Abstract
The study was performed to assess potential differences in the etiological relevance of two coagulase-negative staphylococci (CoNS), Staphylococcus haemolyticus and Staphylococcus hominis, in an observational single-center study. Over a 5-year interval, patients in whom there was detected S. haemolyticus or S. hominis of presumed etiological relevance were assessed for the primary endpoint death during hospital stay and the secondary endpoint transfer to an intensive care unit (ICU) after the detection of S. haemolyticus or S. hominis. Patients with S. haemolyticus or S. hominis died in 11.3% (50 out of 444) and 9.5% (60 out of 631) of cases, respectively, and were transferred to ICU after S. haemolyticus and S. hominis detection in 8.7% (19 out of 219) and 11.7% (44 out of 377) of cases, respectively. There was no significance for species-related influence on the primary outcome parameter (P > 0.1), while ICU transfers were more likely for patients with S. hominis detections (P = 0.016). Delayed diagnosis of both CoNS species was associated with an increased probability of death (P = 0.009). The study revealed comparable morbidity caused by S. haemolyticus and S. hominis identified in a clinically relevant context.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coagulase-negative staphylococci (CoNS) are part of the core composition of the microbiota of the human host’s skin and mucous membrane surfaces [1, 2]. Thus, CoNS are frequently detected from nonsterile compartments in the microbiological diagnostic routine [3]. However, they may prove etiologically relevant depending on the source and the individual host susceptibility. Although—compared with Staphylococcus aureus—CoNS lack most virulence factors responsible for invasiveness, they may cause significant infections based primarily on species- and strain-specific abilities to adhere to surfaces and to form biofilms [4].
Staphylococcus haemolyticus is the second most frequently identified CoNS species in blood culture materials [5,6,7]. Moreover, S. haemolyticus accounts substantially for foreign body-related infections and infections in preterm newborns [8,9,10]. In contrast, invasive infections due to Staphylococcus hominis are less commonly reported [11,12,13], comprising particularly cases of nosocomial bloodstream infections. Strains of both species carry the potential for biofilm formation of putative etiological relevance, with biofilm formation being more strain-dependent than species-dependent [14, 15]. Only S. haemolyticus shows hemolytic activity [6, 16, 17]. Recently, phenol-soluble modulins (PSM)—toxins known to have broad cytolytic activity—have been described for S. haemolyticus, including a new α-type PSM [17].
To assess potential differences between the etiological relevance of S. haemolyticus and that of S. hominis, an observational study was performed in a single-center design at the University Medicine Rostock, Germany, during a 5-year interval between 2007 and 2012. Data were included in the assessment from all inpatients for whom S. haemolyticus and S. hominis were differentiated to species level due to suspected clinical relevance.
Patients and methods
Study design
The assessment was conducted as a single-center retrospective observational study between the years 2007 and 2012. Inclusion criteria were as follows:
Cases were identified by screening the laboratory information system (LIS) of the DIN EN ISO 15189-accredited Institute for Medical Microbiology, Virology and Hygiene of the University Medicine Rostock, Germany, for the search terms Staphylococcus haemolyticus and Staphylococcus hominis. As demanded by the institute’s standard operating procedures, differentiation of CoNS is performed only if etiological relevance is suspected by the investigator.
The bacterial isolates assessed in this study were identified using VITEK 2 identification cards (bioMérieux, Marcy-l’Étoile, France) or matrix-assisted laser-desorption-ionization time-of-flight mass spectrometry (MALDI-TOF-MS) with a Shimadzu/Kratos “AXIMA Assurance” MALDI-TOF mass spectrometer (Shimadzu Germany Ltd., Duisburg, Germany). Alpha-cyano-4-hydroxycinnamic acid preparation was done as described by the manufacturer (bioMérieux) for all strains prior to MALDI-TOF assessment. The Vitek MS-ID IVD-mode database version 3.2.0.-6. (bioMérieux) allowed for the analysis of the spectral fingerprints. The equivalence of the two methods in terms of discriminatory power was demonstrated by a minimum of 20 parallel measurements for each species during the establishment of the MALDI-TOF-MS system in the laboratory as mandated for accredited laboratories in Germany. In addition, equivalence was repeatedly confirmed in the literature [18,19,20,21]. Antibiotic resistance patterns were determined using the appropriate VITEK 2 cards.
Cases were included and assessed anonymously after the removal of copy strains in the case of inpatients of the University Medicine Rostock. Each patient was counted only once.
Data were anonymously extracted from the patient case files as detailed below and collected in Microsoft Excel worksheets for further assessment.
Outcome parameters
A primary and a secondary outcome were defined. The primary outcome was death during hospital stay. The secondary outcome parameter was transfer to an intensive care unit (ICU) after the isolation of S. haemolyticus or S. hominis from the patients in the course of the hospital stay.
Assessed factors potentially affecting the outcome
As well as the identification of S. haemolyticus and S. hominis, a broad variety of factors was documented to assess their effects on the outcome parameters. The parameters assessed comprised continuous parameters such as age, duration of hospital stay, and day of pathogen detection after admission to hospital, and also noncontinuous parameters such as gender, documented intensive care procedures and documented invasive procedures, documented medical disorders (cardiac, dermatological, ear-nose-throat, gastrological, hematological, metabolic, neurological, orthopedic, pneumological, sepsis, solid cancers, urological, vascular, wound infections, and other diseases), application of immunosuppressive drugs, cytostatic drugs and antibodies, fever (defined as body temperature ≥ 38.5 °C), left shift of leukocytes, leukopenia, surgical interventions, and the adequate treatment of all isolated CoNS strains by the antibiotic drugs applied.
Sample materials in which S. haemolyticus and S. hominis were identified were categorized as blood cultures, cerebrospinal fluid, deep respiratory secretions, noninvasive swabs, other invasively sampled body fluids, urine, and tissues. Wards were categorized as ICU, surgical wards, and nonsurgical wards. Additionally detected accompanying bacterial flora were clustered as eight so-called accompanying bacterial categories (ABC): nonfermentative rod-shaped bacteria (ABC 1); environmental or colonizing Gram-positive cocci and rod-shaped bacteria (ABC 2); fungi (ABC 3); anaerobic bacteria (ABC 4); Enterobacteriaceae (ABC 5); Enterococcus spp. (ABC 6); Haemophilus spp. and Moraxella spp. (ABC 7); and Streptococcus spp. (ABC 8). Mycobacterium tuberculosis and Staphylococcus aureus, as bacteria with assured or highly likely etiological relevance, were assessed by species.
A table showing the distribution of both the outcome parameters and the potential factors is presented in Supplementary material 1 for both S. haemolyticus and S. hominis. A distribution of the detected antimicrobial resistance by strain—not by patient—is given in Supplementary material 2. Finally, exposure to antibiotic drugs is presented in Supplementary material 3, again by isolate not by patient.
Inclusion criteria
Patients were included if either S. haemolyticus or S. hominis was identified in the microbiological laboratory in any sample material and if clinical information from the case files was available.
Exclusion criteria
The exclusion criterion for the assessment of both outcome parameters was lack of access to the patient-specific case files for organizational reasons. Incompleteness of the assessable dataset was not an exclusion criterion but led to a reduction in the number of interpretable cases. For the assessment of the secondary outcome parameter, patients were additionally excluded if they were at the ICU from the beginning of their hospital stay or if they were not in the ICU during their hospital stay at all.
Statistical assessment
Statistical assessment was based on a Poisson regression model, which was used to identify relevant associations for the outcome parameters by backward selection. Factors with P > 0.1 were excluded from the model. Using this approach, parameters that were originally included in the analysis can be excluded step-by-step to identify the truly relevant parameters. The modeling was performed as described in detail elsewhere [22].
Rep-PCR-based typing
Rep-PCR-based typing was performed as described by the manufacturer on a subset of the assessed strains using the DiversiLab Staphylococcus kit (BioMerieux, Nürtingen, Germany) to demonstrate clonal diversity of the isolates. The strains were chosen randomly to avoid bias due to potential epidemiological association of isolation events. In fact, care was taken to restrict the analysis to only one isolate if even the suspicion of local epidemic transmission was present. Hence, if clusters were revealed during this assessment, at least they were not recognizable a priori from the clinical-epidemiological point of view.
Ethical clearance
Ethical clearance for the assessment was obtained from the Ethics Committee of the University Medicine Rostock (Registration number A 2012-0129). The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Results
Study population
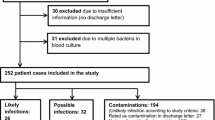
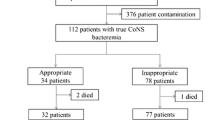
After removal of copy strains, the study population for which clinical data could be retrieved from case files of 1164 patients comprised 483 inpatients with S. haemolyticus detection of presumed etiological relevance and 681 inpatients with potentially relevant S. hominis isolations. The coverages of the assessment as compared with the total numbers of patients with S. haemolyticus or S. hominis detections during the study interval from 2007 to 2012 were 91.9% (444 out of 483) and 92.7% (631 out of 681), respectively.
Using the antimicrobial resistance data of all isolated strains at all times of isolation, i.e., 598 S. haemolyticus and 745 S. hominis strains (Supplementary material 2), and the information on the antimicrobial therapy applied for these isolates (Supplementary material 3), it was assessed whether the antimicrobial therapy administered was appropriate for the CoNS isolates recovered from the patients. Appropriate antibiotic therapy was assumed if an isolate was tested as susceptible for at least one of the antibiotic drugs used. While nearly two out of three S. hominis isolates were treated adequately by the antibiotic drugs used, this was the case for only slightly less than half of the S. haemolyticus isolates (Table 1). With the focus not on isolates but on assessed patients, the percentages were similar. Isolates of 63.3% of patients with S. hominis (n = 431) were treated adequately, but isolates of only 44.3% of patients with S. haemolyticus (n = 214) (Table 1, Supplementary Material 1).
Assessment of the primary study endpoint “death during the hospital stay”
Within the assessed cohort of patients with either S. haemolyticus or S. hominis, there was no statistical relevance of the species for the primary endpoint “death.” The outcome parameter could be extracted from the case files of 1075 patients, i.e., 444 patients with S. haemolyticus and 631 patients with S. hominis. Patients with S. haemolyticus and with S. hominis died in 11.3% (n = 50) and 9.5% (n = 60) of instances, respectively.
Stay in intensive care units was strongly associated with the endpoint death during hospital stay. Other factors associated with an increased risk of dying comprised concomitant detection of the pathogen S. aureus, hematological disease, sepsis, increased patient age, increased number of days in hospital prior to the detection of the CoNS, and left shift in white blood cell microscopy. In contrast, neurological disorders, ear-nose-throat disease, dermatological disease, wound infections, increased hospital stay, and previous surgery were protectively associated factors (Table 2). Adequate treatment with the applied antibiotic drugs according to the susceptibility profiles of the recovered isolates did not show any significant effect.
Assessment of the secondary endpoint “transfer to ICU during the hospital stay”
A total of 596 patients (219 patients with S. haemolyticus and 377 patients with S. hominis) who were not in the ICU before the detection of S. haemolyticus or S. hominis were included in this assessment. Patients were transferred to ICU after S. haemolyticus and S. hominis detection in 8.7% (n = 19) and 11.7% (n = 44) of cases, respectively.
The endpoint “transfer to ICU” was significantly more frequent for detection of S. hominis. Additional identified risk factors comprised proof of CoNS in cerebrospinal fluid, neurological disorders, sepsis, gastrological disorders, left shift in white blood cell microscopy, previous surgical interventions, increased patient age, duration of hospital stay, previous treatment on surgical wards, and concomitant detection of pathogens of ABC 7 (Haemophilus spp. and Moraxella spp.). Apparently “protective” factors (in alphabetical order) were dermatological disease, detection of CoNS in deep respiratory specimens, increased number of days in hospital prior to the detection of the CoNS, orthopedic disease, urological disease, use of immunosuppressive drugs, wound infection, and vascular disease (Table 3). Again, adequate treatment with the applied antibiotic drugs did not show significant effects.
Confirmation of clonal diversity
Rep-PCR analysis of randomly chosen strains with no epidemiological suspicion of nosocomial transmission led to the identification of 3 clonal clusters among 31 assessed S. haemolyticus strains (26/483, 5.4%) and 26 S. hominis strains (25/681, 3.7%), which were believed to be part of small outbreaks. There were 2 S. haemolyticus clusters comprising 3 and 9 isolates, respectively, and an S. hominis cluster comprising 5 isolates. The remaining 40 Staphylococcus spp. strains assessed were not part of detectable clusters in rep-PCR. Moderate molecular diversity with only few and small clonal clusters of the assessed isolates was thereby confirmed.
No patient with isolates from one out of the three identified clonal clusters attained either the primary or secondary outcomes. In comparison, 11.1% (4 out of 36) of patients with cluster-free isolates reached the primary and 25.0% (5 out of 20) reached the secondary outcome, while 9.7% (108 out of 1113) of patients with nonassessed strains reached the primary outcome and 9.4% (61 out of 647) reached the secondary outcome.
Discussion
The study was performed to assess putative differences in the etiological relevance of S. haemolyticus and S. hominis over a study period of 5 years with inpatients at a German University Hospital.
Unlike in previously published papers [5, 6], there was no species-dependent difference regarding the primary outcome parameter death in a multivariate model, and—surprisingly—demonstration of S. hominis was more likely to be associated with the secondary outcome parameter transfer to ICU during the hospital stay than was detection of S. haemolyticus. Of note, delayed diagnosis of both species of CoNS was, however weakly, associated with an increased probability of death. In contrast to previous observations, there was no significant association between proof of CoNS on invasive swabs from deep compartments and risk of death [23].
There were few surprises concerning other observed associations. The high statistical significance for an association of detection of Haemophilus spp. and Moraxella spp. with transfers to ICU is unexpected and is possibly influenced by the comparatively low numbers of affected patients, although respiratory tract infections due to such pathogens can be associated with severe courses. Unlike for the primary outcome death, delayed detection of CoNS was negatively associated with the secondary outcome parameter transfer to ICU, again with comparably weak significance. S. hominis isolates were more frequently treated with antibiotic drugs than were S. haemolyticus isolates and thus one might speculate that S. haemolyticus was less often considered as etiologically relevant by the clinicians and, accordingly, therapeutically neglected. On the contrary, one could argue that detection of S. hominis was more frequently associated with transfer to the ICU and, thus, with severe disease in spite of appropriate therapy. In the event, statistical assessment did not show any significant association between appropriate antibiotic treatment of CoNS and primary or secondary outcome.
The observed low clonality of the coagulase-negative Staphylococcus spp. isolates was in accordance with previous descriptions even for clinically relevant strains [24, 25]. Interestingly, the cluster-associated strains seemed to show lower pathogenicity with focus on the primary and secondary outcome. However, the case numbers were too low for a sound statistical assessment.
The study has a number of limitations. If differentiation of CoNS at species level was performed at all and thus allowed the inclusion of patients with S. haemolyticus or S. hominis in the study, this was regarded as an indication that the investigator in the microbiological routine laboratory considered etiological relevance to be likely. The associated subjectivity is an undeniable limitation of the study. Further, discrimination between community-acquired and hospital-acquired strains was not performed, although previous data on S. lugdunensis revealed potential relevance of this factor [26]. In addition, S. epidermidis, as the species that is most frequently associated with clinical disease among CoNS [27], was not included in the assessment.
In summary, only patients with S. hominis were more frequently transferred to ICU and—comparing S. haemolyticus versus S. hominis—there was no species-specific risk of death.
References
Grice EA, Kong HH, Renaud G, Young AC, NISC Comparative Sequencing Program, Bouffard GG et al (2008) A diversity profile of the human skin microbiota. Genome Res 18:1043–1050
Kaspar U, Kriegeskorte A, Schubert T, Peters G, Rudack C, Pieper DH et al (2016) The culturome of the human nose habitats reveals individual bacterial fingerprint patterns. Environ Microbiol 18:2130–2142
Hall KK, Lyman JA (2006) Updated review of blood culture contamination. Clin Microbiol Rev 19:788–802
Becker K, Heilmann C, Peters G (2014) Coagulase-negative staphylococci. Clin Microbiol Rev 27:870–926
Ing MB, Baddour LM, Bayer AS (1997) Bacteremia and infective endocarditis: pathogenesis, diagnosis and complications. In: Crossley KB, Archer GL (eds) The staphylococci in human disease. Churchill Livingstone Inc, New York, pp 331–354
Takeuchi F, Watanabe S, Baba T, Yuzawa H, Ito T, Morimoto Y et al (2005) Whole-genome sequencing of Staphylococcus haemolyticus uncovers the extreme plasticity of its genome and the evolution of human-colonizing staphylococcal species. J Bacteriol 187:7292–7308
Hitzenbichler F, Simon M, Salzberger B, Hanses F (2017) Clinical significance of coagulase-negative staphylococci other than S. epidermidis blood stream isolates at a tertiary care hospital. Infection 45:179–186
Arciola CR, Campoccia D, An YH, Baldassarri L, Pirini V, Donati ME et al (2006) Prevalence and antibiotic resistance of 15 minor staphylococcal species colonizing orthopedic implants. Int J Artif Organs 29:395–401
von Eiff C, Arciola CR, Montanaro L, Becker K, Campoccia D (2006) Emerging Staphylococcus species as new pathogens in implant infections. Int J Artif Organs 29:360–367
Soeorg H, Huik K, Parm U, Ilmoja ML, Metelskaja N, Metsvaht T et al (2013) Genetic relatedness of coagulase-negative staphylococci from gastrointestinal tract and blood of preterm neonates with late-onset sepsis. Pediatr Infect Dis J 32:389–393
Chaves F, García-Alvarez M, Sanz F, Alba C, Otero JR (2005) Nosocomial spread of a Staphylococcus hominis subsp. novobiosepticus strain causing sepsis in a neonatal intensive care unit. J Clin Microbiol 43:4877–4879
Cunha BA, Esrick MD, Larusso M (2007) Staphylococcus hominis native mitral valve bacterial endocarditis (SBE) in a patient with hypertrophic obstructive cardiomyopathy. Heart Lung 36:380–382
Palazzo IC, d’Azevedo PA, Secchi C, Pignatari AC, Darini AL (2008) Staphylococcus hominis subsp. novobiosepticus strains causing nosocomial bloodstream infection in Brazil. J Antimicrob Chemother 62:1222–1226
Silva PV, Cruz RS, Keim LS, Paula GR, Carvalho BT, Coelho LR et al (2013) The antimicrobial susceptibility, biofilm formation and genotypic profiles of Staphylococcus haemolyticus from bloodstream infections. Mem Inst Oswaldo Cruz 108:812–813
Szczuka E, Telega K, Kaznowski A (2015) Biofilm formation by Staphylococcus hominis strains isolated from human clinical specimens. Folia Microbiol (Praha) 60:1–5
Loyer M, Beaudet R, Bisaillon JG (1990) Comparative study of hemolytic substances produced by coagulase-negative Staphylococcus strains. Infect Immun 58:2144–2148
Da F, Joo HS, Cheung GYC, Villaruz AE, Rohde H, Luo X, Otto M (2017) Phenol-soluble modulin toxins of Staphylococcus haemolyticus. Front Cell Infect Microbiol 7:206
Angeletti S (2017) Matrix assisted laser desorption time of flight mass spectrometry (MALDI-TOF-MS) in clinical microbiology. J Microbiol Methods 138:20–29
Jo SJ, Park KG, Han K, Park DJ, Park YJ (2016) Direct identification and antimicrobial susceptibility testing of bacteria from positive blood culture bottles by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry and the Vitek 2 system. Ann Lab Med 36:117–123
Kassim A, Pflüger V, Preemji Z, Daubenberger C, Revathi G (2017) Comparison of biomarker based matrix assisted laser desorption ionization-time od flight mass spectrometry (MALDI-TOF-MS) and conventional methods in the identification of clinically relevant bacteria and yeast. BMC Microbiol 17:128
Trevisoli LE, Bail L, Rodrigues LS, Conte D, Palmeiro JK, Dalla-Costa LM (2018) Matrix-assisted laser desorption ionization-time of flight: a promising alternative method of identifying the major coagulase-negative Staphylococci species. Rev Soc Bras Med Trop 51:85–87
Barros AJ, Hirakata VN (2003) Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 3:21
von Eiff C, Peters G, Heilmann C (2002) Pathogenesis of infections due to coagulase-negative staphylococci. Lancet Infect Dis 2:677–685
Seo SK, Venkataraman L, DeGirolami PC, Samore MH (2000) Molecular typing of coagulase-negative staphylococci from blood cultures does not correlate with clinical criteria for true bacteremia. Am J Med 109:697–704
Bouchami O, Ben Hassen A, de Lencastre H, Miragaia M (2011) Molecular epidemiology of methicillin-resistant Staphylococcus hominis (MRSHo): low clonality and reservoirs of SCCmec structural elements. PLoS One 6:e21940
Yeh CF, Chang SC, Cheng CW, Lin JF, Liu TP, Lu JJ (2016) Clinical features, outcomes, and molecular characteristics of community- and health care-associated Staphylococcus lugdunensis infections. J Clin Microbiol 54:2051–2057
Deplano A, Vandendriessche S, Nonhoff C, Dodémont M, Roisin S, Denis O (2016) National surveillance of Staphylococcus epidermidis recovered from bloodstream infections in Belgian hospitals. J Antimicrob Chemother 71:1815–1819
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical clearance for the assessment was obtained from the Ethics Committee of the University Medicine Rostock (Registration number A 2012-0129). The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
The requirement for informed consent was not applicable as agreed by the Ethics Committee of the University Medicine Rostock (Registration number A 2012-0129). The study was a retrospective assessment and only blinded data were used.
Rights and permissions
About this article
Cite this article
Frickmann, H., Hahn, A., Skusa, R. et al. Comparison of the etiological relevance of Staphylococcus haemolyticus and Staphylococcus hominis. Eur J Clin Microbiol Infect Dis 37, 1539–1545 (2018). https://doi.org/10.1007/s10096-018-3282-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3282-y