Abstract
The aim of this study was to analyze the clinical and laboratory characteristics of children with peripheral facial nerve palsy (pFP) with a focus on identifying infectious etiology and long-term outcome. We conducted an ICD-10-based retrospective chart review on children hospitalized with pFP between January 1, 2006, and December 31, 2016. Furthermore, a telephone-based follow-up survey was performed. A total of 158 patients were identified, with a median age of 10.9 years (interquartile range 6.4–13.7). An infectious disease was associated with pFP in 82 patients (51.9%); 73 cases were classified as idiopathic pFP (46.2%). Three cases occurred postoperatively or due to a peripheral tumor. Among the infectious diseases, we identified 33 cases of neuroborreliosis and 12 viral infections of the central nervous system (CNS), caused by the varicella-zoster virus, human herpesvirus 6, herpes simplex virus, enterovirus, and Epstein-Barr virus. Other infections were mainly respiratory tract infections (RTIs; 37 cases). Children with an associated CNS infection had more often headache and nuchal rigidity, a higher cerebrospinal fluid cell count, and a longer length of hospital stay. Long-term follow-up revealed an associated lower risk of relapse in CNS infection–associated pFP. Among all groups, permanent sequelae were associated with female sex, a shorter length of hospitalization, and a lower white blood cell count at presentation. pFP is frequently caused by an CNS infection or is associated with concurrent RTIs, with a potential impact on the short- and long-term clinical course.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peripheral facial nerve palsy (pFP) is the most common cranial nerve lesion in children and adults [1]. Its causes are manifold, including infectious diseases such as neuroborreliosis [2], inflammation in the proximity of the facial nerve, such as mastoiditis [3], tumors [4], trauma [5], or systemic inflammatory conditions such as the Melkersson-Rosenthal syndrome [6]. Still, in most cases, no underlying cause can be identified, yielding the diagnosis (idiopathic) Bell’s palsy.
Clinically, the underlying etiology of pFP is difficult to diagnose. In contrast to international guidelines in which a diagnostic lumbar puncture is not deemed indispensable [7,8,9], the newest German guideline for pFP [10] advocates performing lumbar puncture and cerebrospinal fluid (CSF) analysis in adults, but even more so in children, since neuroborreliosis (NB) is more common among children as a cause of pFP than in adults [11]. Thus, CSF analysis has direct therapeutic implications [12, 13]. Although regional differences exist, borreliosis is the most frequent tick-borne disease within Germany, with reported incidences over the last years between 26 and 41 per 100,000 [14]. Apart from NB, other infections that have been linked to pFP are mainly viral central nervous system (CNS) infections, such as the Varicella-zoster virus (VZV) [15, 16]. Other neurotropic viruses that have been linked to pFP are Herpes simplex virus (HSV) [17,18,19], Epstein-Barr virus (EBV) [20,21,22,23], Cytomegalovirus (CMV) [24, 25], and human herpesvirus 6 (HHV6) [26]. These etiologies entail therapeutic consequences, e.g., the initiation of antiviral therapy or the cessation of empirical antibiotics. Most of the aforementioned viruses have been implicated in case reports. Overall, there is a scarcity of systematic studies in children focusing on infections as differential diagnoses. Thus, little is known about the frequency and relevance of other pathogens potentially involved in pediatric pFP. The aim of the study was to analyze clinical and laboratory characteristics in children with infectious and non-infectious etiology of pFP, and to evaluate the long-term outcome.
Materials and methods
Study design
This retrospective cohort study was carried out at the University Children’s Hospital, Mannheim, Germany. An approval from the ethics committee was obtained prior to study initiation (2017-541N-MA). All patients presenting to the hospital with pFP between January 1, 2006, and December 31, 2016, were included in this analysis. Charts were identified by searching the hospital database for the ICD-10 primary diagnosis code G51.-. In order to avoid selection bias, an additional search for G51.- as a secondary diagnosis was conducted. Patients with duplicate entries were only included once. Also, patients with central facial palsy were excluded, as were patients presenting for other reasons than the facial palsy (with a longstanding history of pFP).
Files were reviewed for present and past medical history, clinical findings, laboratory microbiological, and radiological findings, treatment, and the physician’s final diagnosis.
Etiological classification and infectious disease diagnostics
Patients were classified as idiopathic or non-idiopathic according to the physician’s diagnosis and all available data.
For the diagnosis of NB, three subgroups of certainty were used according to guidelines and as previously reported [12, 27, 28]: possible NB, probable NB, and definitive NB.
Possible NB was defined as compatible clinical findings and Borrelia-specific IgG and/or IgM in serum; probable NB was defined as the criteria for possible NB, plus CSF pleocytosis; definitive NB was defined as probable NB, plus the intrathecal synthesis of Borrelia-specific IgG and/or IgM or a positive culture or PCR.
The following diagnostic tests were applied for infectious analysis: blood and CSF IgM and IgG serology for NB (Enzygnost Borreliosis VlsE IgG/IgM ELISA, Dade Behring, Marburg, Germany; Liaison Borrelia IgG/Borrelia IgM Quant CLIA, Diasorin, Saluggia, Italy) with confirmatory western blot (recommBlot Borrelia NB IgG/IgM, and recomLine Borrelia IgG/IgM (lineblot), both Mikrogen, Neuried, Germany); blood or CSF serology for other viral pathogens; CSF culture; and a multiplex PCR (LIPA-CNS, Innogenetics, Ghent, Belgium) from CSF, including the following: HSV types 1 and 2, VZV, EBV, CMV, HHV6, Enterovirus, JC virus.
Trends in treatment
We compared two time periods, i.e., 2006–2011 and 2012–2016, for changes in treatment strategy. This division was chosen because the German guideline on the treatment of idiopathic facial nerve palsy was published in 2012, with the newest update published in 2017.
Follow-up survey
For the follow-up, a standardized questionnaire was designed, including questions about the course of the disease, further therapies, relapses, residuals, other symptoms, impact on the quality of life, and education. Patients were first contacted and asked for their participation in the study. After receiving the written informed consent, a telephone interview was conducted.
Statistical analysis
Statistical analyses were performed with SAS (Statistical Analysis System, Release 9.4, NC, USA). We compared idiopathic pFP with CNS infection-associated pFP and with pFP associated with concomitant RTI (including acute otitis media and mastoiditis) by using the one-way analysis of variance and Kruskal-Wallis test for comparing more than two groups. For comparisons between two groups, we applied the Mann-Whitney U test and t test for continuous variables and chi2 and Fisher’s exact test for categorical data. Furthermore, we performed a logistic regression to assess potential risk factors associated with the presence of long-term sequelae.
Results
Demographics in children with pFP
We identified 187 patients, of whom 29 were excluded (Fig. 1).
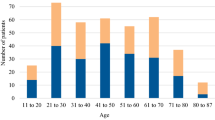
Of 158 patients included, 80 were male (50.6%). The median age at presentation was 10.9 (interquartile range 6.4–13.7). CSF analysis was performed in 137/158 (86.7%). Reasons for deferral were missing consent and unsuccessful lumbar puncture (LP). The most frequent classification was idiopathic pFP in 73 patients (46.2%). In 45 children (30%), an infection of the central nervous system (CNS) was diagnosed. Among those, 33 had NB (20.9%) and 12 had a viral CNS infection (7.6%). Furthermore, 12 patients had acute otitis media (AOM) or mastoiditis (7.6%), and an additional 25 patients had another concomitant RTI (15.8%). In three patients (1.9%), pFP occurred due to a peripheral tumor or postoperatively.
Seasonality in subgroups of children with pFP
Most cases were diagnosed between September and November (56/158; 35.4%). While children with RTI had their peak from October through February (16/25; 64%), NB patients mainly presented in June through October (27/33; 81.8%). In contrast, the presentation peak of viral CNS infections was February/March (5/12; 41.7%), while children with AOM/mastoiditis were evenly distributed (Fig. 2).
Infectious CNS diseases etiology in pediatric pFP
Of the 33 patients with NB, 15 were classified as definitive NB; 11 as probable NB; and 7 as possible NB. The median CSF cell count was highest in definitive NB with 168/μL (IQR 82.5–278.5) vs. 65/μL (37.5–83) and 2/μL (2–3) in probable and possible NB, respectively. Although CSF cell count and Borrelia-specific findings differed between the NB subgroups, the median duration of treatment was 14 days for all NB patients, taking outpatient parenteral antibiotic therapy into account.
A viral CNS infection was detected in 12 patients, in the vast majority of herpes viruses. In 3 patients, VZV was identified, while 2 patients were positive for HHV6, and one patient for Enterovirus (all PCR positive in the CSF). Serological diagnosis was made in two patients with acute HSV and three with acute EBV infection. In one patient, aseptic meningitis was diagnosed without pathogen detection. Antiviral therapy was initiated in 5 patients (3 with VZV, 1 with HSV, 1 without pathogen detection); the median duration of therapy was 7 days (IQR 4–14).
Clinical and laboratory characteristics of patients with pFP
There were no differences between idiopathic FP and CNS infection-associated pFP concerning sex, age at presentation, family history, vaccination status, body temperature, and neurological findings such as vertigo or nystagmus (Table 1). However, a positive tick bite history was more common among CNS infection-associated pFP compared with the other groups, as well as headache and nuchal rigor. The ratio of patients with CNS infection without signs of headache and nuchal rigidity was 21/45 (46.7%) and 39/45 (86.7%), respectively, while in 20/45 (44.4%), neither headache nor nuchal rigidity was reported. A rash was significantly more frequent among CNS infection-associated pFP than in idiopathic pFP, while an altered taste sensation was more frequent in RTI-associated pFP than in CNS infection-associated pFP.
There was no difference in CRP and leukocyte levels, while CSF cell counts differed significantly between all groups, with the highest values in patients with CNS infection-associated pFP. Similarly, patients with CNS infection-associated pFP had significantly higher CSF protein than the other groups. Lastly, length of stay (LOS) was significantly higher in this specific patient group, too.
Trends in treatment in pFP
We found an increased use of corticosteroids (CS), a decreased use of antibiotics, and a slightly decreased use of antivirals among all groups in the period 2012–2016 compared with 2006–2011 (Fig. 3a). This was most markedly seen in idiopathic pFP (Fig. 3b). In children with NB, no change of antibiotic utilization was observed (Fig. 3c).
Long-term follow-up
Data on follow-up were obtainable from 84/158 (53.2%) patients, with a median follow-up interval of 7.7 years (IQR 6.1–9.2). Recurrence of disease was significantly more often in idiopathic pFP compared with those with associated CNS infections, while there was no significant difference between temporary or persistent sequelae (Table 2). We observed more paresthesia and fatigue in CNS infection-associated pFP; furthermore, children with CNS infection-associated pFP reported to have limitations in daily activity more often than children with idiopathic pFP. Both differences were not statistically significant. Data on education was missing for some cases, while those still attending elementary school were not taken into account.
Logistic regression yielded the following three parameters as potentially influencing factors for permanent sequelae among all groups (c-index 0.756): female sex as a risk factor (odds ratio 3.60; 95% confidence interval 1.14–11.36; p = 0.029), long length of hospitalization (OR 0.85; 95%CI 0.70–1.02; p = 0.084), and a higher white blood cell count at presentation (OR 0.77; 95%CI 0.58–1.04; p = 0.087) as potential protective factors.
Discussion
We have shown in our cohort that a substantial amount of pediatric pFP cases is either caused by a CNS infection or associated with a RTI. Moreover, our data support that CNS pathogens other than Borrelia burgdorferi play a role in pFP. In our cohort, pFP caused by CNS infections differs in clinical presentation from the other groups with a higher rate of headache and nuchal rigor. Still, relying on clinical parameters might lead to underdiagnosis of infectious causes, since only 6/45 with CNS infection-associated pFP presented with nuchal rigor. The higher rate of positive tick bite history might have constituted a recall bias.
CSF analysis yielded significantly higher cell count and protein levels in CNS infection-associated pFP. Moreover, pFP associated with CNS infections lead to less recurrence than idiopathic cases. The comparison of idiopathic cases with RTI-associated pFP yielded a comparable presentation and long-term outcome, raising the question whether the latter should be regarded as idiopathic cases with concomitant, but not causally relevant RTI.
The strengths of our study are the cohort size, the thorough diagnostic work-up, and the long follow-up with a median interval of > 7 years. On the other hand, some patients were lost to follow-up or unwilling to participate. Therefore, conclusions on the outcome were hampered by a smaller sample size. Aside from that, a follow-up clinical examination of each patient would have been beneficial in order to obtain a more objective outcome parameter such as the House Brackmann Facial Nerve Grading Scale, as performed previously [29, 30]. Moreover, due to the retrospective design, only a selection of infectious diseases diagnostics initiated by the physician in charge may have led to an underestimation of other causes of pFP. In addition, the causative role of some viruses that were detected via serology remains questionable, since positive serology may not only indicate active disease but can also reflect possible simultaneous virus reactivation (especially HSV).
Our data confirm the prominent role of NB in children with pFP, comparable with other studies [12, 29, 31], and simultaneously highlight the difficulty in diagnosing probable or possible cases, given the fact that in some patients, LP cannot be performed due to various reasons (2/7 in our cases of possible NB). All cases of NB in our cohort, irrespective of diagnostic certainty, were treated with an adequate antibiotic for a median duration of 14 days. Still, patients with CNS infection-associated pFP and hence NB had the highest rate of limitation in daily activity, albeit without statistical significance, which further underscores the importance of a thorough diagnostic work-up and the initiation of an adequate therapy. Interestingly, no substantial effect of NB on the long-term social and educational outcome was found in a recent Danish cohort study with more than 2000 cases [32], confirming previous findings from Sweden [33]. In a previous German study [31], no statistically significant differences in time to recovery and residual symptoms were found between children with idiopathic FP and children with NB. In the same analysis, infectious etiologies other than NB included infections with adenovirus, Mycoplasma pneumoniae, and mumps virus. However, the methodology was insufficiently reported, thus limiting generalizability.
The role of HSV and VZV has been repeatedly reported previously [15, 19], which is further underlined by our findings. Additionally, our data support the role of HHV6 [26] and EBV [20, 34] in the context of pFP. In a study by Genizi and colleagues [35], HHV6 was found in the saliva of 71% of children with pFP, while other herpes viruses were less prevalent. Even after the resolution, HHV6 was detectable in most cases. Interestingly, no viral CSF analyses were reported.
As a rather novel finding, we observed an association between enteroviral infection and pFP. Given the high frequency of enterovirus among CNS infections in children [36], this singular case of a pFP may simply represent a chance finding. Prospective surveillance studies are warranted to confirm this potential association.
Our data on the treatment trends show a decrease in the use of antibiotics in idiopathic pFP, correlating with the updated German national guideline on the management of pFP. Treatment with CS, which is the evidence-based therapy in adults with idiopathic pFP [37], lacks conclusive data to be advocated likewise in children. This is reflected in the increased yet still low rate of CS use within the second time frame of our analysis. Due to the small number of patients who received CS and were available for follow-up, no firm conclusion could be made about CS therapy and its effect on the outcome. There is only limited data, mainly from retrospective studies, for the benefit of CS in children with pFP [38, 39]. Data from randomized controlled trials are scarce or, as in the case of the BellPIC study, yet to be reported [40]. The use of CS in NB has been implicated with worse outcomes in a recent study [41], which further underscores the importance of a thorough diagnostic work-up for clarifying the etiology.
We identified lower white blood cell count and shorter duration of hospitalization as possible risk factors for sequelae, as well as female sex. The latter finding is remarkable seeing that in a previous study, male sex had been identified as a risk factor for having pFP among patients with Lyme disease [42], while in another study, female sex was associated with a higher risk of recurrence among patients with pFP [43]. The rate of recurrence in idiopathic pFP of 10/37 (27%) is seemingly higher than in other studies, in which rates between 0.8 and 19% have been reported [6, 38, 44, 45]. This discrepancy could be partly explained by a more thorough follow-up in our study. Moreover, other etiologies than idiopathic pFP could have biased the recurrence rates in other studies due to the heterogeneity of cohorts and less strict group stratifications, which is somehow reflected in the broad distribution of recurrence rates over several studies. Standardized outcome measures that have recently been proposed may help harmonize future studies and render them more comparable with each other [46].
The generalizability of our results has to be handled with caution; the proportion of NB may be higher in some parts of the world [47] and lower in other parts, although undamped climate change may affect both incidence and seasonality of borreliosis [48]. Still, there is a lack of extensive data on children with pFP concerning potential infectious etiologies, and further studies, especially from other geographic backgrounds, are warranted.
Novel diagnostic techniques, such as next-generation sequencing (NGS), have helped to detect new organisms [49,50,51,52] or long-known but atypically presenting pathogens [53] in CNS infections. It remains to be seen how NGS can be exploited to fully elucidate hitherto underestimated etiologies of pFP. In conclusion, our data support the importance of infectious disease etiology in pediatric pFP patients, with potential impact on the long-term outcome. Novel diagnostics may help to unveil other causes of pFP that may falsely be labelled idiopathic.
References
Garro A, Nigrovic LE (2018) Managing peripheral facial palsy. Ann Emerg Med 71(5):618–624
Nigrovic LE, Thompson AD, Fine AM, Kimia A (2008) Clinical predictors of Lyme disease among children with a peripheral facial palsy at an emergency department in a Lyme disease-endemic area. Pediatrics 122(5):e1080–e1085
Chen XC, Lu CW, Liu CH, Wei CC (2014) Facial palsy complicated by masked otomastoiditis in a 3-month-old infant. J Emerg Med 46(2):e47–e50
Gandolfi MM, Slattery W 3rd (2016) Parotid gland tumors and the facial nerve. Otolaryngol Clin N Am 49(2):425–434
Cools MJ, Carneiro KA (2018) Facial nerve palsy following mild mastoid trauma on trampoline. Am J Emerg Med 36(8):1522.e1521–1522.e1523
Chweya CM, Anzalone CL, Driscoll CLW, Lane JI, Carlson ML (2019) For whom the bell’s toll: recurrent facial nerve paralysis, a retrospective study and systematic review of the literature. Otol Neurotol 40(4):517–528
Baugh RF, Basura GJ, Ishii LE, Schwartz SR, Drumheller CM, Burkholder R, Deckard NA, Dawson C, Driscoll C, Gillespie MB et al (2013) Clinical practice guideline: Bell’s palsy. Otolaryngol Head Neck Surg 149(3 Suppl):S1–S27
Gronseth GS, Paduga R (2012) Evidence-based guideline update: steroids and antivirals for Bell palsy: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology 79(22):2209–2213
Schwartz SR, Jones SL, Getchius TS, Gronseth GS (2014) Reconciling the clinical practice guidelines on Bell’s palsy from the AAO-HNSF and the AAN. Otolaryngol Head Neck Surg 150(5):709–711
S2k-Leitlinie Therapie der idiopathischen Fazialisparese (Bell’s palsy). https://www.dgn.org/leitlinien/3432-030-013-therapie-der-idiopathischen-fazialisparese-bell-s-palsy-2017. Accessed 22 May 2019
Cardenas-de la Garza JA, De la Cruz-Valadez E, Ocampo-Candiani J, Welsh O (2019) Clinical spectrum of Lyme disease. Eur J Clin Microbiol Infect Dis 38(2):201–208
Henkel K, Lange P, Eiffert H, Nau R, Spreer A (2016) Infections in the differential diagnosis of Bell’s palsy: a plea for performing CSF analysis. Infection
Ozkale Y, Erol I, Saygi S, Yilmaz I (2015) Overview of pediatric peripheral facial nerve paralysis: analysis of 40 patients. J Child Neurol 30(2):193–199
Enkelmann J, Bohmer M, Fingerle V, Siffczyk C, Werber D, Littmann M, Merbecks SS, Helmeke C, Schroeder S, Hell S et al (2018) Incidence of notified Lyme borreliosis in Germany, 2013-2017. Sci Rep 8(1):14976
Monsanto RD, Bittencourt AG, Bobato Neto NJ, Beilke SC, Lorenzetti FT, Salomone R (2016) Treatment and prognosis of facial palsy on Ramsay hunt syndrome: results based on a review of the literature. Int Arch Otorhinolaryngol 20(4):394–400
Furuta Y, Ohtani F, Aizawa H, Fukuda S, Kawabata H, Bergström T (2005) Varicella-zoster virus reactivation is an important cause of acute peripheral facial paralysis in children. Pediatr Infect Dis J 24(2):97–101
Vakharia K, Vakharia K (2016) Bell’s palsy. Facial Plast Surg Clin North Am 24(1):1–10
Greco A, Gallo A, Fusconi M, Marinelli C, Macri GF, de Vincentiis M (2012) Bell’s palsy and autoimmunity. Autoimmun Rev 12(2):323–328
Kennedy PG (2010) Herpes simplex virus type 1 and Bell’s palsy-a current assessment of the controversy. J Neuro-Oncol 16(1):1–5
Vogelnik K, Matos A (2017) Facial nerve palsy secondary to Epstein-Barr virus infection of the middle ear in pediatric population may be more common than we think. Wien Klin Wochenschr 129(21–22):844–847
Diedler J, Rieger S, Koch A, Parthe-Peterhans S, Schwaninger M (2006) Bilateral facial palsy: Epstein-Barr virus, not Lyme disease. Eur J Neurol 13(9):1029–1030
Terada K, Niizuma T, Kosaka Y, Inoue M, Ogita S, Kataoka N (2004) Bilateral facial nerve palsy associated with Epstein-Barr virus infection with a review of the literature. Scand J Infect Dis 36(1):75–77
Kleines M, Schiefer J, Stienen A, Blaum M, Ritter K, Hausler M (2011) Expanding the spectrum of neurological disease associated with Epstein-Barr virus activity. Eur J Clin Microbiol Infect Dis 30(12):1561–1569
Hirano T, Tsuji T, Yamasaki H, Tsuda H (2014) Cytomegalovirus mononucleosis complicated with peripheral facial palsy. Rinsho ketsueki 55(3):356–359
Kanerva M, Nissinen J, Moilanen K, Maki M, Lahdenne P, Pitkaranta A (2013) Microbiologic findings in acute facial palsy in children. Otol Neurotol 34(7):e82–e87
Kanerva M, Jaaskelainen AJ, Suvela M, Piiparinen H, Vaheri A, Pitkaranta A (2008) Human herpesvirus-6 and -7 DNA in cerebrospinal fluid of facial palsy patients. Acta Otolaryngol 128(4):460–464
Halperin JJ, Logigian EL, Finkel MF, Pearl RA (1996) Practice parameters for the diagnosis of patients with nervous system Lyme borreliosis (Lyme disease). Quality Standards Subcommittee of the American Academy of Neurology. Neurology 46(3):619–627
Neuroborreliose, S3-Leitlinie (2018) In: Deutsche Gesellschaft für Neurologie (Hrsg.), Leitlinien für Diagnostik und Therapie in der Neurologie. https://www.dgn.org/leitlinien/3567-ll-030-071-2018-neuroborreliose. Accessed 22 May 2019
Drack FD, Weissert M (2013) Outcome of peripheral facial palsy in children - a catamnestic study. Eur J Paediatr Neurol 17(2):185–191
Skogman BH, Croner S, Odkvist L (2003) Acute facial palsy in children--a 2-year follow-up study with focus on Lyme neuroborreliosis. Int J Pediatr Otorhinolaryngol 67(6):597–602
Jenke AC, Stoek LM, Zilbauer M, Wirth S, Borusiak P (2011) Facial palsy: etiology, outcome and management in children. Eur J Paediatr Neurol 15(3):209–213
Obel N, Dessau RB, Krogfelt KA, Bodilsen J, Andersen NS, Moller JK, Roed C, Omland LH, Christiansen CB, Ellermann-Eriksen S et al (2018) Long term survival, health, social functioning, and education in patients with European Lyme neuroborreliosis: nationwide population based cohort study. BMJ 361:k1998
Skogman BH, Glimaker K, Nordwall M, Vrethem M, Odkvist L, Forsberg P (2012) Long-term clinical outcome after Lyme neuroborreliosis in childhood. Pediatrics 130(2):262–269
Grassin M, Rolland A, Leboucq N, Roubertie A, Rivier F, Meyer P (2017) Bilateral facial nerve palsy associated with Epstein-Barr virus infection in a 3-year-old boy. Arch Pediatr 24(6):564–567
Genizi J, Golan-Shany O, Tarazov T, Pechter S, Assaf N, Segal I, Srugo I, Bamberger E (2019) Does herpes 6 infection have a role in Bell’s palsy among children and adolescents? Pediatr Infect Dis J 38(5):481–483
Rudolph H, Prieto Dernbach R, Walka M, Rey-Hinterkopf P, Melichar V, Muschiol E, Schweitzer-Krantz S, Richter JW, Weiss C, Bottcher S et al (2017) Comparison of clinical and laboratory characteristics during two major paediatric meningitis outbreaks of echovirus 30 and other non-polio enteroviruses in Germany in 2008 and 2013. Eur J Clin Microbiol Infect Dis 36(9):1651–1660
Madhok VB, Gagyor I, Daly F, Somasundara D, Sullivan M, Gammie F, Sullivan F (2016) Corticosteroids for Bell’s palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 7:Cd001942
Karalok ZS, Taskin BD, Ozturk Z, Gurkas E, Koc TB, Guven A (2018) Childhood peripheral facial palsy. Childs Nerv Syst 34(5):911–917
Arican P, Dundar NO, Gencpinar P, Cavusoglu D (2017) Efficacy of low-dose corticosteroid therapy versus high-dose corticosteroid therapy in Bell’s palsy in children. J Child Neurol 32(1):72–75
Babl FE, Mackay MT, Borland ML, Herd DW, Kochar A, Hort J, Rao A, Cheek JA, Furyk J, Barrow L et al (2017) Bell’s palsy in children (BellPIC): protocol for a multicentre, placebo-controlled randomized trial. BMC Pediatr 17(1):53
Jowett N, Gaudin RA, Banks CA, Hadlock TA (2017) Steroid use in Lyme disease-associated facial palsy is associated with worse long-term outcomes. Laryngoscope 127(6):1451–1458
Kwit NA, Nelson CA, Max R, Mead PS (2018) Risk factors for clinician-diagnosed Lyme arthritis, facial palsy, carditis, and meningitis in patients from high-incidence states. Open Forum Infect Dis 5(1):ofx254
Cirpaciu D, Goanta CM, Cirpaciu MD (2014) Recurrences of Bell’s palsy. J Med Life 7(3):68–77
Dong SH, Jung AR, Jung J, Jung SY, Byun JY, Park MS, Kim SH, Yeo SG (2019) Recurrent Bell’s palsy. Clin Otolaryngol 44(3):305–312
Yilmaz U, Cubukcu D, Yilmaz TS, Akinci G, Ozcan M, Guzel O (2014) Peripheral facial palsy in children. J Child Neurol 29(11):1473–1478
Butler DP, De la Torre A, Borschel GH, Hadlock TA, Beurskens C, Bogart K, Cardenas Mejia A, Coombs C, Copeland J, Diels J et al (2019) An international collaborative standardizing patient-centered outcome measures in pediatric facial palsy. JAMA Facial Plast Surg
Tveitnes D, Oymar K, Natas O (2007) Acute facial nerve palsy in children: how often is it Lyme borreliosis? Scand J Infect Dis 39(5):425–431
Dumic I, Severnini E (2018) “Ticking Bomb”: the impact of climate change on the incidence of lyme disease. Can J Infect Dis Med Microb 2018:5719081
Kawada J, Okuno Y, Torii Y, Okada R, Hayano S, Ando S, Kamiya Y, Kojima S, Ito Y (2016) Identification of viruses in cases of pediatric acute encephalitis and encephalopathy using next-generation sequencing. Sci Rep 6:33452
Hoffmann B, Tappe D, Hoper D, Herden C, Boldt A, Mawrin C, Niederstrasser O, Muller T, Jenckel M, van der Grinten E et al (2015) A variegated squirrel bornavirus associated with fatal human encephalitis. N Engl J Med 373(2):154–162
Simonin Y, Sillam O, Carles MJ, Gutierrez S, Gil P, Constant O, Martin MF, Girard G, Van de Perre P, Salinas S et al (2018) Human Usutu virus infection with atypical neurologic presentation, Montpellier, France, 2016. Emerg Infect Dis 24(5):875–878
Ashraf U, Ye J, Ruan X, Wan S, Zhu B, Cao S (2015) Usutu virus: an emerging flavivirus in Europe. Viruses 7(1):219–238
Wilson MR, Naccache SN, Samayoa E, Biagtan M, Bashir H, Yu G, Salamat SM, Somasekar S, Federman S, Miller S et al (2014) Actionable diagnosis of neuroleptospirosis by next-generation sequencing. N Engl J Med 370(25):2408–2417
Acknowledgments
We thank all patients and their parents for their willingness to participate in this study. We are grateful to Michael Karremann for his support in data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the ethics committee of the Medical Faculty Mannheim, Heidelberg University (2017-541N-MA). Informed consent was obtained from patients prior to the follow-up interview.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Papan, C., Kremp, L., Weiß, C. et al. Infectious causes of peripheral facial nerve palsy in children—a retrospective cohort study with long-term follow-up. Eur J Clin Microbiol Infect Dis 38, 2177–2184 (2019). https://doi.org/10.1007/s10096-019-03660-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03660-6