Abstract
Acute hepatic illness is an important health issue in children. Our work aimed to determine the prevalence of viral hepatitis in symptomatic children. It is a prospective cohort study of 268 children presented with acute hepatitis. Complete blood count, liver panel, and anti-hepatitis A virus (HAV) IgM were done initially. Cases negative for HAV were tested for anti-hepatitis E (HEV) IgM, anti-Epstein-Barr virus viral capsid antigen (EBV VCA) IgM, anti-cytomegalovirus virus IgM, hepatitis B surface antigen, anti-hepatitis B core IgM antibody, and anti-HCV antibody. Anti-HCV was repeated after 12 weeks to exclude seroconversion. In cases with negative viral serology, ceruloplasmin, total immunoglobulin G, antinuclear antibody, and abdominal ultrasound were done. Follow-up visits were bimonthly till recovery, then after 6 months. The mean age ± SD was 7.1 ± 3.7 years (1.5–18), and 56% were males. Acute HAV infection was diagnosed in 260 (97%) of cases and acute EBV infection in one case (0.4%). HAV/HEV coinfection was excluded in 70 HAV-positive cases. Six (2.2%) children remain undiagnosed and one child lost follow-up. About 80% of HAV-cases had normal laboratory results within 45 days. Unusual presentation of HAV infection was noticed in six children: four (1.5%) were relapsing, one had a cholestatic course, and one case had severe hemolytic anemia. Acute HAV infection was the chief etiology of acute hepatitis in our Egyptian children. The majority of the presentations were mild and children recover within a few weeks. An unusual pattern of HAV in children can be observed in endemic areas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute hepatitis is an important health issue in children, with the magnitude of the problem the greatest in developing countries. Viral infections are the leading causes, mainly primary hepatotropic viruses (~ 90%), and to a lesser extent secondary and exotic hepatotropic viruses. Presentations are similar and cannot be differentiated clinically [1,2,–3]. Viral-type prevalence varies according to geographical areas and the local obligatory immunization schedule [4].
Hepatitis A virus (HAV) and hepatitis E virus (HEV) are primary hepatotropic viruses, which are transmitted by contaminated food and water, mainly by dirty hands [3, 5]. Infrequently, waterborne HAV-outbreaks occur due to sewage-contamination [2, 6]. Acute infection is usually self-limited with no chronic sequelae and provides lifelong immunity for HAV infection [2, 3, 5]. Both viruses have only a single serotype despite frequent well-known four genotypes in humans [7].
Acute hepatitis C virus (HCV) and acute hepatitis B virus (HBV) are rare during childhood. These blood-borne pathogens commonly produce chronic infections [8]. Cytomegalovirus (CMV) and Epstein-Barr virus (EBV) are secondary hepatotropic viruses, and in developing countries, the majority of children got infected via contact with body fluids of infected persons [9].
The aim of this study was to determine the prevalence of viral hepatitis among Egyptian children presenting with acute hepatitis and to describe the course of the disease.
Patients and methods
This is a prospective cohort study of children presenting with acute hepatitis. The protocol was approved by the corresponding ethical committee and recruitment was done after obtaining an informed consent from one of the parents. Patient enrollment was conducted from July 2015 to July 2017, at the Pediatric hepatology clinic, the National Hepatology and Tropical Medicine Research Institute.
Initial patient assessment
Acute hepatitis was defined as an acute illness of fewer than 15-day duration, with a discrete onset of constitutional symptoms, or elevated serum alanine aminotransferase (ALT) levels above 100 IU/mL documented at least twice at a 1-week interval without any history of a pre-existing liver disease [10]. Inclusion criteria were age between 1 and 18 years, both sexes with acute hepatitis. Children with co-existing chronic illness and those receiving long-term hepatotoxic drugs were excluded.
All children were subjected initially to full history taking and systemic and abdominal examination. Laboratory tests included complete blood count, where values were categorized according to normal for age and sex [11], and liver panel which included total bilirubin, direct bilirubin, ALT, aspartate aminotransferase (AST), alkaline phosphatase (ALP), gamma glutamyl transpeptidase (GGT), total proteins, serum albumin, prothrombin time (PT), and international normalized ratio (INR). Anti-HAV IgM was done in all cases, and anti-HEV IgM was tested for in the first 70 positive samples for HAV IgM, to exclude coinfection.
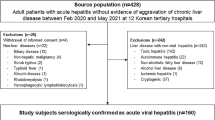
Viral serology for HAV-negative samples was done as follows: anti-HEV IgM, anti-Epstein-Barr virus, viral capsid antigen (EBV VCA) IgM, anti-CMV IgM, hepatitis B surface antigen (HBsAg), anti-hepatitis B core IgM antibody (HBc IgM), and anti-HCV Ab. Children with initial negative anti-HCV Ab were retested 12 weeks later to detect antibody seroconversion, as a more economical alternative for HCV RNA detection. For cases with negative viral serology, measurement of serum ceruloplasmin, total immunoglobulin G (IgG), antinuclear antibody (ANA), and abdominal ultrasound were done. Flowchart of the study group is shown in Fig. 1.
Patients were requested to come bimonthly for follow-up until normalization of abnormal values, then after 6 months from onset. During follow-up visits, total and direct bilirubin, ALT, and AST were retested.
Laboratory tests
A 5-ml venous blood sample was collected initially and at each subsequent visit, centrifuged, and the serum was stored at − 20 °C. Viral serology was done using ELISA technique.
The HAV IgM ELISA assay was done using General biologicals Corp for HAV IgM. It is a two-step capture method; in the first step, the sample and mouse monoclonal anti-human IgM coated microplate are combined. During the incubation, IgM antibodies present in the sample bind to the anti-human IgM-coated on the wells. After washing, in the second step, HAV antigens and enzyme conjugate are added to the wells. During the incubation, HAV antigens are allowed to react with the anti-HAV IgM bound to the microplate and enzyme-labeled antibodies, then a complex is generated among the solid phase, HAV antigens, and enzyme-linked antibodies by immunological reactions. After a second washing, substrate A and substrate B are then added and catalyzed by this complex, resulting in a chromogenic reaction. The resulting chromogenic reaction is measured as absorbance. The color intensity is proportional to the amount of anti-HAV in the sample.
The HEV IgM ELISA using DA-AccuDiagTMHEV-IgM. Antibody class IgM in the sample is first captured by the solid phase coated with anti-human-IgM antibody. After washing out all the other components of the sample including IgG antibodies, the specific IgM captured on the solid phase are detected by the addition of an HRP-conjugated HAV antigen. After incubation, microwells are washed to remove unbound conjugate and then the chromogen solutions are added. In the presence of peroxidase, the colorless chromogens are hydrolyzed to a colored end-product, whose optical density may be detected and is proportional to the amount of HAV IgM present in the sample.
Anti-Epstein-Barr virus, viral capsid antigen (EBV VCA) IgM was done using NovaLisa TM, GWB-4AC0FA, GenWay Biotech, Inc., San Diego, USA. Anti-cytomegalovirus virus (CMV) IgM using NovaLisa TM, GWB-3E8402, GenWay Biotech, Inc., San Diego, USA. HBs Ag was performed using ELISA technique; Abbott Murex. HBc IgM was performed using DiaSorin S.p.A., 13040 SALUGGIA (VERCELLI), Italy). HCV Ab was done using Pro diagnostic Bioprobes Srl via Columella no. 31 20128 Milano, Italy.
Statistical methods
Data were collected and tabulated. Data analysis was done using SPSS, version 17 (Statistical Package for Social Science, Chicago, IL 60606-6412, USA) program. Quantitative data were presented as a mean and standard deviation (SD) or median and interquartile range (IQR), while frequency and percentage were used for qualitative data. Chi-square test was used to compare clinical presentations, and one-way ANOVA was used to compare initial laboratory values of cases with hepatitis A, at different age groups. Paired sample t test for homogenous samples and Friedman test for non-homogenous samples were used to compare follow-up values with initial individual values. A two-sided P value < 0.05 was considered statistically significant.
Results
A total of 268 children with acute hepatitis were enrolled, their mean age ± SD was 7.1 ± 3.7 years (1.5–18), 56% were males, and ~ 90% have an appropriate weight for age centiles. The most common presenting symptoms were yellow sclera and dark urine. Anti-HAV IgM was positive in 260 (97%) children, anti-EBV VCA IgM was positive in one (0.4%), while 7 (2.6%) children remain undiagnosed.
Acute hepatitis A cases (n = 260)
Initially, children with acute hepatitis A had a mean age of 7.1 ± 3.7 years, and male/female ratio of 1:1.3. Demographic data and presentation of the children with acute hepatitis A are shown in Table 1. Examination revealed jaundice in 240 (92.3%), hepatomegaly in 54 (20.8%), and hepatosplenomegaly in 7 (2.7%) children. Initial laboratory results of patients are shown in Table 2. Diagnosis of acute HAV infection was more common in summer (34%) and winter (31%) seasons than in spring (20%) and autumn (15%).
Patients were categorized into four groups of different age ranges, and data are shown in Table 3. Comparing initial laboratory values among different age groups showed that ALP and GGT were significantly higher in the younger age groups (P = 0.001*, P = 0.02*, respectively). Values of total protein, albumin, and INR were significantly higher in the older age groups (P < 0.05 in all); data are not presented.
Children who came for follow-up visits were 208, and ~ 80% of them had normal liver functions within 45 days (Table 4). All liver panel values showed a significant decline on follow-up, except for ALP.
Acute hepatitis A cases with an unusual course (n = 6)
A relapsing course was noticed in four cases (1.5%), who had two acute hepatitis episodes positive for HAV IgM, 6 months apart. Also, a cholestatic course was noticed in a 16-year-old male, who experienced pruritus with increment in bilirubin levels on follow-up. In 12 weeks, he showed no manifestation and normal liver panel. Another 2-year-old male previously known to be HBs Ag-positive experienced severe hemolytic anemia (HB% = 5.9 g/dL—3% retics). HB% stepped to 9.6 g/dL following a single packed red cell transfusion and remains stable on follow up.
Acute hepatitis A cases with associated conditions
Twelve cases had associated medical conditions; 3 had type 1 diabetes mellitus, 2 were known to be HBs Ag-positive, 2 had glucose 6 phosphate dehydrogenase deficiency (G6PD), and each of the following in one epilepsy, psoriasis, Fallout tetralogy, hydatid cyst, and persistent fetal hemoglobin. Acute hepatitis recovered within 4–10 weeks in all patients. Persistent fetal hemoglobin was discovered accidentally in 6.5 years female.
Cases negative for HAV IgM (n = 8)
Only one child was positive for EBV VCA IgM, her clinical and laboratory derangements normalized in 6 weeks. The other cases were negative for all tests performed, with high total IgG level as per recommended for age and no HCV antibody seroconversion observed. A 5-year-old male presented with acute fulminant hepatitis of 15-day duration, with no history of drug intake. His weight was on the 75th percentile, presented with mild ascites, and an INR of 1.5 (Fig. 1).
Discussion
Acute hepatitis represented a common presentation among children attending the outpatient clinic. This study investigated 268 symptomatic children, where viral etiology was evident in 97.4% of them. Acute HAV infection was diagnosed in 260 (97%) and acute EBV infection in one (0.4%) child. HEV coinfection was excluded in 70 cases of acute HAV infection, and 7 (2.6%) children remain undiagnosed. In Egypt, HAV vaccine is not included in obligatory vaccination schedule.
In our cohort, acute HAV was the most prevalent viral infection. This is justified by the fact that Egypt is an area of moderate-to-high endemicity for HAV infection [2]. Prevalence of acute HAV in children varies from one area to another, and studies in developing countries reported rates from 27 to 57% [12, 13].
Among our cohort, ~ 13% with acute HAV gave a history of contact with a jaundiced patient, mainly a family member. Other studies reported a higher percentage of known exposure, in 28.5% of their studied children [14]. Although household contact with an infected sibling is the main risk factor [2, 6], the highest infectivity period always precedes symptoms [15], and thus exposure could be missed.
Age classification of studied children with acute HAV showed that infants and young children represented the major proportion of patients (72.3%). No gender predilection observed except in the older age group, where males were more commonly infected than females. Worldwide, there was a universal agreement towards an epidemiological shift of age at first HAV-exposure towards school age and adolescence. This paradigm shift is contributed to partially improved living conditions, with subsequent risk of possible outbreaks and high case fatality [2, 16]. The absence of gender predilection in children below 18 years was generally agreed upon [14].
Among cases who completed follow-up, about 80% had complete recovery after a mean period of 45 days. The rest recovered within the 6-month follow-up period. Similarly, Kumar et al. [17] and Quirós-Tejeira et al. [18] reported complete recovery of most of their studied children within 2 months. Recovery within 6 months was generally agreed [2].
Unusual presentation of acute HAV infection was observed in 6 (2.3%) children in our study, as relapsing, cholestatic course or associated with hemolysis. The paucity of relapsing or cholestatic course in children with HAV was agreed by many reports, with a prevalence ranged between 1.2 and 2% of cases [14, 17]; meanwhile, Ciocca [19] reported that atypical HAV course may reach up to 7%. Although autoimmune hemolytic anemia is a rare extrahepatic manifestation that may accompany HAV infection [20], cases are observed in countries endemic for HAV.
None of the studied children with HAV was presented with acute fulminant hepatitis and no mortality reported. Liver failure is rare in immunocompetent children without underlying liver affection, which was estimated to be ~ 0.2% [1, 2, 4, 14]. On the other hand, Kumar et al. [17] and Ciocca et al. [21] reported a high incidence of acute liver failure with coagulopathy, observed in up to 15% of their studied children with acute HAV.
Within the studied cohort, only one patient was diagnosed with a benign course of acute EBV infection, and none was diagnosed with acute CMV infection. Our findings are in agreement with that EBV infection in immunocompetent children present mainly with a self-limited pattern of liver functions derangements [22]. Also, acute CMV-hepatitis is common only in immunocompromised, while it is asymptomatic in immunocompetent [23]. Prevalence of secondary hepatotropic viruses differs geographically. In a Canadian study for hospitalized children with acute hepatitis, Cybulska and colleagues [4], reported a low rate of acute EBV hepatitis; meanwhile, they reported more frequent acute CMV-hepatitis. All children with acute CMV or EBV infection were immunocompetent and required no treatment.
Among the studied group, neither acute HEV infection nor HAV/HEV coinfection was diagnosed in examined samples (n = 70). In a rural study for Egyptian adolescents and young adults, only 0.9% with acute hepatitis had positive anti-HEV IgM (median age was 16 years, IQR 13–22) [24]. Another study demonstrated that the majority of Egyptian rural-inhabitants were positive for HEV-IgG, without a previous history of acute hepatitis [25]. In endemic areas for HAV and HEV, HAV predominates in children, while HEV predominates in young adults, with no clear explanation [25, 26]. On the opposite side, acute HEV was diagnosed in 9.8% of Indian children with acute hepatitis, and among them, 8% had coinfection with HAV/HEV [13].
Among our cases negative for HAV infection, none was diagnosed with acute HBV or acute HCV. Compulsory HBV vaccination is given in Egypt since late 1992 with a marked decline in HBV rates. Moreover, in a study from India, 9.8% of children were diagnosed with acute HBV [13]. Lucky enough, acute HCV is very rare in children [8].
Our study limitations included that not all patients completed the follow-up period, and relevant studies used different viral-detection tests. In our study, the antibodies-IgM class was used for diagnosis of acute HAV/HEV infection, based on international recommendations, which recommend the addition of HEV RNA testing only in immunocompromised patients [5, 27, 28].
In conclusions, acute HAV infection is the chief etiology of acute hepatitis in Egyptian children. Most cases are mild and recover spontaneously within a few weeks. Although an atypical pattern of HAV is rarely detected in children, it can be observed in endemic areas.
References
Daniels D, Grytdal S, Wasley A (2009) Centers for Disease Control and Prevention (CDC). Surveillance for acute viral hepatitis—United States, 2007. MMWR Surveill Summ 58(3):1–27
WHO fact sheet (2017) http://www.who.int/mediacentre/factsheets/fs328/en/. Reviewed July 2017, Accessed November 2017
Global Burden of Disease Study C (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet 386(9995):743–800
Cybulska P, Ni A, Jimenez-Rivera C (2011) Viral hepatitis: retrospective review in a Canadian pediatric hospital. ISRN Pediatr; 182964. https://doi.org/10.5402/2011/182964
Centers for disease control and prevention (CDC) (2014) Hepatitis A information for health professionals-statistics and surveillance. https://www.cdc.gov/nchs/data/phcrs/phcrs72.pdf. Accessed 10Jan 2018
Melhem NM, Talhouk R, Rachidi H, Ramia S (2014) Hepatitis A virus in the middle East and North Africa region: a new challenge. J Viral Hepat 21:605–615
Purcell RH, Emerson SU (2008) Hepatitis E: an emerging awareness of an old disease. J Hepatol 48:494–503
Sharland M (2016) Hepatitis B & Hepatitis C. In: Manual of Childhood Infections, 4th edn. Oxford University Press, New York, p 589–93
Cannon MJ, Schmid DS, Hyde TB (2010) Review of cytomegalovirus seroprevalence and demographic characteristics associated with infection. Rev Med Virol 20:202–213
Centers for Disease Control and Prevention (CDC) (2012) National notifiable diseases and conditions and current case definitions. Available from: http://www.cdc.gov/nndss/document/2012_Case%20Definitions.pdf. Accessed on 2014 November
Stanley F (2016) Reference intervals for laboratory tests and procedures. In: Kliegman RM, Stanton BF, Schor NF, St Geme III JW, Behrman RE (eds) Nelson textbook of pediatrics, 20 edn. p 3465-6
Ayoola A, Aderoju A, Gadour MO, Al-Hazmi M, Hamza MK, Ene D et al (2001) Serological profile of sporadic acute viral hepatitis in an area of hyper-endemic hepatitis B virus infection. Saudi J Gastroenterol 7(3):95–102
Jain P, Prakash S, Gupta S, Singh KP, Shrivastava S, Singh DD et al (2013) Prevalence of hepatitis a virus, hepatitis B virus, hepatitis C virus, hepatitis D virus and hepatitis E virus as causes of acute viral hepatitis in North India: a hospital based study. Indian J Med Microbiol 31(3):261–265
Çetinkaya B, Tezer H, Özkaya Parlakay A, Revide Sayli T (2014) Evaluation of pediatric patients with hepatitis A. J Infect Dev Ctries 8(3):326–330
Jacobsen KH, Wiersma ST (2010) Hepatitis A virus seroprevalence by age and world region, 1990 and 2005. Vaccine 28(41):6653–6657
Jacobsen KH (2014) Hepatitis A virus in West Africa: is an epidemiological transition beginning? Niger Med J 55(4):279–284
Kumar KJ, Kumar HC, Manjunath VG, Anitha C, Mamatha S (2014) Hepatitis A in children- clinical course, complications and laboratory profile. Indian J Pediatr 81(1):15–19
Quirós-Tejeira RE, Edwards MS, Rand EB, Hoppin AG (2016) Overview of hepatitis A virus infection in children. At UpToDate: http://www.uptodate.com Last updated: Mar 31, 2016. Accessed February 2018
Ciocca M (2000) Clinical course and consequences of hepatitis A infection. Vaccine 18(Suppl 1):S71–S74
Miri-Aliabad G, Rashidi S (2017) Immune thrombocytopenic purpura and hemolytic anemia secondary to hepatitis A. Int J Hematol Oncol Stem Cell Res 11(2):89–91
Ciocca M, Ramonet M, Cuarterolo M, López S, Cernadas C, Álvarez F (2008) Prognostic factors in paediatric acute liver failure. Arch Dis Child 93(1):48–51
Crum NF (2006) Epstein Barr virus hepatitis: case series and review. South Med J 99(5):544–547
Cisneros-Herreros JM, Herrero-Romero M (2006) Hepatitis due to herpes group viruses. Enferm Infecc Microbiol Clin 24:392–397
Delarocque-Astagneau E, Abravanel F, Moshen A, Le Fouler L, Gad RR, El-Daly M et al (2012) Epidemiological and virologicalcharacteristics of symptomatic acutehepatitis E in greater Cairo, Egypt. Clin Microbiol Infect 18(10):982–988
Blackard JT, Rouster SD, Nady S, Galal G, Marzuuk N, Rafaat MM et al (2009) Genotypic characterization of symptomatic hepatitis E virus (HEV) infections in Egypt. J Clin Virol 46:140–144
Franco E, Meleleo C, Serino L, Sorbara D, Zaratti L (2012) Hepatitis A: epidemiologyand prevention in developing countries. World J Hepatol 4:68–73
Clinical Effectiveness Group (BASHH) (2008) United Kingdom national guideline on the management of the viral hepatitides A, B & C. British Association for Sexual Health and HIV (BASHH), London (UK) Available at: http://www.bashh.org/documents/1927.pdf
Health Protection Agency (HPA) (2009) Guidance for the prevention and control of hepatitis A infection. Available at: http://webarchive.nationalarchives.gov.uk/20140714084352/http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1259152095231. Accessed September 30, 2014
Acknowledgments
I would like to thank all the Pediatric team at NHTMRI, in particular, Dr. Hany Abd Elaziz, for their continuous support and dedicated work.
Funding
This work was funded by the National Hepatology and Tropical Medicine Research Institute, Cairo, Egypt.
Author information
Authors and Affiliations
Contributions
Hanan Mina Fouad: idea, clinical follow up of children, collection of data, and writing draft of manuscript.
Ehab Mahfouz Read: biochemical analysis and approved the final manuscript.
Amany Gmal El-Din: biochemical analysis and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the corresponding ethical committee.
Informed consent
Informed consent was obtained from one of the parents.
Rights and permissions
About this article
Cite this article
Fouad, H.M., Reyad, E.M. & El-Din, A.G. Acute hepatitis A is the chief etiology of acute hepatitis in Egyptian children: a single-center study. Eur J Clin Microbiol Infect Dis 37, 1941–1947 (2018). https://doi.org/10.1007/s10096-018-3329-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3329-0