Abstract
This retrospective case-control study aimed to compare 30 versus 40 W power of CO2 laser for the therapy of genitourinary syndrome of menopause (GSM). Postmenopausal women with severe intensity of dyspareunia and dryness were eligible to be included in this study. Primary outcomes were dyspareunia and dryness. Secondary outcomes were itching/burning, dysuria, frequency and urgency, Female Sexual Function Index (FSFI), vaginal maturation value (VMV), and Vaginal Health Index Score (VHIS). One laser therapy was applied every month for 3 months. Outcomes were evaluated at baseline and 1 month following the 3rd therapy. Fifty (25 per group) women were included in this study. In the 30-W group, mean improvement of dyspareunia, dryness, itching/burning, FSFI, VMV, and VHIS was 6.1 ± 1.7, 6.0 ± 1.9, 5.9 ± 2.0, 16.6 ± 6.7, 29.9 ± 13.0, and 11.0 ± 2.9, respectively (within group comparisons all p < 0.001). In the 40-W group, mean improvement of dyspareunia, dryness, itching/burning, FSFI, VMV, and VHIS was 6.1 ± 1.7, 6.5 ± 2.0, 5.2 ± 2.5, 14.8 ± 7.1, 25.0 ± 13.4, and 10.5 ± 4.1, respectively (within-group comparisons, all p ≤ 0.001). Comparison between 30 and 40 W revealed that mean improvement or presence of all GSM symptoms and clinical signs was not statistically significant different. CO2 laser therapy may improve GSM symptoms and clinical signs. This improvement did not seem to associate to power of 30 or 40 W.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Genitourinary syndrome of menopause (GSM) is a new term for vulvovaginal atrophy (VVA), an old condition occurring at menopause due to low levels of estrogen [1, 2]. However, GSM defines better than VVA all the possible symptoms and clinical signs from the lower genital (VVA) and urinary tract system (LUTS) during menopause [1]. Thus, women with GSM may present with one or more symptoms such as dyspareunia, dryness, itching/burning, sexual dysfunction, dysuria, urinary frequency, and urgency [1].
Recently, microablative fractional CO2 laser (CO2 laser) (SmartXide2 V2LR, Monalisa Touch, DEKA, Florence, Italy) administered intravaginally has been proposed for the management of GSM [3,4,5]. This type of laser has a wavelength of 10,600 nm that allows a superficial microablative effect in soft tissues and a pulsed beam that protects the tissues from possible overheating damage. The laser beam is produced in a fractional manner, creating small spots (called DOTs) alternating parts of tissue treated and not treated [6]. The size of each DOT is set by the manufacturer at 200 μm. Moreover, it has a DEKA pulse (D-pulse) mode that consists of two parts: (a) constant, high energy peak power, for rapid superficial evaporation of the atrophic epithelium with low water content and (b) lower peak power with longer emission times that allows the energy heat to penetrate deeper in the epithelium [6]. This D-pulse mode combined with DOTs remodels the connective tissue via the production of heat shock protein 47 and produces new collagen/fibroblasts and ground matrix. Power (range 0.5-60 W), dwell time (range 100–1000 μs), and spacing between DOTS (range 100–1000 μm) that define the quantity of energy; SmartStak parameter (range 1–5) that define the diffused energy inside the tissue; and D-pulse mode are applicable to be selected from the machine software [6].
CO2 laser therapy may significantly improve symptoms and clinical signs of GSM, as indicated by the current literature [7,8,9,10,11,12,13,14,15,16,17]. However, the therapeutic protocols of the available studies did not use the same power. Seven studies used power of 30 W [7,8,9,10, 12, 14, 17], whereas four used 40 W [11, 13, 15, 16]. Even though CO2 laser efficacy seems to be promising with either power in all studies consistently, a comparison of the two levels of power have not been evaluated yet.
The aim of the current study was to assess whether the power of the CO2 laser results in differences of treatment efficacy. In particular, we assessed objective and subjective measurements of postmenopausal women with severe symptoms of GSM when the 30- or 40-W protocols were applied. We compared these results on the basis to detect potential outcome alterations between the two groups.
Material and methods
This study is a retrospective case-control study with prospectively collected data, conducted in the urogynecological outpatient clinic of a tertiary hospital. Specifically, data was derived from two prospective studies, using intravaginal CO2 laser (SmartXide2 V2LR, Monalisa Touch, DEKA, Florence, Italy) for the management of postmenopausal women with GSM. These studies had the same inclusion-exclusion criteria, outcome assessments, and procedures of CO2 laser. However, the applied power in the vaginal canal was different (30 or 40 W). Approval was obtained from the Institutional Research Ethics Committee for both studies, and all participants had signed informed consents forms. All procedures were performed according to the ethical standards of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Eligibility criteria for inclusion in the present study involved postmenopausal women with severe intensity of dyspareunia and vaginal dryness. Cases where sexual activity was ceased for reasons different than severity of GSM symptoms or when dyspareunia and dryness were rated as absent or mild or moderate were not considered for the current analysis.
Three CO2 laser therapies were applied at monthly intervals. The settings and procedures of CO2 laser and the methodology of outcome assessments have been previously described [9, 15, 16]. The use of 30 or 40 W power defined the compared groups (30- and 40-W groups, respectively). All other laser settings (i.e., dwell time (1000 μs), smart stack parameter (from 1 to 3), emission mode (D-pulse), spacing (1000 μm), density, and fluence were the same for both groups.
Dyspareunia and dryness were considered primary outcomes. All other GSM symptoms (i.e., itching/burning, dysuria, urinary frequency, and urgency), sexual function, and assessments of clinical findings were considered secondary ones. All outcomes were evaluated at baseline (before the initiation of laser therapy) and 1 month following the 3rd laser therapy.
Dyspareunia, dryness, and itching/burning were assessed using a 10-cm Visual Analogue Scale (VAS 0–10). Zero defined absence of symptoms, rates of >0 and <4 mild symptom intensity, ≥4 and <8 moderate intensity, and ≥8 severe intensity.
Sexual function was evaluated by the Female Sexual Function Index (FSFI) [18, 19]. The FSFI evaluates desire, arousal, lubrication, orgasm, satisfaction, and pain, as separate domains [19]. A combination of these domains produces a total score with a minimum value of 2 and a maximum of 36 [19]. Increase of scores defines improvement of sexual function, while a threshold of 26.55 of the total FSFI score differentiates women with and without sexual dysfunction [18].
Dysuria, urinary frequency at daytime, nocturia, and urgency were assessed by the International Consultation of Incontinence Questionnaire-Female Lower Urinary Tract Symptoms (ICIQ-FLUTS) [20]. Answers different than “1–6” or “7–8”in question 5 of ICIQ-FLUTS (Filling domain) defined the presence of abnormal urinary frequency [20,21,22]. Answers different than “0” or “1” in question 2 of ICIQ-FLUTS (Filling domain) defined the presence of nocturia [20,21,22].
Clinical findings were evaluated using the Vaginal Maturation Value (VMV) and Vaginal Health Index Score (VHIS) [23]. VMV is calculated by the formula (1 × %superficial) + (0.5 × %intermediate) + (0 × %parabasal) [23], whereas the threshold of 40 distinguishes atrophic from non-atrophic vaginal smears [25]. VHIS includes five components (elasticity, fluid volume, pH, and epithelial integrity) whereas each one of these could receive values from 1 (worst) to 5 (best) [23]. A score of 15 or lower defines vaginal atrophy [23].
Statistical analysis
Power calculation was performed for the mean improvement of primary outcomes using data from two previously published studies [8, 15]. Twenty-five participants per group were required for 80% power of study, 5% level of significance, and 20% margin of error for a non-inferiority trial. Hence, 30-W power would not be inferior to 40 W if a minimum clinically important difference (MCID) of 2 cm between groups would not be observed. Statistical analyses were performed on the basis of within- and between-group comparisons. For continuous variables, Wilcoxon signed-rank test for related paired samples and t test for independent samples were used for within- and between-group comparisons, respectively, as appropriate. For categorical variables, Fisher’s exact test (for values <5) or chi-square was used for within- and between-group comparisons. Adjustment for all possible confounding factors (i.e., age, years since last period, body mass index (BMI), smoking, GSM symptoms, total FSFI score, VMV, and VHIS at baseline) was performed using ANCOVA or logistic regression (binary or multinomial) when the dependent variable was continuous or categorical (with two or more levels), respectively. Continuous variables are presented as mean ± SD or median/interquartile range (median/IQR) when normally or abnormally distributed, respectively. Categorical variables are presented as percentages (%). Analyses were performed using the SPSS statistical software.
Results
Twenty-five participants per group were randomly selected by a computer, from the preexisting databases. Baseline characteristics of the two groups are presented in Table 1. Statistically significant differences between the baseline characteristics of the two groups were not detected. Twelve of the 40-W group participants have been included in the analyses of a previously published study [16].
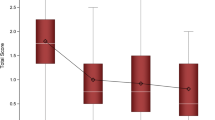
Mean improvement of continuous variables for both groups are presented in Table 2. In within-group comparison, statistically significant improvement of dyspareunia, dryness, itching/burning, FSFI, VHIS, and VMV was observed for both powers. In between-group comparison, improvement of these outcomes was not statistically significantly different. Adjustment for possible confounding factors did not change the results. The MCID of 20% between the two levels of power, as selected for this study, was not surpassed in any of these outcomes.
The changes of categorical variables are presented in Table 3. The observed alteration of the presence of dyspareunia, dryness, itching/burning, dysuria, frequency, urgency, sexual dysfunction, and atrophic values of clinical findings at baseline and 1 month following the 3rd therapy was not statistically significant different between the two groups. Adjustment for possible confounding factors did not change the results. In both groups, all participants at baseline had severe dyspareunia, dryness, and sexual dysfunction. One month following the 3rd therapy, severe dyspareunia disappeared in all participants of both groups, while normal sexual function was resumed in 36% of the participants in both groups. One month following the 3rd therapy, severe dryness disappeared in 96 or 100% of the participants in the 30- or 40-W group, respectively.
Adverse events in both groups included a related to the laser-application irritation-burning sensation of mild intensity at the introitus. The sensation started immediately after the laser application, lasted for approximately 2 h, and resolved spontaneously. Serious adverse events were not present in any of the participants of either group. Vaginal infections of any kind or worsening of symptoms was not found in any of the participants.
Discussion
The results of this study confirmed previous published data, regarding the statistically significant improvement of GSM symptoms and clinical signs after three CO2 laser therapies. This improvement did not seem to associate to the level of 30- or 40-W power. The MCID of 20% difference in mean improvement of outcomes was not exceeded in the comparison of 30 versus 40 W. Moreover, the presence of GSM symptoms and atrophic values of clinical findings appeared to change similarly for both powers.
Power is one of the three parameters of the CO2 laser that determines the quantity of the heat penetrating in the vaginal mucosa, aiming to stimulate tissue rejuvenation. The other two parameters are dwell time and spacing. The 30-W level of power, with a given dwell time of 1000 μs and spacing of 1000 μm, have been evaluated in two histopathological studies, an ex vivo [24] and an in vivo [8]. The ex vivo indicated that these parameters in combination to the SmartStak parameter 3 had the more pronounced ablative effect with an additional presence of activated fibroblasts [24]. The in vivo study showed a thicker vaginal epithelium and increase of glycogen, epithelial exfoliation, extracellular matrix components, and blood vessels in the connective tissue [8]. Regarding the 40-W power, published histopathological data are not available in any peer-reviewed journal. The non-statistically different results of this study, between the 30 and 40 W of energy power in symptom severity and clinical findings (VMV and VHIS), indicated that 40 W probably produces a similar tissue effect. Therefore, a difference of 10 W between the two levels of power, under the same dwell time and spacing, may not contribute to a different laser effect.
In dermatology, even though the CO2 laser settings allow power use of 10–30 W, the energy power usually used is 10–20 W [25]. The concept of this level of power lies in the lower intensity and duration of adverse events [25]. The latter appears not to apply for the vaginal mucosa. In our study, neither 30 nor 40 W had different adverse events. The only potential adverse event that occurred was a mild irritation-burning sensation at the introitus, with an approximate duration of 2 h. In another study using 30 W, a mild or moderate pain lasting 2–3 days has been reported [14]. In other studies, using either 30 or 40 W power, adverse events did not occur in any of the participants [9, 11, 13].
Furthermore, the observed statistically significant mean improvement of dyspareunia, dryness, and FSFI in within-group comparison, is similar to the results of previous studies for either powers [7, 9,10,11,12,13,14, 16, 17]. These studies [7, 9,10,11,12,13,14, 16, 17] had not restricted inclusion criteria, while our study was designed to include solitary severe cases of dyspareunia and dryness. The inclusion of only severe cases could further explain the low percentage of participants (8%) with absence of symptoms following three laser therapies, which was found in this study in either power. Another study, including participants with moderate to severe intensity of symptoms, reported a symptom-free rate of 34% [16]. However, a MCID of 20% of symptom severity was observed in 98% (49/50) of the participants. Furthermore, 36% of participants in both groups resumed normal sexual function, despite the smaller proportion of dyspareunia disappearance. The latter effect likely indicates a positive impact of laser therapy in women’s quality of life, as GSM symptoms mostly interfere with sexual satisfaction, sexual spontaneity, intimacy, and relationship [26,27,28].
A further potential positive impact of laser therapy in women’s quality of life is implied by the observed ameliorate of LUTS in both powers. Although dyspareunia and dryness are the most common and bothersome GSM symptoms [29,30,31,32], presence of urgency and/or frequency at daytime >8 times and/or nocturia more than 1 time has been also related to negatively impaired quality of life [21, 22]. The urinary urge intensity has the greatest association with decreased health-related quality of life and increased symptom bothering [21]. In our study, presence of urgency decreased from 80 or 56% to 36 or 24% in the 30- or 40-W group, respectively.
Alternative medical approaches for the management of GSM symptoms, such as local estrogens, have improvement rates up to 90%, depending on symptoms and estrogen type [33,34,35,36,37,38]. Moreover, symptom-free rates for VVA symptoms and LUTS have been estimated to be 14–82% [35, 37, 39] and 27–70% [35, 36], respectively. However, safety issues with regards to the long-term use makes necessary the finding of new therapeutic strategies (i.e., laser therapy). For laser therapy at other wavelengths than CO2, like the Erbium laser, improvement or success rates are not available in the current literature.
A possible limitation of this study is its retrospective design. However, data were prospectively collected, sample size calculation was performed, and participants were randomly selected by a computer. Another limitation could be the relevant small sample size as calculated by a margin of error at 20%. The larger sample size could possibly result in the detection of potential differences. However, there is lack of data of MCID regarding dyspareunia, dryness, and sexual function of postmenopausal women with GSM. A margin of error at 20% was regarded acceptable by all authors. Additionally, this study has a relatively short follow-up period. Hence, a comparison of the long-term efficacy of 30 or 40 W could not be performed.
Conclusion
CO2 laser therapy intravaginal administered may provide a valid alternative therapeutic option for the management of GSM. Three laser therapies may result in statistically significant improvement of sexual function, GSM symptoms, and clinical signs of postmenopausal women. The level of power did not seem to affect the CO2 laser effectiveness and safety. Prospective randomized controlled trials with long-term follow-up period and a more systematic variation of parameters on a larger group of patients are needed.
References
Portman DJ, Gass MLS, on behalf of the Vulvovaginal Atrophy Terminology Consensus Conference Panel (2014) Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and The North American Menopause Society. Menopause 21:1063–1068
Ward K, Deneris A (2016) Genitourinary syndrome of menopause: a new name for an old condition. Nurse Pract 41:28–33
Palacios S, Castelo-Branco C, Currie H, Mijatovic V, Nappi RE, Simon J, Rees M (2015) Update on management of genitourinary syndrome of menopause: a practical guide. Maturitas 82:308–313
Stefano S, Stavros A, Massimo C (2015) The use of pulsed CO2 lasers for the treatment of vulvovaginal atrophy. Curr Opin Obstet Gynecol 27:504–508
Hutchinson-Colas J, Segal S (2015) Genitourinary syndrome of menopause and the use of laser therapy. Maturitas 82:342–345
http://www.monalisatouch.com/wp-content/uploads/2016/12/Smartxide2-V2LR-Brochure-ING-Rev-12.2.pdf. Accessed at 05/05/2017
Salvatore S, Leone Roberti Maggiore U, Origoni M, Parma M, Quaranta L, Sileo F, Cola A, Baini I, Ferrero S, Candiani M, Zerbinati N (2014) Microablative fractional CO2 laser improves dyspareunia related to vulvovaginal atrophy: a pilot study. J Endom Pelv Pain Disord 6:150–156
Zerbinati N, Serati M, Origoni M, Candiani M, Iannitti T, Salvatore S, Marotta F, Calligro A (2015) Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci 22:845–849
Salvatore S, Nappi RE, Zerbinati N, Calligaro A, Ferrero S, Origoni M, Candiani M, Leone Roberti Maggiore U (2014) A 12-week treatment with fractional CO2 laser for vulvovaginal atrophy: a pilot study. Climacteric 17:363–369
Salvatore S, Nappi RE, Parma M, Chionna R, Lagona F, Zebinati N, Ferrero S, Origoni M, Candiani M, Leone Roberti Maggiore U (2015) Sexual function after fractional microablative CO2 laser in women with vulvovaginal atrophy. Climacteric 18:219–225
Perino A, Calligaro A, Forlani F, Tiberio C, Cucinella G, Svelato A, Saitta S, Calagna G (2015) Vulvo-vaginal atrophy: a new treatment modality using thermo-ablative fractional CO2 laser. Maturitas 80:296–301
Pieralli A, Fallani MG, Becorpi A, Bianchi C, Corioni S, Longinotti M, Tredici Z, Guaschino S (2016) Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet 294:841–846
Perino A, Cucinella G, Gugliotta G, Saitta S, Politi S, Adie B, Marci R, Calagna G (2016) Is vaginal fractional CO2 laser treatment effective in improving overactive bladder symptoms in post-menopausal patients? Preliminary results. Eur Rev Med Pharmacol Sci 20:841–846
Sokol ER, Karram MM (2016) An assessment of the safety and efficacy of fractional CO2 laser system for the treatment of vulvovaginal atrophy. Menopause 23:1102–1107
Athanasiou S, Pitsouni E, Antonopoulou S, Zacharakis D, Salvatore S, Falagas ME, Grigoriadis T (2016) The effect of microablative fractional CO2 laser on vaginal flora of postmenopausal women. Climacteric 19:512–518
Pitsouni E, Grigoriadis T, Tsiveleka A, Zacharakis D, Salvatore S, Athanasiou S (2016) Microablative fractional CO2 laser therapy and the genitourinary syndrome of menopause: an observational study. Maturitas 94:131–136
Murina F, Karram M, Salvatore S, Felice R (2016) Fractional CO2 laser treatment of the vestibule for patients with vestibulodynia and genitourinary syndrome of menopause: a pilot study. J Sex Med 13:1915–1917
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D’Agostino R Jr (2000) The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26:191–208
Wiegel M, Meston C, Rose R (2005) The female sexual function index (FSFI): cross validation and development of clinical cutoff scores. J Sex Marital Ther 31:1–20
Athanasiou S, Grigoriadis T, Kyriakidou N, Giannoulis G, Antsaklis A (2012) The validation of international consultation on incontinence questionnaires in the Greek language. Neurourol Urodyn 31:1141–1144
Coyne KS, Payne C, Bhattacharyya SK, Revicki DA, Thompson C, Corey R, Hunt TL (2004) The impact of urinary urgency and frequency on health-related quality of life in overactive bladder: results from a National Community Survey. Value Health 7:455–463
Lukacz ES, Whitcomb EL, Lawrence JM, Nager CW, Luber KM (2009) Urinary frequency in community-dwelling women: what is normal? Am J Obstet Gynecol 200:552.e1–552.e7
Weber MA, Limpens J, Roovers JPWR (2015) Assessment of vaginal atrophy: a review. Int Urogynecol J 26:15–28
Salvatore S, Leone Roberti Maggiore U, Athanasiou S, Origoni M, Candiani M, Calligaro A, Zerbinati N (2015) Histological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo study. Menopause 22:845–849
Campolmi P, Bonan P, Cannarozzo G, Bassi A, Bruscino N, Arunachalam M, Troiano M, Lotti T, Moretti S (2012) Highlights of thirty-year experience of CO2 laser use at the Florence (Italy) department of dermatology. ScientifWorldJournal 2012:546528
Nappi RE, Placios S, Panay N, Particco M, Krychman ML (2016) Vulvar and vaginal atrophy in four European countries: evidence from the European REVIVE Survey. Climacteric 19:188–197
Nappi RE, Kingsberg S, Maamari R, Simon J (2013) The CLOSER (clarifying vaginal atrophy’s impact on sex and relationships) survey: implications of vaginal discomfort in postmenopausal women and in male partners. J Sex Med 10:2232–2241
Nappi RE, Kokot-Kierepa M (2012) Vaginal health insights, views and attitudes (VIVA)—results from an international survey. Climacteric 1:36–44
Palma F, Volpe A, Villa P, Cagnacci A, as the writing group of the AGATA study (2016) Vaginal atrophy of women in postmenopause. Results from a multicentric observational study: the AGATA study. Maturitas 83:40–44
Ettinger B, Hait H, Reape KZ, Shu H (2008) Measuring symptom relief in studies of vaginal and vulvar atrophy: the most bothersome symptom approach. Menopause 15:885–889
Santoro N, Komi J (2009) Prevalence and impact of vaginal symptoms among postmenopausal women. J Sex Med 6:2133–2142
Kingsberg SA, Wysocki S, Magnus L, Krychman ML (2013) Vulvar and vaginal atrophy in postmenopausal women: findings from the REVIVE (Real Women’s Views of Treatment Options for Menopausal Vaginal Changes) survey. J Sex Med 10:1790–1799
Ballagh SA (2005) Vaginal hormone therapy for urogenital and menopausal symptoms. Semin Reprod Med 23:126–140
Chollet JA (2011) Efficacy and safety of ultra-low-dose Vagifem (10mcg). Patient Prefer Adherence 5:571–574
Simunic V, Banovic I, Ciglar S, Jeren L, Pavicic Baldani D, Sprem M (2003) Local estrogen treatment in patients with urogenital symptoms. Int J Gynaecol Obstet 82:187–197
Lose G, Englev E (2000) Oestradiol-releasing vaginal ring versus oestriol vaginal pessaries in the treatment of bothersome lower urinary tract symptoms. BJOG 107:1029–1034
Weber MA, Lim V, Oryszczyn J, Te West N, Souget J, Jefery S, Roovers JP, Moore KH (2017) The effect of vaginal oestriol cream on subjective and objective symptoms of stress urinary incontinence and vaginal atrophy: an international multi-centre pilot study. Gynecol Obstet Investig 82:15–21
Murina F, Graziottin A, Felice R, Di Francesco S (2016) Coital pain in the elderly: could a low dose estriol gel thrill the vulvar vestibule? Eur J Obstet Gynecol Rerod Biol 207:121–124
Hosseinzadeh P, Ghahiri A, Daneshmand F, Ghasemi M (2015) A comparative study of vaginal estrogen cream and sustained-release estradiol vaginal tablet (Vagifem) in the treatment of atrophic vaginitis in Isfahan, Iran 2010-2012. J Res Med Sci 20:1160–1165
Acknowledgements
We thank Maria Papaefthimiou, Vasiliki Papadopoulou, and Christina Nikka for their help during the study protocol.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding/support
None.
Conflicts of interest
Stefano Salvatore has had financial relations (expert testimonies and lectures) with DEKA Laser. The other authors report no potential conflicts of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Pitsouni, E., Grigoriadis, T., Falagas, M. et al. Microablative fractional CO2 laser for the genitourinary syndrome of menopause: power of 30 or 40 W?. Lasers Med Sci 32, 1865–1872 (2017). https://doi.org/10.1007/s10103-017-2293-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-017-2293-8