Abstract
Purpose
To describe the long-term effects of an ASP among febrile neutropenia (FN) patients.
Methods
A quasi-experimental study was conducted between 2015 and 2023 at a tertiary care hospital in Istanbul, Türkiye. The ASP was implemented for FN patients, and the effects were assessed before and after the ASP interventions, which included FN clinical pathways and regular multi-disciplinary meetings with relevant healthcare workers.
Results
A total of 489 FN episodes of 290 patients were included, 42% were female, and the mean age was 56 years (SD: 15, range: 18–89 years). After the intervention, the rate of appropriate antimicrobial therapy at the levels of starting (p = 0.005), switching (p < 0.001), and de-escalation/discontinuation, (p < 0.001) significantly increased. Another positive impact of the ASP was a significant reduction in candidemia (from 4.88 to 0.74, p = 0.004), as well as a significant reduction in the 90-day mortality rate (from 19 to 5%, p < 0.001). In multivariate analysis, having a gram-negative bloodstream infection, prolonged days with fever, and a high risk for neutropenia were found to be significant predictors of 90-day mortality, while follow-up with ASP significantly reduced mortality.
Conclusion
Implementation of ASP led to reduced candidemia and LOS without increasing mortality, even in a country with a high rate of antimicrobial resistance. Implementation of sustainable ASP for FN patients is critical in combating antimicrobial resistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Febrile neutropenia (FN) remains a significant and challenging complication in patients undergoing chemotherapy, despite remarkable advancements in prevention and treatment modalities. This clinical condition can affect up to 30% of cancer patients [1], with varying rates of occurrence ranging from 10 to 50% in solid tumour cases and up to 80% in patients with haematological malignancies [2, 3]. Emerging resistance to antimicrobials increases the burden of infections among FN patients in addition to well-defined features such as prolonged hospital stays (6–10 days), increased cost, higher morbidity and mortality (> 20% in 30 days) risks [4,5,6,7]. Unnecessary antibiotic consumption not only raises antimicrobial resistance but also leads to adverse drug events, allergic reactions, nephrotoxicity, prolonged hospital stays, and additional costs [8,9,10].
Using unnecessary antibiotics is an important driving parameter for emerging resistance, especially among patients with FN [8, 11]. In countries where antimicrobial resistance (AMR) is high such as Türkiye [12, 13], the approach to managing patients with FN further increases the importance of the problem. To address this, we initiated an antimicrobial stewardship program (ASP) designed to manage all FN patients with a uniform protocol aligned with current guidelines [2, 10, 14, 15]. Although the necessity of ASP is known, their acceptance, clinical application and particularly long-term implementation might be lacking among physicians, therefore stronger evidence of their beneficial use should be presented to convince the implementation of the ASP.
We aimed to assess the long-term effects of the ASP on the rate of appropriate antimicrobial use, laboratory and clinical outcomes of patients, the length of hospital stay (LOS) and mortality rate. Our results will shed light on the challenge of the management of FN patients in countries with high AMR.
Methods
Ethical approval
The ethical approval for this study was obtained from the Institutional Review Board of Koç University with reference number 2023.164.IRB1.054.
Study population
This study was conducted at a hospital in Istanbul, Türkiye, with a bed capacity of 300. The study included all inpatients aged 18 and above, admitted to the haematology and oncology departments, and diagnosed with febrile neutropenia (FN). The study assessed the outcomes before (from January 1, 2015, to December 31, 2015) and after (from January 1, 2016, to June 30, 2023) the implementation of the ASP interventions.
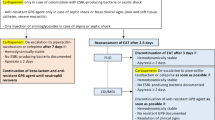
Implementation of the ASP
The ASP was developed by the Antimicrobial Stewardship Team (AST) at the end of 2015. There was no protocol before 2015. The practice of antibiotic selection changed from one physician to another, since there was no systematic approach. “Febrile Neutropenia Clinical Pathway” based on international guidelines was established to define the program’s scope and provide clear recommendations for healthcare workers (Supplement 1). Regular weekly department meetings were held, involving physicians, nurses, and technicians from the Hematology, Oncology, Clinical Microbiology, and Infectious Diseases Departments. During these meetings, the details of the FN clinical pathway were shared, and the AST team was responsible for overseeing, educating, and monitoring the various phases of the clinical pathway.
Data collection
Data on inpatients with FN were collected using a daily electronic system. The surveillance and monitoring of the clinical pathway were conducted by the AST. Inappropriate practices identified through data analysis were discussed during the weekly department meetings, and the initial results of the data analysis were shared with the relevant departments every quarter.
Definitions
Febrile neutropenia refers to the occurrence of fever during a period of severe neutropenia, a condition characterized by a low level of neutrophils in the blood. In this study, the definition of febrile neutropenia is based on the guidelines of the Infectious Diseases Society of America (IDSA) and the National Comprehensive Cancer Network (NCCN). Fever was defined as a single oral temperature > 38.3 °C or > 38.0 °C sustained over 1 h. Neutropenia was defined as an absolute neutrophil count (ANC) of less than 500 neutrophils/mcL, or a predicted decline to less than 500 neutrophils/mcL within the next 48 h [16].
The risk of an FN episode was assessed using the Multinational Association for Supportive Care in Cancer (MASCC) scoring system. Developed in 2000, the MASCC scoring table assigns a maximum of 26 points, with higher scores indicating a lower risk of complications from FN. Patients with a score of ≥ 21 are categorized as having low-risk FN episodes, while those with < 21 points are considered to have high risk [4].
The appropriateness of antimicrobial consumption among FN patients was evaluated based on the “Febrile Neutropenia Clinical Pathway” (Supplement 1). This evaluation consists of three phases: 1) Appropriate antimicrobial agent choice, 2) Appropriate de-escalation or switch therapy if needed, and 3) Appropriate continuation or discontinuation of antimicrobials which were clearly defined in the clinical pathway. The endpoints were length of stay, duration of days with FN, duration of days with fever, and 90-day mortality.
Fluoroquinolones prophylaxis have been used among patients at high risk of febrile neutropenia or profound, protracted neutropenia during the period of expected neutropenia [17].
Ceftazidim-avibactam has been used in Türkiye since 2020. Since then ceftazidim-avibactam susceptibility test has been performed routinely among Klebsiella pneumonia, Pseudomonas aeruginosa and E. coli strains once carbapenem resistance was detected.
Statistical analysis
Continuous variables were analyzed using independent group t-tests to compare means, while categorical variables were assessed using chi-square tests to compare proportions. To determine the improvement in antimicrobial consumption after the implementation of the ASP, multivariate analyses and logistic regression analyses were performed. The independent variables included in the analysis were gram-negative, gram-positive, and candida infections, LOS, high risk of FN episode (MASCC score < 21), duration of FN episode days, and appropriateness of antimicrobial use. Significance was set at p < 0.05 for two-sided comparisons. The statistical analyses were performed by Stata, version 15.0.
Results
A total of 489 febrile neutropenia (FN) episodes were included in the study, involving 290 inpatients from the haematology and oncology departments. Data were collected for two distinct periods: before the implementation of the ASP from January 1, 2015, to December 31, 2015 (82 FN episodes among 50 inpatients with FN), and after the ASP interventions from January 1, 2016, to June 30, 2023 (407 FN episodes among 240 inpatients with FN).
Fourty-two per cent (n = 128) of the patients who had an FN episode were female, with the mean age being 56 years (SD: 15, Range: 18–89 years). Remarkably, 36% of the patients had additional chronic disease (n = 175), and 69% of all FN episodes (n = 336) were classified as “high risk” based on the Multinational Association for Supportive Care in Cancer (MASCC) score. Regarding the distribution of diagnoses, 46% of patients had leukaemia, 24% had lymphoma, 17% had solid tumours or cancer, 8% had multiple myeloma, and 5% were diagnosed with other chronic illnesses. Before and after the ASP intervention, mean age (p = 0.287), gender (p = 0.976), rate of patients with additional comorbidity (p = 0.093), and rate of high-risk FN patients (p = 0.070) were similar (Table 1). The rate of leukaemia patients was higher in the pre-ASP period than in the post-ASP period (p = 0.005, Table 1).
During the study period, the implementation of the local FN clinical pathway resulted in a significant increase in the rate of appropriate empirical therapy (step 1, from 76 to 88%, p = 0.005), appropriate switching (step 2, from 51 to 90%, p < 0.001), and appropriate resuming of antibiotics (step 3, from 69 to 92%, p < 0.001) among FN patients (Table 2). After the implementation of the ASP, there was a significant decrease in the average LOS at the hospital from 20.17 days to 15.13 days (p = 0.035), the average duration of fever decreased from 5.09 days to 3.90 days (p = 0.036), the average duration of FN episode days decreased from 4.74 days to 3.52 days (p = 0.022), and finally 90-day mortality rate significantly decreased from 19% (n = 16) to 5% (n = 22) (p < 0.001) (Table 1).
After the implementation of the ASP, there was a significant decrease in the rate of candidemia (from 4.88 to 0.74, p = 0.004) (Table 3). However, the decline in the rate of gram-positive bacterial infections (from 18.29 to 14.74%, p = 0.416) and gram-negative bacterial infections (from 15.85 to 12.04%, p = 0.344) was not statistically significant. Additionally, there was an increase in the rate of methicillin resistance of Staphylococci isolates (from 53.33 to 66.67%, p = 0.342) (Table 3). The carbapenem resistance rate among Klebsiella pneumoniae and Pseudomonas aeruginosa was 66% (2/3) pre-ASP and 23% (5/22) post-ASP period (p = 0.826). Among Escherichia coli strains there was no carbapenem resistance. Colistin resistance has not been detected among gram-negative bacteria during the study period and one ceftazidime-avibactam strain was detected in K. pneumoniae in the post-ASP period.
In multivariate analysis, prolonged days with fever (95% CI:1.03–1.15, OR:1.09, p = 0.001), and having gram-negative bloodstream infections (95% CI:1.22–7.58, OR:3.053, p = 0.016) increased mortality, while having a low risky (MASCC ≥ 21) score (95% CI:0.79–0.94, OR:0.862, p = 0.001) and being followed up with ASP (95% CI:0.12–0.66, OR:0.292, p = 0.003) were significantly associated with a decrease in mortality rate in the last 90-day months (Table 4).
Discussion
We present the beneficial impact of the long-term ASP among patients with FN in a country with a high AMR rate among gram-negative bacterial infections. Compared to our previous study in the same centre [18], long-term follow-up allowed us to detect a significant change in mortality, LOS, duration of days with fever, and a decrease in Candida infections. The mortality rate (90-day) in our study decreased from 19 to 5% after the implementation of ASP. In multivariate analysis, implementation of ASP (95% CI:0.12–0.66, OR:0.292) significantly reduced the mortality, in a setting where gram-negative bloodstream infections have a significant impact on mortality (95% CI:1.22–7.58, OR:3.053, Table 4). Contejean et al. reported that the implementation of ASP decreased the 30-day mortality rate among FN patients (post-intervention period: odds-ratio = 0.29, 95% CI: 0.15–0.53) [19]. In our analysis, it was found that the number of days with fever had an impact on the 90-day mortality rate. Hosiriluck et al. also found that a fever duration of more than four days independent risk factor for 30-day mortality [20]. Akova et al. proved that the duration of hospitalization days before the FN episodes, gram-negative infections, sepsis, and inappropriate antimicrobial prophylaxis were found as predictive factors for 30-day mortality [21].
Another significant finding was the reduction in Candidemia (4.88% vs. 0.74%). After the implementation of ASP, the selection of appropriate empiric antibiotics increased from 76 to 88%, appropriate switching therapy increased from 51 to 90%, and the resuming of appropriate therapy from 69 to 92%. Besides the ASP implementation, improvement in infection control measures [22, 23], and implementation of clinical pathways [18] could also account for this progress. In a study with similar findings, Contejean et al. reported a parallel decrease in antimicrobial consumption among FN patients following the implementation of an ASP (post-intervention period: odds-ratio = 0.29, 95% CI: 0.15–0.53) [19]. However, Martire et al. demonstrated a reduction in antibiotic consumption without a proven effect on bacteremia and mortality rates [24]. Verlinden et al. proved that reduced antibiotic consumption through ASP interventions did not result in increased infection complications [25]. Keck et al. suggested that rapid de-escalation of therapy may reduce the adverse effects and cost without compromising clinical outcomes [9].
Among the most compelling results of this study are the significant reductions in LOS (20.17 vs. 15.13), the number of days with fever (from 5.09 to 3.90 days) and the number of days with FN episodes (from 4.74 to 3.52 days) following the implementation of the ASP. Pickard et al. reported a reduction in total antibiotic duration (8.7 vs. 3.2) and LOS (13.2 vs. 6.1) among FN patients with an effective planned ASP. Another study by Itoh et al. also claims that the ASP can reduce carbapenem use without negative effects on patients [26].
Another contribution of our findings is to show the association between antimicrobial consumption and resistance. Despite the increasing level of resistance in our region for seven and a half-year period, the rate of appropriate use increased, it has been observed that the gram-negative and positive agents decreased in blood cultures. Despite the rate of colistin and ceftazidime avibactam resistance varying up to 39% among P. aeruginosa and K. pneumoniae isolates in our country [13, 27], we did not detect any colistin-resistant isolates and only one ceftazidime avibactam-resistant agent was detected among FN patients during the study period. We think that our significantly low rate of resistance rate is associated with stringent practice of infection control measures and antimicrobial stewardship measures by a vigilant team.
One of the strongest features of this study was 8 years of follow-up so that we demonstrated the significant impact on mortality more clearly than our previous study in 2018, which focused on 152 FN episodes in 17 months [18]. There are some limitations in this research. Firstly, it was conducted in a single centre. The rate of leukemia patients were higher in the pre-ASP period than the post-ASP period (Tables 1 and 60% vs. 43%, p = 0.005), however the fatality rates among leukemia patients versus non-leukemia patients were similar in pre-ASP (18% vs. 21%, p = 0.839) and post-ASP periods (5.1% vs. 5.6%, p = 0.839). Thirdly, the study spanned over seven years, during which changes in mindset and potential maturity bias could have influenced outcomes positively. Another limitation was related to the MASCC score, since there were changes in some of the parameters such as definition of neutropenia. However despite all these caveats and inconsistencies in the results of the validation studies, the MASCC tool continues to be endorsed by many cancer care guidelines [28].
In conclusion, we demonstrated that in a high prevalence of MDR gram-negative bacterial infections, the appropriate use of antimicrobials significantly increased with the implementation of ASP, leading to a reduction in candidemia and LOS without increasing mortality rates. Sustainability of antimicrobial stewardship programs is critical in combating antimicrobial resistance.
Data availability
No datasets were generated or analysed during the current study.
References
Baus CJ et al (2023) Neutropenic Fever-Associated admissions among patients with solid tumors receiving Chemotherapy during the COVID-19 pandemic. JAMA Netw Open 6(3):e234881
Freifeld AG et al (2011) Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of America. Clin Infect Dis 52(4):e56–93
Rasmy AA, Fotih A, Selwi S (2016) Febrile neutropenia in cancer patient: epidemiology, microbiology, pathophysiology and management. J Cancer Prev Curr Res 5(3):273–278
Klastersky J et al (2000) The Multinational Association for Supportive Care in Cancer risk index: a multinational scoring system for identifying low-risk febrile neutropenic cancer patients. J Clin Oncol 18(16):3038–3051
Tai E et al (2017) Cost of Cancer-related Neutropenia or Fever hospitalizations, United States, 2012. J Oncol Pract 13(6):e552–e561
Hosiriluck N et al (2015) Prognostic factors for mortality with febrile neutropenia in hospitalized patients. Southwest Respiratory Clin Care Chronicles, 3(9)
Boccia R et al (2022) Chemotherapy-Induced Neutropenia and Febrile Neutropenia in the US: a Beast of Burden that needs to be tamed? Oncologist 27(8):625–636
Ishikawa K et al (2023) Systematic review of the short-term versus long-term duration of Antibiotic Management for Neutropenic Fever in patients with Cancer. Cancers (Basel), 15(5)
Keck JM et al (2022) Approach to fever in patients with neutropenia: a review of diagnosis and management. Ther Adv Infect Dis 9:20499361221138346
Averbuch D et al (2013) European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance: summary of the 2011 4th European conference on infections in Leukemia. Haematologica 98(12):1826–1835
Nesher L, Rolston KV (2014) The current spectrum of infection in cancer patients with chemotherapy related neutropenia. Infection 42(1):5–13
Isler B et al (2019) Antibiotic overconsumption and resistance in Turkey. Clin Microbiol Infect 25(6):651–653
Pınarlık F, Gücer LS, Boral J, Ekinci G, Cooper FK, Ataç N (2023) Klebsiella pneumoniae: surveillance of antimicrobial resistance, clinical and molecular characteristics. ; https://elibrary.escmid.org/?search%5Bfrom%5D=0&search%5Bquery%5D=PİNARLIK&search%5Bdate%5D=#results
Taplitz RA et al (2018) Outpatient Management of Fever and Neutropenia in adults treated for malignancy: American Society of Clinical Oncology and Infectious Diseases Society of America Clinical Practice Guideline Update. J Clin Oncol 36(14):1443–1453
Crawford J et al (2017) NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 15(12):1520–1541
Baden LR et al (2012) Prevention and treatment of cancer-related infections. J Natl Compr Canc Netw 10(11):1412–1445
Flowers CR et al (2013) Antimicrobial prophylaxis and outpatient management of fever and neutropenia in adults treated for malignancy: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 31(6):794–810
Madran B et al (2018) Implementation of an antimicrobial stewardship program for patients with febrile neutropenia. Am J Infect Control 46(4):420–424
Contejean A et al (2022) Antimicrobial stewardship in high-risk febrile neutropenia patients. Antimicrob Resist Infect Control 11(1):52
Hosiriluck N, Saranapoom K, Rassameehiran S, Sutamtewagul G, Tijani L, Radhi S (2015) Prognostic factors for mortality with febrile neutropenia in hospitalized patients, vol 3. The Southwest Respiratory and Critical Care Chronicles, 9
Ayaz CM, Hazırolan G, Sancak B, Hasçelik G, Akova M (2022) Factors associated with gram-negative bacteremia and mortality in neutropenic patients with haematologic malignancies in a high-resistance setting. Infect Disease Clin Microbiol 4(2):87–98
Ergonul O et al (2022) Elimination of healthcare-associated Acinetobacter baumannii infection in a highly endemic region. Int J Infect Dis 114:11–14
Keske Ş (2019) The significance of Multidirectional Studies in Control of Health Care-Associated Infections. KLIMIK J 32(2):190–194
la Martire G et al (2018) De-escalation and discontinuation strategies in high-risk neutropenic patients: an interrupted time series analyses of antimicrobial consumption and impact on outcome. Eur J Clin Microbiol Infect Dis 37(10):1931–1940
Verlinden A et al (2022) Safety and efficacy of antibiotic de-escalation and discontinuation in high-risk hematological patients with febrile Neutropenia: a single-center experience. Open Forum Infect Dis 9(3):ofab624
Itoh N et al (2022) Effects of infectious disease consultation and antimicrobial stewardship program at a Japanese cancer center: an interrupted time-series analysis. PLoS ONE 17(1):e0263095
Pınarlık F, Gücer LS, Boral J, Ekinci G, Cooper FK, Ataç N (2023) The molecular characteristics of carbapenem resistant pseudomonas aeruginosa. [cited 2024; https://elibrary.escmid.org/?search%5Bfrom%5D=0&search%5Bquery%5D=PİNARLIK&search%5Bdate%5D=#results
Wijeratne DT, Wright K, Gyawali B (2021) Risk-stratifying treatment strategies for Febrile Neutropenia-Tools, Tools everywhere, and not a single one that works? JCO Oncol Pract 17(11):651–654
Acknowledgements
We thank the hospital administration of the American Hospital for their continuous support.
Author information
Authors and Affiliations
Contributions
B.M., S.K.: Collected data, designed the analysis, wrote the main manuscript.N.M.M., B.F. and Ö.E.: Edited the manuscript, contributed data or analysis tool.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Madran, B., Keske, Ş., Ferhanoğlu, B. et al. The long-term impact of an antimicrobial stewardship program in febrile neutropenia: an 8 years follow up. Eur J Clin Microbiol Infect Dis (2024). https://doi.org/10.1007/s10096-024-04939-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10096-024-04939-z