Abstract
With regard to increasing number of antifungal-resistant dermatophytes, antifungal susceptibility testing of dermatophytes serves as a useful tool in managing clinical dermatophytosis. This study aimed to determine antifungal susceptibility profile of clinically important dermatophytes and determination of point mutations in terbinafine-resistant isolates. Based on our results, dermatophytosis was confirmed in 97 cases by direct microscopic examination, culture, and sequencing of ITS region. Antifungal susceptibility of 97 dermatophyte isolates distributed in four species including Trichophyton interdigitale (26 isolates), T. rubrum (19 isolates), T. tonsurans (29 isolates), and Epidermophyton floccosum (21 isolates) was assessed to nine antifungal agents using CLSI M38-A2 guidelines. Minimum inhibitory concentration range (MIC range) for luliconazole and terbinafine was 0.001–0.008 μg/ml and 0.003–> 32 μg/ml, compared to 0.03–64 μg/ml for griseofulvin, 0.01–16 μg/ml for itraconazole and voriconazole, 0.03–8 μg/ml for ketoconazole, 0.03–32 μg/ml for econazole, 0.03–1 μg/ml for lanoconazole, and 0.01–4 μg/ml for butenafine. Trichophyton tonsurans was the most susceptible (MIC = 0.006 μg/ml) and E. floccosum was the most resistant (MIC = 0.02 μg/ml) species to terbinafine. Terbinafine resistance was reported for two species, i.e., T. rubrum and T. tonsurans at the total rate of 2% which was due to Leu393Phe substitution in both species. Taken together, our results assist clinicians and prompt the current knowledge about the necessity of antifungal susceptibility testing to select effective strategies for management of clinical cases of dermatophytosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antifungal susceptibility testing of dermatophytes is a helpful tool for managing patients with different types of dermatophytosis [1]. It has been estimated that over 500 million $ per year spent for treatment of dermatophyte infections [2]. The increased use of antifungal drugs, often for prolonged periods, has led to the recognition of the phenomenon of acquired antifungal resistance [3]. A number of antifungal agents have been recommended for treating all types of dermatophytosis. Because of provides long-term clinical efficacy and lower relapse [4], terbinafine (TER) is considered as the best choice drug for treatment of dermatophytosis [5, 6]. Unfortunately, reports of drug-resistant strains to TER are increasing by the year [7,8,9]. Terbinafine is an allylamine antifungal drug that acts as an inhibitor of squalene epoxidase (SQLE), a crucial enzyme involved in ergosterol biosynthesis [10]. Inhibition of this enzyme leads to accumulation of squalene inside the fungal cells, depletion of ergosterol, and finally causes cell death [9, 11]. The molecular mechanisms of TER resistance in T. rubrum clinical strains have been investigated in different studies [8, 10, 12,13,14,15]. Furthermore, TER resistance has been reported in clinical T. interdigitale isolates [8, 15]. The resistance mechanism involves the single point mutations at one of four positions (Leu393, Phe397, Phe415, and His440) of the SQLE protein [8, 10, 12,13,14,15]. However, no effective mutations mediated by efflux transporter genes of the ATP-binding cassette (ABC) or the major facilitator superfamily (MFS) transporter family have yet been reported in dermatophyte isolates [8]. Previous studies have focused on T. rubrum and T. interdigitale isolates resistant to TER [8, 10, 12,13,14,15]. In the present study, in addition to T. rubrum, point mutations of T. tonsurans and E. floccosum isolates resistant to TER were investigated. Likewise, in vitro antifungal activity of common and new antifungal drugs including TER, griseofulvin (GRI), itraconazole (ITC), voriconazole (VOC), luliconazole (LUL), lanoconazole (LAN), ketoconazole (KTC), butenafine (BUT), and econazole (ECO) was assessed against 97 dermatophyte isolates using CLSI broth microdilution M38-A2 method together with evaluating point mutations in strains resistant to TER for the first time in Iran.
Materials and methods
Chemical antifungal drugs
All tested antifungal drugs except terbinafine which was obtained from Dr. Reddy’s Laboratories were purchased from Sigma-Aldrich (St. Louis, MO, USA). Compounds were dissolved in dimethylsulfoxide (Sigma-Aldrich®, St. Louis, USA) at a final concentration of 10 mg/ml.
Clinical fungal isolates
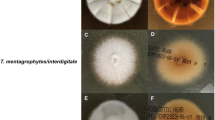
Clinical samples obtained from patients suspected to dermatophytosis referred to the Department of Mycology of the Pasteur Institute of Iran were examined for etiologic dermatophytes. Identification of isolates was primarily carried out using direct microscopy and culture and confirmed by ITS sequencing. A total 97 identified dermatophyte isolates including T. rubrum (n = 19), T. interdigitale (n = 26), T. tonsurans (n = 29), and E. floccosum (n = 23) were included in this study. Reference strains of T. rubrum (PFCC 51431) and T. mentagrophytes (PTCC 5054) were tested in all steps. The datasets generated during the current study are available in the Pathogenic Fungi Culture Collection repository, http://fa.pasteur.ac.ir/MBankResult.aspx.
Molecular identification by PCR assay and sequencing targeting ITS region
All dermatophyte strains were cultured on mycobiotic agar (Merck, Germany) and incubated at 28 °C for 7 days. DNA was extracted using the chloroform and proteinase K method. The fungal mycelium was disrupted by Pestle in presence of liquid nitrogen and DNA extraction buffer (200 M Tris-HCl, pH 8, 25 mM EDTA, SDS 0.5% W/V, NaCl 250 mM). After that, the mixture was vortexed, proteinase K was added, and total content was incubated at 55 °C for 60 min. The DNA was extracted with an equal volume of chloroform. Total nucleic acids were precipitated with isopropanol, washed in 300 μl ethanol 70%, air-dried, rehydrated in 50 μl TE buffer, and stored at − 20 °C till it was used [16].
The ITS region was PCR amplified using primers ITS1 (5′-TCCGTAGGTGAACCTGCGG-3′) and ITS4 (5′-TCCTCCGCTTATTGATATGC-3′) [17]. Each mixture contained 12.5 μl of Premix, 1 μl of DNA template, 0.3 μM of each primer, and enough water to reach a final reaction volume of 25 μl. Negative controls (water instead of fungal DNA) were added to each PCR. The reaction mixture was initially denatured at 95 °C for 5 min followed by 30 cycles of 30 s at 94 °C, 30 s at 56 °C, and 45 s at 72 °C, and a terminal extension step of 72 °C for 5 min. Five microliters of the PCR products was electrophoresed on 1% agarose gel in TAE buffer and then observed and photographed under ultraviolet irradiation.
Antifungal drug susceptibility testing
Stock solutions of antifungal drugs were prepared in dimethyl sulfoxide (DMSO) (Sigma-Aldrich, St. Louis, MO, USA) according to CLSI M38-A2 broth microdilution protocol [18] and diluted in standard RPMI 1640 medium buffered to pH 7.0 with 0.165 mol/l 3-(N-morpholino)propanesulfonic acid (MOPS) with L-glutamine without bicarbonate (Sigma-Aldrich, St. Louis, MO, USA). The final concentration of drugs, fungal spore suspensions, and drug dilutions was prepared according to CLSI M38-A2 broth microdilution protocol [18]. All the dermatophytes were exposed to different concentrations of antifungal drugs in 96-well round bottom microplates. The inoculated microplates were incubated at 35 °C and visually assessed for fungal growth after 4 days incubation. The MIC was defined as the point at which the growth of dermatophyte was inhibited by 80% for eight antifungals in comparison with the control. All tests were performed in duplicate. Trichophyton rubrum (PTCC 5143) and C. parapsilosis (ATCC 22019) were used as quality controls. MIC range, geometric mean, MIC50, and MIC90 were provided for all the isolates tested.
PCR assay targeting the SQLE region
For SQLE gene amplification, a novel set of pan-dermatophyte primers was designed manually with lasergene 7 software as Drsq1 (5′-TTGCCAACGGAGGTGTAAAG-3′) and Drsq2 (5′-GGGGCCATCTATAAGTCCAAGTT-3′). This primer designed by use of DNA sequence of clinical T. rubrum isolated NFI 5166 [13]. The PCR was performed using a Taq DNA Polymerase Master Mix, with primers Drsq1/2. Each mixture contained 25 μl of Premix 3 μl of DNA template, 0.6 μM of each primer, and enough water to reach a final reaction volume of 50 μl. Negative controls were added to each PCR. The reaction mixture was initially denatured at 95 °C for 5 min, followed by 30 cycles of 30 s at 94 °C, 30 s at 58 °C, and 45 s at 72 °C, and a terminal extension step of 72 °C for 5 min. Five microliters of the PCR products (520 bp) was electrophoresed on 1% agarose gel in TAE buffer and then observed and photographed under ultraviolet irradiation.
ITS and SQLE sequencing
The PCR products of ITS and SQLE regions were sequenced by the ABI PRISM BigDye Terminator Cycle Sequencing Ready Reaction Kit. The forward and reverse sequences of isolates showing reduced susceptibility to TER were subjected to ClustalW pairwise alignment using the MEGA7.0.21 software and edited manually to improve the alignment accuracy [10].
Statistical analysis
Quantitative data of MIC range, geometric mean MIC, MIC50, and MIC90 were subjected to statistical analysis of one-way ANOVA and multiple comparisons test using the statistical SPSS package version 19. P values of < 0.05 were considered significant.
Results
Clinical features of studied dermatophytes
General features of 97 dermatophyte isolates studied in the present work are summarized in Table S1. Among the 97 patients, 77.3% were male and 22.7% were female distributed in the age range of 2 to 77 years. The most common infected age group was the 21 to 30 years (Fig. 1A). Tinea pedis (29.8%) and tinea cruris (29.8%) were the most common types of dermatophytosis followed by tinea corporis (18.5%), tinea capitis (9.2%), tinea faciei (6.1%), and tinea manuum (2%). The difference between the prevalence of tinea pedis in men and women was statistically significant and the most common species involved was T. interdigitale. Also, E. floccosum in tinea cruris was the most frequent fungal pathogen, followed by T. tonsurans in other anatomical sources. Overall, T. tonsurans was the most important dermatophyte regard to infecting various anatomical sites (Fig. 1B).
Identification of dermatophytes by ITS-PCR sequencing
All dermatophyte isolates further identified by ITS-rDNA region sequencing. The query sequences were paired with those in the GenBank database by the Blast analysis. The sequences were deposited in the GenBank ITS-rDNA and the nucleotide sequences of the following accession numbers were considered: T. interdigitale: MF109036-MF109062, T. rubrum: MF155577-MF155596, T. tonsurans: MH337848, MF158259-MF158287, and E. floccosum: MF158288-MF158310.
Antifungal susceptibility of dermatophyte isolates
The MIC range, geometric mean MIC, MIC50, and MIC90 were obtained by the CLSI method for the dermatophyte species against the eight antifungals tested (Table 1). LUL susceptibility was tested against isolates resistant to other drugs (Table 2). A significant sensitivity to TER was reported in T. tonsurans (MIC50 = 0.006 μg/ml). The most susceptible and resistant species to GRI were T. interdigitale (MIC50 = 0.12 μg/ml) and E. floccosum (MIC50 = 1.0 μg/ml), respectively. TER and GRI had the lowest and the highest geometric mean MICs which were 0.01 and 1.64 μg/ml for T. interdigitale and E. floccosum, respectively. TER was the most effective antifungal drug against all dermatophyte species (Table 1). Among 99 tested isolates, 5 (2 isolates of T. rubrum, 2 isolates of T. tonsurans, and 1 isolate of E. floccosum) showed reduced TER susceptibility.
Point mutations detected in the SQLE gene of terbinafine-resistant isolates
After amplification of the genomic DNAs of five isolates that showed reduced susceptibility to TER by the PCR using Drsq, the expected size (520 bp) of the product for each species was generated in all cases. The forward and reverse sequences of each sample were subjected to ClustalW pairwise alignment using the MEGA7.0.21 software and edited manually to improve the alignment accuracy (Fig. S1). The data were compared in GenBank using the BLASTn. Then, the nucleic acid sequence converts to the amino acid sequence, the alignment of these amino acid is presented in Fig. S2. Among 5 isolates which showed reduced susceptibility to terbinafine, only 2 isolates (89_610, 92_256) with MICs > 32 showed amino acid substitution at position (Leu393Phe) of the squalene epoxidase protein. In both of these isolates were found A- to -T substitutions at position 1179 of the squalene epoxidase partial sequence gene, leading to the replacement of 393 by Phe in the squalene epoxidase protein. The DNA sequences of two TER resistant isolates have been deposited in the GenBank with the accession numbers of MH523150 for T. rubrum and MH523151 for T. tonsurans.
Discussion
In the present study, 97 isolates of dermatophytes isolated from clinical cases of dermatophytosis were identified at species level and subjected to antifungal susceptibility testing to nine antifungal drugs and resistance mechanisms to terbinafine. Besides the global importance of dermatophytosis as the commonest superficial infection in the world, in vitro susceptibility testing plays an essential role to determine emerging resistance patterns among etiologic dermatophytes. Generally, TER therapy is considered as common therapeutic strategy for curing clinical dermatophytosis. In a few studies, the point mutation in T. rubrum and T. interdigitale isolates resistant to TER has been investigated. In this study, in addition the point mutation of T. rubrum isolates resistant to terbinafine, for the first time point mutations of T. tonsurans and E. floccosum isolates that showed reduced TER susceptibility were investigated. According to the previous studies, relatively low levels of TER resistance were recorded in dermatophyte strains, proving that this drug encompasses suitable activity on a variety of clinical strains. In the present study, TER showed a variable range of activity against the different species of Trichophyton (MICs of 0.003–2) and Epidermophyton (MICs of 0.003–1). MICs of ITC and VOC for Trichophyton and Epidermophyton species were almost equal, while MICs of KTC, ECO, LAN, and BUT for T. rubrum species were higher than the other species. Our results highlight the usefulness of TER in majority cases of dermatophytosis especially in infections caused by GRI resistance species. This finding is in accordance with previous investigations [9, 19].
The MIC50 for LUL was 0.004 μg/ml against isolates which were resistant to other drugs while it was 0.01 μg/ml for terbinafine against all tested isolates. Interestingly, all isolates resistant to tested antifungal drugs even those resistant to terbinafine were susceptible to luliconazole. This is in accordance with the reports of Wiederhold et al. [20] and Baghi et al. [21].
In the present study, the Gm MIC of TER was lower for T. interdigitale and T. tonsurans and higher for T. rubrum and E. floccosum than that those reported by Ansari et al. [22]. Also, the Gm MIC of ITC for T. rubrum, T. interdigitale, and T. tonsurans was lower than that of Esteban et al. [23] and Adimi et al. [24].
According to our results, the MIC of GRI against 99 dermatophyte isolates was in the range of 0.03 to 64 μg/ml. T. interdigitale was the most susceptible species to GRI (MIC50, 0.12 μg/ml). GRI showed the reduced susceptibility to E. floccosum (MIC50, 1 μg/ml). These results are in agreement with the report by Nowrozi et al. [25].
It has been shown that the resistance mechanism of dermatophytes for TER is related to the single point mutations at one of four positions (Leu393, Phe397, Phe415, and His440) of the SQLE protein [8, 10, 12,13,14,15]. Recently, Yamada et al. [8] reported a TER resistant rate of 1% which mainly included T. rubrum isolates. In the present study among 97 tested isolates, 5 (5%) showed reduced terbinafine susceptibility, of which 2 were found to be related to amino acid substitution Leu393 by Phe in the squalene epoxidase protein. This is in accordance with the reports by other investigators [8, 10, 15]. Singh et al. [15] reported the substitution Phe397Leu and Leu393Phe in TER resistant T. interdigitale isolates, while Yamada et al. [8] showed the substitution in Phe397Leu as the resistance mechanism to TER. We did not find resistance to TER in 27 tested T. interdigitale isolates.
Strain resistance to TER has been reported for dermatophytes isolated from tinea pedis and tinea unguium [8, 15]. We reported TER resistance for dermatophytes isolated from tinea pedis and tinea corporis. Interestingly, in the study by Singh et al. [15], of 20 patients infected with TER resistant T. interdigitale isolates, 10 did not respond to TER therapy. Also, Yamada et al. [8] reported that 8 of the 17 patients with TER resistant etiologic dermatophytes were resistant to TER therapy.
Taken together, results of the present study further indicate the importance of dermatophytes as fungal pathogens of the skin and nail and confirms the necessity of antifungal susceptibility testing to choose effective drugs and efficient management strategies of clinical case of dermatophytosis. Likewise, increasing resistance to TER as the choice drug for treatment of dermatophytosis even in new species like as T. rubrum and T. tonsurans reported by us in the present shows the urgent of caring with the use of antifungal drugs at the clinic and stressed the necessity of follow up the patient’s condition after antifungal treatment.
References
Shehata AS, Mukherjee PK, Ghannoum MA (2008) Comparison between the standardized clinical and laboratory standards institute M38-A2 method and a 2,3-bis 2-methoxy-4-nitro-5-[(sulphenylamino) carbonyl]-2H-tetrazolium hydroxide-based method for testing antifungal susceptibility of dermatophytes. J Clin Microbiol 46:3668–3671
Achterman R, White T (2012) A foot in the door for dermatophyte research. PLoS Pathog 8:1–4
Favre B, Hofbauer B, Hildering KS, Ryder NS (2003) Comparison of in vitro activities of 17 antifungal drugs against a panel of 20 dermatophytes by using a microdilution assay. J Clin Microbiol 41:4817–4819
Lupi O, Tyring SK, McGinnis MR (2005) Tropical dermatology: fungal tropical diseases. J Am Acad Dermatol 53:931–951
Roberts BJ, FriedIander SF (2005) Tinea capitis: a treatment update. Pediatr Annal 34:191–200
Gupta A, Summerbell R (2000) Tinea capitis. Med Mycol 38:255–287
Mukherjee PK, Leidich SD, Isham N, Leitner I, Ryder NS, Ghannoum MA (2003) Clinical Trichophyton rubrum strain exhibiting primary resistance to terbinafine. Antimicrob Agents Chemother 47:82–86
Yamada T, Maeda M, Alshahni MM, Tanaka R, Yaguchi T, Bontems O, Salamin K, Fratti M, Monodd M (2017) Terbinafine resistance of Trichophyton clinical isolates caused by specific point mutations in the squalene epoxidase gene. Antimicrob Agents Chemother 61:115–117
Afshari M, Shams-Ghahfarokhi M, Razzaghi-Abyaneh M (2016) Antifungal susceptibility and virulence factors of clinically isolated dermatophytes in Tehran, Iran. Iran J Microbiol 8:36–46
Osborne CS, Leitner I, Favre B, Ryder NS (2005) Amino acid substitution in Trichophyton rubrum squalene epoxidase associated with resistance to terbinafine. Antimicrob Agents Chemother 49:2840–2844
Ghannoum MA, Chaturvedi V, Espinel-Ingroff A, Pfaller MA, Rinaldi MG, Lee-Yang W, Warnock DW Intra- and interlaboratory study of a method for testing the antifungal susceptibilities of dermatophytes. J Clin Microbiol 42:2977–2979
Mukherjee PK, Leidich SD, Isham N, Leitner I, Ryder NS, Ghannoum MA (2003) Clinical Trichophyton rubrum strain exhibiting primary resistance to terbinafine. Antimicrob Agents Chemother 47:82–86
Osborne CS, Leitner I, Hofbauer B, Fielding CA, Favre B, Ryder NS (2006) Biological, biochemical, and molecular characterization of a new clinical Trichophyton rubrum isolate resistant to terbinafine. Antimicrob Agents Chemother 50:2234–2236
Rudramurthy SM, Shankarnarayan SA, Dogra S, Shaw D, Mushtaq K, Paul RA, Narang T, Chakrabarti A (2018) Mutation in the squalene epoxidase gene of Trichophyton interdigitale and Trichophyton rubrum associated with allylamine resistance. Antimicrob Agents Chemother 62:e02522-17
Singh A, Masih A, Khurana A, Singh PK, Gupta M, Hagen F, Meis JF, Chowdhary A (2018) High terbinafine resistance in Trichophyton interdigitale isolates in Delhi, India harbouring mutations in the squalene epoxidase (SQLE) gene. Mycose 61:477-484
Graser Y, Fari MEL, Vilgalys R, Kuijpers AFA, De Hoog GS, Presber W, Tietz HJ (1999) Phylogeny and taxonomy of the family Arthrodermataceae (dermatophytes) using sequence analysis of the ribosomal ITS region. Med Mycol 37:105–114
White TJ, Bruns T, Lee S, Taylor J (1990) Amplification and direct sequencing of fungal ribosomal RNA genes for phylogenetics. PCR protocols: a guide to methods and applications. Chapter 18, pp. 315–322
CLSI (2008) Reference method for broth dilution antifungal susceptibility testing of filamentous fungi. Approved standard, 2nd ed. CLSI document M38–A2. Clinical and Laboratory Standards Institute, Wayne, PA
Bueno J, Martinez C, Zapata B, Sanclemente G, Gallego M, Mesa AC (2010) In vitro activity of fluconazole, itraconazole, voriconazole and terbinafine against fungi causing onychomycosis. Clin Exp Dermatol 35:658–663
Wiederhold NP, Fothergill AW, McCarthy DI, Tavakko A (2014) Luliconazole demonstrates potent in vitro activity against dermatophytes recovered from patients with onychomycosis. Antimicrob Agents Chemother 58:3553–3555
Baghi N, Shokohi T, Badali H, Makimura K, Rezaei-Matehkolaei A, Abdollahi M, Didehdar M, Haghani I, Abastabar M (2016) In vitro activity of new azoles luliconazole and LAN compared with ten other antifungal drugs against clinical dermatophyte isolates. Med Mycol 54:757–763
Ansari S, Hedayati MT, Zomorodian K, Pakshir K, Badali H, Rafiei A, Ravandeh M, Seyedmousavi S (2016) Molecular characterization and in vitro antifungal susceptibility of 316 clinical isolates of dermatophytes in Iran. Mycopathologia 18:89–95
Esteban A, Abarca ML, Cabanes FJ (2005) Comparison of disk diffusion method and broth microdilution method for antifungal susceptibility testing of dermatophytes. Med Mycol 43:61–66
Adimi P, Hashemi SJ, Mahmoudi M, Mirhendi H, Shidfar MR, Emmami M, Rezaei-Matehkolaei A, Gramishoar M, Kordbacheh P (2013) In-vitro activity of 10 antifungal agents against 320 dermatophyte strains using microdilution method in Tehran. Iranian J Pharm Res 12:537–545
Nowrozi H, Nazeri G, Adimi P, Bashashati M, Emami M (2008) Comparison of the activities of four antifungal agents in an in vitro model of dermatophyte nail infection. Indian J Dermatol 53:125–128
Funding
This study was funded by Iran National Science Foundation: INSF for funding our research (grant number 94003277) to MSG and a PhD grant to ZS by the Research Deputy of Tarbiat Modares University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Salehi, Z., Shams-Ghahfarokhi, M. & Razzaghi-Abyaneh, M. Antifungal drug susceptibility profile of clinically important dermatophytes and determination of point mutations in terbinafine-resistant isolates. Eur J Clin Microbiol Infect Dis 37, 1841–1846 (2018). https://doi.org/10.1007/s10096-018-3317-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3317-4