Abstract
The combination of multiple therapeutic and diagnostic functions is fast becoming a key feature in the area of clinical oncology. The advent of nanotechnology promises multifunctional nanoplatforms with the potential to deliver multiple therapeutics while providing diagnostic information simultaneously. In this study, novel iron oxide-gold core–shell hybrid nanocomposites (Fe3O4@Au HNCs) coated with alginate hydrogel carrying doxorubicin (DOX) were constructed for targeted photo-chemotherapy and magnetic resonance imaging (MRI). The magnetic core enables the HNCs to be detected through MRI and targeted towards the tumor using an external magnetic field, a method known as magnetic drug targeting (MDT). The Au shell could respond to light in the near-infrared (NIR) region, generating a localized heating for photothermal therapy (PTT) of the tumor. The cytotoxicity assay showed that the treatment of CT26 colon cancer cells with the DOX-loaded HNCs followed by laser irradiation induced a significantly higher cell death as opposed to PTT and chemotherapy alone. The in vivo MRI study proved MDT to be an effective strategy for targeting the HNCs to the tumor, thereby enhancing their intratumoral concentration. The antitumor study revealed that the HNCs can successfully combine chemotherapy and PTT, resulting in superior therapeutic outcome. Moreover, the use of MDT following the injection of HNCs caused a more extensive tumor shrinkage as compared to non-targeted group. Therefore, the as-prepared HNCs could be a promising nanoplatform for image-guided targeted combination therapy of cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent years have witnessed an emerging trend in cancer therapy to shift from monotherapy to combination therapy [1]. It has been widely reported that the antitumor activity of certain treatments could act synergistically as delivered simultaneously, leading to superior therapeutic outcome. Nanotechnology has attracted remarkable interest in the area of cancer combination therapy. The rational design and synthesis of nanomaterials with several functionalities could facilitate simultaneous delivery of multiple treatments to the tumor in order to achieve synergistic therapeutic effects [2,3,4,5]. On the other hand, there are specific nanomaterials that could be used as image contrast agents with the aim of improving tumor diagnosis, as well as image-guided cancer therapy [6,7,8,9]. Therefore, nanotechnology could offer a distinct advantage for simultaneous cancer diagnosis and therapy.
Photothermal therapy (PTT) using photo-responsive nanomaterials has gained increased attention in cancer research, with several clinical trials reported for the treatment of head and neck and lung tumors [10]. Unlike the conventional thermal therapy approaches, PTT using nanomaterials offers a site-specific treatment through generating localized heat within the tumor while minimizing the thermal damages to collateral tissues. Gold nanoparticles (AuNPs) are the mostly-reported nanomaterials for PTT by virtue of their high photothermal conversion efficiency, biocompatibility, and facile synthesis [11,12,13,14,15]. Given that the cytotoxic effect of many anticancer drugs is intensified at higher temperatures via different molecular mechanisms, many attempts have been made to exploit AuNPs for simultaneous drug delivery and PTT [16,17,18]. Accordingly, targeting drug-loaded AuNPs towards the tumor and subsequent laser irradiation can realize a synergistic photo-chemotherapy.
Iron oxide nanoparticles (Fe3O4 NPs) are one of the most widely used nanomaterials in biomedicine, offering a wide-range application from diagnosis to therapy. They are extensively employed as contrast agents in order to enhance the sensitivity of magnetic resonance imaging (MRI) [19, 20]. Furthermore, thanks to their magnetic properties, Fe3O4 NPs could enable a physical targeting approach, known as magnetic drug targeting (MDT) through which they are directed to the desired location under an external magnetic field [21, 22].
In this study, we developed Fe3O4@Au core–shell hybrid nanocomposites (HNCs) coated with alginate hydrogel carrying doxorubicin (DOX) for magnetic targeted photo-chemotherapy and MR imaging. Fe3O4@Au core–shell nanoparticles have been the subject of growing studies in recent years, as they provide theranostic function by enabling PTT and MR imaging. However, the use of the magnetic core of these hybrid nanoparticles for MDT could enhance the selectivity of their applications, which has received scant attention in the literature. Therefore, this study intends to take the full advantages of Fe3O4@Au HNCs for site-specific co-delivery of PTT and chemotherapy under MR imaging guidance. To this end, CT26 colorectal tumor-bearing mice are injected with the HNCs and thanks to their magnetic core they are targeted to the tumor via a magnet. The biodistribution of the HNCs is monitored via MRI to ensure their tumor localization. Next, the antitumoral activity of the treatment is assessed following the irradiation of mice with near-infrared (NIR) laser.
Materials and methods
Materials
Fetal bovine serum (FBS), Roswell Park Memorial Institute (RPMI) 1640 cell culture medium, trypsin-ethylene diamine tetra acetic acid (EDTA), and penicillin–streptomycin were prepared form Sigma-Aldrich (St. Louis, MO, USA) and used for cell culture. Iron (II) chloride tetrahydrate (> 99%), iron (III) chloride hexahydrate (> 99%), ammonia (32%), hydrochloric acid, nitric acid, 3-amino-propyltrimethoxysilane (APTMS, 97%), gold (III) chloride solution, sodium alginate ((NaC6H7O6)n), and doxorubicin hydrochloride were purchased from Merck Chemicals and reagents, India, and used for synthesizing the HNCs.
Synthesis and characterization of Fe3O4@Au-DOX HNCs
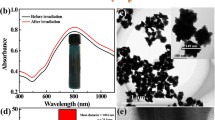
Fe3O4@Au HNCs were synthesized according to the method reported in our previous study [23]. Briefly, Fe3O4 NPs were prepared by the co-precipitation method of Massart through adding ammonia to the mixture solution of iron (II) and iron (III) (molar ratio: 1:2). The precipitated Fe3O4 NPs were washed with methanol and dispersed in toluene, followed by adding APTMS under sonication for 30 min to form APTMS-coated Fe3O4 NPs. To cover Fe3O4 NPs with a gold layer, AuNPs with diameter of ~ 3.5 nm were synthesized by Jana et al. method [24] and immobilized onto the surface of APTMS-coated Fe3O4 NPs. Next, 20 mL of sodium alginate solution (0.4%) was prepared followed by adding DOX (40 µg/mL) upon stirring for 15 min. Finally, the as-prepared Fe3O4@Au HNCs solution was added to the mixture of sodium alginate-DOX and the resulting solution was homogenized for 2 h at 35 °C to form Fe3O4@Au-DOX. Transmission electron microscopy (TEM, LEO 906, Zeiss, Germany) and dynamic light scattering (DLS, ZS-90, Malvern, UK) were conducted to determine the morphology and size of the particles. The DOX loading efficiency was calculated by the increased UV–Vis absorption at ~ 520 nm according to previous reports [18]. The photothermal effect of the HNCs was investigated by measuring the temperature changes of Fe3O4@Au solution at varying concentrations (5–50 µg/mL) under a 808-nm laser irradiation (808–nm NIR laser source, Nanobon, Iran) at 1.6 W/cm2 using an infrared thermal imaging camera (Testo 875–1i, Germany).
In vitro photo-chemotherapy
The murine colon adenocarcinoma cell line CT26 was obtained from Pasteur Institute of Iran. Cells were cultured in RPMI 1640 medium supplemented with 10% FBS, 100 units/mL penicillin, and 100 µg/mL streptomycin at 37 °C in 5% CO2. Firstly, the viability of CT26 cells treated with different agents including DOX and Fe3O4@Au with or without DOX loading was measured. Cells were seeded on 96-well plates at a density of 5 × 103 per well, and then incubated with varying concentrations of Fe3O4@Au (0–50 µg /mL per Au), DOX (0–2 µg/mL), and Fe3O4@Au-DOX (0–50 µg/mL per Au, 0–2 µg/mL per DOX). After incubation for 4 h, cells were washed three times with PBS and the cell viability was measured using 3,[4,5-dimethylthiazol-2- yl]-2,5-diphenyl-tetrazolium bromide (MTT) assay. To investigate the effect of PTT and photo-chemotherapy, cells pretreated with Fe3O4@Au and Fe3O4@Au-DOX were exposed with NIR laser at 1.6 W/cm2 for 5 min and examined by MTT assay.
Tumor induction
Male Balb/c mice (5–8 weeks old, 20–25 g) were obtained from Pasteur Institute of Iran. Following three passages, cells were counted and resuspended in medium solution and injected subcutaneously on the right flank of mice at a density of 2 × 106 cells per mice. All animal experiments were conducted in accordance with guidelines established by institutional animal Care Committee. Tumor-bearing mice were used in subsequent experiments as the tumor size reached ~ 100 mm3.
MRI study
Firstly, the ability of Fe3O4@Au as MRI contrast agent was assessed through T2 relaxivity measurement. A series dilution of Fe3O4@Au solution (0.025, 0.05, 0.1, 0.2, 0.5, 1 mM per Fe) were prepared and imaged using a clinical MRI scanner (1.5 T, Magnetom Avanto, Siemens, Germany) with the following acquisition parameters: repetition time (TR) = 2000 ms; echo time (TE) = 12–168 ms with 12 ms increments; slice thickness = 1 mm; matrix size = 256 × 256; field of view (FOV) = 20 × 10 cm. Next, the transverse relaxivity (r2) was measured through linear fitting of the T2 relaxation rate (1/T2) versus Fe concentration. For in vivo imaging, tumor-bearing mice were intravenously (i.v.) injected with Fe3O4@Au (5 Fe mg/kg) and scanned using a 1.5 T MRI with the following parameters: TE = 66 ms, TR = 2000 ms, slice thickness = 1 mm, matrix size = 256 × 256, and FOV = 12 × 12 cm.
In vivo photo-chemotherapy
CT26 tumor-bearing mice were randomly divided into seven groups (n = 5 each): control (untreated), NIR irradiation, DOX (5 mg/kg), Fe3O4@Au-DOX (5 mg/kg per DOX, 10 mg/kg per Au), Fe3O4@Au-DOX + NIR, Fe3O4@Au-DOX + MDT, Fe3O4@Au-DOX + MDT + NIR. For non-targeted group, NIR irradiation was performed 24 h post i.v. injection using a continuous-wave 808-nm NIR laser at the power density of 1.2 W/cm2 for 15 min. For MDT-targeted group, a magnet with a magnetic field strength of 0.4 T was placed on the tumor immediately after i.v. injection for 4 h to accumulate the magnetic particles inside the tumor. The mice were subjected to NIR irradiation with the same exposure condition and the temperature elevation of the tumor was also monitored during NIR irradiation using a thermal camera. The mice were treated in one treatment session. The antitumor effect of various treatments was assessed through measuring the tumor growth rate during 18 days of follow-up period. Furthermore, the histological changes of tumor tissue were also studied using hematoxylin and eosin (H&E) staining. To this end, tumors were extracted after three days post-treatments, fixed in 10% neutral buffered formalin, embedded in paraffin, cut into 5-mm sections, stained with H&E, and observed under a microscope.
Statistical analysis
For statistical analysis, one-way ANOVA was performed using SPSS (version 11; SPSS Inc., Chicago, IL). All data are expressed as the mean ± standard deviation (SD). A value of p < 0.05 was considered to be statistically significant.
Results
Characterization of Fe3O4@Au-DOX HNCs
The morphology of Fe3O4@Au-DOX HNCs was characterized by TEM. As shown in Fig. 1a, the as-prepared HNCs have a core–shell structure with the average diameter of 30.5 nm, including the gold layer of ~ 7.4 nm thick that uniformly covers the magnetic core of 15.7 nm in diameter. The hydrodynamic diameter of the HNCs measured by DLS shows the size distribution of the HNCs ranging from 10 to 60 nm, with the maximum frequency at 20–30 nm (Fig. 1b). The loading content of DOX reached up to 9.8% by varying the concentrations of Fe3O4@Au and DOX. The photothermal performance of the HNCs was also investigated by exposing varying concentrations of the HNCs upon NIR laser (Fig. 1c). The HNCs displayed a remarkable heat generation capability with a clearly concentration-dependent manner. While the temperature of water as control increased by only 1.8 °C after a 5-min laser irradiation, the HNCs solutions with concentrations of 5, 10, 25, and 50 µg/mL exhibited significantly higher temperature rises of 3.7, 5.6, 11.2, and 17 °C, respectively, under the same NIR exposure condition.
In vitro photo-chemotherapy
Firstly, the viability of CT26 cells treated with Fe3O4@Au without DOX loading was investigated to ensure the safety of the blank HNCs as nanovehicles for drug delivery. As shown in Fig. 2a, a slight decrease in cell viability can be noted by increasing the concertation of Fe3O4@Au where the highest tested concentration of 50 µg/ml reduced the cell viability to 86.5%, certifying the biocompatibility of the HNCs. To draw a comparison between the chemotherapeutic effect of free DOX and DOX-loaded HNCs, the viability of CT26 cells treated with DOX and Fe3O4@Au-DOX was measured, as shown in Fig. 2b. Under the equivalent drug concentration, DOX-treated cells indicated a significantly higher cell death as compared to those treated with Fe3O4@Au-DOX. For example, the treatment of cells with Fe3O4@Au-DOX at drug concertation of 0.5 µg/mL reduced the cell viability to 85%, whereas free DOX induced a markedly greater cell death, lowering the cell viability to 47%. Next, the effect of NIR irradiation was investigated on cells pretreated with Fe3O4@Au and Fe3O4@Au-DOX. As shown in Fig. 2c, NIR irradiation alone for 5 min at 1.6 W/cm2 did not affect the cell viability significantly. However, the treatment of cells with Fe3O4@Au and Fe3O4@Au-DOX followed by NIR irradiation caused a dramatic reduction in the cell viability. Apparently, the group receiving photo-chemotherapy (Fe3O4@Au-DOX + NIR) showed a notably lower cell viability compared to the cells treated with Fe3O4@Au + NIR as PTT alone group. For example, the viability of cells treated with PTT and photo-chemotherapy at the same Au concentration of 30 µg/mL was 58 and 37%, respectively, indicating that the HNCs are able to effectively integrate PTT and drug delivery in order to achieve a superior anticancer effect.
a The viability of CT26 cells incubated with Fe3O4@Au at varying Au concentrations for 4 h. b The viability of CT26 cells incubated with DOX and Fe3O4@Au-DOX at varying DOX concentrations for 4 h. The viability of CT26 cells after 4 h incubation with Fe3O4@Au and Fe3O4@Au-DOX followed by NIR irradiation
MRI study
As shown in Fig. 3a, MR imaging of the HNCs solutions displayed a dose-dependent negative contrast enhancement, and the T2 relaxivity was calculated to be 47.53 mM−1S−1. The tumor uptake of the HNCs was also explored after i.v. injection with or without MDT. It can be clearly visualized from the T2-weighted MR images of mice that the injection of the HNCs notably enhanced the T2 MR signal intensity compared to non-injected mice (Fig. 3b). Interestingly, MDT-targeted group showed enhanced T2 contrast in the tumor region in comparison to non-targeted group, indicating the benefit of using MDT to increase the tumor accumulation of the HNCs.
In vivo photo-chemotherapy
The antitumor effect of various treatment formulations was evaluated on CT26 tumor-bearing mice. Firstly, the superficial temperature of tumor in mice with or without injection of the HNCs was monitored using a thermal camera. As shown in Fig. 4, NIR irradiation alone for 15 min at 1.2 W/cm2 increased the tumor temperature by 3.9 °C to 40.4 °C, whereas mice pretreated with the HNCs showed a significantly higher temperature rise under the same laser exposure condition. More importantly, MDT-targeted group in which a magnet was used to target the HNCs towards the tumor reached a substantially higher average temperature of 46.8 °C as compared to 43.6 °C for non-targeted group. Figure 5a shows the tumor volume changes in mice receiving various treatments over 18 days follow-up period. The mice treated with NIR irradiation alone and free DOX indicated a comparable tumor growth rate with untreated control group. While the injection of Fe3O4@Au-DOX caused a slight tumor growth inhibition (TGI = (1-V/V0) × 100) rate of 31.3%, the use of MDT improved the chemotherapy efficiency, resulting in the TGI of 46.2%. The non-targeted photo-chemotherapy group (Fe3O4@Au-DOX + NIR) showed a dramatic reduction in tumor growth, with the TGI rate of 67.1%. Similarly, the addition of MDT markedly enhanced the antitumor function of photo-chemotherapy and resulted in massive tumor shrinkage, showing the TGI rate of 85.2%.
To ensure that the treatments are safe with minimal systemic toxicity, the body weight changes of animals were monitored during the treatment period (Fig. 5b). Except free DOX-treated mice that experienced a loss in body weight within several days post-injection, other treatment groups showed no significant reduction in body weight, proving that the treatments can be well-tolerated by animals. To further assess the antitumor function of the treatments, tumor specimens were collected 3 days post-treatments and prepared for H&E staining. It is apparent from Fig. 5c that DOX treatment caused no obvious damage to tumor cells as evident by the normal cell density, whereas photo-chemotherapy induced an extensive damage to tumor cells which can be noted from reduced tumor cell density. Consistent with the tumor growth study, MDT-targeted photo-chemotherapy yielded a stronger antitumor efficiency as compared to non-targeted group.
Discussion
Given the fact that heat can intensify the cytotoxic effects of anticancer drugs through different mechanisms, a considerable amount of pre-clinical and clinical efforts have been made to combine thermal therapy and chemotherapy [25, 26]. Mild hyperthermia at 39–43 °C has been found to weaken the junctional integrity of endothelia cells, which in turn increases the permeability of tumor vasculature, thus enhancing the tumor uptake of drugs [27]. At the cellular level, heat can also increase the intracellular uptake of drugs through permeabilizing the cell membrane [28]. Furthermore, compelling evidences have been found the beneficial effect of heat to overcome multidrug resistance (MDR) which is the main reason of chemotherapy failure. In this regard, a report by Wang et al. revealed that PTT using silica-coated gold nanorods can suppress the P-gp as the primary MDR transmembrane protein that actively pumps the drugs out of the cell, thereby inhibiting the drug resistance pathway [29]. Despite these remarkable benefits, the simultaneous delivery of heat and drug to achieve maximal synergistic outcome is not completely feasible in clinical practice. The advent of nanotechnology promises multifunctional nanoplatforms that can enable co-delivery of heat and drug with high selectivity to the tumor site for superior therapeutic outcome.
In this study, we designed a core–shell Fe3O4@Au HNCs carrying DOX for combined photo-chemotherapy under NIR laser irradiation. The magnetic core of the HNCs served for two purposes, (I) targeted delivery of the HNCs towards the tumor under an external magnetic field knowns as MDT and (II) tracing the biodistribution of the HNCs through MRI. Thanks to the well-known effect of surface plasmon resonance (SPR), the Au shell could respond to laser light and generate a localized heat for photothermal ablation of tumor cells. Compared to Au nanospheres that absorb light in the visible region, the Au shell displays a red-shift in the SPR band, giving the advantage of light absorbance in the NIR region where light has the maximum tissue penetration depth [30]. The as-prepared HNCs was also modified with alginate hydrogel as a natural polysaccharide to serve as drug loading matrix. It has been found that alginate can improve the biocompatibility, circulation half-life and stability of nanoparticles, and enhance the aqueous solubility of drugs [31,32,33].
A dramatic rise in the temperature of the HNCs solution versus concertation under NIR irradiation demonstrated the efficient photothermal conversion ability of the particles. In vivo PTT operation also noted an obvious temperature enhancement in mice treated with the HNCs as compared to NIR irradiation alone, further proving the photothermal effect of the HNCs. A significant part of this study is that it explores the effect of MDT to improve site-specific delivery of the treatments by taking the advantages of rationally designed nanoplatforms equipped with magnetic particles. MRI study revealed that MDT can successfully elevate the accumulation of the HNCs inside the tumor. In vivo thermometry results also certified that the tumor in MDT-targeted group experienced higher temperature rises during NIR irradiation due to enhanced tumor accumulation of the HNCs. Finally, the antitumor study indicated that the injection of the HNCs followed by MDT caused notably stronger tumor suppression as compared to non-targeted group, further corroborating that MDT is an effective strategy to enhance treatment selectivity and efficiency.
Conclusion
The objective of this study was to provide a representative on how nanomaterials could be designed to offer multiple functionalities including therapy, diagnosis, and targeting at the same time. To this end, we developed a theranostic nanocomposite consisting of Fe3O4 NPs and AuNPs that could integrate PTT and drug delivery, MR imaging, and MDT. Taken together, the findings of this study highlight the various beneficial roles of nanotechnology and encourage further studies to take its full advantages to combat cancer.
References
Beik J, Khateri M, Khosravi Z, Kamrava SK, Kooranifar S, Ghaznavi H, Shakeri-Zadeh A (2019) Gold nanoparticles in combinatorial cancer therapy strategies. Coord Chem Rev 387:299–324
Mirrahimi M, Beik J, Mirrahimi M, Alamzadeh Z, Teymouri S, Mahabadi VP, Eslahi N, Tazehmahalleh FE, Ghaznavi H, Shakeri-Zadeh A (2020) Triple combination of heat, drug and radiation using alginate hydrogel co-loaded with gold nanoparticles and cisplatin for locally synergistic cancer therapy. Int J Biol Macromol 158:617–626
Tian G, Zhang X, Gu Z, Zhao Y (2015) Recent advances in upconversion nanoparticles-based multifunctional nanocomposites for combined cancer therapy. Adv Mater 27:7692–7712
He C, Lu J, Lin W (2015) Hybrid nanoparticles for combination therapy of cancer. J Control Release 219:224–236
Beik J, Shiran MB, Abed Z, Shiri I, Ghadimi-Daresajini A, Farkhondeh F, Ghaznavi H, Shakeri-Zadeh A (2018) Gold nanoparticle-induced sonosensitization enhances the antitumor activity of ultrasound in colon tumor-bearing mice. Med Phys 45:4306–4314
Beik J, Alamzadeh Z, Mirrahimi M, Sarikhani A, Ardakani TS, Asadi M, Irajirad R, Mirrahimi M, Mahabadi VP, Eslahi N (2021) Multifunctional theranostic graphene oxide nanoflakes as MR imaging agents with enhanced photothermal and radiosensitizing properties. ACS Appl Bio Mater 4:4280–4291
Asadi M, Beik J, Hashemian R, Laurent S, Farashahi A, Mobini M, Ghaznavi H, Shakeri-Zadeh A (2019) MRI-based numerical modeling strategy for simulation and treatment planning of nanoparticle-assisted photothermal therapy. Physica Med 66:124–132
Khademi S, Sarkar S, Kharrazi S, Amini SM, Shakeri-Zadeh A, Ay MR, Ghadiri H (2018) Evaluation of size, morphology, concentration, and surface effect of gold nanoparticles on X-ray attenuation in computed tomography. Physica Med 45:127–133
Keshavarz M, Moloudi K, Paydar R, Abed Z, Beik J, Ghaznavi H, Shakeri-Zadeh A (2018) Alginate hydrogel co-loaded with cisplatin and gold nanoparticles for computed tomography image-guided chemotherapy. J Biomater Appl 33:161–169
Beik J, Abed Z, Ghoreishi FS, Hosseini-Nami S, Mehrzadi S, Shakeri-Zadeh A, Kamrava SK (2016) Nanotechnology in hyperthermia cancer therapy: from fundamental principles to advanced applications. J Control Release 235:205–221
Beik J, Asadi M, Mirrahimi M, Abed Z, Farashahi A, Hashemian R, Ghaznavi H, Shakeri-Zadeh A (2019) An image-based computational modeling approach for prediction of temperature distribution during photothermal therapy. Appl Phys B 125:1–13
Beik J, Khademi S, Attaran N, Sarkar S, Shakeri-Zadeh A, Ghaznavi H, Ghadiri H (2017) A nanotechnology-based strategy to increase the efficiency of cancer diagnosis and therapy: folate-conjugated gold nanoparticles. Curr Med Chem 24:4399–4416
Hashemian AR, Eshghi H, Mansoori GA, Shakeri-Zadeh A, Mehdizadeh AR (2009) Folate-conjugated gold nanoparticles (synthesis, characterization and design for cancer cells nanotechnology-based targeting). Int J Nanosci Nanotechnol 5(1):25–34
Shakeri-Zadeh A, Eshghi H, Mansoori GA, Hashemian AR (2009) Gold nanoparticles conjugated with folic acid using mercaptohexanol as the linker. Journal Nanotechnology Progress International 1
Movahedi MM, Mehdizadeh A, Koosha F, Eslahi N, Mahabadi VP, Ghaznavi H, Shakeri-Zadeh A (2018) Investigating the photo-thermo-radiosensitization effects of folate-conjugated gold nanorods on KB nasopharyngeal carcinoma cells. Photodiagnosis Photodyn Ther 24:324–331
Alamzadeh Z, Beik J, Mirrahimi M, Shakeri-Zadeh A, Ebrahimi F, Komeili A, Ghalandari B, Ghaznavi H, Kamrava SK, Moustakis C (2020) Gold nanoparticles promote a multimodal synergistic cancer therapy strategy by co-delivery of thermo-chemo-radio therapy. European Journal of Pharmaceutical Sciences 145:105235
Mirrahimi M, Abed Z, Beik J, Shiri I, Dezfuli AS, Mahabadi VP, Kamrava SK, Ghaznavi H, Shakeri-Zadeh A (2019) A thermo-responsive alginate nanogel platform co-loaded with gold nanoparticles and cisplatin for combined cancer chemo-photothermal therapy. Pharmacol Res 143:178–185
Liu J, Detrembleur C, De Pauw-Gillet MC, Mornet S, Jérôme C, Duguet E (2015) Gold nanorods coated with mesoporous silica shell as drug delivery system for remote near infrared light-activated release and potential phototherapy. Small 11:2323–2332
Li L, Jiang W, Luo K, Song H, Lan F, Wu Y, Gu Z (2013) Superparamagnetic iron oxide nanoparticles as MRI contrast agents for non-invasive stem cell labeling and tracking. Theranostics 3:595
Gao Z, Ma T, Zhao E, Docter D, Yang W, Stauber RH, Gao M (2016) Small is smarter: nano MRI contrast agents–advantages and recent achievements. Small 12:556–576
Price PM, Mahmoud WE, Al-Ghamdi AA, Bronstein LM (2018) Magnetic drug delivery: where the field is going. Front Chem 6:619
Liu Y-L, Chen D, Shang P, Yin D-C (2019) A review of magnet systems for targeted drug delivery. J Control Release 302:90–104
Safari A, Sarikhani A, Shahbazi-Gahrouei D, Alamzadeh Z, Beik J, Dezfuli AS, Mahabadi VP, Tohfeh M, Shakeri-Zadeh A (2020) Optimal scheduling of the nanoparticle-mediated cancer photo-thermo-radiotherapy. Photodiagnosis and Photodynamic Therapy 32:102061
Jana NR, Gearheart L, Murphy CJ (2001) Seeding growth for size control of 5–40 nm diameter gold nanoparticles. Langmuir 17:6782–6786
van der Zee J (2002) Heating the patient: a promising approach? Ann Oncol 13:1173–1184
Hildebrandt B, Wust P, Ahlers O, Dieing A, Sreenivasa G, Kerner T, Felix R, Riess H (2002) The cellular and molecular basis of hyperthermia. Crit Rev Oncol Hematol 43:33–56
Huilgol N (2019) Hyperthermic oncology from bench to bedside. Journal of Radiation and Cancer Research 10:186–186
Hettinga JVE, Konings AWT, Kampinga HH (1997) Reduction of cellular cisplatin resistance by hyperthermia—a review. Int J Hyperth 13:439–457
Wang L, Lin X, Wang J, Hu Z, Ji Y, Hou S, Zhao Y, Wu X, Chen C (2014) Novel Insights into combating cancer chemotherapy resistance using a plasmonic nanocarrier: enhancing drug sensitiveness and accumulation simultaneously with localized mild photothermal stimulus of femtosecond pulsed laser. Adv Func Mater 24:4229–4239
Beik J, Asadi M, Khoei S, Laurent S, Abed Z, Mirrahimi M, Farashahi A, Hashemian R, Ghaznavi H, Shakeri-Zadeh A (2019) Simulation-guided photothermal therapy using MRI-traceable iron oxide-gold nanoparticle. Journal of Photochemistry and Photobiology B: Biology 199:111599
Almalik A, Alradwan I, Kalam MA, Alshamsan A (2017) Effect of cryoprotection on particle size stability and preservation of chitosan nanoparticles with and without hyaluronate or alginate coating. Saudi pharmaceutical journal 25:861–867
Feng W, Nie W, He C, Zhou X, Chen L, Qiu K, Wang W, Yin Z (2014) Effect of pH-Responsive alginate/chitosan multilayers coating on delivery efficiency, cellular uptake and biodistribution of mesoporous silica nanoparticles based nanocarriers. ACS Appl Mater Interfaces 6:8447–8460
Mirrahimi M, Khateri M, Beik J, Ghoreishi FS, Dezfuli AS, Ghaznavi H, Shakeri-Zadeh A (2019) Enhancement of chemoradiation by co-incorporation of gold nanoparticles and cisplatin into alginate hydrogel, Journal of Biomedical Materials Research Part B: Applied. Biomaterials 107:2658–2663
Funding
This work was supported by the National Institute for Medical Research Development Grant No.971962 and Iran University of Medical Sciences Grant No. 16669.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khani, T., Alamzadeh, Z., Sarikhani, A. et al. Fe3O4@Au core–shell hybrid nanocomposite for MRI-guided magnetic targeted photo-chemotherapy. Lasers Med Sci 37, 2387–2395 (2022). https://doi.org/10.1007/s10103-021-03486-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-021-03486-9