Abstract
Acute kidney injury (AKI) is a frequent complication in patients with Staphylococcus aureus bacteremia (SAB), with a significant impact on patient management and outcome. This study aimed to provide insight in the proportion of patients with SAB that develop AKI, the risk factors for developing AKI in this population, and its reversibility. In this retrospective, multicenter cohort study, adult patients with SAB were eligible for inclusion. Patient characteristics, clinical variables, and laboratory results were retrieved from the electronic patient files. Primary outcome was development of AKI, defined as 1.5 times baseline creatinine. Secondary outcomes were reversibility of AKI and risk factors for AKI. A total of 315 patients with SAB were included, of whom 115/315 (37%) developed acute kidney injury. In 68/115 (59%), the AKI was reversible. If kidney function recovered, this occurred within 7 days in 56/68 (82%) of patients. In multivariable logistic regression analyses, independent risk factors for AKI were as follows: complicated SAB, use of diuretics, and hemodynamic instability. Development of AKI was associated with 30-day mortality (OR 3.9; CI 2.2–6.9; p < 0.01). Acute kidney injury is a frequent complication in patients with Staphylococcus aureus bacteremia. Considering the irreversibility in a relevant proportion of patients, future research into the underlying pathophysiology and potential interventions is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Staphylococcus aureus is a major cause of bloodstream infections and is associated with high morbidity and mortality rates [1, 2]. Acute kidney injury (AKI) is a frequent complication in patients with Staphylococcus aureus bacteremia (SAB), with a significant impact on patient management and outcome [3, 4]. The etiology of AKI in SAB is diverse, including prerenal, toxic/drug-related, immune-mediated, tubulointerstitial nephritis (TIN), acute tubular necrosis (ATN), and postrenal pathophysiology.
Despite the fact that acute kidney injury in patients with SAB is common, little is known about the proportion of patients with SAB that develop AKI, the risk factors for developing AKI in these patients, and its reversibility.
The SAB patient population is heterogeneous, and the disease course varies greatly, from transient bacteremia in uncomplicated SAB to widespread infection and metastatic disease in complicated SAB [5]. Although likely on theoretical grounds, it is unknown whether the incidence, etiology, and outcome of AKI differ between complicated and uncomplicated SAB [6].
The aim of this study was to investigate the incidence of AKI in SAB, its reversibility, the risk factors for the development of AKI, and differences in disease course between complicated and uncomplicated SAB. Additional knowledge of AKI in SAB may provide clinicians tools to predict risk of AKI in individual patients and support diagnostic and therapeutic management. Eventually, it could lead to initiation of intervention studies aimed at prevention or treatment of AKI in patients with SAB.
Methods
Study population
This multicenter retrospective cohort study was performed in one academic and two large teaching hospitals in the Netherlands. Patients that were diagnosed with SAB in the period January 2013 to December 2017 were eligible for inclusion. Data on this study cohort have been published previously [7].
All consecutive adult patients (≥ 18 years) with ≥ 1 blood culture positive for S. aureus were eligible for inclusion. Patients were excluded if (a) S. aureus was detected simultaneously with other pathogens (polymicrobial culture), (b) patients were already on renal dialysis before admission, (c) and AKI occurred prior to the episode of SAB. In patients with multiple episodes of SAB, only the first episode was included. Both patients with community acquired SAB and patients who developed SAB during hospitalization for another indication (hospital acquired SAB) were eligible for inclusion.
Data collection
Blood samples were inoculated in both anaerobic and aerobic bottles and incubated in the BACTEC FX continuous monitoring system (Becton Dickinson BV, Breda, The Netherlands).
The clinical data were obtained through review of the electronic patient files. The following data were collected: demographic data, medical history, chronic medication, antibiotic therapy administered for treatment of the SAB episode, vital parameters, and the presence of complicated versus uncomplicated SAB.
Baseline serum creatinine (µmol/L), i.e., the most recent known serum creatinine before the presentation with SAB, creatinine at presentation, and maximum creatinine during admission were retrieved from the electronic laboratory system. Furthermore, the time to maximum serum creatinine and the time from maximum creatine to recovery of creatinine were retrieved.
Definitions
Acute kidney injury was defined as 1.5 times baseline creatinine. Recovery of kidney function was defined as creatinine returning to below 1.5 times baseline creatinine during follow-up. The absence of recovery of renal function < 1.5 times baseline creatinine during follow-up was considered non-reversible AKI. Hemodynamic instability was defined as a mean arterial pressure (MAP) < 65 mmHg or systolic blood pressure < 90 mmHg or need of inotropic or vasopressor agents [8]. Chronic kidney disease was defined as an eGFR < 60 ml/min/1.73 m2. Uncomplicated SAB was defined as an episode of bacteremia with ≥ 1 blood culture with Staphylococcus aureus, without evidence of endocarditis/metastatic infection, and without positive cultures after 48 h of adequate therapy and that was treated for a maximum of 2 weeks, and no relapse occurred, and the patient survived > 72 h after presentation. All situations that did not meet the criteria for uncomplicated SAB were considered complicated SAB. Infective endocarditis was defined by the modified Duke’s criteria [9]. Metastatic infection was defined as a clinical and/or radiographical examination and/or culture concordant with vertebral osteomyelitis, epidural abscess, deep tissue abscess (e.g., psoas‐) septic pulmonary or cerebral emboli, arthritis, or meningitis.
Statistical analysis
Data were presented as percentages or proportions for categorical variables and as medians plus interquartile range (IQR) for continuous variables. The overall development of AKI and the recovery of AKI were presented as a rate, with 95% confidence interval (95%CI), and were stratified for complicated and uncomplicated SAB. Cox regression analysis was performed to assess time to development and time to recovery of AKI. Recovery of AKI in patients still alive at day 30 was presented as a rate. Univariate analysis was performed by calculating odds ratio’s (with 95%CI) and using Fisher’s exact tests to identify clinical factors associated with AKI. To assess the correlation of different variables and outcome, a multivariable regression analysis was performed including the variables with p < 0.20 from univariate analysis.
Subgroup analyses of prevalence of AKI and reversibility were also performed on patients with hemodynamic instability at presentation and patients with preexistent chronic kidney disease.
Ethical approval
Ethical approval was granted by the institutional ethical review committee of the Leiden University Medical Center.
Results
In total, 339 patients with SAB were reviewed. Because of prior chronic (long-term) hemodialysis or development of AKI prior to SAB, respectively 14 and 10 patients were excluded, leaving 315 patients eligible for inclusion in this study. The patient characteristics are summarized in Table 1. In 181/315 (58%) of patients, the SAB episode met the criteria for complicated SAB. All of the cultured S. aureus isolates were methicillin-sensitive (MSSA). Overall 30-day mortality was 21% (67/315).
Incidence and severity of AKI
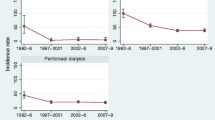
Acute kidney injury developed in 115/315 (37%; 95%CI 31–42%) of all patients. In the majority of patients, the maximum creatinine was between 1.5 and 2.5 times baseline (Table 2). In patients with complicated SAB, AKI was found more frequently (83/181; 46%) compared to patients with uncomplicated SAB (32/134; 24%; p = < 0.01; OR = 2.70; 95%CI 1.65–4.42). Figure 1a depicts the time from first positive blood culture to maximum creatinine in days, in the 115 patients with AKI. In 45/115 (39%) patients, the maximum creatinine was reached on the day of first blood culture sampling. The median time from first positive blood culture to AKI was 3 days (IQR = 0–11 days). Development of AKI during SAB was associated with 30-day mortality (OR 3.9; 95%CI 2.2–6.9; p < 0.01). In the patients with non-reversible AKI, 27/47 (57%) died within 30 days after blood culture sampling.
a Time from blood culture sampling to maximum creatinine in days. b Time from maximum creatinine to recovery of creatinine in days. Legend: a Cox regression of all patients with acute kidney injury. Recovery of kidney function was defined as return of creatinine < 1.5 × baseline creatinine. Both: Uncomplicated SAB was defined as an episode of bacteraemia with ≥ 1 blood culture with Staphylococcus aureus, without evidence of endocarditis/metastatic infection, and without positive cultures after 48 h of adequate therapy and that was treated for a maximum of 2 weeks, and no relapse occurred, and the patient survived > 72 h after presentation. All situations that did not meet the criteria for uncomplicated SAB were considered complicated SAB
Reversibility
Recovery of renal function to < 1.5 times baseline creatinine occurred in 68/115 (59%; 95%CI 49–68%) of patients. There was a small numerical difference in reversibility between complicated and uncomplicated SAB (respectively 60% versus 56%, p = 0.83). The proportion of recovery of AKI was higher in the category of patients with a maximum creatinine of < 2.5 times baseline creatine compared to the more severe kidney injuries (respectively 68% vs 44%, p = 0.02).
In patients with reversible AKI, the median time to recovery was two days (IQR = 1–4 days). In 56/68 (82%; 95%CI 73–92%), the recovery occurred within 7 days (Fig. 1b). Among the patients with persistent renal impairment after 7 days, only 12/59 (20%; 95%CI 11–32%) recovered eventually, after temporary renal replacement therapy in five of them. There was no statistically significant difference in reversibility of AKI between patients who presented with AKI and patient who developed AKI during admission (respectively 64% vs 56%, p = 0.45). In the selection of patients still alive at day 30, the recovery rate within 30 days after SAB onset was 52/71 (72%).
Risk factors for AKI
In the univariate analyses, age > 60 years, complicated SAB, chronic kidney disease, cardiovascular disease, the use of diuretics or ACE-i/ARB, hemodynamic instability, temperature > 38.5˚C, and CRP > 150 mg/L, all at baseline, were associated with development of AKI (Table 3). In the multivariable logistic regression analysis, independent risk factors for AKI were complicated SAB, use of diuretics and hemodynamic instability (Table 3).
Subgroup analyses
In the subgroup of patients presenting with hemodynamic instability (n = 35), 26/35 (74%) developed AKI. In 12/26 (46%) patients, AKI was reversible. In the subgroup of patients with chronic kidney insufficiency (n = 53), 31/53 (59%) developed AKI. In 16/31 (52%), AKI was reversible.
Discussion
The main finding of our study is the high overall incidence of AKI in patients with SAB (37%), particularly in patients with complicated disease. This high incidence, combined with the limited reversibility, illustrates the significance of this complication.
We found that AKI in SAB develops early in most patients. In a high proportion (39%) of patients developing AKI the creatinine level peaked at the day of first positive blood culture. Furthermore, the median time to peak creatinine was 3 days after first positive blood culture. These findings are similar with those reported by Holmes et al. [3]. The slightly higher incidence of AKI in the study by Holmes may be explained by a different definition of AKI. They included low urine output in their definition, whereas our definition was based on serum creatinine alone. Other research on AKI in SAB is limited to studies that were primarily aimed at comparing treatment outcome of different antibiotic therapies. In these studies, the incidence of nephrotoxicity was highly variable, ranging from 2 to 33% [10,11,12,13,14].
Acute kidney injury was reversible in the majority of patients (59%), but a significant proportion of patients suffered from irreversible renal impairment. In patients with reversible AKI, recovery occurred within 7 days after onset in the majority of patients (82%). Persistent kidney injury beyond this time point is prognostically unfavorable. In patients with persistent AKI at T = 7 days, recovery was observed in only 20%. The high proportion of non-reversible AKI in our study may partially be explained by disease severity. The association between disease severity and both the prevalence and the reversibility of AKI has been demonstrated for sepsis-associated kidney injury in general [15, 16]. Several risk factors for the development of AKI were identified in our study. Apart from diagnosis of complicated SAB, the use of diuretics as well as hemodynamic instability at time of admission remained independent risk factors for AKI in multivariable analysis. Together with the time course of renal insufficiency showing early onset and quick recovery, this finding suggests that hemodynamic deterioration early in the disease plays an important role in the development of AKI.
However, the results of our study do not yield definite answers regarding pathophysiology. Toxicity of antibiotics, i.e., nafcillin and aminoglycosides, has been suggested in the literature to be important in development of AKI, although this assumption was not confirmed by kidney biopsies [10,11,12,13,14, 17, 18]. In the current study, the vast majority (86%) of patients was treated with flucloxacillin according to the Dutch guideline, limiting the comparison of different antibiotic therapies on AKI development [19, 20]. However, based on the median time to AKI of 3 days, toxicity caused by antibiotic therapy does not seem to have been a major cause of AKI. For example, TIN on antibiotic therapy is unlikely if the onset is < 5 days after start of antibiotic therapy [21]. Secondly, TIN is unlikely to recover within 1 week. This is relevant, as falsely attributing AKI to beta-lactams may deter a patient from optimal antibiotic treatment.
The current lack of non-invasive diagnostic tools to differentiate between the divergent etiologies of AKI in SAB leads to misdiagnoses that cannot be refuted. Insight in the etiology of AKI in SAB and the probability of different causal mechanisms has important diagnostic and therapeutic consequences and warrants prospective studies, focusing on etiology. Urine biomarkers could possibly be of additional value herein, but still need future research.
An association between occurrence of AKI and 30-day mortality in patients with SAB was previously reported and confirmed in this study [22]. Although causality cannot be determined based on either study, AKI is likely to affect patient outcome on theoretical grounds. Patients with AKI—in general—are at increased future risk of chronic kidney disease and death [23]. The high burden of morbidity and mortality stresses the importance of further studies on AKI in SAB.
An important limitation of our study is the fact that the cause of AKI was rarely proven histologically, limiting insights in the etiology of SAB in our population. The lack of biopsy-confirmed etiologic diagnoses in both our study and previously mentioned studies is a reflection of daily practice, as renal biopsies are rarely performed [10,11,12,13,14, 17, 18]. A second limitation of this study is the retrospective design. Variables that were not measured—such as aminoglycoside therapy— may be associated with the development of AKI in SAB.
In conclusion, this study shows that AKI is common in patients with SAB. The risk factors found, and the swift reversibility in most patients, suggest that a major cause for AKI is hemodynamic in nature. This knowledge may provide insights that support diagnostic and therapeutic management of patients with SAB. Future prospective intervention studies are warranted to evaluate the underlying pathophysiology and potential interventions.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Lam JC, Gregson DB, Robinson S, Somayaji R, Conly JM, Parkins MD (2019) Epidemiology and outcome determinants of Staphylococcus aureus bacteremia revisited: a population-based study. Infection 47(6):961–971
Souli M, Ruffin F, Choi SH, Park LP, Gao S, Lent NC et al (2019) Changing characteristics of Staphylococcus aureus bacteremia: results from a 21-year, prospective, longitudinal study. Clin Infect Dis 69(11):1868–1877
Holmes NE, Robinson JO, van Hal SJ, Munckhof WJ, Athan E, Korman TM et al (2018) Morbidity from in-hospital complications is greater than treatment failure in patients with Staphylococcus aureus bacteraemia. BMC Infect Dis 18(1):107
Tong SYC, Lye DC, Yahav D, Sud A, Robinson JO, Nelson J et al (2020) Effect of vancomycin or daptomycin with vs without an Antistaphylococcal beta-lactam on mortality, bacteremia, relapse, or treatment failure in patients with MRSA bacteremia: a randomized clinical trial. JAMA 323(6):527–537
Holland TL, Arnold C, Fowler VG Jr (2014) Clinical management of Staphylococcus aureus bacteremia: a review. JAMA 312(13):1330–1341
Tong SYC, Lee TC (2020) Staphylococcus aureus bacteraemia: does duration matter? Lancet Infect Dis 20(12):1353–1354
Lambregts MMC, Molendijk EBD, Meziyerh S, Schippers EF, Delfos NM, Leendertse M, et al. Early differentiation between uncomplicated and complicated Staphylococcus aureus bacteraemia: potential value and limitations of a clinical risk score. Int J Clin Pract. 2020:e13601.
Dellinger RP (2003) Cardiovascular management of septic shock. Crit Care Med 31(3):946–955
Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T et al (2000) Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30(4):633–638
Burrelli CC, Broadbent EK, Margulis A, Snyder GM, Gold HS, McCoy C et al (2018) Does the beta-lactam matter? Nafcillin versus cefazolin for methicillin-susceptible Staphylococcus aureus Bloodstream Infections. Chemotherapy 63(6):345–351
Flynt LK, Kenney RM, Zervos MJ, Davis SL (2017) The safety and economic impact of cefazolin versus nafcillin for the treatment of methicillin-susceptible Staphylococcus aureus bloodstream infections. Infect Dis Ther 6(2):225–231
Miller MA, Fish DN, Barber GR, Barron MA, Goolsby TA, Moine P et al (2020) A comparison of safety and outcomes with cefazolin versus nafcillin for methicillin-susceptible Staphylococcus aureus bloodstream infections. J Microbiol Immunol Infect 53(2):321–327
Monogue ML, Ortwine JK, Wei W, Eljaaly K, Bhavan KP (2018) Nafcillin versus cefazolin for the treatment of methicillin-susceptible Staphylococcus aureus bacteremia. J Infect Public Health 11(5):727–731
Youngster I, Shenoy ES, Hooper DC, Nelson SB (2014) Comparative evaluation of the tolerability of cefazolin and nafcillin for treatment of methicillin-susceptible Staphylococcus aureus infections in the outpatient setting. Clin Infect Dis 59(3):369–375
Fani F, Regolisti G, Delsante M, Cantaluppi V, Castellano G, Gesualdo L et al (2018) Recent advances in the pathogenetic mechanisms of sepsis-associated acute kidney injury. J Nephrol 31(3):351–359
Peerapornratana S, Priyanka P, Wang S, Smith A, Singbartl K, Palevsky PM et al (2020) Sepsis-associated acute kidney disease. Kidney Int Rep 5(6):839–850
Cosgrove SE, Vigliani GA, Fowler VG Jr, Abrutyn E, Corey GR, Levine DP et al (2009) Initial low-dose gentamicin for Staphylococcus aureus bacteremia and endocarditis is nephrotoxic. Clin Infect Dis 48(6):713–721
Bruss JB (2009) Lack of evidence associating nephrotoxicity with low-dose gentamicin for Staphylococcus aureus bacteremia and endocarditis. Clin Infect Dis. 49(5):806 (author reply 7-8)
Microbiologie NVvM. Guideline Staphylococcus aureus bacteraemia 2021 [Available from: https://www.nvmm.nl/media/3123/clean-richtlijn-s-aureus-bacteriemie-24-mei-2019.pdf.
Weis S, Kesselmeier M, Davis JS, Morris AM, Lee S, Scherag A et al (2019) Cefazolin versus anti-staphylococcal penicillins for the treatment of patients with Staphylococcus aureus bacteraemia. Clin Microbiol Infect 25(7):818–827
Rossert J (2001) Drug-induced acute interstitial nephritis. Kidney Int 60(2):804–817
Gagliardi JP, Nettles RE, McCarty DE, Sanders LL, Corey GR, Sexton DJ (1998) Native valve infective endocarditis in elderly and younger adult patients: comparison of clinical features and outcomes with use of the Duke criteria and the Duke Endocarditis Database. Clin Infect Dis 26(5):1165–1168
See EJ, Jayasinghe K, Glassford N, Bailey M, Johnson DW, Polkinghorne KR et al (2019) Long-term risk of adverse outcomes after acute kidney injury: a systematic review and meta-analysis of cohort studies using consensus definitions of exposure. Kidney Int 95(1):160–172
Acknowledgements
We thank E. Molendijk and S. Meziyerh for their invaluable help with the data collection.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Annette C. Westgeest, Merel M.C. Lambregts, and Emile F. Schippers. The first draft of the manuscript was written by Annette C. Westgeest, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was granted by the institutional ethical review committee of the Leiden University Medical Center.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Westgeest, A.C., Schippers, E.F., Delfos, N.M. et al. Acute kidney injury in Staphylococcus aureus bacteremia. Eur J Clin Microbiol Infect Dis 41, 431–437 (2022). https://doi.org/10.1007/s10096-021-04391-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-021-04391-3