored in cooler boxes with ice, and immediately sent to the laboratory for identification and microbial counting. The collection was performed 24 and 48 h after the treatments were applied.
Pretrial
After the diagnosis of mastitis, 12 udder halves with clinical mastitis (seven animals) and 16 udder halves with strong positive subclinical mastitis (+ + +) (16 animals) were selected, demonstrating a prevalence of 23% of the examined animals. The experiment was laid out in a completely randomized design with a 2 × 2 factorial arrangement in which the main treatments were split into four groups (G1 [PS], group treated with photosensitizer methylene blue (MB) alone; G2 [laser], group treated with PBM G3 [aPDT], group treated with MB and diode laser (λ = 660 nm); and G4 [control], no treatment) and the second factor was the evaluation times (0, 24, and 48 h). The study was performed in triplicate for clinical and four times for the subclinical cases. The methodology used in the treatments followed the recommendations of Cieplik et al. [10] and Moreira et al. [12]. The treatments were performed only once.
Main trial
After manual milking, the udder allocated in G1 was treated with 0.3 mL of MB in an aqueous solution (0.01% methylene blue, Sigma-Aldrich, USA). The solution was applied to the mammary parenchyma and teats using a sterile catheter after sterilizing the area with 70% alcohol. Subsequently, the region was massaged allowing the penetration of the PS into the gland.
In G2, after milking, the udder halves were irradiated with a diode laser (Therapy EC – DMC Equipamentos, São Carlos Brazil) with an output power of 100 mW, wavelength of 660 nm, and exposure time of 60 s. The energy delivered under these specifications was 6 J, with a fluency of 210 J/cm2 and a spot size of 0.028 cm2 on two levels. After prior local cleaning, a catheter attached to the laser equipment was introduced into the teat canal, followed by compression of the teat so that the application reached the glandular parenchyma (level 1). Then, the catheter was lowered for the application on level 2, which involved the teat cistern and the beginning of the gland cistern.
In G3, after milking, 0.3 mL of MB 0.01% was applied to the mammary parenchyma using a catheter after the previous cleaning. After application, the region was massaged for PS distribution into the mammary parenchyma with a pre-irradiation time of 3 min. Irradiation was carried out with the same parameters as previously described (λ = 660 nm, 100 mW, 6 J, and 210 J/cm2). The same two steps irradiation was performed as described in G2 to reach all tissue depth.
In G4, no treatment was performed; milk was only collected for isolation and identification of the agent and microbial counting.
All groups received only one session of treatment.
Microbiological assay
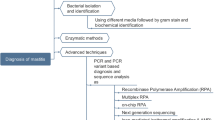
To isolate and identify the microorganisms, the milk samples collected before the treatments were cultured on blood agar (5%), Methylene Blue Eosin Agar (MBE), and MacConkey medium followed by incubation at 37 °C for 48 h. After this period, the colonies were identified based on morphology and staining characteristics (Gram stain). Further biochemical tests were performed as follows: carbohydrate fermentation, nitrate reduction, motility, indole, Simmons citrate, catalase, and coagulase.
The samples collected before and 24 and 48 h after treatment were used for the standard plate count (SPC) of the microorganisms. For this step, decimal dilutions were prepared using peptone saline solution (0.1%) as diluent. Afterward, 1 mL of each dilution (up to 10–4) were deposited in Petri dishes containing trypticase soy agar (TSA) in quadruplicate and incubated in a BOD incubator at 37 °C for 24 h.
Statistical analyses
To calculate the SPC, the colonies were counted and, subsequently, the arithmetic means were obtained by multiplying the number found by the inverse of the dilution, which generated the number of colony-forming units (CFU) per milliliter of milk.
The collected data were arranged in a table, and the effect of the isolated factors and their interaction on microbial count was evaluated by analysis of variance (ANOVA). In the case of statistical significance (p < 0.05), the Scott-Knott test was used to compare the means. The analyses were performed using SISVAR 5.6 software [17].
Results
One hundred sheep (200 teats) were evaluated to detect animals positive for clinical and subclinical mastitis. For this investigation, 7 teats were enrolled in each experimental group, and as abovementioned, a 23% prevalence of mastitis, both clinical and subclinical, was detected in the herd.
Figure 1 summarizes the main pathogens isolated and identified in our research. Coagulase-negative Staphylococcus (81.2%) and Streptococcus spp (18.8%) were isolated from the cases of subclinical mastitis, whereas Escherichia coli was mainly isolated from the cases of clinical mastitis.
Pathogens isolated from cases of clinical and subclinical mastitis in sheep in the northwest region of São Paulo, Brazil, 2020. From the 28 detected cases of mastitis both clinical and subclinical 12 cases presented E. coli, 3 cases with Streptococcus spp, and 13 cases with Coagulase-negative Staphylococcus. Source: Developed by the authors
After the sheep with clinical and subclinical mastitis were identified, they received the treatments proposed in this study. The statistical results of microbial count over time for the treatment of clinical mastitis are described in Table 1. As we can observe, both treatments (PBM and aPDT) showed a statistically significant difference over time, meanwhile, PS alone and control showed no difference in any time interval.
After 24 h, aPDT showed a 1-log reduction in the bacterial count, and 48 h after treatment, we did not recover any bacteria, denoting a microbial reduction of about 5 logs. In the meantime, in the PBM group, after 48 h, we obtained a 2-log microbial reduction.
The results for subclinical mastitis are presented in Table 2. A statistically significant difference was observed after 24 h of treatment for G2 and G3. In 48 h, the PBM group presented a 3-log of bacterial reduction and aPDT group a 5-log reduction without microbial recovery.
Therefore, we observed that after 24 h, PBM and aPDT treatments caused a significant decrease in the total bacterial count of coagulase-negative Staphylococcus, Streptococcus spp, and E. coli, both in the cases of clinical and subclinical mastitis, when compared with the control group. We also observed that the use of 0.01% MB (G1) did not have a notable cytotoxic effect against the tested bacteria, as the reduction in microbial load did not show any significant difference from the control group.
Discussion
The prevalence of subclinical mastitis in sheep herds was 31.4% in experiments led by Acosta et al. [18], and it was also reported in the study of MacDougall et al. [19]. MacDougall et al. [19] also mentioned an average prevalence rate of 23.3%% of clinical mastitis in herds of small ruminants, whereas Oget et al. [20] stated that the incidence of mastitis has increased and it has a burden on the animal’s body weight and the overall production of the flock.
These data are similar to those found in the present study (23%); however, data on the prevalence of mastitis in small ruminants are still scarce [21].
The main infectious agents related to the cases of subclinical mastitis in this study were coagulase-negative Staphylococcus and Streptococcus spp, and in the cases of clinical mastitis, E. coli. Data from other studies corroborate these findings, indicating the coagulase-negative Staphylococcus is the main contagious agent of mastitis in ruminants and Streptococcus spp, Enterococcus spp, E. coli, and Klebsiella pneumoniae as environmental agents [20, 22,23,24,25,26,27].
After the sheep with clinical and subclinical mastitis were identified, the treatments proposed in this study (PBM and aPDT) were carried out, and two control groups, one without treatment, and the other with only PS were also evaluated. We did not find a notable cytotoxic effect of methylene blue on the evaluated pathogens. These findings are similar to those described in other studies, in which no deleterious effects were found on microorganisms with the isolated use of methylene blue [27,28,29,30,31].
The PBM and aPDT techniques showed greater efficiency, given the decrease in TBC. By contrast, Prates et al. [30] and Sellera [31] did not observe a cytotoxic effect of PBM on the tested microorganisms. However, it should be noted that the experiments developed in the cited studies were performed in vitro, unlike the present study.
Malinowski et al. [32], in turn, employed PBM in cattle with mastitis and observed positive effects on microbial recovery. Nussbaum et al. [33] also reported a possible microbial reduction following the application of PBM with different wavelengths, although the observed decrease cannot be characterized as antimicrobial. In addition, PBM also suppressed polymorphonuclear neutrophils (PMNs) induced by LPS that entered the alveoli of the mammary gland. The number of PMNs in the mammary alveoli and myeloperoxidase activity decreased after irradiation. These results suggest that the therapy could be beneficial in reducing somatic cell count and improving the nutritional quality of milk from cows with intramammary infection, according to the authors [16].
The application of aPDT, on the other hand, has been proven, for some years, to be effective in inactivating microorganisms, as demonstrated in this study [12, 34].
According to Reginato et al. [35], the immunological effects of aPDT make the therapy more effective when used in the treatment of bacterial infections due to the increased infiltration of neutrophils in the infected regions that seem to potentiate the treatment result.
Thus, the effect seen after 48 h may be due to the disorganization of biofilm followed by an immune response that would lead to the clinical resolution of the case.
Antimicrobial photodynamic therapy has already been reported to be effective in the control of microorganisms as Streptococcus dysgalactiae, coagulase-positive Staphylococcus, coagulase-negative Staphylococcus, Bacillus spp, Staphylococcus aureus, Streptococcus agalactiae, Corynebacterium bovis, and 12 other isolates].
The use of light therapies, such as aPDT, photodetection, and PBM, among others, has been largely adopted for the treatment of diseases, suggesting their potential beneficial effect on human and animal health [36].
The results presented here reveal the potential of aPDT to cause the inactivation of pathogenic microorganisms related to cases of clinical and subclinical mastitis in sheep.
Nevertheless, further studies are warranted to examine this ability against other pathogens also related to cases of mastitis in sheep, as well as to identify the role of the PBM and aPDT therapies in the immune system so the clinical mechanisms of action of both therapies can be understood.
Conclusion
Based on the microbiological results, treatment with PBM and aPDT in vivo induced a reduction in the initial TBC of coagulase-negative Staphylococcus, Streptococcus spp, and E. coli, which cause clinical and subclinical mastitis in sheep. Antimicrobial photodynamic therapy stood out as compared with PBM since aPDT was able to stop microbial growth, as verified by the microbial reduction 48 h after treatment. This result is promising since aPDT can be used as an alternative treatment for cases of clinical and subclinical mastitis in sheep. Further studies are warranted to support the use of these techniques in farms since the lack of research in the literature involving the use of aPDT and PBM to treat clinical and subclinical mastitis in sheep makes the present study a pioneer.
Data availability
Not applicable.
Code availability
Not applicable.
References
Peixoto RM, França CAD, Souza Júnior AF et al (2010) Etiologia e perfil de sensibilidade antimicrobiana dos isolados bacterianos da mastite em pequenos ruminantes e concordância de técnicas empregadas no diagnóstico. Pesquisa Veterinária Brasileira 30:735–740
Menzies PI, Ramanoon SZ (2001) Mastitis of sheep and goats. Vet Clin North Am Food Anim Pract 17(2):333–58, vii
Zafalon LF, Cunha MLRS, Riboli DFM et al (2017) Persistência de Staphylococcus coagulase-negativos em glândulas mamárias de ovelhas com mastite subclínica após o tratamento antimicrobiano à secagem. Ciência Animal Brasileira 18:1–11
Guaraná ELS, Santos RA, Campos AGSS et al (2011) Dinâmica celular e microbiológica do leite de ovelhas Santa Inês acompanhadas durante a lactação. Pesquisa Veterinária Brasileira 31:851–858
Pantoja JCF, Hulland C, Ruegg P (2009) Somatic cell count status across the dry period as a risk factor for the development of clinical mastitis in the subsequent lactation. J Dairy Sci 92:139–148
Mavrogianni VS, Menzies PI, Fragkou IA et al (2011) Principles of mastites treatment in sheep and goats. Vet Clin N Am Food Anim Pract 27:115–120
Naccari F, Martino D, Giofrè F et al (2003) Therapeutic efficacy of tilmicosin in ovine mammary infections. Small Rumin Res 47:1–9
Souza CN, Almeida AC, Xavier MTR et al (2017) Atividade antimicrobiana de plantas medicinais do cerrado mineiro frente a bactérias isoladas de ovinos com mastite. Revista UNIMONTES Científica 19:51–61
Baptista MS, Cadet J, Di Mascio P et al (2017) Type I and type II photosensitized oxidation reactions: guidelines and mechanistic pathways. Photochem Photobiol 93:912–919
Cieplik F, Deng D, Crielaard W, Buchalla W, Hellwig E, Al-Ahmad A, Maisch T (2018) Antimicrobial photodynamic therapy - what we know and what we don’t. Crit Rev Microbiol 44(5):571–589
Queirós C, Garrido PM, Maia J et al (2020) Photodynamic therapy in dermatology: beyond current indications. Dermatol Ther 33(6):e13997
Moreira LH, Souza JCP, Lima CJ et al (2018) Use of photodynamic therapy in the treatment of bovine subclinical mastitis. Photodiagn Photodyn Ther 21:246–251
Kashef N, Hamblin MR (2017) Can microbial cells develop resistance to oxidative stress in antimicrobial photodynamic inactivation? Drug Resist Updat 31:31–42
Ribeiro MS, Gargano RG, Sabino CP et al (2018) Clinical challenges of antimicrobial photodynamic therapy for bovine mastitis. Photodiagnosis Photodyn Ther 21:327
Andrade FSSD, Clark RMO, Ferreira ML et al (2014) Efeitos da laserterapia de baixa potência na cicatrização de feridas cutâneas. Rev Col Bras Cir 41:129–133
Wang Y, He X, Hao D et al (2014) Low-level laser therapy attenuates LPS-induced rats mastitis by inhibiting polymorphonuclear neutrophil adhesion. J Vet Med Sci 76:1443–1450
Ferreira DF. Sisvar. Software estatístico. Versão 5.6. 2018. Disponível em: http://www.dex.ufla.br/~danielff/programas/sisvar.html. Acesso em 20 ago. 2020
Acosta AC, Silva LBG, Medeiros ED et al (2016) Mastites em ruminantes no Brasil. Pesquisa Veterinária Brasileira 36:565–573
McDougall S, Malcolm D, Prosser C (2014) Prevalence and incidence of intramammary infections in lactating dairy goats. N Z Vet J 62(3):136–145
Oget C, Tosser-Klopp G, Rupp R (2019) Genetic and genomic studies in ovine mastitis. Small Rumin Res 176:55–64
Contreras A, Sierra D, Sánchez A et al (2007) Mastitis in small ruminants. Small Rumin Res 68:145–153
Peixoto RM, Mota RA, Costa MM (2010) Mastite em pequenos ruminantes no Brasil. Pesquisa Veterinária Brasileira 30:754–762
Monteiro JS, de Oliveira SC, Pires Santos GM, Pires Sampaio FJ, Pinheiro Soares LG, Pinheiro AL (2017) Effectiveness of antimicrobial photodynamic therapy (AmPDT) on Staphylococcus aureus using phenothiazine compound with red laser. Lasers Med Sci 32(1):29–34
Bandeira FS, Picoli T, Zani JL et al (2013) Frequency of Staphylococcus aureus from bovine subclinical mastitis cases, in southern Rio Grande do Sul, Brazil. Arq Inst Biol 80:1–6
Castelani L, Santos AFS, Santos MM et al (2013) Molecular typing of mastitis-causing Staphylococcus aureus isolated from heifers and cows. Int J Mol Sci 14:4326–4333
Kulkarni AG, Kaliwal B (2013) Bovine mastitis: a review. Int J Recent Sci Res 4:543–548
Jamali H, Radmehr B, Ismail S (2014) Short communication: prevalence and antibiotic resistance of Staphylococcus aureus isolated from bovine clinical mastites. J Dairy Sci 97:2226–2230
Zanin IC, Lobo MM, Rodrigues LK et al (2006) Photosensitization of in vitro biofilms by toluidine blue O combined with a light-emitting diode. Eur J Oral Sci 114:64–69
Hajim KI, Salih DS, Rassam YZ (2010) Laser light combined with a photosensitizer may eliminate methicillin-resistant strains of Staphylococcus aureus. Lasers Med Sci 25:743–748
Prates RA, Silva EG, Suzuki LC et al (2010) Parâmetros de irradiação influenciam na inativação de leveduras tratadas com terapia fotodinâmica. Revista Brasileira de Física Médica 4:53–57
Sellera FP (2014) Fotoinativação de patógenos causadores da mastite bovina. Dissertação (Mestrado em Ciências). Universidade de São Paulo, São Paulo
Malinowski E, Krumrych W, Markiewicz H (2019) The effect of low intensity laser irradiation of inflamed udders on the efficacy of antibiotic treatment of clinical mastitis in dairy cows. Vet Ital 55(3):253–260
Nussbaum EL, Lilge L, Mazzulli T (2003) Effects pf 630-, 660-, 810-, and 905-nm laser irradiation delivering radiant exposure of 1–50J/cm2 on three species of bacteria in vitro. J Clin Laser Med Surg 20:325–333
Sellera FP, Sabino CP, Ribeiro MS et al (2016) In vitro photoinactivation of bovine mastitis related pathogens. Photodiagnosis Photodyn Ther 13:276–281
Reginato E, Wolf P, Hamblin MR (2014) Immune response after photodynamic therapy increases anti-cancer and anti-bacterial effects. World J Immunol 27:1–11
Sorbellini E, Rucco M, Rinaldi F (2018) Photodynamic and photobiological effects of light-emitting diode (LED) therapy in dermatological disease: an update. Lasers Med Sci 33:1431–1439
Acknowledgements
Universidade Brasil, Campus Fernandópolis amd CNPq – Conselho Nacional de Desenvolvimento Científico e Tecnológico
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by all authors. The first draft of the manuscript was written by Silvia Cristina Nunez and Danila Fernanda Rodrigues Frias, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The research project that gave rise to this study was approved by the Ethics Committee for the Use of Animals – CEUA/Universidade Brasil, under protocol no. 1900019.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Silva, L.O., da Silva Souza, K.L., de Jesus Beloti, L. et al. Use of photodynamic therapy and photobiomodulation as alternatives for microbial control on clinical and subclinical mastitis in sheep. Lasers Med Sci 37, 2305–2310 (2022). https://doi.org/10.1007/s10103-022-03506-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-022-03506-2