Abstract
The purpose of this study was to investigate the epidemiological characteristics of carbapenem-resistant Klebsiella pneumoniae (CRKP) in Shanghai Children’s Hospital in China. Twenty-two non-duplicate CRKP strains were collected from pediatric patients between March and June in 2014. Antimicrobial susceptibility testing was conducted by the agar dilution method. Beta-lactamases were characterized by polymerase chain reaction (PCR) and DNA sequencing. The transferability of bla NDM-1 was investigated by conjugation experiment. The plasmids bearing antibiotic resistance genes were characterized by S1 nuclease pulsed-field gel electrophoresis (S1-PFGE) and Southern hybridization. Clonal relatedness was evaluated by PFGE and multilocus sequence typing (MLST). The clinical data of patients were retrospectively reviewed. The 22 CRKP strains were resistant to most of the antimicrobial agents tested, except tigecycline and colistin. Overall, 59, 77, and 100 % of these strains were resistant to imipenem, meropenem, and ertapenem, respectively. The bla NDM-1 was positive in 77.3 % (17/22) of the CRKP strains, of which the 16 isolates from inpatients were designated as ST37 (n = 9) and ST76 (n =7) and one isolate from an outpatient belonged to ST846. The 17 bla NDM-1-positive isolates belonged to PFGE type A (n = 9), type C (n = 7), or type B (n = 1). The plasmids bearing bla NDM-1 could be transferred into recipient Escherichia coli J53 through conjugation in 88.2 % (15/17) of the strains. The hybridization results showed that the plasmids carrying the bla NDM-1 gene were approximately 50–240 kb in size. This is the first report of an outbreak caused by NDM-1-producing K. pneumoniae ST76 and ST37 among neonates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carbapenem-resistant Klebsiella pneumoniae (CRKP) has become a major public concern, which was mainly mediated by the production of carbapenemases [1]. As a novel carbapenemase, NDM-1 was initially reported in 2008 from the K. pneumoniae and Escherichia coli isolated from a Sweden patient who had received medical care in India [2]. Since then, carbapenem-resistant Enterobacteriaceae (CRE) bearing bla NDM-1 and its nine minor variants have been identified all over the world [3–5].
Since the first NDM-1-producing K. pneumoniae was detected in Nanchang, China in 2013, they have spread rapidly in mainland China [6]. To date, NDM-1-producing K. pneumoniae have been reported in several regions of China [7, 8]. However, outbreak in neonates remains uncommon in China. In this study, we observed a soaring number of CRKP sourced from neonatal intensive care unit (NICU) and neonatal wards in less than three months.
Materials and methods
Bacterial strains
Twenty-two non-duplicate sequential strains of CRKP were isolated from Shanghai Children’s Hospital to investigate the epidemiological characteristics. Most (86.5 %, 19/22) of the 22 CRKP were isolated from sputum, and 4.5, 4.5, and 4.5 % were isolated from trachea cannula, urine, and pus, respectively. All the strains were identified using the VITEK 2 Compact system (bioMérieux, France). Escherichia coli ATCC 25922, Salmonella ser. Braenderup H9812, and E. coli J53 (sodium azide resistant) were used as the quality control for antimicrobial susceptibility testing, reference marker for pulsed-field gel electrophoresis (PFGE), and recipient strain for conjugation experiment, respectively.
Antimicrobial susceptibility testing and β-lactamase characterization
Antimicrobial susceptibility testing was performed using the agar dilution method. The results were interpreted following the criteria of the Clinical and Laboratory Standards Institute (CLSI; 2014) [9]. Breakpoint minimum inhibitory concentrations (MICs) of tigecycline were determined following the guidelines of the U.S. Food and Drug Administration (MIC ≤2 mg/L denoting susceptibility and ≥8 mg/L denoting resistance). The presence of genes encoding β-lactamase, including CTX-M-type extended-spectrum β-lactamases (ESBLs), plasmid-borne AmpC β-lactamases, and carbapenemases, were investigated using primers previously described [10–14]. Polymerase chain reaction (PCR) amplicons were sequenced and the DNA sequences obtained were compared with those available in the NCBI GenBank database using BLAST searches.
Transfer of carbapenemase resistance, plasmid analysis, and bacterial genotyping
Conjugation experiment was carried out with E. coli J53 as the recipient to determine the transferability of the carbapenemase gene, as described previously [15]. Whole-cell DNA of clinical strains embedded in agarose gel plugs, digested with S1 nuclease, was separated by PFGE. Plasmids obtained by PFGE were transferred to nylon membranes and hybridized with digoxigenin-labeled bla NDM-1-specific probes. Clonal relationships were analyzed using PFGE of XbaI-digested genomic DNA as previously described, and the results were analyzed according to the criteria proposed by Tenover et al. [16, 17]. Multilocus sequence typing (MLST) for these isolates was performed as described previously [18].
Clinical epidemiology
The clinical data were reviewed for each patient. Several parameters were assessed, including demographics, prior use of broad-spectrum antimicrobial agents, particularly carbapenems, and potential risk factors for infection or colonization with CRKP. Infection or colonization with CRKP was defined according to the definition of nosocomial infections from the Centers for Disease Control and Prevention (CDC) [19].
Results
Antimicrobial susceptibility testing and β-lactamase characterization
All 22 isolates were resistant to cephalosporin and β-lactam/β-lactamase inhibitor combinations, while none were resistant to tigecycline or colistin. Overall, 59.1, 77.3, and 100 % of these strains were resistant to imipenem, meropenem, and ertapenem, respectively. And 4.5 % (1/22), 4.5 % (1/22), and 90.9 % (20/22) were resistant to amikacin, ciprofloxacin, and aztreonam, respectively (Table 1). Seventeen isolates were bla NDM-1-positive by PCR and DNA sequencing. Of the 17 bla NDM-1-positive isolates, 47 % (8/17) co-harbored bla CTX-M-15 and 5.9 % (1/17) co-harbored bla DHA-1. No carbapenemase genes were detected among the remaining four isolates; however, 50 % (2/4) of isolates produced bla CTX-M-15. Half (11/22) of the isolates carried class 1 integron, while sequence data showed that none has resistant gene cassettes. No other PCR products were obtained for any of the other genes investigated (Table 1).
Transfer of carbapenemase resistance, plasmid analysis, and bacterial genotyping
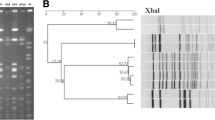
The 17 bla NDM-1-positive K. pneumoniae isolates were selected for conjugation. The results of conjugation experiments indicated that the plasmids with bla NDM-1 from 15 isolates were successfully transferred from donors to recipient E. coli J53, and the conjugants exhibited high resistance to carbapenems, consistent with the detection of bla NDM-1. The MICs of imipenem, meropenem, and ertapenem for the conjugants ranged from 1 to 8 mg/L, and the antimicrobial susceptibility patterns of the conjugants were similar to their donors (Table 1). Hybridization analysis showed that the plasmids carrying the bla NDM-1 gene were approximately 50–240 kb in size (Fig. 1).
Five distinct PFGE patterns (PFGE types A–E) were observed among the 22 CRKP isolates: type A (11/22, 50 %), type C (8/22, 36.4 %), and one isolate each for type B, type D, and type E (Fig. 2). Five distinct MLST sequence types (STs) were observed among the 22 CRKP isolates, including ST76 (n = 8), ST37 (n = 11), ST846 (n = 1), ST11 (n = 1), and ST571 (n = 1). Of the 17 bla NDM-1-positive K. pneumoniae isolates, 16 from inpatients were identified as ST76 (n = 7) and ST37 (n = 9) and one isolate from an outpatient belonged to ST846. One bla KPC-positive K. pneumoniae belonged to ST11 (Fig. 2).
Clinical epidemiology
The clinical details of the patients are shown in Table 1. The 22 isolates were identified in a diverse population of children. The median age of the 22 children (17 males and 5 females) was 1 month (range, 1 day to 12 years). The most common underlying conditions were neonatal respiratory distress syndrome (27.3 %, 6/22), pneumonia and bronchopneumonia (31.8 %, 7/22), and neonatal asphyxia or perinatal asphyxia (13.6 %, 3/22). Indwelling devices were used in some patients, including endotracheal tube (45.5 %, 10/22), arteriovenous intubation (31.8 %, 7/22), mechanical ventilation (9.1 %, 2/22), urinary catheter (9.1 %, 2/22), and gastric tube (9.1 %, 2/22). Most patients (81.8 %, 18/22) were treated with antimicrobial agents, including ampicillin–sulbactam, cefotaxime, ceftriaxone, imipenem, and meropenem. Most patients were improved or discharged after treatment, except for two deaths (Table 1).
Discussion
Infectious diseases caused by NDM-1-producing isolates were known to be associated with significant morbidity and mortality, which was even worse among pediatric populations due to limited therapeutic options [20]. All the isolates were susceptible to tigecycline and colistin in our study; however, tigecycline is not recommended in children because of the risk of dental staining and, currently, colistin is not available for patients in China. Besides, aminoglycosides and fluoroquinolones are also restricted in children due to nephrotoxicity and ototoxicity. In the absence of effective antibiotic therapy, early monitoring of CRKP infection or colonization on admission may play a more important role for timely control of the spread of CRKP [21].
In our study, K. pneumoniae ST76 (n = 8) and ST37 (n = 11) were predominant epidemic clones. Although both STs did not belong to the most common NDM-1-positive clones (ST14 and ST11), K. pneumoniae ST37 has also been reported in India, the UK, and the USA, while K. pneumoniae ST76 bearing bla NDM-1 was reported for the first time in this study [22]. The results of clinical epidemiology indicated that the risk factors for acquiring CRE isolates included invasive procedures (especially surgical operations), indwelling urinary catheters, change of sickbeds, and previous in-hospital cephalosporin use [23]. Our study indicated that immunodepression, invasive procedures, and prior use of broad-spectrum antibiotics might increase the chance of infection or colonization of CRE isolates. In our study, two pediatric patients died of K. pneumoniae ST37 infection, while no patients died of K. pneumoniae ST76 infection.
It is noteworthy that no carbapenemase resistance genes were detected in 18.2 % (4/22) of the CRKP strains. We suspect that a new mechanism, such as the presence of new metallo-β-lactamases or variants of certain carbapenemases, might contribute to the resistance to carbapenems. Further studies are needed to confirm this point. In this study, we reported a nosocomial outbreak of bla NDM-1-producing K. pneumoniae ST37 and ST76 in neonates. Although two outbreaks involving K. pneumoniae ST17 and ST20 were reported recently, to our knowledge, this is the first report of an NDM-1-producing K. pneumoniae ST37 and ST76 outbreak [24, 25]. The vulnerability to colonization or infection with CRE isolates among pediatric patients highlights the necessity of intervention with strict infection-control measures, including proper hand hygiene, contact precautions, and cohort nursing care, to reduce the cross-infection and avoid the rapid spread or clonal dissemination of carbapenemase-producing Enterobacteriaceae strains in healthcare facilities.
References
Queenan AM, Bush K (2007) Carbapenemases: the versatile beta-lactamases. Clin Microbiol Rev 20(3):440–458
Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee K, Walsh TR (2009) Characterization of a new metallo-beta-lactamase gene, bla NDM-1, and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob Agents Chemother 53(12):5046–5054
Tada T, Miyoshi-Akiyama T, Dahal RK, Sah MK, Ohara H, Kirikae T, Pokhrel BM (2013) NDM-8 metallo-beta-lactamase in a multidrug-resistant Escherichia coli strain isolated in Nepal. Antimicrob Agents Chemother 57(5):2394–2396
Göttig S, Hamprecht AG, Christ S, Kempf VA, Wichelhaus TA (2013) Detection of NDM-7 in Germany, a new variant of the New Delhi metallo-beta-lactamase with increased carbapenemase activity. J Antimicrob Chemother 68(8):1737–1740
Rahman M, Shukla SK, Prasad KN, Ovejero CM, Pati BK, Tripathi A, Singh A, Srivastava AK, Gonzalez-Zorn B (2014) Prevalence and molecular characterisation of New Delhi metallo-beta-lactamases NDM-1, NDM-5, NDM-6 and NDM-7 in multidrug-resistant Enterobacteriaceae from India. Int J Antimicrob Agents 44(1):30–37
Hu L, Zhong Q, Tu J, Xu Y, Qin Z, Parsons C, Zhang B, Hu X, Wang L, Yu F, Pan J (2013) Emergence of bla NDM-1 among Klebsiella pneumoniae ST15 and novel ST1031 clinical isolates in China. Diagn Microbiol Infect Dis 75(4):373–376
Qin S, Fu Y, Zhang Q, Qi H, Wen JG, Xu H, Xu L, Zeng L, Tian H, Rong L, Li Y, Shan L, Xu H, Yu Y, Feng X, Liu HM (2014) High incidence and endemic spread of NDM-1-positive Enterobacteriaceae in Henan Province, China. Antimicrob Agents Chemother 58(8):4275–4282
Wu HS, Chen TL, Chen IC, Huang MS, Wang FD, Fung CP, Lee SD (2010) First identification of a patient colonized with Klebsiella pneumoniae carrying bla NDM-1 in Taiwan. J Chin Med Assoc 73(11):596–598
Clinical and Laboratory Standards Institute (CLSI) (2014) Performance standards for antimicrobial susceptibility testing; Twenty-fourth informational supplement. CLSI document M100-S24
Datta P, Gupta V, Garg S, Chander J (2012) Phenotypic method for differentiation of carbapenemases in Enterobacteriaceae: study from north India. Indian J Pathol Microbiol 55(3):357–360
Woodford N, Fagan EJ, Ellington MJ (2006) Multiplex PCR for rapid detection of genes encoding CTX-M extended-spectrum (beta)-lactamases. J Antimicrob Chemother 57(1):154–155
Poirel L, Walsh TR, Cuvillier V, Nordmann P (2011) Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis 70(1):119–123
Dallenne C, Da Costa A, Decré D, Favier C, Arlet G (2010) Development of a set of multiplex PCR assays for the detection of genes encoding important beta-lactamases in Enterobacteriaceae. J Antimicrob Chemother 65(3):490–495
Goldstein C, Lee MD, Sanchez S, Hudson C, Phillips B, Register B, Grady M, Liebert C, Summers AO, White DG, Maurer JJ (2001) Incidence of class 1 and 2 integrases in clinical and commensal bacteria from livestock, companion animals, and exotics. Antimicrob Agents Chemother 45(3):723–726
Borgia S, Lastovetska O, Richardson D, Eshaghi A, Xiong J, Chung C, Baqi M, McGeer A, Ricci G, Sawicki R, Pantelidis R, Low DE, Patel SN, Melano RG (2012) Outbreak of carbapenem-resistant Enterobacteriaceae containing bla NDM-1, Ontario, Canada. Clin Infect Dis 55(11):e109–e117
Schlesinger J, Navon-Venezia S, Chmelnitsky I, Hammer-Münz O, Leavitt A, Gold HS, Schwaber MJ, Carmeli Y (2005) Extended-spectrum beta-lactamases among Enterobacter isolates obtained in Tel Aviv, Israel. Antimicrob Agents Chemother 49(3):1150–1156
Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, Persing DH, Swaminathan B (1995) Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol 33(9):2233–2239
Diancourt L, Passet V, Verhoef J, Grimont PA, Brisse S (2005) Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J Clin Microbiol 43(8):4178–4182
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections, 1988. Am J Infect Control 16(3):128–140
Patel G, Huprikar S, Factor SH, Jenkins SG, Calfee DP (2008) Outcomes of carbapenem-resistant Klebsiella pneumoniae infection and the impact of antimicrobial and adjunctive therapies. Infect Control Hosp Epidemiol 29(12):1099–1106
Pannaraj PS, Bard JD, Cerini C, Weissman SJ (2015) Pediatric carbapenem-resistant Enterobacteriaceae in Los Angeles, California, a high-prevalence region in the United States. Pediatr Infect Dis J 34(1):11–16
Giske CG, Fröding I, Hasan CM, Turlej-Rogacka A, Toleman M, Livermore D, Woodford N, Walsh TR (2012) Diverse sequence types of Klebsiella pneumoniae contribute to the dissemination of bla NDM-1 in India, Sweden, and the United Kingdom. Antimicrob Agents Chemother 56(5):2735–2738
Qin X, Yang Y, Hu F, Zhu D (2014) Hospital clonal dissemination of Enterobacter aerogenes producing carbapenemase KPC-2 in a Chinese teaching hospital. J Med Microbiol 63(Pt 2):222–228
Jin Y, Shao C, Li J, Fan H, Bai Y, Wang Y (2015) Outbreak of multidrug resistant NDM-1-producing Klebsiella pneumoniae from a neonatal unit in Shandong Province, China. PLoS One 10(3):e0119571
Zhang X, Li X, Wang M, Yue H, Li P, Liu Y, Cao W, Yao D, Liu L, Zhou X, Zheng R, Bo T (2015) Outbreak of NDM-1-Producing Klebsiella pneumoniae causing neonatal infection in a teaching hospital in mainland China. Antimicrob Agents Chemother 59(7):4349–4351
Acknowledgments
This work was supported by the National Natural Science Foundation of China (grant no. 81273559), the Shanghai Municipal Commission of Health and Family Planning (grant no. 20124026), the National Major Scientific and Technological Special Project for “Significant New Drugs Development” (grant no. 2014ZX09507009-027), and the Zhejiang Provincial Natural Science Foundation of China (grant no. Y12H190008). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
J. Zhu and L. Sun contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhu, J., Sun, L., Ding, B. et al. Outbreak of NDM-1-producing Klebsiella pneumoniae ST76 and ST37 isolates in neonates. Eur J Clin Microbiol Infect Dis 35, 611–618 (2016). https://doi.org/10.1007/s10096-016-2578-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2578-z