Abstract
In Egypt, pneumococcal vaccines have not yet been introduced as being compulsory. Identification of the circulating serotypes in Egypt is mandatory to determine whether or not the pneumococcal vaccines will be beneficial. The current study aims to identify the serotypes, vaccine coverage, and antimicrobial resistance of Streptococcus pneumoniae colonizing the nasopharynx of Egyptian children younger than 5 years old. The study was conducted in two successive winter seasons (December 2012–February 2013 and December 2013–February 2014). Two hundred children were enrolled, aged from 6 months to 5 years, excluding those with fever, signs of infection, history of antibiotic intake, and hospitalization in the preceding month. Nasopharyngeal (NP) secretions were collected, subjected to culture, and underwent antibiotic susceptibility testing if positive for pneumococci. Real-time polymerase chain reaction (PCR) and serotyping by sequential multiplex PCR for positive cases were included as well. Streptococcus pneumoniae was isolated from 62 subjects. All isolates were sensitive to vancomycin and levofloxacin, but the majority showed resistance to multiple antibiotics. PCR was positive for pneumococci in 113 subjects (56.5%). The most commonly detected serotypes (st) were 6A6B6C (n = 21, 20.8%), 19F (n = 19, 18.8%), 1 (n = 11, 10.9%), 34 (n = 8, 7.9%), and 19A (n = 6, 5.9%). The theoretical coverage of the PCV13 vaccine for the detected serotypes was 72.4%, while that of PCV10 was 65.5%. Based on these percentages, we recommend including pneumococcal conjugate vaccines in the Egyptian national vaccination program.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Streptococcus pneumoniae is one of the most common pathogens causing a wide range of ailments, from otitis media to serious invasive pneumococcal diseases (IPD). Pneumococcal infections are more prevalent in children and the elderly. The resultant pneumonia may be non-invasive or may lead to bacteremia (invasive form), with an estimated ratio of three to one. In the United States and Europe, mortality of IPD amounts to 12%, with a high clinical and economic burden [1]. The disease burden has increased due to the worldwide emergence of antimicrobial resistance [1].
Pneumococcal infections are usually preceded by nasopharyngeal colonization. The main virulence factor of S. pneumoniae is the polysaccharide capsule, which is also used for the classification of pneumococci into serotypes. Ninety serotypes have been identified, based on their reaction with type-specific antisera [2]. Though most S. pneumoniae serotypes can provoke serious disease, only a few serotypes produce the majority of pneumococcal infections and IPD; hence, they were introduced into the formulation of the current vaccines. The ten most common serotypes are estimated to account for about 62% of invasive disease worldwide [2].
Available vaccines include the pneumococcal polysaccharide vaccine (PPV) and the pneumococcal conjugate vaccine (PCV) [3]. PPV23 contains capsular polysaccharide antigens targeting 23 of the most common serotypes of S. pneumoniae [4]. PPV23 is effective in healthy individuals younger than 65 years of age, but not in children less than 2 years of age. PPV23 does not interrupt carriage, has no discernible impact on the population incidence of IPD, and the older and high-risk individuals are less likely to benefit [5].
On the other hand, PCV contains an immunogenic non-pneumococcal protein conjugated to individual pneumococcal polysaccharides [4]. There are currently two commercially available PCVs; PCV10 and PCV13 [1] that are used in infants and young children less than 2 years of age in many countries [4].
In Egypt, pneumococcal vaccines have not yet been introduced as being compulsory in the national vaccination program and no data are available on the rate of carriage, antimicrobial resistance, or the burden IPD. Hence, identification of the circulating serotypes in Egypt is needed in order to determine whether pneumococcal vaccines are potentially beneficial.
Materials and methods
The study was approved by the Research Ethics Committee of the Clinical Pathology Department of Cairo University in January 2013. Children were enrolled after obtaining consent from parents or guardians.
The study was conducted in two successive winter seasons (December 2012–February 2013 and December 2013–February 2014). We enrolled 200 children, aged 6 months to 5 years attending the outpatient general clinics of Cairo University Children Hospital, with a non-infectious disease. We excluded children with fever, signs of infection, history of antibiotic intake, and hospitalization in the preceding month.
Collection of NP secretion
We used nasopharyngeal (NP) patented flocked swabs (Copan Flock Technologies, Brescia, Italy) to collect NP secretions according to the World Health Organization (WHO) guidelines [6]. We transported swabs to the laboratory within 30 min.
Culture of NP secretion
Each NP swab was added to 1 mL of brain heart infusion broth with 15% glycerol [7]. These NP swabs were vortexed for 10 to 20 s and 10 μL of each specimen was streaked on a sheep blood agar plate (BAP). BAPs were incubated at 37 °C in a CO2-enriched atmosphere using a candle jar for 18 to 24 h, and the rest of the broth was aliquoted and stored at −80 °C. Plates were examined and alpha-hemolytic colonies were tested for optochin susceptibility and bile-solubility. Susceptible isolates were identified as S. pneumoniae and tested for antimicrobial susceptibility using disk diffusion and the Etest to confirm susceptibility to penicillin, ceftriaxone, and vancomycin following the guidelines of the Clinical and Laboratory Standards Institute (CLSI) [8].
Molecular methods
DNA was extracted directly from specimens using the DNeasy Blood & Tissue Kit (Qiagen, Valencia, CA), according to the manufacturer’s instructions.
A pneumococcus-specific real-time polymerase chain reaction (PCR) targeting the lytA and Ply genes was performed as described previously [9] with DNA extracts prepared directly from NP specimens. Negative samples were defined as those with cycle threshold (CT) values greater than 35 [10].
Serotyping
Streptococcus pneumoniae serotyping was performed on real-time PCR-positive samples, using the Centers for Disease Control and Prevention (CDC) procedure [11]. We conducted a sequential multiplex PCR on DNA extracted from biological samples. Forty-two primer pairs [12] for serotypes 1, 2, 3, 4, 5, 6A/B/C/D, 7F/A, 7C/7B/40, 8, 9V/A, 9N/F, 10A, 10F/10C/33C, 11A/D, 12F/12A/12B/44/46, 13, 14, 15A/F, 15B/C, 16F, 17F, 18C/18F/18B/18A, 19A, 19F, 20, 21, 22A/F, 23A, 23B, 23F, 24A/B/F, 38/25F/25A, 31, 33F/33A/37, 34, 35A/35C/42, 35B, 35F/47F, and 39 were grouped into eight multiplex reactions. CpsA (pneumococcal capsular polysaccharide synthesis gene) primers [13] were included in each mix as a confirmatory test. The PCRs were performed in 25-μL volumes, with the mixture containing PCR Master Mix (Qiagen) and primers (0.2–0.5 mM each); 5 mL of DNA extract was used in each PCR. Amplification was performed in a SeeAmp Thermal Cycler (Seegene) under the following conditions: 95 °C for 15 min followed by 35 amplification cycles of 94 °C for 30 s, 54 °C for 90 s, and 72 °C for 60 s. A final hold was performed at 72 °C for 10 min.
The PCR products were analyzed by gel electrophoresis on 2% agarose gels in TAE buffer. Gels were stained with ethidium bromide (0.5 mg/mL) and gel images were recorded. The sizes of the PCR products were determined by comparison with the molecular size standard, as well as with the bands of the respective controls.
Forty-one clinical isolates of pneumococci representing different serotypes and serogroups were used as a control set. The serotypes included 1, 2, 3, 4, 5, 6A, 6C, 7C, 7F, 8, 9N, 9V, 10A, 10F, 11A, 11B, 12F, 13, 14, 15A, 15C, 16F, 17F, 18C, 19A, 19F, 20, 21, 22F, 23A, 23B, 23F, 24F, 31, 33F, 34, 35B, 35F, 35A, 38, and 39.
Results
The age distribution of the enrolled children is shown in Table 1.
Streptococcus pneumoniae was cultivated from 62 subjects. 38.5% (n = 77) were healthy children and 61.5% (n = 123) visited the clinic for non-infectious etiology. Table 2 shows the results of antimicrobial susceptibility testing by disk diffusion. All isolates were sensitive to vancomycin and levofloxacin but the majority showed resistance to multiple antibiotics. The minimal inhibitory concentrations (MICs) of penicillin, vancomycin, and ceftriaxone were determined by the Etest (Table 3).
PCR was positive for pneumococci in 113 subjects (56.5%). There was a statistically significant higher rate of PCR-positive cases among infants (70.3%) compared to toddlers (59.4%) and the preschool age group (43.5%) (p = 0.024). No statistically significant differences were found in PCR positivity as per gender and as per presence or absence of non-infectious morbidities.
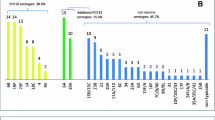
The most commonly detected serotypes (st) were 6A/6B/6C/6D (n = 21, 20.8%), 19F (n = 19, 18.8%), 1 (n = 11, 10.9%), 34 (n = 8, 7.9%), and 19A (n = 6, 5.9%). Four cases each were detected of 18C/18F/18B/18A, 9V/9A, 15B/15C, and 16F, three for each of 5, 23F, and 11A/11D, two for each of 8, 12F/12A/12B/44/46, 9N/9L, 13, 10A, and one for each of 14, 7C/7B/40, 3, 17F, 22F/22A, 24F/24A/24B, 21, 33F/33A/37, and 35B. The following serotypes were not detected: 4, 38/25F/25A, 7F/7A, 23A, 2, 35F/47F, 15A/15F, 39, 23B, 35A/35C/42, 20, 10F/10C/33C, and 31.
There was no statistically significant difference in the distribution of various serotypes according to age, gender, or clinical status (healthy or with non-infectious morbidity).
Comparing the aforementioned serotypes detected in the current samples of Egyptian children to those addressed in the PCV13 and PCV10 vaccines, the percent coverage of PCV13 is 72.4%, while that of PCV10 is 65.5%. Several strains were detected among Egyptian children that are not represented in the two vaccines. Serotypes 34, 15B/15C, 16F, 11A/11D, 8, 12F/12A/12B/44/46, 9N/9L, 13, 10A, 7C/7B/40, 17F, 22F/22A, 24F/24A/24B, 21, 33F/33A/37, and 35B were missing in PCV13 (16 strains). The aforementioned strains, in addition to 19A and 3, were missing in PCV10 (18 strains).
Discussion
Our study detected, by culture and PCR, a high carriage rate of S. pneumoniae among children less than 5 years old (31% and 56.5%, respectively).
Currently, vaccination against S. pneumoniae is not in the national vaccination program in Egypt [14], despite the high burden of disease described. Recently, in a description of IPD in the Arabian Peninsula and Egypt, the most common serotypes/serogroups in the region were 14, 23F, 6B, 19F, and 6A (patients aged ≤ 5 years) [15].
In 1990, Guirguis et al., identified and serotyped 131 strains of pneumococci isolated from meningitis cases in Egypt. The most frequently isolated serotype was 1 (32%). Serotypes 6A, 9L, 12A, 19A, and 29 were next in prevalence. A vaccine was suggested to be administered in the first two years of life [16].
A study by Wasfy et al. [17] examined antimicrobial susceptibility against six antibiotics using disk diffusion and the Etest among 205 isolates of S. pneumoniae, collected from the cerebrospinal fluid of meningitis patients identified between 1998 and 2003, during sentinel meningitis surveillance in Egypt [16]. Five serotypes (6B, 1, 19A, 23F, and 6A) accounted for 37% of the total isolates. Ten isolates (5%) were non-typable. Overall, 29% and 42% of these serotypes were represented in the 7- and 11-valent conjugate vaccines, respectively. However, vaccine coverage for children <2 years old was 38% and 56% for the 7- and 11-valent conjugate vaccines, respectively [17].
Our study confirms the prevalence of the serotypes 1 and 6 as reported before, and adds the emergence of serotypes 19F and 34 among the most commonly detected serotypes [17]. Compared to available conjugate vaccines, PCV13 and PCV10 provide a high coverage to the serotypes detected in our study (72.4% and 65.5%, respectively). Both vaccines do not cover at least 16 of the serotypes circulating in Egypt.
Surveillance of serotypes of S. pneumoniae has been conducted in many countries. In 2010, 26 European countries reported 21,565 cases of IPD to The European Surveillance System (TESSy), with serotyping performed in 46.1% of the cases. The most common serotypes were 19A, 1, 7F, 3, 14, 22F, 8, 4, 12F, and 19F, accounting for 59.8% of the total. Non-susceptibility to erythromycin came first at 17.6%, followed by penicillin at 8.9%. PCV7 serotype coverage among children <5 years old in Europe was 19.2%; for the same age group, the serotype coverages for PCV10 and PCV13 were 46.1% and 73.1%, respectively. Of the 5927 cases for which serotype and age were reported, serotypes 19A and 7F were the most commonly reported in children under 1 year of age. In children aged 1 to 4 years, serotypes 19A and 1 were the most frequently reported [18].
A study from Gambia evaluating NP carriage of S. pneumoniae among 236 infants found 65 serotypes, and the five most common serotypes (6B, 19F, 6A, 14, and 23F) accounted for 51% of isolates [19]. In South Africa, pneumococci were isolated from 121 children out of 303 examined (40%), and the most common serotypes were 6B, 19F, 6A, 23F, 14, and 19A [20]. In Ethiopia, 41.0% of 234 children carried S. pneumoniae [21]. In Ghana, NP pneumococcal colonization was found in 51.4% of 311 children, in accordance with our results [22]. In Tunisia, the most prevalent pediatric serotypes were 1 (32%) and 14 (29%), followed by each of 23F, 6B, 3, 19A, and 19F; 22% of isolates were untyped [23]. In Saudi Arabia, from 2005 to 2010, the most frequently isolated IPD serotypes were 23F, 19F, 6B, 5, and 1 [24]. Note that most of these data are well aligned with ours.
Our results are in broad agreement with studies on carriage in Africa and the Middle East. It appears that types 6A and 6B are the most prevalent, followed by 19F, 1, 23F, and 14, with the first three being the most commonly detected in Egypt.
In conclusion, we detected high rates of carriage of S. pneumoniae among infants and children. The isolates showed high levels of antimicrobial resistance. The most common pneumococcal serotypes were 6A/6B/6C/6D, 19F, 1, 34, and 19A. PCV13 will cover 72.4% of serotypes compared to 65.5% for PCV10. We recommend including pneumococcal conjugate vaccines in the national vaccination program in Egypt.
References
Ludwig E, Bonanni P, Rohde G et al (2012) The remaining challenges of pneumococcal disease in adults. Eur Respir Rev 21:57–65
Gladstone RA, Jefferies JM, Tocheva AS et al (2015) Five winters of pneumococcal serotype replacement in UK carriage following PCV introduction. Vaccine 33:2015–2021
Centers for Disease Control and Prevention (CDC) (2014) Pneumococcal vaccination
Cox CM, Link-Gelles R (2014) Manual for the surveillance of vaccine-preventable diseases. Chapter 11: Pneumococcal
Musher DM (2012) Editorial commentary: should 13-valent protein-conjugate pneumococcal vaccine be used routinely in adults? Clin Infect Dis 55:265–267
Satzke C, Turner P, Virolainen-Julkunen A et al (2013) Standard method for detecting upper respiratory carriage of Streptococcus pneumoniae: updated recommendations from the World Health Organization Pneumococcal Carriage Working Group. Vaccine 32:165–179
Croisier-Bertin D, Piroth L, Charles PE et al (2011) Ceftaroline versus ceftriaxone in a highly penicillin-resistant pneumococcal pneumonia rabbit model using simulated human dosing. Antimicrob Agents Chemother 55:3557–3563
Clinical and Laboratory Standards Institute (CLSI) (2012) Performance standards for antimicrobial susceptibility testing; Twenty second informational supplement. CLSI document M100-S22. CLSI, Wayne, Pennsylvania
Carvalho Mda G, Tondella ML, McCaustland K et al (2007) Evaluation and improvement of real-time PCR assays targeting lytA, ply, and psaA genes for detection of pneumococcal DNA. J Clin Microbiol 45:2460–2466
da Gloria Carvalho M, Pimenta FC, Jackson D et al (2010) Revisiting pneumococcal carriage by use of broth enrichment and PCR techniques for enhanced detection of carriage and serotypes. J Clin Microbiol 48:1611–1618
Centers for Disease Control and Prevention (CDC) (2010) Protocol for Multiplex PCR - S. pneumoniae SEROTYPING - clinical specimens and pneumococcal isolates - African set
Centers for Disease Control and Prevention (CDC). List of oligonucleotide primers used in 41 conventional multiplex* PCR assays for pneumococcal serotype deduction of 70 serotypes
Pai R, Gertz RE, Beall B (2006) Sequential multiplex PCR approach for determining capsular serotypes of Streptococcus pneumoniae isolates. J Clin Microbiol 44:124–131
Ministry of Health and Population (MOHP) (2014) Routine vaccination
Shibl A, Memish Z, Pelton S (2009) Epidemiology of invasive pneumococcal disease in the Arabian Peninsula and Egypt. Int J Antimicrob Agents 33:410.e1–410.e9
Guirguis NI, Helmy MF, Mohamed MR et al (1990) A suggested vaccine formulation for the control of pneumococcal meningitis in Egypt. J Egypt Public Health Assoc 65:291–303
Wasfy MO, Pimentel G, Abdel-Maksoud M et al (2005) Antimicrobial susceptibility and serotype distribution of Streptococcus pneumoniae causing meningitis in Egypt, 1998–2003. J Antimicrob Chemother 55:958–964
Navarro Torné A, Dias JG, Quinten C et al (2014) European enhanced surveillance of invasive pneumococcal disease in 2010: data from 26 European countries in the post-heptavalent conjugate vaccine era. Vaccine 32:3644–3650
Hill PC, Cheung YB, Akisanya A et al (2008) Nasopharyngeal carriage of Streptococcus pneumoniae in Gambian infants: a longitudinal study. Clin Infect Dis 46:807–814
Huebner RE, Wasas AD, Klugman KP; Paediatric Study Group (2000) Prevalence of nasopharyngeal antibiotic-resistant pneumococcal carriage in children attending private paediatric practices in Johannesburg. S Afr Med J 90:1116–1121
Assefa A, Gelaw B, Shiferaw Y et al (2013) Nasopharyngeal carriage and antimicrobial susceptibility pattern of Streptococcus pneumoniae among pediatric outpatients at Gondar University Hospital, North West Ethiopia. Pediatr Neonatol 54:315–321
Denno DM, Frimpong E, Gregory M et al (2002) Nasopharyngeal carriage and susceptibility patterns of Streptococcus pneumoniae in Kumasi, Ghana. West Afr J Med 21:233–236
Marzouk M, Ferjani A, Bouafia N et al (2014) Serotype distribution and antimicrobial resistance of invasive and noninvasive pneumococcal isolates in Tunisia. Microb Drug Resist 21:85–89
Shibl AM, Memish ZA, Al-Kattan KM (2012) Antibiotic resistance and serotype distribution of invasive pneumococcal diseases before and after introduction of pneumococcal conjugate vaccine in the Kingdom of Saudi Arabia (KSA). Vaccine 30(Suppl 6):G32–G36
Said MA, Johnson HL, Nonyane BA et al (2013) Estimating the burden of pneumococcal pneumonia among adults: a systematic review and meta-analysis of diagnostic techniques. PLoS One 8:e60273
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Acknowledgments/funding
None.
Rights and permissions
About this article
Cite this article
Badawy, M., El Kholy, A., Sherif, M.M. et al. Serotypes of Streptococcus pneumoniae in Egyptian children: are they covered by pneumococcal conjugate vaccines?. Eur J Clin Microbiol Infect Dis 36, 2385–2389 (2017). https://doi.org/10.1007/s10096-017-3071-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-017-3071-z