Abstract
This randomized placebo-blind study aimed to evaluate the effect of laser phototherapy (LPT) on pain caused by symptomatic irreversible pulpitis (SIP). Sixty patients diagnosed with SIP were randomly assigned to treatment groups (n = 15): G1 (control), G2 (laser placebo—sham irradiation), G3 (laser irradiation at 780 nm, 40 mW, 4 J/cm2), and G4 (laser irradiation at 780 nm, 40 mW, 40 J/cm2). Spontaneous pain was recorded using a VAS score before (T0), immediately after (T1), and 15 min after treatment (T2). Local anesthetics failure during emergency endodontic treatment was also assessed. There was no pain difference in T1 and T2 between the experimental laser groups (G3 and G4) and the placebo group (G2). The 4-J/cm2 (G3) irradiation resulted in significant increase in the local anesthetics failure in lower jar teeth. This effect could be suggested as consequence of the LPT improvement in local circulation and vasodilatation that would result in the increase of local anesthetic agent absorption. The application of 780-nm diode laser irradiation, at 4 and 40 J/cm2, showed no effect in reducing the pain in SIP in comparison to the placebo group. The fluence of 4 J/cm2 showed a negative effect in local anesthetics, resulting in significant increase of complimentary local anesthesia during emergency endodontic treatment. This work provides evidence of the consequence of LPT application on teeth with symptomatic irreversible pulpitis. LPT should be avoided in teeth with pain due to irreversible pulpitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pressure built up in the pulp cavity during pulp inflammation results in the nerve fiber pressure. This pressure causes mild to extreme pain, depending on the severity of the inflammation and the body’s response [1]. Laser phototherapy (LPT) has been shown to effectively relive pain of various etiologies [2, 3]. Particularly, infrared laser wavelength is widely used in pain modulation due to deeper penetration into tissues [4]. The exact mechanism of laser-induced pain relief is not yet completely understood; however, some hypotheses are described in literature. It has been postulated that LPT: 1—modulates the threshold of nociceptors [5]; 2—modulates inflammation by reducing prostaglandin E2(PGE2) concentrations, thus inhibiting cyclooxygenase 2 (COX-2) [6, 7]; 3—reduces tumor necrosis factor α (TNF-α) [8]; 4—enhances the release of endorphins [9]; and 5—enhances local hemodynamic, thus aiding the removal of pain-causing substances from the site of lesion [10, 11]. LPT, in vivo, has been shown to cause microcirculatory changes [12]. A significant arteriolar vasodilatation and a consequent increase of blood flow in microcirculation after irradiation with low power laser through infrared wavelength (830 nm) was described [12].
Although some mechanisms of laser induced pain relief as nociceptor threshold modulation, PGE2 reduction and increase in endorphin release could interpose positively in an acute pulp pain; others, as the increase of blood flow, could cause more pressure inside the pulp chamber, resulting in pain increase. At the present, it is not known if LPT would be beneficial or detrimental regarding pain during symptomatic irreversible pulpitis (SIP). This randomized placebo-blind study aimed to investigate the effect of LPT on pain caused by SIP.
Material and methods
This phase I clinical trial was conducted according to the Helsinki declaration, and was approved by the ethical committee of the School of Dentistry, University of Sao Paulo (#.08509912.3.0000.0075). Each patient signed a written informed consent to participate in the study, which was registered within ClinicalTrials.gov (NCT02169102).
Sixty adult patients participated in this study. All the patients were admitted to the Emergency Center of the School of Dentistry at the University of São Paulo.
The inclusion criteria were as follows: (1) patient with more than 18 years, (2) complain at the moment of the attendance of acute actively dental pain due to irreversible inflammation, and (3) prolonged pulp response to cold testing with Endo-Frost (Coltene-Roeko, Langenau, Germany).
The exclusion criteria were as follows: (1) pregnant and breastfeeding women, (2) exposed dental pulp, (3) necrotic dental pulp, and (4) patients making use of any medication that could interfere on pain.
After being diagnosed with irreversible pulpitis, the patients were randomly allocated in study groups by the Research Randomizer (computer software) (Version 4.0) [13]. The patients were blind to the treatment received.
Study groups
-
Group 1: control (no treatment)
-
Group 2: laser placebo (sham irradiation—equipment was turned off)
-
Group 3: laser irradiation at 40 mW, energy density: 4 J/cm2, energy per point: 0.16 J/point, total energy applied: 0.32 J. Two points of irradiation (4 s/point) were performed: the first perpendicularly to the tooth in the middle third of the crown and the second perpendicularly to the periapex.
-
Group 4: laser irradiation at 40 mW, energy density: 40 J/cm2, energy per point: 1.6 J/point, total energy applied: 3.2 J. Two points of irradiation (40 s/point) were performed: the first perpendicularly to the tooth in the middle third of the crown and the second perpendicularly to the periapex.
The low power laser used has beam area of 0.04 cm2 (MMOPTICSTM, São Carlos, Brazil). Before every laser irradiation, the power output was confirmed through a power meter (Laser Check, MMOptics, São Carlos, Brazil).
Before any clinical intervention, the patients were instructed to report initial pain (T0). Each patient pain level (spontaneous pain) was recorded before the initiation of each treatment procedure using a VAS score (0–10 scale: 0, no pain; 10, extremely severe pain) [14]. After the initial pain report, the patients were submitted to respective treatment according to the group allocation. Post-treatment pain levels were recorded immediately after treatment (T1) and 15 min later (T2). After that, local anesthesia was performed by the same operator using 2 % mepivacaine with epinephrine 1:100.000 (Mepinor®, DFL, Brazil), and emergency endodontic treatment was executed. The requirement of complimentary local anesthesia during emergency endodontic treatment was evaluated.
Statistical analysis
The pain score among the experimental groups was analyzed using a nonparametric Kruskal-Wallis analysis. Dunn’s test was used for multiple comparisons. The differences in the need of complimentary anesthesia between the groups were statistically analyzed using a nonparametric Chi-squared test. Separate analyses of the upper and lower teeth regarding the need of complimentary anesthesia were performed using Fisher test. The level of significance was set at 5 %.
Results
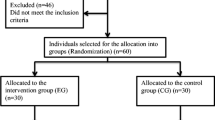
A flow chart of the progress of this randomized placebo-blind study, according to the CONSORT statement, is included (Fig. 1) [15]. The baseline characteristics from the 60 patients (60 teeth) enrolled in this study is given in Table 1.
The preliminary statistical analysis confirmed no evidence of selection bias in terms of the treatment group assignment. There was no statistical difference regarding the initial pain (T0) reported between the groups (p = 0.5445).
Pain reported in T1 and T2
In T1, the group 2 (placebo), group 3 (4 J/cm2), and group 4 (40 J/cm2) presented significant pain reduction in comparison to the group 1 (control group). However, all the laser groups (groups 3 and 4 that applied 4 and 40 J/cm2, respectively) did not present difference in comparison to the group 2 (placebo) (Table 2). In T2, the group 2 (placebo) and group 3 (4 J/cm2) presented significant pain reduction in comparison to the group 1 (control group). All the laser groups (groups 3 and 4 that applied 4 and 40 J/cm2, respectively) did not present difference in comparison to the placebo group (Table 2).
Need of complementary anesthesia
During emergency endodontic treatment, the need of complementary anesthesia was assessed. Analysis of the need of complementary anesthesia in all the teeth (no distinction regarding upper and lower jaw teeth) has shown that laser irradiation at 4 J/cm2 (group 3) presented a significant increase in the requirement of complementary anesthesia (p = 0.028). The other groups did not show significant difference. The separate analysis of the upper jaw teeth did not show any significant difference regarding the need of complementary anesthesia (p = 0.701). The separate analysis of lower jaw teeth has shown that laser irradiation at 4 J/cm2 (group 3) presented a significant increase in the requirement of complementary anesthesia (p = 0.023). The percentage of complementary anesthesia required in lower jaw teeth is illustrated in Fig. 2.
Discussion
Laser phototherapy (LPT) has been shown benefits on pain relief, regardless of its etiology [2]. In acute pain, LPT has shown properties in inflammatory process modulation in a dose-dependent manner [16]. In symptomatic irreversible pulpitis (SIP), however, the effect of LPT is not known. The pain of SIP is generally severe and acute, leading patients to seek treatment as quickly as possible [17]. Because of the high sensitivity of the inflamed vital pulp, in SIP, it cannot always obtain a satisfactory anesthetic effect, which would make sometimes neither patient nor clinician confident and comfortable with the treatment [18]. In some cases of SIP, failure of inferior alveolar nerve block can be detected. It has been reported in clinical studies that failure of inferior alveolar nerve block happens between 44 and 81 % of patients with SIP [19–24]. The control of pain, anxiety, and fear is important step for a successful SIP treatment [25].
Some theories describe that LPT leads pain relief through the modulation of inflammatory mediators, reducing the levels of PGE2 and inhibiting COX [6, 7]. As prostaglandins are one of a vast arrays of inflammatory mediators found in the dental pulp in patients experiencing SIP [26], it would be expected that LPT could modulate acute dental pain. In addition, it has been postulated that LPT induces athermal photochemical reactions that modulate nerve transmission, thereby altering the pain threshold of nociceptors [27]. There are also evidences that LPT enhances the release of endorphins [28]. So, considering LPT properties, if effective in SIP, it would be suggested as an additional therapeutic tool in the emergency endodontic treatment through pain modulation, and consequently indirect control of anxiety and fear. However, the present study did not detect a positive outcome of LPT in pain modulation. The results found showed a high standard deviation. As pain is a subjective experience, a high standard deviation in the results could be expected. This study was conducted between February 2013 and October 2014, and between this period, 60 patients could be selected for the study (n = 15). One limitation of the study was the sample size and high standard deviation found.
Another effect of LPT described in literature in several tissues is the increase of local microcirculation, thereby reducing pain and swelling [2]. Considering etiology and anatomical characteristics that influence SIP, it would be expected that the increase of blow flow would cause an immediate increase of pain, once the increase blood flow would enhance the pressure inside the pulp chamber. However, the present study did not detect any outcome of LPT regarding increase of spontaneous pain. The negative outcome detected after LPT in the present study was related to anesthetic failure. After LPT at 4 J/cm2, a significant increase in anesthetic failure was detected.
Among several theories that describe the possible reasons of anesthetic failure in SIP are the lower tissue pH present in inflammation and infection, anatomic variation, tachyphylaxis of anesthetic solution [17], and the most readily acceptable reason, which is the activation of nociceptors by inflammation mediated by prostaglandins generated by cyclooxygenase (COX) pathways [17, 29]. Nociceptors could express a tetrodotoxin-resistant class of voltage-gated channels, which are resistant to local anesthetics and sensitive to prostaglandin. This ensures that the voltage-gated channels could not be blocked by inferior alveolar nerve block [17]. Consequently, some studies evaluated the effect of nonsteroidal anti-inflammatory drugs (NSAIDs) that inhibit COX activities and further inhibit the production of prostaglandin on pain, with positive results [17]. However, the adverse effects of NSAIDS cannot be neglected [17], and further studies are need concerning the finding of improving anesthetics in these cases of failure. As LPT can reduce the levels of PGE2 and COX [6, 7], without side effects, an improvement in local anesthetics in case of SIP would be expected, but this effect was not detected in the results found in this clinical trial. On the contrary, a significant increase in anesthetic failure was detected.
In the results found in this study, both fluences tested (4 and 40 J/cm2) at 780 nm wavelength showed an immediately (T1) significant reduction of pain in comparison to the control group. However, the difference was not significant in comparison to the placebo group. In T2, 15 min after LPT, only 4 J/cm2 maintained a significant reduction of pain in comparison to the control group. However, there is also no significant difference in comparison to the placebo group. According to the literature, the magnitude of placebo analgesia is highly variable and depends on several contextual factors [30]. The context of the patients that seek emergency dental treatment in the School of Dentistry, University of São Paulo, involves low socio-economic status meaning they cannot afford a private dental treatment. The patients have been presenting pain for some hours or days, or have already experienced acute dental pain previously. This reflects a patient with anxiety and stress, aiming for pain relief. Placebo analgesia often occurs under conditions wherein subjects want a therapeutic agent to provide pain relief [31]. That is, an individual’s desire for reduction of pain may also directly contribute to subsequent pain relief by providing a need to experience a treatment as effective [31]. The possible mediating role of motivation or desire for relief could indirectly account for the increase in placebo response with the severity of clinical pain [32]. It might also account the observation that placebo responses increase as a function of its duration and severity in experimental pain [31]. In this context, it is to be expected that patients that joined this study experienced severe acute dental pain during hours or days; consequently, they can be considered more susceptible to respond with a placebo analgesic effect when a new therapy is proposed. As a result, in the present study, any LPT effect on SIP could not be detected due to the high placebo effect found.
This study assessed the need of complementary anesthesia during emergency endodontic treatment. LPT at fluence of 4 J/cm2 leads to a significant anesthetic failure in the lower jaw teeth in 100 % of the patients. By this way, it could be suggested that the increased blood flow effect was caused by LPT over sizing other mechanisms, and resulted in an increase in anesthetic failure. A review of literature discussed a possible antianesthetic effect of LPT [33] that could support the results found in the present study. Authors reviewed literature regarding the effect of LPT applied for postoperative pain management [33]. In surgeries, the maximal intensity of pain occurs during the first hours, when the local anesthetic has worn off [33]. Theoretically, postoperative pain control can be increased with the use of a local anesthetic with a more-prolonged action [33]. An antianesthetic effect may block these effects. It is discussed in the publication that LPT improves local circulation and increases vasodilatation; therefore, it would increase the absorption of a local anesthetic agent [33]. Consequently, local anesthesia presented shorter duration, and postoperative pain manifested earlier in comparison to patients that were not submitted to LPT [33]. This effect could also occur in SIP condition in the present study. The improvement of local circulation after LPT could result in the increase of the local anesthetic agent absorption, and therefore, complementary anesthetics were needed. Other study confirmed in vivo the effect of laser (1064-nm Nd:YAG laser) in pulpal blood flow rate increase [34]. According to authors, the pulpal blood flow was strongly influenced immediately after Nd:YAG laser irradiation [34]. Despite the difference in wavelength, the results found in the present could be suggested as a result from increase blood flow circulation in SIP.
In the present study, two different fluences of laser irradiation were tested (4 and 40 J/cm2) at 780 nm wavelength. Most responses of LPT, whether positive or negative, occurred after 4 J/cm2. The use of the fluence of 40 J/cm2 showed minimal tissue answer after irradiation. The higher energy could have inhibited cell activity [16] and consequently could result in less tissue response, whether positive or negative.
Although in this study, no benefit of LPT in SIP was detected with the parameters of 780 nm, 40 mW, 4 J/cm2, and 40 J/cm2, it is important not to rule out any benefit of LPT in inflammation modulation in SIP. In literature, there are few studies investigating the effect of LPT in modulating inflammation in endodontics. A randomized clinical trial showed significant pain reduction and inflammation modulation in symptomatic apical periodontitis using a 1064-nm Nd:YAG laser irradiation inside the root canal in addition to conventional root canal treatment [14]. Considering the wide range of laser wavelengths available and the numerous combinations of possible parameters that can be applied in LPT, further studies should be performed in order to enrich the knowledge regarding inflammation, pulp, pain, and LPT. Additionally, molecular answers after LPT applied in irreversible pulpitis, as decrease PGE2, or detection of blood flow should be studied in order to confirm any hypothesis suggested in this clinical trial. In conclusion, considering the limitations of this study, 780-nm diode laser irradiation at 4 and 40 J/cm2 showed no effect in reducing the pain in SIP in comparison to the placebo group. The fluence of 4 J/cm2 showed a negative effect in local anesthetics, resulting in significant increase need of complementary local anesthesia during emergency endodontic treatment. This work provides unpublished results of the consequence of laser phototherapy application on teeth with symptomatic irreversible pulpitis.
References
Seltzer S, Bender IB, Ziontz M (1963) The dynamics of pulp inflammation: correlations between diagnostic data and actual histologic findings in the pulp. Oral Surg Oral Med Oral Pathol 16:969–977
Fulop AM, Dhimmer S, Deluca JR, Johanson DD, Lenz RV, Patel KB, Douris PC, Enwemeka CS (2010) A meta-analysis of the efficacy of laser phototherapy on pain relief. The clinical journal of pain 26(8):729–736. doi:10.1097/AJP.0b013e3181f09713
Enwemeka CS, Parker JC, Dowdy DS, Harkness EE, Sanford LE, Woodruff LD (2004) The efficacy of low-power lasers in tissue repair and pain control: a meta-analysis study. Photomed Laser Surg 22(4):323–329. doi:10.1089/1549541041797841
Tsuchiya K, Kawatani M, Takeshige C, Sato T, Matsumoto I (1993) Diode laser irradiation selectively diminishes slow component of axonal volleys to dorsal roots from the saphenous nerve in the rat. Neurosci Lett 161 (1):65-68. doi:0304-3940(93)90141-7
Ferreira DM, Zangaro RA, Villaverde AB, Cury Y, Frigo L, Picolo G, Longo I, Barbosa DG (2005) Analgesic effect of He-Ne (632.8 nm) low-level laser therapy on acute inflammatory pain. Photomed Laser Surg 23(2):177–181. doi:10.1089/pho.2005.23.177
Honmura A, Ishii A, Yanase M, Obata J, Haruki E (1993) Analgesic effect of Ga-Al-As diode laser irradiation on hyperalgesia in carrageenin-induced inflammation. Lasers Surg Med 13(4):463–469
Sakurai Y, Yamaguchi M, Abiko Y (2000) Inhibitory effect of low-level laser irradiation on LPS-stimulated prostaglandin E2 production and cyclooxygenase-2 in human gingival fibroblasts. Eur J Oral Sci 108(1):29–34
Sousa LR, Cavalcanti BN, Marques MM (2009) Effect of laser phototherapy on the release of TNF-alpha and MMP-1 by endodontic sealer-stimulated macrophages. Photomed Laser Surg 27 (1):37-42. doi:10.1089/pho.2007.2220
Hagiwara S, Iwasaka H, Hasegawa A, Noguchi T (2008) Pre-Irradiation of blood by gallium aluminum arsenide (830 nm) low-level laser enhances peripheral endogenous opioid analgesia in rats. Anesth Analg 107 (3):1058-1063. doi:107/3/1058
Braverman B, McCarthy RJ, Ivankovich AD, Forde DE, Overfield M, Bapna MS (1989) Effect of helium-neon and infrared laser irradiation on wound healing in rabbits. Lasers Surg Med 9(1):50–58
Mester E, Spiry T, Szende B, Tota JG (1971) Effect of laser rays on wound healing. Am J Surg 122 (4):532-535. doi:0002-9610(71)90482-X
Maegawa Y, Itoh T, Hosokawa T, Yaegashi K, Nishi M (2000) Effects of near-infrared low-level laser irradiation on microcirculation. Lasers Surg Med 27(5):427–437. doi:10.1002/1096-9101(2000)27:5<427::AID-LSM1004>3.0.CO;2-A
Urbaniak GC, Plous S (2013) Research Randomizer (Version 4.0) [Computer software]. Retrieved on June 22, 2013, from http://www.randomizer.org/
Yoo YJ, Shon WJ, Baek SH, Kang MK, Kim HC, Lee W (2014) Effect of 1440-nanometer neodymium:yttrium-aluminum-garnet laser irradiation on pain and neuropeptide reduction: a randomized prospective clinical trial. J Endod 40 (1):28-32
Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 63 (8):834-840
Bjordal JM, Johnson MI, Iversen V, Aimbire F, Lopes-Martins RA (2006) Low-level laser therapy in acute pain: a systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials. Photomed Laser Surg 24(2):158–168. doi:10.1089/pho.2006.24.158
Li C, Yang X, Ma X, Li L, Shi Z (2012) Preoperative oral nonsteroidal anti-inflammatory drugs for the success of the inferior alveolar nerve block in irreversible pulpitis treatment: a systematic review and meta-analysis based on randomized controlled trials. Quintessence Int 43 (3):209-219. doi:22758
Hargreaves KM, Keiser K (2002) Local anesthetic failure in endodontics: mechanisms and management. Endod Top 1(1):26–33
Bigby J, Reader A, Nusstein J, Beck M (2007) Anesthetic efficacy of lidocaine/meperidine for inferior alveolar nerve blocks in patients with irreversible pulpitis. J Endod 33 (1):7-10. doi:S0099-2399(06)00810-7
Claffey E, Reader A, Nusstein J, Beck M, Weaver J (2004) Anesthetic efficacy of articaine for inferior alveolar nerve blocks in patients with irreversible pulpitis. J Endod 30 (8):568-571. doi:00004770-200408000-00002
Cohen HP, Cha BY, Spangberg LS (1993) Endodontic anesthesia in mandibular molars: a clinical study. J Endod 19 (7):370-373. doi:S0099-2399(06)81366-X
Lindemann M, Reader A, Nusstein J, Drum M, Beck M (2008) Effect of sublingual triazolam on the success of inferior alveolar nerve block in patients with irreversible pulpitis. Journal of endodontics 34(10):1167–1170. doi:10.1016/j.joen.2008.07.013
Sampaio RM, Carnaval TG, Lanfredi CB, Horliana AC, Rocha RG, Tortamano IP (2012) Comparison of the anesthetic efficacy between bupivacaine and lidocaine in patients with irreversible pulpitis of mandibular molar. J Endod 38 (5):594-597
Tortamano IP, Siviero M, Costa CG, Buscariolo IA, Armonia PL (2009) A comparison of the anesthetic efficacy of articaine and lidocaine in patients with irreversible pulpitis. J Endod 35 (2):165-168
Jeske AH (2002) Selecting new drugs for pain control: evidence-based decisions or clinical impressions? J Am Dent Assoc 133 (8):1052-1056; quiz 1093-1054
Cohen JS, Reader A, Fertel R, Beck M, Meyers WJ (1985) A radioimmunoassay determination of the concentrations of prostaglandins E2 and F2alpha in painful and asymptomatic human dental pulps. J Endod 11(8):330–335
Walker J (1983) Relief from chronic pain by low power laser irradiation. Neurosci Lett 43(2-3):339–344
Gibson KF, Kernohan WG (1993) Lasers in medicine—a review. J Med Eng Technol 17(2):51–57
Aggarwal V, Singla M, Kabi D (2010) Comparative evaluation of effect of preoperative oral medication of ibuprofen and ketorolac on anesthetic efficacy of inferior alveolar nerve block with lidocaine in patients with irreversible pulpitis: a prospective, double-blind, randomized clinical trial. J Endod 36 (3):375-378
Vase L, Riley JL, 3rd, Price DD (2002) A comparison of placebo effects in clinical analgesic trials versus studies of placebo analgesia. Pain 99 (3):443-452
Price DD, Milling LS, Kirsch I, Duff A, Montgomery GH, Nicholls SS (1999) An analysis of factors that contribute to the magnitude of placebo analgesia in an experimental paradigm. Pain 83 (2):147-156
Beecher HK (1955) The powerful placebo. J Am Med Assoc 159(17):1602–1606
Aras MH, Omezli MM, Gungormus M (2010) Does low-level laser therapy have an antianesthetic effect? A review. Photomed Laser Surg 28(6):719–722. doi:10.1089/pho.2008.2430
Yamaguchi H, Kobayashi K, Sato Y, Osada R, Sakuraba E, Nomura T, Arai T, Nakamura J, Cox CF (2000) Nd:YAG laser irradiation of the human dental pulp: implications as a predictor of pulp hemodynamics. Lasers Surg Med 26 (3):270-276. doi:10.1002/(SICI)1096-9101(2000)26:3<270::AID-LSM4>3.0.CO;2-9
Acknowledgments
This study was supported by grants from the State of São Paulo Research Foundation (FAPESP) (# 2012/21670-1; #2013/12317-9).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval and informed consent
This clinical trial was approved by the ethical committee of the School of Dentistry, University of Sao Paulo (#.08509912.3.0000.0075). Each patient signed a written informed consent to participate in the study, which was registered within ClinicalTrials.gov (NCT02169102).
Conflict of interest
The authors declare that they have no conflict of interest.
Role of funding source
Research grants from the State of São Paulo Research Foundation (FAPESP) # 2012/21670-1 (undergraduate grant); #2013/12317-9 (postdoctoral grant).
Rights and permissions
About this article
Cite this article
Ramalho, K.M., de Souza, L.M.P., Tortamano, I.P. et al. A randomized placebo-blind study of the effect of low power laser on pain caused by irreversible pulpitis. Lasers Med Sci 31, 1899–1905 (2016). https://doi.org/10.1007/s10103-016-2068-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-016-2068-7