Abstract
Infections are among the top three causes of death of older adults in the first year after kidney transplantation (KT). Our aim was to describe infectious complications among KT recipients aged ≥ 65 during the first 12 months post-transplant. Single-center retrospective cohort study. Ninety-one KTs had been performed in patients ≥ 65 years of age between 2011 and 2015. 92.3% of the patients developed at least one infection. Infectious episodes increased the risk of future infection by 10% (p = 0.0018) with each infection portending a greater risk. At a patient level, viral (71.4%) and bacterial (70.2%) infections predominated. Urinary tract infections were the most frequent complication (30.3%), followed by cytomegalovirus infections (22.7%). Infections were the main reason for readmission. 7.7% of the patients developed rejection; and overall 3.3% lost their graft. Mortality at 1 year was 9.9%. Older KT recipients have a high incidence of infectious complications the first year after KT. Infections were the number one reason for readmission, and an infection episode predicted future infections for the individual patient. Despite these complications, the majority of older KT recipients were alive with a functioning graft at 1 year.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Older adults are the fastest growing group with end-stage renal disease and in increasing need of kidney transplantation. These individuals are at risk for infectious complications [1], not only due to the immunosuppression associated with transplantation but also due to aging-related immune senescence [2, 3].
Infections imply a higher incidence of morbidity and mortality in this group. Infection is among the top three causes of death among kidney transplant (KT) recipients, and death with a functioning graft is the most common form of graft loss in older adults [4,5,6].
A gap in knowledge exists regarding the infectious complications after kidney transplant in this group. Additionally, their clinical presentation is often atypical, making diagnosis challenging. Information in the literature mainly comprises traditional outcomes such as rejection, patient, and graft survival [7, 8]; information regarding infection specifics is limited [1, 9, 10].
Our aim was to describe infectious complications by syndrome and pathogen as well as 12-month outcomes among older KT recipients.
Material and methods
Study design and study center
This is a single-center retrospective cohort study of kidney-only transplants performed in adults aged ≥ 65 years between 2011 and 2015 at Duke University Medical Center; 551 KTs were performed during the study period. The study was approved by the Duke Institutional Review Board.
Patient cohort
An institutional tool, Duke Enterprise Data Unified Content Explorer (DEDUCE) [11] was used to identify all patients aged ≥ 65 that received a kidney-only transplant in the 5-year study period.
Our center-specific antimicrobial prophylaxis after KT included Pneumocystis jiroveci pneumonia (PJP) prophylaxis for 12 months and/or for 3 months after acute rejection, whichever was longer. Cytomegalovirus (CMV) prophylaxis depended on CMV serostatus [12]. For donor and recipient negative CMV serostatus, valacyclovir/acyclovir was used for 90 days if the herpes simplex serostatus was positive. For recipient CMV-positive serostatus, preemptive monitoring was performed, which included weekly CMV monitoring for 12 weeks, plus 90 days of valacyclovir/acyclovir if HSV serostatus was positive. High-risk patients (mismatches and CMV recipient serostatus positive after thymoglobulin induction) received ganciclovir/valganciclovir for 180 days; following cessation of prophylaxis, CMV PCR monitoring was performed every 2 weeks for a minimum of 3 months. Standard perioperative antibacterial prophylaxis included cefazolin or, if penicillin allergic, ciprofloxacin and clindamycin.
Induction immunosuppression protocols varied. Low-risk renal transplants got no induction; high risk got thymoglobulin induction (e.g., panel reactive antibodies (PRA) ≥ 30, historic donor-specific antibodies, per team discretion if at high risk for delayed graft function or for biopsy) and some high risk with contraindication to thymyglobulin received basiliximab. Targeted tacrolimus levels for maintenance therapy were 8–10 ng/ml (first month), 6–8 ng/ml (month 1–3) and 5–7 ng/ml (> 6 months).
Data extraction
Demographic, clinical, microbiological, and outcome data were extracted manually from the chart. Data collected were managed using REDCap™ data capture tool [13]. Infection data collection included information about infectious syndromes and microbiological data. Standard definitions and definitions per CDC/NSHN as described elsewhere were used [12, 14]. Ambulatory status was classified as “independent,” “needs assistance” (cane, walker), or “dependent.” Karnofsky scores prior to transplant and at approximately 1 year were collected.
Statistical analysis
Descriptive results are shown as total numbers/percentages, mean/standard deviations, and medians/interquartile range (IQR). Several types of infections were listed: pneumonia, urinary tract infection (UTI), surgical site infection (SSI), intraabdominal infection, blood stream infection (BSI), skin and soft tissue infection (SSTI), Clostridium difficile colitis, meningitis, osteomyelitis, prosthetic joint infection (PJI), hepatitis, sepsis, central line-associated bloodstream infection (CLABSI), candidemia, and other, as well as CMV and BK polyomavirus (BKV) infection. Coagulase-negative Staphylococcus BSI were only included when not deemed to be a contaminant. Patients were censored at death, or at the 1-year mark after KT, whichever occurred first, thus the rates of infections controlled for “time on study.” Several versions of infections were assessed: the total number of all types, the total number of unique types, and the number of infections within types. Further, since infections often co-occur on the same date, we calculated the number of unique dates (episodes) when an infection occurred. To address the question, “does the presence of an infection, increase the likelihood of subsequent infections?”, we employed proportional hazards modeling with recurrent events. Here, we modeled time-to-event (episode), with episode number as an only predictor. Assuming proportionality during the time between episodes, we assessed if the underlying hazards increased as the episode number increased. Statistical analysis was performed using SAS software, version 9.4. Copyright© SAS Institute Inc., Cary, NC, USA.
Results
Baseline characteristics
Ninety-one kidney-only transplants were performed between 2011 and 2015 in patients ≥ 65 years. Baseline characteristics of recipients and donors are shown in Tables 1 and 2. Median time from dialysis to transplant was 1308 days (range 38–4971), and median time on the waiting list was 589 days (range 0–2336). Further peri-transplant characteristics are shown in Table 3. The main underlying conditions responsible for renal disease were hypertension (42.9%) and diabetes mellitus (34.1%).
All patients received perioperative antibiotic prophylaxis for surgery per standard of care. Peri- and post-transplant prophylaxis included 90 patients (98.9%) receiving PJP and 58 (63.7%) antiviral prophylaxis.
Discharge location included 88 patients going home; one patient went on hospice. Of the 84 patients still alive at 1 year, at least 47.6% remained independent for ambulation, and 23.8% needed assistance; the median Karnofsky score was 70.
Infectious complications
Infectious complications occurred in 84 patients (92.3%). Infection was the main reason for readmission in the first year (58%), followed by laboratory abnormalities (25.5%) and surgical complications (20.4%).
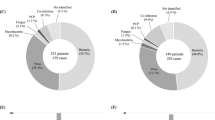
Infectious episodes increased the risk of future episodes with increasing risk (hazard ratios (HR)) with each additional infection. Relative to the baseline risk, each additional infection episode increased the HR by 10% (95% CI = 1.04, 1.17; p = 0.0018). Among patients with infection, 71.4% (60/84) developed viral, 70.2% (59/84) bacterial, 16.7% (14/84) fungal, and 1.2% (1/84) mycobacterial infections. For timing of infection based on infection type, see Fig. 1. Episode-specific infection data is shown in Table 4.
Viral infections
The most frequent infection in the first year after KT was CMV which occurred in 51 patients (56%), with 6 (11.7%) of these being primary infections. The median time to first peak viremia was 72 days (IQR 47–149).
BK viremia occurred in 28/91 (30%) patients with a median time to first detection of 102 days (IQR 77.8–168.8).
Bacterial infections
The most frequent bacterial infections were UTIs; 44 (48.4%) patients experienced at least one UTI. The median time to first UTI was 61.5 days (IQR 31.8–160.2). Seventy-nine cultures were available for review; the most frequent pathogens were gram-negative bacteria; mainly Klebsiella spp. (31.6%), Escherichia coli (17.7%), Enterobacter spp. (13.9%), and Pseudomonas spp. (11.4%). Among gram-positive infections, Enterococcus was most common (12.7%).
Bloodstream infections were the second most frequent type of bacterial infection with a total of 22 episodes in 17 (18.7%) patients. None met the definition for CLABSI. Median time to first BSI infection was 59 days (IQR 32–128). Twenty-three blood cultures were available for review; the most frequent pathogens were gram negatives, mainly Klebsiella (8) and E. coli (5), followed by gram positives such as coagulase-negative Staphylococcus (5) and Enterococcus (2). Eleven (12.1%) patients developed a SSI; median time to first SSI was 18 days (IQR 10–52.5). Enterococcus was the predominant pathogen recovered in 50% of the cultures. Nine (9.9%) patients developed pneumonia (10 episodes); median time to first episode was 74 days (IQR 20–150). Eight (8.8%) patients developed sepsis, a median of 163.5 days after KT (IQR 47–256.8). Seven (87.5%) of these episodes were associated with BSI.
C. difficile colitis occurred in 7 patients (7.7%), a median of 8 days after KT (IQR 7–17.5). Two patients suffered recurrent C. difficile-associated diarrhea.
Other
Fungal infections, primarily Candida, were documented in 14 (16.7%) patients, including one case of cryptococcal meningitis that presented 310 days after KT. There were no invasive mold infections.
Rejection, graft, and patient survival
Seven (7.7%) patients experienced rejection, six acute cellular and one humoral; the latter one resulting in graft loss. Overall, nine (9.9%) patients died during the first year; 2 (22.2%) deaths secondary to gram-negative sepsis occurred during the transplant admission. Eight (88.9%) patients died with a functioning graft. Three graft losses (3.3%) were reported in the first year.
Discussion
We describe outcomes including infectious complications in the first year after KT in adults ≥ 65 of age. The infection rate was very high, with 92.4% of patients experiencing at least one infectious complication. This is higher than the 67%–80% rate reported from comparable small series of similar aged patients [9, 15] and substantially higher than in younger cohorts (25.5%) [16]. Despite this very high number of infectious complications during the first post-transplant year, the number of deaths, graft rejections, and graft losses was low compared to similar aged patients [9].
Mortality during the first year after transplant (9.9%) was comparable to OPTN data for this age group but lower than other series [8, 9, 15, 17]. While it is known that older adults have lower rejection rates after transplant [7, 15, 18], our rate (8%) is extremely low. Other groups have described rejection rates ranging from 11 to 25% in patients with varying ages over 60 [9, 10, 15, 18, 19]. The paradox of higher infection and lower rejection rates in the aged KT population calls to question whether the older cohort is over-immunosuppressed, a consequence of too much exogenous immunosuppression and immunosenescence.
While outcomes after KT over the last 20 years have been improving [5, 8], the reasons for these favorable outcomes are likely multivariate, including improvements in surgical techniques and immunosuppressive regimens. The idea of individualized immunosuppression in older adults is not new [20] but has yet to be properly defined and implemented. The immunosuppressive regimens as well as the targeted levels of calcineurin inhibitors were not modified for older adults.
One might also question the impact of chronological versus physiological age of the recipient. By definition, older adults considered for any type of transplantation represent a highly selected subpopulation [7], although certainly not free of comorbidities. In the USA, no uniform criteria for pre-transplant evaluation of older KT candidates exist [21]. Studies have shown that transplantation in this age group offers a cardiovascular and mortality benefit over staying on dialysis [22,23,24,25,26]. Cardiovascular events in KT recipients develop at an annual rate of 3.5–5% [27]. Interestingly, in our series, although half of our patients had a history of cardiovascular disease, admissions in the first year after KT for cardiac causes were rare (2.2%).
The absence of standardized measurement of functional status and quality of life after KT in older adults is a major gap and opportunity for research and clinical care particularly since older adults rate independence as a critically important goal of care. A prior study in younger KT recipients addressed some subjective measures of functional status; worse functional status was associated with a shorter 3-year survival [28].
Looking more closely at the type and timing of infectious complications (Fig. 1), infections were most frequent between 1 and 6 months post-transplant. Further, BSI and UTIs for which gram negatives were the most common cause, peaked after the first month, raising the question of the urinary system as the source of BSI and the need for hospital readmissions.
UTIs are of distinct interest in KT recipients as they represent the most frequent infection [29,30,31]. Reasons for this include surgical manipulation of the urinary system during the procedure, stent placement, absence of a sphincter between the transplanted ureter and the bladder, non-functioning native kidneys that serve as potential reservoirs for bacteria and the use of Foley catheters. Other classic risk factors for UTIs are older age, female gender, acute rejection, and deceased donation [32, 33]. Surprisingly, in our cohort, most UTIs occurred 3 months after KT. One might expect that most infections happen early, as this is when the immunosuppression is most profound [34] and ureteral stents, if used, are still in place.
As anticipated, based on our preemptive prophylaxis protocol for intermediate risk recipients and universal prophylaxis in the high-serologic-risk group, CMV was the most common infectious pathogen emerging after the first month. Historically, increased age, positive serostatus of the donor, T cell depleting induction, rejection, and concomitant infection with other viruses have been associated with CMV disease [35, 36]. Our percentage of patients with CMV viremia is higher than anticipated in seropositive recipients (expected 15–25%). Over-immunosuppression, immunosenescence, or the fact that low-level viremias were included in our study could explain this finding. As shown in other studies, CMV tended to be delayed in onset after prophylaxis ended in the high-serologic-risk group [37].
Of special interest is the high incidence of BK viremia in this cohort (30%), on the higher end of the reported 13–30% [38, 39]. Again, we query if this represents a surrogate marker of over-immunosuppression.
A unique finding of our study is that infectious episodes increased the risk of future infections, each additional infection episode increased the HR by 10%. We speculate that this is multifactorial but could be a marker of worse immune function after acute infection. Further, it has been reported that the risk of dying of an infection is exponentially increased in older KT recipients [1]. These findings support the importance of early recognition and prevention of infectious complications in older adults, including proper pre-transplant immunizations, review of serologies and cultures of recipients and donors, adjustment of peri-procedure antimicrobial prophylaxis, individualized adjustment of immunosuppression, close follow-up, and potential immunologic profiling.
The limitations of this study include its retrospective single-center nature and sample size; local patterns may vary and should be taken into account when interpreting our results.
In conclusion, older KT recipients have a high incidence of infectious complications during the first year after surgery. Infections were the number one reason for readmission. Specifically, UTIs, BSI, CMV, and BKV are mainly responsible for an increased morbidity. Infectious episodes increased the risk of future infection by 10% which each infection portending a greater risk. Despite these complications, the majority of older KT recipients were alive with a functioning graft at 1 year although with possible reduced independence.
Future studies should include young transplant recipients to address questions regarding the effects of age on infections. Additionally, studies should include immunosuppressive levels, measures of functional status, frailty, and immune function as either direct or surrogate markers for overall immune function. Understanding the immunologic risk for infection and recognizing infection as a predictor of future infections is an area for study and targeted prevention strategies.
References
Meier-Kriesche HU, Ojo AO, Hanson JA, Kaplan B (2001) Exponentially increased risk of infectious death in older renal transplant recipients. Kidney Int 59(4):1539–1543. https://doi.org/10.1046/j.1523-1755.2001.0590041539.x
Gruver AL, Hudson LL, Sempowski GD (2007) Immunosenescence of ageing. J Pathol 211(2):144–156. https://doi.org/10.1002/path.2104
Kinnunen S, Karhapaa P, Juutilainen A, Finne P, Helantera I (2018) Secular trends in infection-related mortality after kidney transplantation. Clin J Am Soc Nephrol 13(5):755–762. https://doi.org/10.2215/cjn.11511017
Saran R, Li Y, Robinson B, Ayanian J, Balkrishnan R, Bragg-Gresham J, Chen JT, Cope E, Gipson D, He K, Herman W, Heung M, Hirth RA, Jacobsen SS, Kalantar-Zadeh K, Kovesdy CP, Leichtman AB, Lu Y, Molnar MZ, Morgenstern H, Nallamothu B, O'Hare AM, Pisoni R, Plattner B, Port FK, Rao P, Rhee CM, Schaubel DE, Selewski DT, Shahinian V, Sim JJ, Song P, Streja E, Kurella Tamura M, Tentori F, Eggers PW, Agodoa LY, Abbott KC (2015) US renal data system 2014 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis 66(1 Suppl 1):Svii):S1–S305. https://doi.org/10.1053/j.ajkd.2015.05.001
Matas AJ, Smith JM, Skeans MA, Thompson B, Gustafson SK, Stewart DE, Cherikh WS, Wainright JL, Boyle G, Snyder JJ, Israni AK, Kasiske BL (2015) OPTN/SRTR 2013 annual data report: kidney. Am J Transplant 15(Suppl 2):1–34. https://doi.org/10.1111/ajt.13195
Saucedo-Crespo H, Haakinson DJ, Croome KP, Mai ML, Taner CB, Heilman RL, Gonwa T (2016) Prognostic factors in kidney transplantation in the septuagenarian: a multicenter analysis. Clin Transpl 30(7):828–835. https://doi.org/10.1111/ctr.12756
Hod T, Goldfarb-Rumyantzev AS (2015) Clinical issues in renal transplantation in the elderly. Clin Transpl 29(2):167–175. https://doi.org/10.1111/ctr.12481
McAdams-DeMarco MA, James N, Salter ML, Walston J, Segev DL (2014) Trends in kidney transplant outcomes in older adults. J Am Geriatr Soc 62(12):2235–2242. https://doi.org/10.1111/jgs.13130
Trouillhet I, Benito N, Cervera C, Rivas P, Cofan F, Almela M, Angeles Marcos M, Puig de la Bellacasa J, Pumarola T, Oppenheimer F, Moreno-Camacho A (2005) Influence of age in renal transplant infections: cases and controls study. Transplantation 80(7):989–992
Neri F, Furian L, Cavallin F, Ravaioli M, Silvestre C, Donato P, La Manna G, Pinna AD, Rigotti P (2017) How does age affect the outcome of kidney transplantation in elderly recipients? Clin Transpl 31(10). https://doi.org/10.1111/ctr.13036
Horvath MM, Rusincovitch SA, Brinson S, Shang HC, Evans S, Ferranti JM (2014) Modular design, application architecture, and usage of a self-service model for enterprise data delivery: the Duke Enterprise Data Unified Content Explorer (DEDUCE). J Biomed Inform 52:231–242. https://doi.org/10.1016/j.jbi.2014.07.006
Ljungman P, Boeckh M, Hirsch HH, Josephson F, Lundgren J, Nichols G, Pikis A, Razonable RR, Miller V, Griffiths PD (2016) Definitions of cytomegalovirus infection and disease in transplant patients for use in clinical trials. Clin Infect Dis. https://doi.org/10.1093/cid/ciw668
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381. https://doi.org/10.1016/j.jbi.2008.08.010
CDC (2017) CDC/NHSN surveillance definitions for specific types of infections. https://www.cdc.gov/nhsn/pdfs/pscmanual/17pscnosinfdef_current.pdf
Kang SS, Park WY, Jin K, Park SB, Han S (2017) Kidney transplantation in Korean patients with end-stage renal disease aged 65 and older: a single-center experience. Transplant Proc 49(5):987–991. https://doi.org/10.1016/j.transproceed.2017.03.060
Cippa PE, Schiesser M, Ekberg H, van Gelder T, Mueller NJ, Cao CA, Fehr T, Bernasconi C (2015) Risk stratification for rejection and infection after kidney transplantation. Clin J Am Soc Nephrol 10(12):2213–2220. https://doi.org/10.2215/cjn.01790215
Kauffman HM, McBride MA, Cors CS, Roza AM, Wynn JJ (2007) Early mortality rates in older kidney recipients with comorbid risk factors. Transplantation 83(4):404–410. https://doi.org/10.1097/01.tp.0000251780.01031.81
Mendonca HM, Dos Reis MA, de Castro de Cintra Sesso R, Camara NO, Pacheco-Silva A (2007) Renal transplantation outcomes: a comparative analysis between elderly and younger recipients. Clin Transplant 21(6):755–760. https://doi.org/10.1111/j.1399-0012.2007.00734.x
Cho H, Yu H, Shin E, Kim YH, Park SK, Jo MW (2016) Risk factors for graft failure and death following geriatric renal transplantation. PLoS One 11(4):e0153410. https://doi.org/10.1371/journal.pone.0153410
Meier-Kriesche H, Ojo AO, Arndorfer JA, Leichtman AB, Lake K, Cibrik DM, Punch JD, Armstrong DR, Kaplan B (2001) Need for individualized immunosuppression in elderly renal transplant recipients. Transplant Proc 33(1–2):1190–1191
Mandelbrot DA, Fleishman A, Rodrigue JR, Norman SP, Samaniego M (2017) Practices in the evaluation of potential kidney transplant recipients who are elderly: a survey of U.S. transplant centers. Clin Transpl 31(10). https://doi.org/10.1111/ctr.13088
Rao PS, Merion RM, Ashby VB, Port FK, Wolfe RA, Kayler LK (2007) Renal transplantation in elderly patients older than 70 years of age: results from the scientific registry of transplant recipients. Transplantation 83(8):1069–1074. https://doi.org/10.1097/01.tp.0000259621.56861.31
Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, Held PJ, Port FK (1999) Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med 341(23):1725–1730. https://doi.org/10.1056/nejm199912023412303
Hernandez D, Alonso-Titos J, Armas-Padron AM, Ruiz-Esteban P, Cabello M, Lopez V, Fuentes L, Jironda C, Ros S, Jimenez T, Gutierrez E, Sola E, Frutos MA, Gonzalez-Molina M, Torres A (2018) Mortality in elderly waiting-list patients versus age-matched kidney transplant recipients: where is the risk? Kidney Blood Press Res 43(1):256–275. https://doi.org/10.1159/000487684
Legeai C, Andrianasolo RM, Moranne O, Snanoudj R, Hourmant M, Bauwens M, Soares J, Jacquelinet C, Couchoud C, Macher MA (2018) Benefits of kidney transplantation for a national cohort of patients aged 70 years and older starting renal replacement therapy. Am J Transplant. https://doi.org/10.1111/ajt.15110
Gill JS, Schaeffner E, Chadban S, Dong J, Rose C, Johnston O, Gill J (2013) Quantification of the early risk of death in elderly kidney transplant recipients. Am J Transplant 13(2):427–432. https://doi.org/10.1111/j.1600-6143.2012.04323.x
Ojo AO (2006) Cardiovascular complications after renal transplantation and their prevention. Transplantation 82(5):603–611. https://doi.org/10.1097/01.tp.0000235527.81917.fe
Reese PP, Shults J, Bloom RD, Mussell A, Harhay MN, Abt P, Levine M, Johansen KL, Karlawish JT, Feldman HI (2015) Functional status, time to transplantation, and survival benefit of kidney transplantation among wait-listed candidates. Am J Kidney Dis 66(5):837–845. https://doi.org/10.1053/j.ajkd.2015.05.015
Alangaden GJ, Thyagarajan R, Gruber SA, Morawski K, Garnick J, El-Amm JM, West MS, Sillix DH, Chandrasekar PH, Haririan A (2006) Infectious complications after kidney transplantation: current epidemiology and associated risk factors. Clin Transpl 20(4):401–409. https://doi.org/10.1111/j.1399-0012.2006.00519.x
Ak O, Yildirim M, Kucuk HF, Gencer S, Demir T (2013) Infections in renal transplant patients: risk factors and infectious agents. Transplant Proc 45(3):944–948. https://doi.org/10.1016/j.transproceed.2013.02.080
Parasuraman R, Julian K (2013) Urinary tract infections in solid organ transplantation. Am J Transplant 13(Suppl 4):327–336. https://doi.org/10.1111/ajt.12124
Camargo LF, Esteves AB, Ulisses LR, Rivelli GG, Mazzali M (2014) Urinary tract infection in renal transplant recipients: incidence, risk factors, and impact on graft function. Transplant Proc 46(6):1757–1759. https://doi.org/10.1016/j.transproceed.2014.05.006
Ooms L, IJ J, Voor In 't Holt A, Betjes M, Vos M, Terkivatan T (2017) Urinary Tract Infections After Kidney Transplantation: A Risk Factor Analysis of 417 Patients. Ann Transplant 22:402–408
Veroux M, Giuffrida G, Corona D, Gagliano M, Scriffignano V, Vizcarra D, Tallarita T, Zerbo D, Virgilio C, Sciacca A, Cappello D, Stefani S, Veroux P (2008) Infective complications in renal allograft recipients: epidemiology and outcome. Transplant Proc 40(6):1873–1876. https://doi.org/10.1016/j.transproceed.2008.05.065
De Keyzer K, Van Laecke S, Peeters P, Vanholder R (2011) Human cytomegalovirus and kidney transplantation: a clinician’s update. Am J Kidney Dis 58(1):118–126. https://doi.org/10.1053/j.ajkd.2011.04.010
Karuthu S, Blumberg EA (2012) Common infections in kidney transplant recipients. Clin J Am Soc Nephrol 7(12):2058–2070. https://doi.org/10.2215/cjn.04410512
Santos CA, Brennan DC, Fraser VJ, Olsen MA (2014) Delayed-onset cytomegalovirus disease coded during hospital readmission after kidney transplantation. Transplantation 98(2):187–194. https://doi.org/10.1097/tp.0000000000000030
Bressollette-Bodin C, Coste-Burel M, Hourmant M, Sebille V, Andre-Garnier E, Imbert-Marcille BM (2005) A prospective longitudinal study of BK virus infection in 104 renal transplant recipients. Am J Transplant 5(8):1926–1933. https://doi.org/10.1111/j.1600-6143.2005.00934.x
Hirsch HH, Knowles W, Dickenmann M, Passweg J, Klimkait T, Mihatsch MJ, Steiger J (2002) Prospective study of polyomavirus type BK replication and nephropathy in renal-transplant recipients. N Engl J Med 347(7):488–496. https://doi.org/10.1056/NEJMoa020439
Funding
Research reported in this publication was supported by the National Institute of Allergy and Infectious Diseases (NIAID) of the National Institutes of Health under award number 5T32AI100851 (MHM, BDA). Dr. Schmader was supported by the National Institute on Aging, Duke Pepper Older Americans Independence Center P30AG028716.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
For this type of study formal consent is not required.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Rights and permissions
About this article
Cite this article
Hemmersbach-Miller, M., Alexander, B.D., Sudan, D.L. et al. Single-center analysis of infectious complications in older adults during the first year after kidney transplantation. Eur J Clin Microbiol Infect Dis 38, 141–148 (2019). https://doi.org/10.1007/s10096-018-3405-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3405-5