Abstract
Men who have sex with men (MSM) have a disproportionate risk of acquiring sexually transmitted infections (STIs), such as syphilis. However, prevalence and determinants of syphilis among this population are less known in West Africa. This study aims to estimate syphilis prevalence among MSM in Burkina Faso. We conducted a cross-sectional biological and behavior survey in the two main cities of Burkina Faso, Ouagadougou and Bobo-Dioulasso. MSM were recruited using Respondent Driven Sampling (RDS) methods. Data were collected from January to April 2013 in Ouagadougou and from May to August 2013 in Bobo-Dioulasso. Out of the 657 MSM screened for syphilis, 6.1% (40/657) tested positive for Treponema pallidum antibodies and 1.1% (7/657) for active syphilis. Population-weighted prevalence of active syphilis was 2.1% (95% CI, 01.1–04.4) in Ouagadougou and 0.0% in Bobo-Dioulasso. Serologic markers of syphilis (anti-Treponema antibodies) were found among 7.4% (95% CI 5.0–10.8) of MSM in Ouagadougou and 5.0% (95% CI 3.1–8.0) in Bobo-Dioulasso. No significant differences were found in syphilis serological markers prevalence by participants’ sociodemographic and behavioral characteristics. The prevalence of syphilis among MSM is low and comparable to that of other individuals of reproductive age in Burkina Faso. This low prevalence is very encouraging and suggests implementation of effective public health intervention programs which direct resources and services toward MSM to prevent further spread of syphilis infection and to limit HIV transmission in this group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Syphilis remains an important public health problem in many low-income countries where it is endemic [1]. Additionally, it has reemerged in several high-income countries, particularly in high-risk groups such as men who have sex with men (MSM) [1,2,3]. For example, in the United States of America (USA), between 2016 and 2017, the number of reported primary and secondary syphilis increased by 10.5%, and 58% of 30,644 primary and secondary syphilis cases reported in 2017 were among MSM [4]. Findings from a systematic review of trend studies published between 2004 and 2015 indicate an increase in both the absolute numbers, as well as the rates (per 100,000) of syphilis infections among MSM in the USA and Western Europe since 1998 [3]. Similar findings were reported in China where the prevalence of syphilis increased from 6.8% in 2003–2004 to 13.5% in 2007–2008 [5].
This resurgence of infection has been strongly associated with the increase in HIV incidence [6]. The risk factors commonly associated with both HIV and syphilis include biological, e.g., anal sex and presence of other STIs, and behavioral risks, e.g., condomless intercourse and injectable drug use [7,8,9]. Prevention tools, such as condoms, risk-reduction counseling, and syphilis screening and treatment, can alter syphilis rates by modifying its incidence [7]. As a result, the screening and treatment of syphilis in most-at-risk populations can help to reduce the transmission of HIV and other STIs. MSM have been studied as a most-at-risk population for HIV in Africa [10,11,12]. However, very little information is available on the epidemiology of syphilis among this population in many African countries, particularly in West Africa [12]. This study aims to estimate syphilis seroprevalence among MSM in two major cities in Burkina Faso, a low-income West African country.
Materials and methods
Study design and location
We conducted a cross-sectional study among MSM in the two main cities of Burkina Faso, Ouagadougou and Bobo-Dioulasso.
Study participants
MSM were eligible to participate if they were (i) at least 18 years old, (ii) assigned male sex at birth, (iii) reported they had anal sex with a man at least once in the past 12 months, (iv) were able to provide informed consent in French, Mòoré, or Dioula, (v) had a valid peer recruitment coupon (each coupon included a unique coupon code, study office phone number, hours of operation, expiration date), (vi) lived in either Ouagadougou or Bobo-Dioulasso for at least the past 3 months, and (vii) agreed to complete a behavioral survey and HIV and syphilis testing.
The sample size was based on expected HIV prevalence and calculated to recruit 345 MSM in each city, anticipating 10% non-response.
Participants were recruited using RDS, a non-probability sampling approach used to sample individuals whose behavior or identity may be stigmatized or even criminalized but who are well-networked [13]. Six MSM seeds in Ouagadougou and four MSM seeds in Bobo-Dioulasso were purposely selected to initiate recruitment chains. After giving informed consent, seeds were required to complete a survey and have their blood drawn. These seeds were each provided with three coded coupons, which were valid for 4 weeks to recruit peer MSM from their social networks. Individuals who were recruited by seeds and enrolled in the study were then provided with three coded study coupons for further recruitment of peers. This process continued until the target sample size was reached in each city. The study method has been described previously in greater detail [14, 15].
Data collection
Data were collected from January to April 2013 in Ouagadougou and May to August 2013 in Bobo-Dioulasso. Following informed consent, MSM participants completed interviewer-administered face-to-face surveys in a private room. Participant information was anonymized and identified with a unique code number to protect confidentiality. Data collected in the questionnaire included demographic and socioeconomic information, the number of sexual partners, sexual behavior (including condom use), and STD screening and symptoms [14, 15].
Laboratory methods
Venous blood was collected from each participant who consented to the screening test. Blood samples were centrifuged and the serum obtained was used in situ for syphilis screening. Alere Determine™ Syphilis TP (“Alere Ltd,” USA) rapid diagnostic test was used to screen the syphilis serological markers as per manufacturer recommendations. Positive samples were consecutively tested with Rapid Plasma Reagin (RPR-CHARBON®) test kit (BIOLABO SAS, French) test to detect antibodies to non-treponemal antigens [16]. Alere Determine™ Syphilis TP is a qualitative in vitro immune-chromatographic test detecting antibodies against the Treponema pallidum bacteria in patient’s serum, plasma, and whole blood [17]. Positivity to the Alere Determine™ Syphilis TP test reveals the presence of antibodies against the Treponema pallidum bacteria indicating the presence either of previous, acute, or treated syphilis. Antibody to non-treponemal antigens is found in active disease and the levels subside after successful treatment, while Treponema-specific antibodies persist for a long time after the infection has been successfully treated [18]. Active syphilis was defined as Alere Determine™ Syphilis TP and RPR positive.
Data processing and analysis
Data were analyzed with Stata 14 (StataCorp, College Station, TX). RDS weighted analysis was only used to estimate active syphilis and syphilis serological markers prevalence for each city. The weighting takes into consideration the probability of each participant to be included in the study. This probability was measured through weighting based on the size of each participant’s network. Network size was determined using the survey question: “How many different people do you know personally who are men who have sex with men? i.e., you know them and they know you, and you could contact them if you needed to?”
Due to the low number of positive cases of syphilis serological markers for statistical analysis, data from both study cities were pooled. Bivariate logistic regression analyses were conducted to identify factors associated with syphilis serological markers. Associations were expressed as unadjusted odds ratios (OR) with 95% confidence intervals (CIs). Results were considered statistically significant at the p < 0.05 level.
Ethical considerations
The study protocol was approved by Johns Hopkins Bloomberg School of Public Health Institutional Review Board and the National Ethics Committee for Health Research (Comité d’Ethique pour la Recherche en Santé, CERS) of Burkina Faso. Individual informed consent was obtained from all participants. All participants received pre- and post-test counseling for syphilis screening. MSM detected with positive antibodies to treponemal antigens were treated in situ with one intramuscular dose of benzathine benzylpenicillin G 2.4 MUI and kept under observation over 30 min to capture any immediate adverse event. Positive cases presenting allergy received doxycycline 100 mg tablet over 2 weeks. All participants were sensitized on safe sex (protection measures against STDs), were encouraged to undergo a serological test for syphilis every 3 to 6 months, and were provided with condoms and lubricants free of charge.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Results
A total of 657 MSM out of 673 who participated in the study agreed to be screened for syphilis (97.6%). Forty (6.1%) MSM tested positive for Treponema pallidum antibodies, and only seven (1.1%) MSM had active syphilis. All of the active syphilis cases were found in Ouagadougou. Figure 1 shows the flow chart of syphilis screening among study participants.
Characteristics of MSM
The sample consists of 330 MSM from Ouagadougou and 327 from Bobo-Dioulasso. The mean age (SD) of MSM was 22.7 ± 0.17 years. Most MSM were single (95.3%, 626/657), with secondary education (70.6%, 454/657). Pupils/students represented 63.2% (415/657) and public or private sector workers made up 30.4% (95% CI 27.0–34.1). Regarding gender identity, over 66.4% of MSM identified themselves as men, 14.5% as women, and 19.0% identify as intersex. The vast majority of MSM surveyed were of Burkinabe origin, 83.2% (Table 1).
Prevalence of active syphilis and syphilis serological markers
Population-weighted prevalence of active syphilis by city was 2.1% (95% CI 01.1–04.4) in Ouagadougou and 0.0% in Bobo-Dioulasso. Serologic markers of syphilis (anti-Treponema antibodies) were found in 7.4% (95%CI 5.0–10.8) of MSM in Ouagadougou and 5.0% (95%CI 3.1–08.0) of them in Bobo-Dioulasso (Table 2).
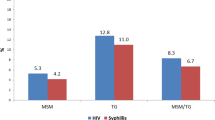
The prevalence of serologic markers of syphilis (anti-treponemic antibodies) by participants’ characteristics and results of the bivariate analysis on pooled data are presented in Table 3. These markers were found in 4.6% of MSM less than 25 years old, 7.3% among those between 25 to 29 years old, and 12.5% (95% CI 6.2–24.1) of MSM of 35 years or older. However, the differences observed were not significant (OR = 2.97, 95% CI 0. 95–9.29). No statistically significant difference was found in syphilis serological markers prevalence regarding participant education level. Among MSM who reported a history of STIs in the last 12 months, 8.0% had serologic markers for syphilis versus 5.6% in those who did not report symptoms (OR = 1.47, 95% CI 0.73–2.98). No positive serological marker of syphilis was found among HIV-positive MSM.
Discussion
This study reports on seroprevalence of syphilis among MSM in West Africa and represents the first epidemiological data on this infection among this group in Burkina Faso. The results indicate that the prevalence of active syphilis in MSM is relatively low in Ouagadougou (2.1%), and Bobo-Dioulasso (0.0%) compared to those of some African cities but remains high compared to others. Johnston et al. in Morocco reported higher prevalence of active syphilis among MSM in Morocco in 2012, specifically 7.0% in Agadir and 10.8% in Marrakesh [19]. In Eastern Africa, active syphilis seroprevalence was reported to be 9.0% among MSM in Kampala, Uganda [20], while in Tanzania, the prevalence of active syphilis was estimated at 0.2% in MSM [21]. These disparities observed between countries could be explained by the epidemiologic profile of syphilis in each country, but also by the profile of MSM and the risk level of sexual behavior. In Uganda, majority of MSM reported inconsistent condom use and high level of engagement in sex work.
Other studies tend to confirm low prevalence of syphilis in Burkina Faso. A 2010 study found prevalence of 1.7% (95% CI 1.3 to 2.2) with similar rates between women (1.2%, 95% CI 0.7 to 2.3) and men (1.8%, 95% CI 1.0 to 3.0) in Ouagadougou [22]. Another study among blood donors reported seroprevalence estimates of 0.7%, 1.5%, 1.7%, and 2.5% respectively in Bobo-Dioulasso, Fada Ngourma, Ouagadougou, and Koudougou [23]. In a recent study among female sex workers in five cities of Burkina Faso, Ouedraogo et al. estimated the syphilis prevalence at 1.4% in 2014 [24], while authors in another 10-year-old study found a prevalence of 15% among this population [25].
The low prevalence of active syphilis among our study participants could be explained by the success of the HIV prevention through safe sex promotion and condom use, and the widespread use of antibiotics which may have contributed to the decrease in new transmission events. In addition to penicillin, the Treponema pallidum (bacterial cause of infectious syphilis) is also treated with other antibiotics such as cephalosporins (for example, cephaloridine), tetracyclines, macrolides (erythromycin, spiramycin), and chloramphenicol [26].
This study has a few limitations. First, self-reporting risk behavior in a context of social stigmatization of and discrimination toward MSM may have led to social desirability bias; however, this did not impact the prevalence of syphilis, as this was evaluated through syphilis serological markers. Although RDS is designed to capture a representative sample of the target population, RDS is based on a number of assumptions that may not have been met because this discrimination may have biased recruitment toward a certain subgroup of MSM [27, 28]. Due to the small number of active syphilis cases, we were limited in the number of predictors of syphilis we could evaluate. Despite these limitations, our study provides the first data on syphilis serological markers among MSM in Burkina Faso and strengthens knowledge on the epidemiology of syphilis in key populations in Africa.
Conclusion
In conclusion, the prevalence of syphilis among MSM is low and comparable to that of other individuals of reproductive age in Burkina Faso. This low prevalence is very encouraging and suggests implementation of effective public health intervention programs which direct resources and services toward MSM to prevent further spread of syphilis infection and to limit HIV transmission in this group. Comprehensive interventions to diagnose, treat, and prevent syphilis and other sexually transmitted diseases among this population should be implemented to ensure sustained control of syphilis and other STIs.
References
Kojima N, Klausner JD (2018) An update on the global epidemiology of syphilis. Curr Epidemiol Rep 5:24–38. https://doi.org/10.1007/s40471-018-0138-z
Stamm LV. Syphilis: re-emergence of an old foe. Microb Cell [Internet] [cited 2018 18];3:363–70. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5354565/. https://doi.org/10.15698/mic2016.09.523
Abara WE, Hess KL, Neblett Fanfair R, Bernstein KT, Paz-Bailey G. Syphilis trends among men who have sex with men in the United States and Western Europe: a systematic review of trend studies published between 2004 and 2015. PLoS One [Internet] 2016 22 [cited 2018 18];11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4957774/. https://doi.org/10.1371/journal.pone.0159309
CDC. Syphilis & MSM (men who have sex with men) - CDC facts sheet. [Internet] [cited 2018 18]; 2017. https://www.cdc.gov/std/syphilis/syphilis-msm-fact-sheet.pdf
Chow EPF, Wilson DP, Zhang L (2011) HIV and syphilis co-infection increasing among men who have sex with men in China: a systematic review and meta-analysis. PLoS One 6:e22768. https://doi.org/10.1371/journal.pone.0022768
HIV and syphilis rates were highest among MSM [Internet]. [cited 2017 17]. http://www.healio.com/infectious-disease/stds/news/online/%7B329eec8c-8329-4936-b801-d59ae2b2ca4b%7D/hiv-and-syphilis-rates-were-highest-among-msm
Stoltey JE, Cohen SE. Syphilis transmission: a review of the current evidence. Sex. Health [Internet] 2015 [cited 2018 18];12:103–9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC597382e4/. https://doi.org/10.1071/SH14174
Phipps W, Kent CK, Kohn R, Klausner JD. Risk factors for repeat syphilis in men who have sex with men, San Francisco: Sex. Transm. Dis. [Internet] 2009 [cited 2017 30];36:331–5. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00007435-200906000-00001. https://doi.org/10.1097/OLQ.0b013e3181990c85
Peterman TA, Furness BW. The resurgence of syphilis among men who have sex with men: Curr Opin Infect Dis [Internet] 2007 [cited 2017 30];20:54–9. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00001432-200702000-00010. https://doi.org/10.1097/QCO.0b013e32801158cc
Sanders EJ, Graham SM, Okuku HS, van der Elst EM, Muhaari A, Davies A et al (2007) HIV-1 infection in high risk men who have sex with men in Mombasa, Kenya. AIDS London, England 21:2513–2520. https://doi.org/10.1097/QAD.0b013e3282f2704a
Niccolai LM, Livingston KA, Richardson W, Jenkins H. Sex partner meeting venues and out-of-state sex partners among men who have sex with men with early syphilis in Connecticut: Sex. Transm. Dis. [Internet] 2007 [cited 2017 30];34:887–91. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00007435-200711000-00012. https://doi.org/10.1097/OLQ.0b013e3180646422
Wade AS, Kane CT, Diallo PAN, Diop AK, Gueye K, Mboup S, et al. HIV infection and sexually transmitted infections among men who have sex with men in Senegal. AIDS [Internet] 2005 2 [cited 2019 21];19:2133. https://journals.lww.com/aidsonline/Fulltext/2005/12020/HIV_infection_and_sexually_transmitted_infections.10.aspx. https://doi.org/10.1097/01.aids.0000194128.97640.07
Heckathorn Douglas D. Respondent-driven sampling: a new approach to the study of hidden populations. Univ Calif Press Behalf Soc Study Soc Probl 1997;44:174–99
Ouedraogo HG, Kouanda S, Grosso A, Compaoré R, Camara M, Dabire C, et al. Hepatitis B, C, and D virus and human T-cell leukemia virus types 1 and 2 infections and correlates among men who have sex with men in Ouagadougou, Burkina Faso. Virol J [Internet] 2018 29 [cited 2019 11];15. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6311018/. https://doi.org/10.1186/s12985-018-1110-8
Ouedraogo HG, Ky-Zerbo O, Grosso A, Goodman S, Samadoulougou BC, Tarnagda G, et al. Human immunodeficiency virus (HIV) among men who have sex with men: results of the first integrated biological and behavioral survey in Burkina Faso, West Africa. BMC Public Health [Internet] 2019 3 [cited 2019 11];19:5. https://doi.org/10.1186/s12889-018-6361-1
WHO/TDR. The use of rapid syphilis test. [Internet] 2016 [cited 2019 11]; 2006. https://apps.who.int/iris/bitstream/handle/10665/43590/TDR_SDI_06.1_eng.pdf;jsessionid=94C2337C6F565F87C0E0CBCBAD5B9159?sequence=1
Bocoum F, Ouedraogo H, Tarnagda G, Kiba A, Tiendrebeogo S, Bationo F, et al. Evaluation of the diagnostic performance and operational characteristics of four rapid immunochromatographic syphilis tests in Burkina Faso. Afr Health Sci. [Internet] 2015 28 [cited 2017 15];15:360. http://www.ajol.info/index.php/ahs/article/view/117507. https://doi.org/10.4314/ahs.v15i2.8
Naidu NK, Bharucha ZS, Sonawane V, Ahmed I. Comparative study of treponemal and non-treponemal test for screening of blood donated at a blood center. Asian J Transfus Sci. [Internet] 2012 [cited 2019 31];6:32–5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3353627/. https://doi.org/10.4103/0973-6247.95048
Johnston LG, Alami K, El Rhilani MH, Karkouri M, Mellouk O, Abadie A et al (2013) HIV, syphilis and sexual risk behaviours among men who have sex with men in Agadir and Marrakesh, Morocco. Sex Transm Infect 89(Suppl 3):iii45–iii48. https://doi.org/10.1136/sextrans-2012-050918
Kim EJ, Hladik W, Barker J, Lubwama G, Sendagala S, Ssenkusu JM et al (2016) Sexually transmitted infections associated with alcohol use and HIV infection among men who have sex with men in Kampala, Uganda. Sex Transm Infect 92:240–245. https://doi.org/10.1136/sextrans-2015-052034
Mmbaga EJ, Moen K, Makyao N, Mpembeni R, Leshabari MT (2017) HIV and STI s among men who have sex with men in Dodoma municipality, Tanzania: a cross-sectional study. Sex Transm Infect:15. https://doi.org/10.1136/sextrans-2016-052770
Kirakoya-Samadoulougou F, Defer M-C, Yaro S, Fao P, Ilboudo F, Langani Y et al (2011) Low seroprevalence of syphilis in Burkina Faso. Sex Transm Infect 87:35–37. https://doi.org/10.1136/sti.2010.042465
Bisseye C, Sanou M, Nagalo BM, Kiba A, Compaoré TR, Tao I et al (2013) Epidemiology of syphilis in regional blood transfusion centres in Burkina Faso, West Africa. Pan Afr Med J 16:69. https://doi.org/10.11604/pamj.2013.16.69.2767
Ouedraogo HG, Meda IB, Zongo I, Ky-Zerbo O, Grosso A, Samadoulougou BC et al (2018) Syphilis among female sex workers: results of point-of-care screening during a cross-sectional behavioral survey in Burkina Faso, West Africa. Int J Microbiol 2018:4790560. https://doi.org/10.1155/2018/4790560
Lankoandé S, Meda N, Sangaré L, Compaoré IP, Catraye J, Sanou PT et al (1998) Prevalence and risk of HIV infection among female sex workers in Burkina Faso. Int J STD AIDS 9:146–150. https://doi.org/10.1258/0956462981921909
Singh AE, Romanowski B Syphilis. Review with emphasis on clinical, epidemiologic, and some biologic features. Clin Microbiol Rev [Internet] 1999 [cited 2017 16];12:187–209. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC88914/
Lansky A, Drake A, Wejnert C, Pham H, Cribbin M, Heckathorn DD. Assessing the assumptions of respondent-driven sampling in the national HIV behavioral surveillance system among injecting drug users. Open AIDS J [Internet] 2012 7 [cited 2018 24];6:77–82. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3462332/. https://doi.org/10.2174/1874613601206010077
Kendall C, Kerr LRFS, Gondim RC, Werneck GL, Macena RHM, Pontes MK et al (2008) An empirical comparison of respondent-driven sampling, time location sampling, and snowball sampling for behavioral surveillance in men who have sex with men, Fortaleza, Brazil. AIDS Behav 12:S97–S104. https://doi.org/10.1007/s10461-008-9390-4
Acknowledgments
The authors acknowledge the team of Research to Prevention (R2P) Project led by the Johns Hopkins Center for Global Health and managed by the Johns Hopkins Bloomberg School of Public Health Center for Communication; the Global Fund to Fight AIDS, Tuberculosis, and Malaria, the Permanent Secretary of the National Council against AIDS (SP/CNLS), Burkina Faso; the Association African Solidarity (AAS) at Ouagadougou; the NGO REV+ of Bobo-Dioulasso; and all others organizations that were involved in this study. They are grateful to all the study participants.
Funding
This study was funded by The USAID and Project SEARCH; Task Order No. 2, is funded by the US Agency for International Development under Contract No. GHH-I-00-0700,032–00. The Research Project is led by the Johns Hopkins Center for Global Health and managed by the Johns Hopkins Bloomberg School of Public Health Center for Communication Programs.
Author information
Authors and Affiliations
Contributions
HGO, SK, SB, and OKZ (study design, implementation, and manuscript writing); SZ (manuscript writing); KS and GT (data processing); and RB, HL, AR, TS, YT, and NB (manuscript review).
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ouedraogo, H.G., Zida, S., Compaore, T.R. et al. Seroepidemiology of syphilis among men who have sex with men in Burkina Faso, West Africa. Eur J Clin Microbiol Infect Dis 38, 1803–1809 (2019). https://doi.org/10.1007/s10096-019-03610-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03610-2