Abstract
Serotyping of Streptococcus pneumoniae is essential for monitoring changes in the pneumococcal population and the impact of vaccines. Recently, various DNA-based methods have become available and are increasingly used because they are cheaper and easier to perform than the Quellung reaction. Our aim was to apply a DNA-based method, capsular sequence typing (CST), to a collection of non-viable lyophilized pneumococcal isolates dating from the 1980s to elucidate the serotypes circulating in Italy 30 years ago. As a preliminary evaluation of the method, CST was applied to 68 recent pneumococcal isolates representative of the most common serotypes circulating in Italy in invasive pneumococcal disease (IPD) previously serotyped by the Quellung reaction. CST was then applied to 132 lyophilized non-viable isolates. A serotype-specific polymerase chain reaction (PCR), using primers suggested by the Centers for Disease Control and Prevention (CDC), was performed when CST did not yield a univocal serotype. Considering the control isolates, CST concordance with the Quellung reaction was 95.6 %. For the non-viable lyophilized isolates, CST identified a univocal serotype for 59.4 % of the isolates. This percentage increased to 78.1 % if CST was combined with serotype-specific PCR. The most frequent serotypes in the collection of non-viable strains were: 3 (15.6 %), 14 (11.7 %), 35B (5.5 %), 19A (5.5 %), and 8 (4.7 %). CST proved to be a valid method for serotyping pneumococcal strains and provided information about pneumococcal serotypes present in Italy 30 years ago. The combination of CST with serotype-specific PCR was an effective strategy to identify pneumococcal serotypes that can be suggested also for routine laboratories.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Streptococcus pneumoniae is an important human pathogen that causes a wide range of infections, including otitis media, sinusitis, pneumonia, and invasive pneumococcal diseases (IPDs), such as meningitis and bacteremia [1]. Streptococcus pneumoniae is responsible for a high rate of morbidity and mortality in the extreme ages of life; that is, in infants and adults over 60 years age, for whom immunization with pneumococcal vaccines is recommended [1].
More than 90 serotypes of S. pneumoniae have been described on the basis of the immunochemical structure of the polysaccharide capsule, the principal virulence factor of S. pneumoniae against which antibodies provide protection [2]. Vaccines in use against the pneumococcus contain the capsular polysaccharides of the most common serotypes associated with serious disease and, over the years, have undergone several changes in their composition. In 1977, a pneumococcal vaccine composed of polysaccharides from 14 different serotypes (14-valent vaccine) was introduced, which was then replaced by a 23-valent vaccine in 1983 [3]. These polysaccharide vaccines were effective in adults but provided low immunogenicity in children younger than 2 years old. This limitation led to the development of vaccines conjugated with carrier proteins to increase immunogenicity [4]. In 2000, the first glycoconjugate vaccine containing seven different serotypes, named PCV7, was introduced in the USA and subsequently in other countries [5]. PCV7 included polysaccharides of serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F, the most common serotypes isolated from infants younger than 5 years old in the USA [6]. PCV7 introduction led to a conspicuous overall decline of IPD associated with vaccine serotypes. Concurrently, however, there was a replacement of vaccine serotypes with non-vaccine serotypes in carriage and infections that led to an increased incidence of IPD associated with less common serotypes. The selective pressure due to immunization also contributed to the expansion of “capsular switch” variants, emerging by a recombination event at the capsular locus (cps) that caused a switch from vaccine to non-vaccine serotype [7]. Higher valency polysaccharides–protein conjugated vaccines, PCV10 and PCV13, were introduced in the following years, including all the PCV7 serotypes with the addition of serotypes 1, 5, and 7F in PCV10 and serotypes 1, 3, 5, 6A, 7F, and 19A in PCV13 [4].
Information about serotype distribution is essential to monitor changes in the pneumococcal population due to the selective pressure of the vaccines in use and to evaluate the possible impact of future vaccines.
Nowadays, different serological and genotyping approaches are used to assign a capsular type to pneumococcal isolates. The Quellung reaction is still considered the gold standard for serotyping, although it has the disadvantage of requiring an expensive array of specific antisera and technical expertise [8, 9]. Several genotyping methods, based on the detection of specific sequences in the capsular loci, have been described and are widely used, such as polymerase chain reaction (PCR)-based serotyping, DNA microarray, and sequence-based methods [4]. Among these, several multiplex PCR assays [10–12] and real-time PCR [13, 14] targeting genes in the cps locus have been developed in the last decade. The most widely used methods are those proposed by the Centers for Disease Control and Prevention (CDC), able to identify up to 40 different serotypes/serogroups by a sequential series of assays (http://www.cdc.gov/streplab/pcr.html). Molecular methods have the advantage of being cheaper and easier to perform and, in addition, do not require viable isolates.
Recently, Elberse et al. developed a new molecular method designed for identifying pneumococcal serotypes, named capsular sequence typing (CST) [15]. In particular, these authors used CST to better understand changes in the pneumococcal population, analyzing a large number of isolates obtained from IPD before and after PCV7 introduction in the Netherlands. CST is based on the amplification and sequencing of a fragment of the capsular gene wzh (cpsB), a regulatory gene involved in tyrosine phosphorylation required for capsule biosynthesis [16]. Elberse and collaborators chose to target wzh because it is conserved enough among the different serotypes to be amplified by using the same set of primers, yet its sequence is divergent in the various serotypes to allow serotype assignment [15].
The aim of this study was to assess the CST feasibility for pneumococcal serotyping and its application on a collection of lyophilized non-viable pneumococcal strains from IPD dating back to the 1980s, in order to elucidate the serotypes circulating in Italy 30 years ago.
Materials and methods
Isolates
As a preliminary step and evaluation of the method, a total of 68 S. pneumoniae isolates were chosen to verify the agreement between the Quellung reaction and CST. The pneumococcal isolates were representative of the 33 most common serotypes circulating in Italy in IPD in recent years (2012–2013) and included all PCV13 serotypes (Table 1). The isolates (1 to 3 for each serotype) had been previously serotyped by the Quellung reaction, using a panel of commercially available antisera produced by the Statens Serum Institut, Copenhagen, Denmark.
To perform molecular analyses, bacteria were grown overnight on Columbia agar plates with 5 % sheep blood at 37 °C in an atmosphere enriched with 5 % CO2. For each isolate, one loopful of the bacterial growth was resuspended in 200 μl of distilled water and heated for 10 min at 95 °C; the lysate was then immediately used for PCR or stored at −20 °C until use.
A total of 132 pneumococcal isolates were available in lyophilized form in the collection of Istituto Superiore di Sanità originating from a surveillance of IPD conducted in Italy during the 1980s [17]. No records describing the source of the isolates or their serotype were found.
Each lyophilized isolate was resuspended in 400 μl of distilled water. No growth was obtained from the lyophilized suspensions on repeated subcultures. For molecular serotyping, DNA was extracted from 200 μl of lyophilized suspensions using the QIAmp DNA Mini Kit (Qiagen, Hilden, Germany).
Molecular analyses: CST
CST is based on the amplification of a fragment of the wzh gene. To amplify the different alleles of wzh, seven amplification primers are used, comprising three forward primers and four reverse primers. Primers are modified with an M13-tail at the 5′ end that allows sequencing of the amplicon with an M13 universal primer pair [15].
The PCR assay to amplify wzh was performed in a 25 μl volume containing Qiagen HotStarTaq mix, 10 μM of each of the seven primers and 5 μl of sample (pneumococcal lysate or DNA extract), according to the protocol described by Elberse et al. [15]. Amplicons were sequenced and DNA sequences were analyzed using DNASTAR Lasergene software (version 8.0.2; DNASTAR, Madison, WI, USA). The sequence of 506 base pairs obtained was then submitted to the CST website (http://www.rivm.nl/mpf/spn/cst) that automatically assigns the capsular type (CT) and the associated serotype of the isolate. The CT is composed of two parts, the first indicating the serotype and the second representing the number of the wzh allele belonging to the same serotype. For example, CT07F-01 indicates the first allele of a strain identified as 7F [15].
If a sample did not yield wzh amplification, PCR for wzg (cpsA), a conserved capsular gene, was performed to confirm S. pneumoniae identification (http://www.cdc.gov/streplab/pcr.html).
When CST did not yield a univocal serotype but multiple serotypes or serogroup(s), or did not yield a known CT but only a best matching CT for a serotype, we tried to determine the specific serotype by performing one or more additional PCR assay(s). Each additional PCR (serotype-specific PCR) targeted each of the serotypes suggested by CST, if specific primers were available. The primers used were derived from the protocol of the CDC for multiplex PCR serotype deduction (http://www.cdc.gov/streplab/pcr.html). The PCR conditions were adapted for single reactions instead of multiplex reactions.
Since, in most cases, CST was not able to distinguish between 6A and 6B, an additional PCR targeting the wcpI gene and sequencing were performed in order to recognize the canonical single point mutation distinguishing 6A from 6B [18].
Results
CST evaluation in control strains
Comparison of the results obtained by the Quellung reaction and CST revealed concordance for 65 out of 68 (95.6 %) of the isolates. In 34 isolates (52.3 %), CST yielded a CT associated with a univocal serotype, while in the other isolates, CST yielded a CT associated with multiple serotypes or serogroup(s) that included the serotype obtained by the Quellung reaction. Only for 3 out of 68 control isolates (4.4 %) were the CST and the Quellung results not concordant (Fig. 1 and Table 1). In one case, the Quellung reaction identified serotype 15C, while CST identified CT23F-06 associated with serotype 15B; in the second case, the Quellung reaction assigned serotype 16F, while CST assigned CT23A-01 associated with serotype 23A; in the third case, the Quellung reaction identified serotype 29 (this result was confirmed at the Statens Serum Institut, Copenhagen, Denmark), while CST identified CT15C-01 associated with serotypes 17A/35B/35C. These discrepancies were confirmed on repeated testing.
CST univocally identified 15 of the 33 serotypes included in this study, in agreement with the Quellung reaction (serotypes 1, 3, 4, 5, 6A, 8, 9V, 10A, 14, 15A, 18A, 19A, 19F, 23A, and 23B). All serotypes included in PCV13 were correctly identified by CST. Nine of these serotypes were identified as univocal serotypes (Table 1). As for the other four PCV13 serotypes, serotypes 7F and 18C were identified at the corresponding serogroup level, while serotype 23F was identified as multiple serotypes including 23F. Of the two serotype 6B isolates, one was associated with the univocal serotype 6B, while the other was associated with serotypes 6A/6B (Table 1).
CST application to lyophilized non-viable strains
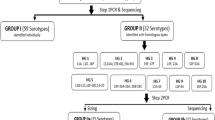
After this evaluation, CST was applied to 132 lyophilized strains that were non-viable in culture. Four of the 132 lyophilized strains did not yield any amplicon for the wzh gene, although they were positive for wzg, indicating that they were, indeed, strains of S. pneumoniae. Among the 128 wzh-positive strains, CST identified a CT associated with a univocal serotype in 76 isolates (59.4 %), with multiple serotypes or serogroup(s) in 50 isolates (39 %), while for two isolates (1.6 %), CST identified a novel CT allele with a sequence not associated to any serotype or serogroup(s) (Fig. 2 and Table 2).
In order to clarify the serotype of isolates for which CST indicated multiple serotypes or serogroup(s), further testing was attempted. Based on the availability of published specific primers, one or more serotype-specific PCR assays targeting each serotype suggested by CST were performed. Out of 42 isolates that were submitted to additional PCR assays, a univocal serotype was obtained for 23 isolates (54.8 %); for 13 isolates (30.9 %), a univocal serogroup was obtained, while for 6 isolates (14.3 %), the serotype remained undetermined (ND) (Fig. 2 and Table 2).
Regarding the two isolates for which CST identified a novel allele, the CST database assigned a best match CT with 99.8 % identity associated with the corresponding serotype 18C and serotype 19A for the two isolates (Table 2). These serotype assignments were confirmed by PCR that identified serogroup 18 and serotype 19A, respectively. The sequences were submitted to the CST database curator, obtaining the new allele designations CT18X-01 and CT19A-09, respectively.
Overall, the combination of CST with serotype-specific PCR was able to characterize 78.1 % of isolates to the serotype level and 17.2 % to the serogroup level.
Four isolates were assigned by CST to serogroup 6. A PCR assay targeting wcpI followed by sequencing of the amplicon was performed to detect the single point mutation distinguishing between serotypes 6A and 6B. The results showed that two of the isolates were serotyped 6A and two were serotyped 6B (Table 2).
On the basis of CST and serotype-specific PCR, the most frequent serotypes in the collection of 132 non-viable Italian IPD strains isolated during the 1980s were: 3 (15.6 %), 14 (11.7 %), 35B (5.5 %), 19A (5.5 %), and 8 (4.7 %); 51 % of the strains were serotypes included in PCV13 (in order of frequency, serotypes 3, 14, 19A, 5, 1, 4, 23F, 19F, and 6A) (Fig. 3).
Discussion
The serotyping of S. pneumoniae is essential to monitor the epidemiology of this microorganism and to evaluate the impact of current vaccines. In the last decade, several molecular methods for pneumococcal serotyping have been described and different multiplex PCR assays have been developed [10–12]. Recently, Elberse and collaborators demonstrated that CST is a useful molecular method for serotyping a large number of S. pneumoniae isolates because of its rapidity and easiness to perform, requiring only one amplification step and sequencing [15, 19]. One limitation that CST shares with multiplex PCR assays and other molecular techniques is that, in several cases, it does not indicate a single serotype but multiple serotypes or serogroup(s). However, CST is able to identify a wide range of serotypes, including rare serotypes, whereas multiplex PCR assays can identify only selected serotypes based on the availability of specific primers.
In this study, we applied CST to a collection of lyophilized non-viable pneumococcal isolates dating back to the 1980s. This collection was potentially precious to gain information about the pneumococcal serotypes causing IPD in Italy 30 years ago.
The feasibility and performance of CST was firstly evaluated with contemporary viable pneumococcal isolates circulating in Italy. The results of this step showed a high concordance (95.6 %) between CST and the Quellung reaction serotyping, in line with data reported by Elberse and collaborators [15]. In only a few cases was there a discrepancy leading to a different serotype. In particular, for one isolate, identified as serotype 15C by the Quellung reaction and as 15B by CST, this cannot be considered a real discrepancy because switching between these serotypes can occur both in vivo and in vitro, and is a reversible phenomenon [20].
Recently, a method similar to CST, named the sequetyping assay, which is also based on amplification of the wzh gene for serotyping S. pneumoniae was developed by Leung et al. [21]. Differences with CST rely on the size of the amplicon, in the number of primers used for the amplification, and in the database used to analyze the sequences and assign the serotype. Dube et al. have applied the sequetyping assay on control pneumococcal isolates and on carriage isolates also tested by real-time multiplex PCR in order to compare the two molecular methods. The results of the control isolates showed a concordance between the Quellung reaction and the sequetyping assay or the real-time multiplex PCR of 88 and 100 %, respectively [22]. When the two molecular methods were applied to a large number of pneumococcal carriage isolates, the Quellung reaction concordance with the sequetyping assay and real-time multiplex PCR was 85 and 52 %, respectively.
The application of CST on lyophilized isolates yielded a univocal serotype for 59.4 % of the isolates. In addition, applying one or more serotype-specific PCRs, a univocal serotype was obtained in 24 other isolates, reaching a total percentage of 78.1 % of isolates serotyped.
Based on our results, we propose an algorithm that combines two molecular methods: CST followed by serotype-specific PCR assay(s) when CST indicates more than one serotype. This algorithm could be applied to serotype viable as well as non-viable pneumococcal isolates and could also be applied to serotype S. pneumoniae directly in clinical samples, without the use of culture. Elberse and collaborators described the use of a modified CST protocol with enhanced sensitivity for directly serotyping S. pneumoniae in DNA extracts from blood samples [23].
An added value of CST is the possibility to use it also in laboratories that do not have the technical expertise of performing the Quellung reaction or that cannot afford the cost of an expensive panel of antisera. The importance of developing a simple and cheap strategy for routine pneumococcal serotyping and serotype surveillance has also been underlined by Jin and collaborators [24], who proposed a combination of the sequetyping assay described by Leung et al. with multiplex PCR. This strategy has been designed for studying the pneumococcal distribution especially in countries such as China, where the conventional Quellung reaction is only available in a few laboratories due to the high cost of the reagents.
In this study, the use of the collection of lyophilized strains dating back to the 1980s has also allowed us to evaluate the distribution of pneumococcal serotypes in Italy during that period; serotypes 3, 14, 35B, 19A, and 8 were more frequent among invasive disease. Two out of the five most common serotypes (serotypes 3 and 8) were included in the 14-valent vaccine that was available at that time [3]. Few studies regarding the pneumococcal serotype distribution in Italy were performed during the 1980s. An Italian multicenter study on the distribution of pneumococcal serotypes conducted in 1979 showed that serotypes/serogroup(s) 19, 6, 3, 20, 9, and 4 were the most common [25]. Another surveillance study dating from 1981 found that serotypes 19A, 3, and 8 were very frequent among S. pneumoniae causing serious diseases in Italy, while serotype 14 was less frequent and serotype 35B was not mentioned [26]. Our results are also in line with the serotype distribution reported in a large surveillance study of S. pneumoniae isolates mainly from European countries, including Italy, obtained in the years 1982–1987, although in this study, serotype 35B was infrequent in both adults and children [17].
The major limit of our study is that no demographic or clinical information of patients, from whom non-viable isolates derived, is available. Therefore, we could not ascertain that our data are representative of overall pneumococcal serotypes circulating in Italy during the 1980s.
In conclusion, even if the Quellung reaction remains the gold standard for pneumococcal serotyping of viable strains, CST has proven to be a valid method for serotyping large collections of both viable and non-viable pneumococcal strains because of the cheapness, easiness of use, and ability to identify rare or uncommon serotypes. CST also has the advantage of a free accessibility database for the assignment of serotype, although our experience suggests that it should be more interactive. The algorithm that we propose combining CST with serotype-specific PCR may increase the possibility of obtaining more univocal results in a very tight timescale and may become a powerful combination for laboratories for routinely serotyping S. pneumoniae strains.
References
Bogaert D, De Groot R, Hermans PW (2004) Streptococcus pneumoniae colonisation: the key to pneumococcal disease. Lancet Infect Dis 4(3):144–154. doi:10.1016/S1473-3099(04)00938-7
Kadioglu A, Weiser JN, Paton JC, Andrew PW (2008) The role of Streptococcus pneumoniae virulence factors in host respiratory colonization and disease. Nat Rev Microbiol 6(4):288–301. doi:10.1038/nrmicro1871
Grabenstein JD, Klugman KP (2012) A century of pneumococcal vaccination research in humans. Clin Microbiol Infect 18(Suppl 5):15–24. doi:10.1111/j.1469-0691.2012.03943.x
Geno KA, Gilbert GL, Song JY, Skovsted IC, Klugman KP, Jones C, Konradsen HB, Nahm MH (2015) Pneumococcal capsules and their types: past, present, and future. Clin Microbiol Rev 28(3):871–899. doi:10.1128/CMR.00024-15
Black S, Shinefield H, Fireman B, Lewis E, Ray P, Hansen JR, Elvin L, Ensor KM, Hackell J, Siber G, Malinoski F, Madore D, Chang I, Kohberger R, Watson W, Austrian R, Edwards K (2000) Efficacy, safety and immunogenicity of heptavalent pneumococcal conjugate vaccine in children. Northern California Kaiser Permanente Vaccine Study Center Group. Pediatr Infect Dis J 19(3):187–195
Pilishvili T, Lexau C, Farley MM, Hadler J, Harrison LH, Bennett NM, Reingold A, Thomas A, Schaffner W, Craig AS, Smith PJ, Beall BW, Whitney CG, Moore MR; Active Bacterial Core Surveillance/Emerging Infections Program Network (2010) Sustained reductions in invasive pneumococcal disease in the era of conjugate vaccine. J Infect Dis 201(1):32–41. doi:10.1086/648593
Wyres KL, Lambertsen LM, Croucher NJ, McGee L, von Gottberg A, Liñares J, Jacobs MR, Kristinsson KG, Beall BW, Klugman KP, Parkhill J, Hakenbeck R, Bentley SD, Brueggemann AB (2013) Pneumococcal capsular switching: a historical perspective. J Infect Dis 207(3):439–449. doi:10.1093/infdis/jis703
Austrian R (1976) The quellung reaction, a neglected microbiologic technique. Mt Sinai J Med 43(6):699–709
Lund E (1960) Laboratory diagnosis of Pneumococcus infections. Bull World Health Organ 23:5–13
Pai R, Gertz RE, Beall B (2006) Sequential multiplex PCR approach for determining capsular serotypes of Streptococcus pneumoniae isolates. J Clin Microbiol 44(1):124–131. doi:10.1128/JCM.44.1.124-131.2006
Brito DA, Ramirez M, de Lencastre H (2003) Serotyping Streptococcus pneumoniae by multiplex PCR. J Clin Microbiol 41(6):2378–2384
Richter SS, Heilmann KP, Dohrn CL, Riahi F, Diekema DJ, Doern GV (2013) Evaluation of pneumococcal serotyping by multiplex PCR and quellung reactions. J Clin Microbiol 51(12):4193–4195. doi:10.1128/JCM.01876-13
Tarragó D, Fenoll A, Sánchez-Tatay D, Arroyo LA, Muñoz-Almagro C, Esteva C, Hausdorff WP, Casal J, Obando I (2008) Identification of pneumococcal serotypes from culture-negative clinical specimens by novel real-time PCR. Clin Microbiol Infect 14(9):828–834. doi:10.1111/j.1469-0691.2008.02028.x
Azzari C, Moriondo M, Indolfi G, Cortimiglia M, Canessa C, Becciolini L, Lippi F, de Martino M, Resti M (2010) Realtime PCR is more sensitive than multiplex PCR for diagnosis and serotyping in children with culture negative pneumococcal invasive disease. PLoS One 5(2):e9282. doi:10.1371/journal.pone.0009282
Elberse KE, van de Pol I, Witteveen S, van der Heide HG, Schot CS, van Dijk A, van der Ende A, Schouls LM (2011) Population structure of invasive Streptococcus pneumoniae in The Netherlands in the pre-vaccination era assessed by MLVA and capsular sequence typing. PLoS One 6(5):e20390. doi:10.1371/journal.pone.0020390
Bender MH, Yother J (2001) CpsB is a modulator of capsule-associated tyrosine kinase activity in Streptococcus pneumoniae. J Biol Chem 276(51):47966–47974. doi:10.1074/jbc.M105448200
Nielsen SV, Henrichsen J (1992) Capsular types of Streptococcus pneumoniae isolated from blood and CSF during 1982–1987. Clin Infect Dis 15(5):794–798
Mavroidi A, Godoy D, Aanensen DM, Robinson DA, Hollingshead SK, Spratt BG (2004) Evolutionary genetics of the capsular locus of serogroup 6 pneumococci. J Bacteriol 186(24):8181–8192. doi:10.1128/JB.186.24.8181-8192.2004
Elberse KE, van der Heide HG, Witteveen S, van de Pol I, Schot CS, van der Ende A, Berbers GA, Schouls LM (2012) Changes in the composition of the pneumococcal population and in IPD incidence in The Netherlands after the implementation of the 7-valent pneumococcal conjugate vaccine. Vaccine 30(52):7644–7651. doi:10.1016/j.vaccine.2012.04.021
Venkateswaran PS, Stanton N, Austrian R (1983) Type variation of strains of Streptococcus pneumoniae in capsular serogroup 15. J Infect Dis 147(6):1041–1054
Leung MH, Bryson K, Freystatter K, Pichon B, Edwards G, Charalambous BM, Gillespie SH (2012) Sequetyping: serotyping Streptococcus pneumoniae by a single PCR sequencing strategy. J Clin Microbiol 50(7):2419–2427. doi:10.1128/JCM.06384-11
Dube FS, van Mens SP, Robberts L, Wolter N, Nicol P, Mafofo J, Africa S, Zar HJ, Nicol MP (2015) Comparison of a real-time multiplex PCR and sequetyping assay for pneumococcal serotyping. PLoS One 10(9):e0137349. doi:10.1371/journal.pone.0137349
Elberse K, van Mens S, Cremers AJ, Meijvis SC, Vlaminckx B, de Jonge MI, Meis JF, Blauwendraat C, van de Pol I, Schouls LM (2015) Detection and serotyping of pneumococci in community acquired pneumonia patients without culture using blood and urine samples. BMC Infect Dis 15:56. doi:10.1186/s12879-015-0788-0
Jin P, Wu L, Oftadeh S, Kudinha T, Kong F, Zeng Q (2016) Using a practical molecular capsular serotype prediction strategy to investigate Streptococcus pneumoniae serotype distribution and antimicrobial resistance in Chinese local hospitalized children. BMC Pediatr 16(1):53. doi:10.1186/s12887-016-0589-7
De Bac C, Andreoni O, Fara GM, Giammanco G, La Placa M, Mascellino MT (1981) A multicentric study for serotyping and susceptibility to antibiotics of pneumococci in Italy. Ric Clin Lab 11(2):145–149
Luzzi I, Gianfrilli P, D’Angelantonio A (1981) Surveillance of Streptococcus pneumonia serotypes circulating in Italy. Ann Sclavo 23(5–6):562–568
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no specific funding.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The authors declare that ethical approval was not required.
Informed consent
The authors declare that informed consent was not required.
Additional information
G. Errico and C. Lucarelli contributed equally to this work.
Rights and permissions
About this article
Cite this article
Errico, G., Lucarelli, C., D’Ambrosio, F. et al. Application of capsular sequence typing (CST) to serotype non-viable Streptococcus pneumoniae isolates from an old collection. Eur J Clin Microbiol Infect Dis 35, 2025–2031 (2016). https://doi.org/10.1007/s10096-016-2755-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2755-0