Abstract
Innovations in optical spectroscopy have helped the technology reach a point where performance previously seen only in laboratory settings can be translated and tested in real-world applications. In the field of oncology, spectral tissue sensing (STS) by means of optical spectroscopy is considered to have major potential for improving diagnostics and optimizing treatment outcome. The concept has been investigated for more than two decades and yet spectral tissue sensing is not commonly employed in routine medical practice. It is therefore important to understand what is needed to translate technological advances and insights generated through basic scientific research in this field into clinical practice. The aim of the discussion presented here is not to provide a comprehensive review of all work published over the last decades but rather to highlight some of the challenges found in literature and encountered by our group in the quest to translate optical technologies into useful clinical tools. Furthermore, an outlook is proposed on how translational researchers could proceed to eventually have STS incorporated in the process of clinical decision-making.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The interaction of light within tissue to recognize disease has been widely researched since the mid-19th century when Joseph von Fraunhofer developed diffraction grating. A large number of scientists have brought optical spectroscopy forward and enabled it to become a precise and quantitative scientific technology. In recent years, improvements made to spectrometers, software, and overall design positively affected instrument characteristics such as speed, sensitivity, size, and price. These technological advances, combined with increased awareness of the potential of optical spectroscopy have led to the development of optical systems which were usable for clinical research purposes and allowed further exploration of the potential applications. In the medical field the technology has gained interest for numerous biomedical applications for its advantages over existing conventional techniques. Optical spectroscopy at infrared and visible wavelengths avoids the use of ionizing radiation, is non-destructive, utilizes relatively inexpensive equipment, and can be performed near real-time without pharmaceutical means to enhance contrast, i.e., contrast agents. Several spectroscopic techniques have been applied for tissue characterization, including; diffuse reflectance spectroscopy (DRS); autofluorescence spectroscopy (FS); elastic scattering spectroscopy (ESS); and Raman Spectroscopy (RS). All of these methods rely on the same underlying principle: tissue characterization is performed by measuring the spectral response after the tissue is illuminated with a selected spectral band of light. This spectral response contains specific quantitative morphologic, compositional, and functional information about the probed tissue, thereby enabling tissue discrimination. Especially in the field of oncology, characterization of human tissues by optical spectroscopy (spectral tissue sensing; STS) is considered to have major potential. Various STS methods already have been used for tissue assessment in several organs for years with promising results [1–11].
How to transfer optical spectroscopy research to clinical practice
Despite these technological advancements and promising results, fiber-optic STS technology has not (yet) found widespread clinical acceptance in medical practice. This gap between original research and final clinical implementation is not specific for STS. It is considered to be one of the key aspects of translational research in general, as it can take more than two decades before the findings of original research become part of routine clinical practice [12, 13]. However, awareness of the causes of the gap and potential bridging strategies could help the field of STS avoiding unnecessary delay in the evolution of this technology into clinical useful tools.
For example, research in this field is often not focused on the potential application or clinical relevance [14]. This might not come across as a problem, since indeed, many transformative discoveries leading to inventions that are now used in daily clinical practice did not originate from application-directed research [15, 16]. However, in the case of STS, the field has become mature technologically and reached a point where spectral tissue sensing in its current form is ready to enter the clinical arena. Since translating novel technologies into clinical applications is a very time-consuming and expensive process, it is important to assess the clinical relevance of an application and keep this under constant review during clinical research as this will eventually be a dominating force in the process of successful implementation in the clinic [17, 18]. Furthermore, the success of an intended application will also partly depend on the extent of additional improvements in detection sensitivity and specificity in combination with instrument cost. Expensive techniques that are slightly better compared to well-established methods will be more difficult to implement in the hospital. It can be highly rewarding to perform a cost-benefit analysis in a very early stage and understand the preferences and drivers of the various stakeholders (e.g., patients, health insurances, health care providers, regulatory bodies) [16, 19]. In addition to the clinical relevance, also the extent to which the clinical workflow needs to be adapted is a major factor determining the feasibility of a new method in clinical practice. Techniques that are not compatible with the existing clinical routines are likely to encounter more resistance from physicians during implementation than those that can easily be added to the accustomed process. Moreover, modification of the accepted workflow can generate secondary effects on the outcome of the procedure that may counteract the intended benefits. On the other hand, when a new method significantly improves procedure outcome or shortens procedure time, disrupting the existing clinical workflow is likely to be a smaller obstacle. Researchers should be aware of this important trade-off in an early stage of clinical research.
Besides these clinical aspects, it should be noted that optical spectroscopy is a very broad concept including many settings and configurations. The range of different optical technologies and available hardware choices lead to a complicated process of convergence upon the optimal system for each specific clinical need. For example, for reflectance spectroscopy, distance between source and detection fibers to a large extend defines the probing depth and spatial resolution, and therefore determines the feasibility of a system for a certain clinical application. Since challenges in the biomedical field are extremely versatile, developing a universal solution applicable to each clinical problem is unlikely to be possible. As a consequence, the clinical success of optical spectroscopy in general is highly dependent on finding the best modality with appropriate optical geometry for a specific application.
Seeking in-depth collaboration with medical physicians may help basic and translational scientists to acquire greater understanding of both the medical aspects and the optics of the clinical problem, and design a solution appropriate for the specific clinical problem [19, 20]. Comprehensive collaboration is not only important to elucidate the relevant details of the clinical problem [18], but also for tackling other non-scientific challenges (i.e., previously mentioned barriers such as workflow issues and clinical acceptance as well as regulation issues) that translational researchers are faced with [21, 22]. Invariably, extensive expertise is needed as technology develops from the preclinical stage towards increasingly complex and demanding phases of clinical testing, where patient safety and clinical usability become major determinants for progress. Furthermore, similar to the process of translating drug discoveries, the participation of industrial partners, especially during testing in clinical trials, can help financing the often costly trials and help to reflect on the feasibility of implementing an application in terms of cost-effectiveness [23, 24]. Therefore, close collaboration and continuous communication between researchers (basic and translational), clinicians, and industry professionals is required, even if individuals’ needs, motivations, and research attitudes may differ [21, 24–26]. Because the perspectives of co-operating partners may be different and might even change during the development of an application it is difficult to set up a network of co-operating partners. However, this interactive multidisciplinary approach is the only way to properly match technology and clinical problem and give direction to clinically valuable research which can ultimately lead to an accepted clinical application.
Translating technology into clinical applications is not confined to taking into account the previously described non-technical barriers and establishing an optimal environment for translational research. Conducting translational optical research in a medical environment brings some typical challenges and potential pitfalls that are likely to be universal across the biomedical optical research field. To our knowledge, few investigators have undertaken the task of describing these key challenges. In the following sections we attempt to provide an overview of the practical challenges that were found in literature as well as those that the authors encountered during nearly a decade of clinical testing and evaluation. The first four key challenges presented are related to the struggles encountered during the acquisition of reliable optical data and interpretation of it. The last key challenge discusses how fiber-optic STS can impact clinical decision-making which is the ultimate goal of translational research.
Key challenges
Proper study design
Obviously, the design of a study is important as it influences the quality and relevance of study results. Preclinical studies on animals or ex vivo measurements on human specimens may serve as a surrogate for in vivo measurements and usually provide useful information in the first phase of development. However, when it comes to human disease applicability, they do not necessarily reflect the in vivo status of human tissue for all applications. For example, given the differences between in vivo and ex vivo tissues, validating a database from ex vivo data and applying it to in vivo data may not work as various tissue parameters (e.g., blood content, oxygenation) might change once the tissue has been removed from the patient’s body [27]. On the contrary, research also suggests that these differences are limited to the blood-related wavelengths and for example, the near-infrared wavelengths are not affected by tissue status. Furthermore, in vivo studies gathering spectral tissue data in a well-controlled setting can be limited because this data might not be representative for real-world situation. For instance, estimates for blood content and associated oxygenation levels might show promising differences when measured in vivo during surgery. However, once measured during a percutaneous biopsy procedure, these parameters do not necessarily reflect the true physiological composition of the measured tissue due to pooling of blood around the needle tip [28]. Similarly, blood present on top of the surface of a resection margin may be major obstacle for resection margin assessment by STS [29]. All these circumstances should be taken in consideration when interpreting measurements but also in a later stage during the designing and constructing of a clinical STS tool.
Much of the research reported to date has been based on observational studies, and a large portion of the scientific knowledge in this field comes from analyzing spectroscopic data observational studies. Data from such studies may help to prove clinical feasibility and develop new trials by determining sample size requirements and optimal design, but may be confounded when data used for algorithm training is also used for validation.
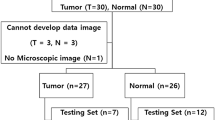
Once early-phase human studies have been conducted, research efforts generally move to the larger clinical trials. Such studies and subsequent clinical implementation require that the equipment and analytical algorithms have been optimized and fitted to be used in the clinical routine. Especially in this stage of clinical validation it is important that the basic principles and potential pitfalls of diagnostic test development are well understood. For instance, as clearly elaborated by M. Fitzmaurice [30], unintentional bias in selecting patients for study groups may lead to the conclusion that a new optical technique is a better or worse diagnostic tool than it really is. Furthermore, measures of test performance, such as sensitivity and specificity are not only influenced by the definition of the threshold between positive and negative results but also disease prevalence. For instance, if a new diagnostic tool is tested in a high prevalence setting, it is more likely that persons who test positive, truly have disease than if the test is performed in a population with low prevalence. In addition, selection of patients based on visual clues may lead to serious optical bias in a dataset. For instance in a study described by de Veld et al. on oral cancer an apparently excellent sensitivity and specificity for distinguishing a visually detected suspect lesion from normal mucosa was reported, while the clinically relevant question: can we distinguish malignant lesions from benign lesions could not be answered [31].
Thus, researchers have to concede the restrictive nature of testing in a preclinical and in well-controlled clinical settings when it comes to real-world applicability. Eventually, performing well-designed large-scale clinical trials will help to gain trust in the actual performance of new optical technologies.
Co-registration between spectral measurements and histology
Histology remains the gold-standard for diagnosis and staging in oncology, making it in essence a ground truth for new technologies attempting to measure and quantify these pathologies. Once registered, histopathology provides valuable information regarding the structure and composition of tissues and is often used to understand the physiological mechanisms behind spectral contrasts.
Consequently, registration of histology serves as an important and necessary validation step for novel optical spectroscopy based diagnostic techniques. However, the use of histopathology as benchmark does suffer from a number of critical limitations. Co-registration of separate optical and physical biopsies is subject to imperfect spatial correlation of the optical reading and the tissue sample removed for histopathological analysis [30, 32]. Several methods have been employed to achieve sufficient accurate co-registration. To facilitate registration, usually a tissue sample is removed from the measurement spot after spectral measurements are completed or a marker is left behind, such as a dye or suture. These methods are susceptible to location mismatch that can be particularly challenging in the case of micro-environmental heterogeneity. Even more difficulties in co-registration arise when the tissue site being investigated is not directly accessible to the operator. For example, in cases that in vivo measurements are obtained through the working channel of an endoscope or through a hollow needle at deep located tissue. In these cases the tissue sample for histopathological evaluation is generally obtained by a second needle after retracting the fiber-optic probe used for spectral measurements. Linking spectral data with such a “best estimate” of the spectral measurement spot leads to inherent registration inaccuracies.
An approach to address discrepancies between spectral data and histology is to integrate fiber-optics into standard tissue-sampling tools, such as a core biopsy needle or endoscopic biopsy forceps [32–34], thereby linking spectral tissue sensing and biopsy functionality in a single instrument. A few examples are shown in Fig 1. These integrated fiber-optic instruments represent a major step forward for clinical evaluation of new spectral tissue sensing techniques by greatly increasing the spatial correlation of physical biopsies with spectral measurement spots and simplifying study procedures. Beyond validation studies, the developed integrated fiber-optic tools could be clinically useful for increasing the pre-biopsy probability of obtaining representative tissue samples in diagnostic biopsy procedures (Fig. 2). Despite (almost) perfect co-registration between the optical and physical biopsy with integrated fiber-optic tools, histopathological analysis still is fundamentally limited in accuracy. With the use of fiber-optic probes tissue volumes of approximately 1 mm3 can be interrogated, whereas usually the conventional biopsy samples are larger than this. Another complicating factor is the fact that histopathological evaluation of specimens is performed on two-dimensional histological section where as optical measurements yield information of three-dimensional tissue volumes. Finding and orienting a representative two-dimensional histological section in a three-dimensional ex vivo tissue volume can therefore be challenging. Especially when taken in consideration that during the processing of the tissue deformation and cutting artifacts are also common [35].
Integrated fiber-optics in clinical biopsy tools allow 1:1 correlation between spectral data and biopsy sample. a The WavSTAT biopsy forceps for optical diagnosis based on laser-induced autofluorescence spectroscopy. Image courtesy of SpectraScience Inc., San Diego, CA, USA. b Elastic scattering spectroscopy through an integrated endoscopic tool for use in a range of applications suitable to the upper gastrointestinal (GI) tract and the colon. Image courtesy of I.J. Bigio, Boston University. c Added quantitative spectral functionality during routine percutaneous biopsy procedures using a fiber-optic core biopsy needle (Philips Research, Eindhoven, the Netherlands)
Example of spectral tissue sensing functionality integrated in a “smart” clinical instrument. Real-time tissue characterization of the tissue at the needle tip is performed during lung biopsy, thereby providing guidance to the physician. This could help to increase successful biopsy yield. Image courtesy of Clinical Cancer Research [28]
To make the problem even more complex, histopathological tissue diagnosis by pathologists is subject to significant inter- and intra-observer variability [30]. This is a particularly difficult problem in the diagnosis and grading of dysplasia, a premalignant lesion seen in patients at high risk for development of carcinoma.
Furthermore, in case of STS the acquired information from tissue is from a different nature compared to the information provided by histopathologic assessment. In example, STS can provide quantified measures of substances present in tissue whereas the pathologist regards tissue in terms of normal or tumorous. Classifying STS measurements based on these historically developed pathologic definitions can lead to erroneous classification. This mismatch between information types requires translational scientist to fully comprehend the limitations and biases of the gold standard as it will seriously hamper clinical acceptance of a novel method.
Thus, the apparent diagnostic performance of a new technology will therefore depend not only on its ability to detect abnormalities, but also on the (in)accuracy of the gold standard. Even if a novel technology is 100% sensitive and 100% specific, it may appear inaccurate when either the golden standard is imperfect or incorrectly applied. Therefore, careful attention should be paid to adequacy of tissue samples, correlation with measured tissue sites, and consistency of pathology reporting terminology. Although comparison between STS and histopathology is challenged in many ways, this should not be interpreted or used as an argument to stop the efforts of translating STS to the clinic.
Inter-patient and intra-patient variation
Characterizing and differentiating between various tissues by an optical spectroscopy system relies on measurement of the absolute or relative differences in intensity or spectral contrasts between the tissue types of interest. However, sources of variation such as inter- and intra-patient variability may outweigh the difference between the tissue types of interest leading to hampered diagnostic performance. Tumor tissue is well known for its heterogeneity,[36] but also in healthy tissues non-uniformity is a common phenomenon [37, 38]. In particular, breast tissue is a well-known example of inter and intra-patient variation [39, 40]. The optical contrast between healthy and tumorous tissue can be manipulated by other sources of contrast which are related to biological processes such as menopausal status and the phase of the menstrual cycle [41]. This does not necessarily have to be the case, but researchers should be aware of these potential disturbing factors. Including patient demographics to the databases with reference measurements can circumvent the unwanted blurring of optical contrast by sources not related to the difference between normal and tumor tissue [39]. However, this might also require further extending the database with a comprehensive amount of reference measurements to comprise the influence of all patient characteristics. Another approach is to measure optical characteristics at a distant location from the tissue site under evaluation and use these measurements as an internal reference. In this case, instead of the absolute values, relative changes between tissue sites are used. Taroni et al. [42], Laughney et al. [43], and Spliethoff et al. [44] found that such methods could be applied to account for the tissue- and patient heterogeneity in breast and lung tissue. This indicates that using the patient’ measurement as its own reference is effective in reducing the influence of inter-patient variation. Such a method might be very useful in a clinical setting since heterogeneity is also reported in studies of other tissues such as prostate and nasopharyngeal tissue [45, 46].
For biopsy procedures, STS measurements can also be performed in a continuous mode. Opposed to points measurements of the different tissue types a continuous series of measurements has the advantage of providing a full overview of the tissue characterization along the needle path and allows an evaluation of the local changes, rather than a comparison to a cohort based reference value. Recently, Nachabe et al. demonstrated the potential of real-time tissue characterization by diffuse optical spectroscopy measurements at the tip of a needle during percutaneous interventions [47]. Such continuous measurements may be of great relevance during percutaneous procedures, because they enable detection of the transition from healthy tissue to tumor based on the clinical parameters derived from STS measurements.
Thus, several investigators have shown the benefit of deriving relative diagnostic criteria by calculating differential spectral tissue parameters between the tumor and a reference tissue. The use of relative tissue parameters may help to define more effective detection criteria that are less sensitive to inter-patient variations and tissue heterogeneities.
Spectral analysis and classification methods
There is no substitute for a good study design and proper data collection, but after proper data collection, pre-processing of raw spectral data is often an important subsequent step. The goal of pre-processing of raw spectral data is to apply the calibrations to remove device specific features of the data. After preprocessing, the data can be interpreted by performing further analysis on the spectral data which ultimately enables classification of the measured tissue sites.
One method for tissue classification is to use pattern recognition by supervised machine learning methods. This method correlates spectral features directly to tissue type labels, thereby enabling identification of unknown tissue based on the measured spectra without the need for extensive data processing. Various approaches of spectral analysis have been developed, including multivariate statistical data analysis [3], partial least squares discriminant analysis [48], support vector machines and statistical learning [48], k-nearest neighbor classification [49], as well as neural network methods [50, 51]. Due to the nature of the supervised machine-learning approaches, the diagnostic performance is usually compromised when the number of classes increases. Theoretically, discriminating tumor from surrounding healthy tissue is a two-class problem (healthy versus malignant). However, in practice tumor tissue is surrounded by many tissue types, both healthy and diseased, and this demands identification of a wider variety of tissue pathologies, including histological tumor subtypes, inflammation, and fibrosis. Having to deal with this tissue heterogeneity poses a true challenge in the development of machine learning approaches [52, 53]. To overcome this difficulty a comprehensive high-quality spectral database is required containing any healthy or diseased tissue type that is likely to be encountered during a clinical procedure [54].
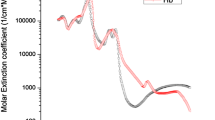
Several investigators have analyzed the spectral information in a different manner by applying mathematical models based on knowledge of light propagation in tissue to determine the scattering and absorption properties within the tissue [55–57]. Each measured spectra is in fact a combination of the spectral signatures of various tissue chromophores present in the probed volume. Meaningful estimation of these components can be extracted by using the known absorption spectra of these biologically relevant chromophores. The main benefit of this approach is that it uses a priori knowledge of light-tissue interaction that can help to understand the underlying biological composition and physiological processes that determine spectral shape. Over the years, the differences in composition between malignant and normal tissues have been extensively researched by this approach. Understanding which biological substances could potentially play a role in identification of abnormal tissue may be very useful. In our own group we found that, the biological chromophore bile is significantly higher in healthy liver as opposed to colorectal liver metastases [5, 58]. In the same way, breast tumor has shown to contain far less fat and more water compared to surrounding healthy tissue [59]. The often-used diffusion theory has proven to be sufficiently realistic to describe light transport in many different human tissues. But is should be noticed that these diffusion theory based fit models require that the optical properties of the tissue are either homogeneous or close to homogeneous as well as sufficient source-detector distance. Care should be taken when basic assumptions of the theory are violated. Highly inhomogeneous tissue (for example layered tissue) or tissue with high absorption and low scattering (for example when a substantial amount of blood is present) may result in unrealistic estimations of the tissue composition. And, even when the criteria are met, a realistic estimation of the true composition of the tissue can only be obtained when all the absorption spectra of tissue chromophores actually present in the measurement are included in this process. However, adding absent or too many chromophores in this method may lead to erroneous estimations of the tissue characteristics.
Over the years, a variety of advanced computational methods has been developed to improve the quantitative and qualitative diagnostic capability of spectral tissue sensing. The occurrence and co-occurrence of specific spectral signatures depend on the underlying physical, morphological, and biochemical tissue composition. Whatever method is used for interpretation of the spectral data, expert knowledge should be employed throughout the various stages of clinical research such that robust tissue discrimination algorithms can be developed.
Impacting clinical decision-making
The objective of each new technology is to support clinicians in reaching a decision regarding diagnosis or treatment of a disease, and ultimately fundamentally improve patient care. In order to help in the process of decision-making, it is important to consider at which point in the workflow the technology can play a central role, based on its strengths and weaknesses. The main advantage of STS methods that use endogenous contrast is the possibility to perform real-time tissue characterization in a non-destructive manner at multiple points in time. This enables to obtain optical measurements without obstructing pathological examination protocols and allows optical tissue sensing to be employed as a pre-pathology modality by surgeons and radiologist while performing a procedure. Furthermore, since the technology can be integrated in needles or probes, STS can be combined with other complementary modalities. In combination with the versatility of configurations that STS can have this permits a wide range of different applications. These strong qualities provide STS with the power to make a difference in cancer treatment.
As mentioned previously, spectral tissue sensing technologies have been researched for several oncological applications. The question is which applications at which point in oncological care (e.g., prevention, screening, diagnosis, treatment, management, surveillance) have the greatest potential to contribute substantially to clinical decision-making. Application of STS in different stages of this process also demands different requirements in order to provide useful input for clinical decision-making. For example, a screening application is likely to affect the entire care path of a patient. This can improve prognosis for the patient tremendously since successful early detection of cancer enables curative treatment and hence, result in considerable gain for the patient [60]. Unfortunately, implementation of early detection methods is also challenging since the information provided by the new technology can alter the entire workflow of patient care as a consequence. Introducing an end-of-line application on the other hand, will likely change the procedure of cancer management less radically and by leaving the current workflow intact the much needed clinical acceptance can be acquired faster.
Another important consideration when preparing a tool for clinical use is the trade-off between sensitivity and specificity. Depending on the intended application, a higher sensitivity or specificity is desired. Furthermore, in order to optimize the diagnostic performance, it may be necessary to adjust the decision threshold, based on the specific type of patient studied. The same diagnostic tool may need different decision thresholds when used in high-risk patients (high disease prevalence) than when used as a screening test in the general population (low disease prevalence) [30].
Ultimately, cost effectiveness and the impact on procedure outcome are major important considerations for successful clinical application. It is crucial to view the expected added clinical value of a new clinical method in the context of the evolving landscape of medical practice (need for increased productivity and improved patient outcomes) and the macroeconomic health care environment (cost constraints). From a clinical application perspective, it makes sense to start with the development of applications that can be used as adjunct tools to other established imaging modalities in oncology. Because STS can be integrated into familiar clinical instruments, it could be easily adopted as an “add-on” to the existing protocols with minimal impact on procedure flow. For instance, in case of biopsy guidance, STS can be used in conjunction with conventional imaging modalities thereby exploiting the complementary strengths of each method. We anticipate that STS will also find its way to clinical settings where no good tools exist today, especially in situations where under-treatment has a significant negative impact. For example, in case of guided surgery, STS has the potential to influence “on-table” decision-making during treatment.
Outlook
Spectral tissue sensing research holds tremendous promise for the development of novel diagnostic and therapeutic tools for many oncological applications. After a quarter century of rapid advances, spectroscopic research has generated a rich body of ideas, insights, and discoveries as well as the necessary technical improvements. As in all areas of medicine, the maturation of an experimental, early-phase technological concept into useful clinical tool is a long and complex process usually involving many years of rigorous preclinical and clinical testing and many setbacks and failures. The goal of this article is to raise awareness among the optical community about some key challenges that should be acknowledged in the process of translating STS technology towards the clinic, and thus contribute to the clinical implementation of STS. In order to realize the potential of spectral tissue sensing, there are still hurdles to overcome to bridge the gap between technological advances and clinical practice. These issues are clearly surmountable although this does require effort from the entire scientific, medical, and industrial community. Without any claim of completeness, we highlighted various challenges faced by translational researchers as they move from the proof-of-concept stage through the translational stage and into the clinical setting. We believe that a broad-based, multidisciplinary effort and in-depth collaboration between biomedical researchers and clinicians as well as involvement of industrial partners with a clear focus on a well-defined clinical problem can help to address these key challenges.
References
Cerussi A, Shah N, Hsiang D, Durkin A, Butler J, Tromberg BJ (2006) In vivo absorption, scattering, and physiologic properties of 58 malignant breast tumors determined by broadband diffuse optical spectroscopy. J Biomed Opt 11(4):044005. doi:10.1117/1.2337546
Brown JQ, Wilke LG, Geradts J, Kennedy SA, Palmer GM, Ramanujam N (2009) Quantitative optical spectroscopy: a robust tool for direct measurement of breast cancer vascular oxygenation and total hemoglobin content in vivo. Cancer Res 69(7):2919–2926. doi:10.1158/0008-5472.CAN-08-3370
Volynskaya Z, Haka AS, Bechtel KL, Fitzmaurice M, Shenk R, Wang N, Nazemi J, Dasari RR, Feld MS (2008) Diagnosing breast cancer using diffuse reflectance spectroscopy and intrinsic fluorescence spectroscopy. J Biomed Opt 13(2):024012. doi:10.1117/1.2909672
Evers DJ, Nachabe R, Vranken Peeters MJ, van der Hage JA, Oldenburg HS, Rutgers EJ, Lucassen GW, Hendriks BH, Wesseling J, Ruers TJ (2013) Diffuse reflectance spectroscopy: towards clinical application in breast cancer. Breast Cancer Res Treat 137(1):155–165. doi:10.1007/s10549-012-2350-8
Evers DJ, Nachabe R, Hompes D, van Coevorden F, Lucassen GW, Hendriks BH, van Velthuysen ML, Wesseling J, Ruers TJ (2013) Optical sensing for tumor detection in the liver. Eur J Surg Oncol 39(1):68–75. doi:10.1016/j.ejso.2012.08.005
Zonios G, Dimou A, Carrara M, Marchesini R (2010) In vivo optical properties of melanocytic skin lesions: common nevi, dysplastic nevi and malignant melanoma. Photochem Photobiol 86(1):236–240. doi:10.1111/j.1751-1097.2009.00630.x
Rajaram N, Reichenberg JS, Migden MR, Nguyen TH, Tunnell JW (2010) Pilot clinical study for quantitative spectral diagnosis of non-melanoma skin cancer. Lasers Surg Med 42(10):716–727. doi:10.1002/lsm.21009
A’Amar OM, Liou L, Rodriguez-Diaz E, Delas Morenas A, Bigio IJ (2013) Comparison of elastic scattering spectroscopy with histology in ex vivo prostate glands: potential application for optically guided biopsy and directed treatment. Lasers Med Sci 28(5):1323–1329. doi:10.1007/s10103-012-1245-6
Chang VT, Bean SM, Cartwright PS, Ramanujam N (2010) Visible light optical spectroscopy is sensitive to neovascularization in the dysplastic cervix. J Biomed Opt 15(5):057006. doi:10.1117/1.3495730
Bard MP, Amelink A, Skurichina M, Noordhoek Hegt V, Duin RP, Sterenborg HJ, Hoogsteden HC, Aerts JG (2006) Optical spectroscopy for the classification of malignant lesions of the bronchial tree. Chest 129(4):995–1001. doi:10.1378/chest.129.4.995
Bigio IJ, Bown SG (2004) Spectroscopic sensing of cancer and cancer therapy. Cancer Biol Ther 3(3):259–267
Hanney SR, Castle-Clarke S, Grant J, Guthrie S, Henshall C, Mestre-Ferrandiz J, Pistollato M, Pollitt A, Sussex J, Wooding S (2015) How long does biomedical research take? Studying the time taken between biomedical and health research and its translation into products, policy, and practice. Health Res Policy Syst 13:1. doi:10.1186/1478-4505-13-1
Westfall JM, Mold J, Fagnan L (2007) Practice-based research—“Blue Highways” on the NIH roadmap. JAMA 297(4):403–406. doi:10.1001/jama.297.4.403
Ioannidis JPA (2006) Evolution and translation of research findings: from bench to where? PLoS Clin Trials 1(7):e36. doi:10.1371/journal.pctr.0010036
Vale NB, Delfino J, Vale LF (2005) Serendipity in medicine and anesthesiology. Rev Bras Anestesiol 55(2):224–249
Crowley WF (2003) Translation of basic research into useful treatments: how often does it occur? Am J Med 114:503–505. doi:10.1016/S0002-9343(03)00119-0
Fernandez-Moure JS (2016) Lost in translation: the gap in scientific advancements and clinical application. Front Bioeng Biotechnol 4. doi:10.3389/fbioe.2016.00043
Rousche P, Schneeweis DM, Perreault EJ, Jensen W (2008) Translational neural engineering: multiple perspectives on bringing benchtop research into the clinical domain. J Neural Eng 5(1):16–20. doi:10.1088/1741-2560/5/1/P02
Wagstaff A (2014) Five steps to putting innovation at the heart of cancer care. Cancer World 58:8
Peters NHGM, van Esser S, van den Bosch MAAJ, Storm RK, Plaisier PW, van Dalen T, Diepstraten SCE, Weits R, Westenend PJ, Stapper G, Fernandez-Gallardo MA, Borel Rinkes IHM, van Hillegersberg R, Mali WPTM, Peeters PHM (2011) Preoperative MRI and surgical management in patients with nonpalpable breast cancer: the MONET – randomised controlled trial. Eur J Cancer 47:879–886
Fudge N, Sadler E, Fisher HR, Maher J, Wolfe CDA, McKevitt C (2016) Optimising translational research opportunities: a systematic review and narrative synthesis of basic and clinician scientists’ perspectives of factors which enable or hinder translational research. PLoS One 11(8):e0160475. doi:10.1371/journal.pone.0160475
Meslin EM, Blasimme A, Cambon-Thomsen A (2013) Mapping the translational science policy ‘valley of death’. Clin Transl Med 2(14). doi:10.1186/2001-1326-2-14
Wagner PD, Sirvastava S (2012) New paradigms in translational science research in cancer biomarkers. Transl Res 159(4):343–353. doi:10.1016/j.trsl.2012.01.015
Ioannidis JPA (2004) Materializing research promises: opportunities, priorities and conflicts in translational medicine. J Transl Med 2(5)
Madry H, Alini M, Stoddart MJ, Evans C, Miclau T, Steiner S (2014) Barriers and strategies for the clinical translation of advanced orthopaedic tissue engineering protocols. Eur Cell Mater 27:17–21, discussion 21
Johnston SC, Hauser SL, Desmond-Hellmann S (2011) Enhancing ties between academia and industry to improve health. Nat Med 17(4):434–436
Palmer GM, Marshek CL, Vrotsos KM, Ramanujam N (2002) Optimal methods for fluorescence and diffuse reflectance measurements of tissue biopsy samples. Lasers Surg Med 30:191–200. doi:10.1002/lsm.10026
Spliethoff JW, Prevoo W, Meier MA, de Jong J, Evers DJ, Sterenborg HJ, Lucassen GW, Hendriks BH, Ruers TJ (2015) Real-time in vivo tissue characterization with diffuse reflectance spectroscopy during transthoracic lung biopsy: a clinical feasibility study. Clin Cancer Res. doi:10.1158/1078-0432.ccr-15-0807
Lin W-C, Toms SA, Jansen D, Mahadevan-Jansen A (2001) Intraoperative application of optical spectroscopy in the presence of blood. IEEE J Sel Top Quantum Electron 7(6):996–1003
Fitzmaurice M (2000) Principles and pitfalls of diagnostic test development: implications for spectroscopic tissue diagnosis. J Biomed Opt 5(2):119–130. doi:10.1117/1.429978
De Veld DCG, Skurichina M, Witjes MJH, Duin RPW, Sterenborg HJCM, Roodenburg JLN (2004) Clinical study for classification of benign, dysplastic, and malignant oral lesions using autofluorescence spectroscopy. J Biomed Opt 9(5):940–950. doi:10.1117/1.1782611]
Rodriguez-Diaz E, Bigio IJ, Singh SK (2011) Integrated optical tools for minimally invasive diagnosis and treatment at gastrointestinal endoscopy. Robot Comput Integr Manuf 27(2):249–256. doi:10.1016/j.rcim.2010.06.006
Rodriguez-Diaz E, Huang Q, Cerda SR, O’Brien MJ, Bigio IJ, Singh SK (2014) Endoscopic histological assessment of colonic polyps by using elastic scattering spectroscopy. Gastrointest Endosc. doi:10.1016/j.gie.2014.07.012
Kuiper T, Alderlieste YA, Tytgat KM, Vlug MS, Nabuurs JA, Bastiaansen BA, Lowenberg M, Fockens P, Dekker E (2015) Automatic optical diagnosis of small colorectal lesions by laser-induced autofluorescence. Endoscopy 47(1):56–62. doi:10.1055/s-0034-1378112
Chen LH, Ho H, Lazaro R, Thng CH, Yuen J, Ng WS, Cheng C (2010) Optimum slicing of radical prostatectomy specimens for correlation between histopathology and medical images. Int J Comput Assist Radiol Surg 5(5):471–487. doi:10.1007/s11548-010-0405-z
Marusyk A, Almendro V, Polyak K (2012) Intra-tumour heterogeneity: a looking glass for cancer? Nat Rev Cancer 12(5):323–334. doi:10.1038/nrc3261
Shah N, Cerussi AE, Jakubowski D, Hsiang D, Butler J, Tromberg BJ (2004) Spatial variations in optical and physiological properties of healthy breast tissue. J Biomed Opt 9(3):534–540. doi:10.1117/1.1695560
Gabrecht T, Lovisa B, van den Bergh H, Wagnieres G (2009) Autofluorescence bronchoscopy: quantification of inter-patient variations of fluorescence intensity. Lasers Med Sci 24(1):45–51. doi:10.1007/s10103-007-0518-y
Kennedy S, Geradts J, Bydlon T, Brown JQ, Gallagher J, Junker M, Barry W, Ramanujam N, Wilke L (2010) Optical breast cancer margin assessment: an observational study of the effects of tissue heterogeneity on optical contrast. Breast Cancer Res 12(6):R91. doi:10.1186/bcr2770
O’Sullivan TD, Leproux A, Chen J, Bahri S, Matlock A, Roblyer D, McLaren CE, Chen W, Cerussi AE, Su M, Tromberg BJ (2013) Optical imaging correlates with magnetic resonance imaging breast density and reveals composition changes during neoadjuvant chemotherapy. Breast Cancer Res 15(R14)
Pogue BW, Jiang S, Dehghani H, Kogel C, Soho S, Srinivasan S, Song X, Tosteson TD, Poplack SP, Paulsen KD (2004) Characterization of hemoglobin, water, and NIR scattering in breast tissue: analysis of intersubject variability and menstrual cycle changes. J Biomed Opt 9(3):541–552. doi:10.1117/1.1691028
Taroni P, Pifferi A, Quarto G, Spinelli L, Torricelli A, Abbate F, Balestreri N, Ganino S, Menna S, Cassano E, Cubeddu R (2012) Effects of tissue heterogeneity on the optical estimate of breast density. Biomed Opt Express 3(10):2411–2418. doi:10.1364/boe.3.002411
Laughney AM, Krishnaswamy V, Rizzo EJ, Schwab MC, Barth RJ, Pogue BW, Paulsen KD, Wells WA (2012) Scatter spectroscopic imaging distinguishes between breast pathologies in tissues relevant to surgical margin assessment. Clin Cancer Res 18(22):6315–6325. doi:10.1158/1078-0432.ccr-12-0136
Spliethoff JW, De Boer LL, Meier MA, Prevoo W, De Jong J, Bydlon TM, Sterenborg HJCM, Burgers JA, Hendriks BHW, Ruers TJM (2016) Spectral sensing for tissue diagnosis during lung biopsy procedures: the importance of an adequate internal reference and real-time feedback. Lung Cancer 98:62–68. doi:10.1016/j.lungcan.2016.05.019
Svensson T, Andersson-Engels S, Einarsdóttír M, Svanberg K (2007) In vivo optical characterization of human prostate tissue using near-infrared time-resolved spectroscopy. J Biomed Opt 12(1):014022. doi:10.1117/1.2435175
Nyst HJ, Van Veen RLP, Tan IB, Peters R, Spaniol S, Robinson DJ, Stewart FA, Levendag PC, Sterenborg HJCM (2007) Performance of a dedicated light delivery and dosimetry device for photodynamic therapy of nasophareyngeal carcinoma: phantom and volunteer experiments. Lasers Surg Med 39:647–653. doi:10.1002/lsm.20536
Nachabe R, Hendriks BH, Schierling R, Hales J, Racadio JM, Rottenberg S, Ruers TJ, Babic D, Racadio JM (2015) Real-time in vivo characterization of primary liver tumors with diffuse optical spectroscopy during percutaneous needle interventions: feasibility study in Woodchucks. Investig Radiol 50(7):443–448. doi:10.1097/rli.0000000000000149
Zhu C, Palmer GM, Breslin TM, Harter J, Ramanujam N (2006) Diagnosis of breast cancer using diffuse reflectance spectroscopy: comparison of a Monte Carlo versus partial least squares analysis based feature extraction technique. Lasers Surg Med 38(7):714–724. doi:10.1002/lsm.20356
Laughney AM, Krishnaswamy V, Garcia-Allende PB, Conde OM, Wells WA, Paulsen KD, Pogue BW (2010) Automated classification of breast pathology using local measures of broadband reflectance. J Biomed Opt 15(6):066019–066011–066019–066016. doi:10.1117/1.3516594
Farrell TJ, Wilson BC, Patterson MS (1992) The use of a neural network to determine tissue optical properties from spatially resolved diffuse reflectance measurements. Phys Med Biol 37(12):2281–2286
Bigio IJ, Bown SG, Briggs G, Kelley C, Lakhani S, Pickard D, Ripley PM, Rose IG, Saunders C (2000) Diagnosis of breast cancer using elastic-scattering spectroscopy: preliminary clinical results. J Biomed Opt 5(2):221–228
Li T, Zhang C, Ogihara M (2004) A comparative study of feature selection and multiclass classification methods for tissue classification based on gene expression. Bioinformatics 20(15):2429–2437. doi:10.1093/bioinformatics/bth267
Hsu H-H (2006) Advanced data mining technologies in bioinformatics. Idea Group Pub
Balog J, Szaniszlo T, Schaefer KC, Denes J, Lopata A, Godorhazy L, Szalay D, Balogh L, Sasi-Szabo L, Toth M, Takats Z (2010) Identification of biological tissues by rapid evaporative ionization mass spectrometry. Anal Chem 82(17):7343–7350. doi:10.1021/ac101283x
Palmer GM, Ramanujam N (2006) Monte Carlo-based inverse model for calculating tissue optical properties. Part I: theory and validation on sythetic phantoms. Appl Opt 45(5):1062–1071. doi:10.1364/AO.45.001062
Cerussi A, Shah N, Hsiang D, Durkin A, Butler J, Tromberg B (2006) In vivo absorption, scattering, and physiologic properties of 58 malignant breast tumors determined by broadband diffuse optical spectroscopy. J Biomed Opt 11(4):044005–044001–044005–044016. doi:10.1117/1.2337546
Zonios G, Dimou A (2009) Light scattering spectroscopy of human skin in vivo. Opt Express 17(3):1256–1267
Nachabé R, Evers DJ, Hendriks BHW, Lucassen GW, Van der Voort M, Wesseling J, Ruers TJM (2011) Effect of bile absorption coefficients on the estimation of liver tissue optical properties and related implications in discriminating healthy and tumorous samples. Biomed Opt Express 2(3):600–614
de Boer LL, Molenkamp BG, Bydlon TM, Hendriks BHW, Wesseling J, Sterenborg HJCM, Ruers TJM (2015) Fat/water ratios measured with diffuse reflectance spectroscopy to detect breast tumor boundaries. Breast Cancer Res Treat 152(3):509–518. doi:10.1007/s10549-015-3487-z
Etzioni R, Urban N, Ramsey S, McIntosh M, Schwartz S, Reid B, Radich J, Anderson G, Hartwell L (2003) The case for early detection. Nat Rev Cancer 3:1–10. doi:10.1038/nrc1041
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interests to declare.
Role of funding source
In this research was no involvement of funding sources.
Ethical approval/Informed consent
This research did not involve patients
Additional information
Lisanne L. de Boer and Jarich W. Spliethoff contributed equally to this work.
Rights and permissions
About this article
Cite this article
de Boer, L.L., Spliethoff, J.W., Sterenborg, H.J.C.M. et al. Review: in vivo optical spectral tissue sensing—how to go from research to routine clinical application?. Lasers Med Sci 32, 711–719 (2017). https://doi.org/10.1007/s10103-016-2119-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-016-2119-0